* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Key Points: Neuroscience Exam #2 Lecture 16 and 17: Development of
Synaptogenesis wikipedia , lookup
Proprioception wikipedia , lookup
Neuroesthetics wikipedia , lookup
Optogenetics wikipedia , lookup
Caridoid escape reaction wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Time perception wikipedia , lookup
Human brain wikipedia , lookup
Affective neuroscience wikipedia , lookup
Microneurography wikipedia , lookup
Environmental enrichment wikipedia , lookup
Emotional lateralization wikipedia , lookup
Cortical cooling wikipedia , lookup
Development of the nervous system wikipedia , lookup
Neuroeconomics wikipedia , lookup
Central pattern generator wikipedia , lookup
Neuroplasticity wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Limbic system wikipedia , lookup
Evoked potential wikipedia , lookup
Embodied language processing wikipedia , lookup
Muscle memory wikipedia , lookup
Aging brain wikipedia , lookup
Cognitive neuroscience of music wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Circumventricular organs wikipedia , lookup
Orbitofrontal cortex wikipedia , lookup
Neuroanatomy of memory wikipedia , lookup
Neural correlates of consciousness wikipedia , lookup
Hypothalamus wikipedia , lookup
Premovement neuronal activity wikipedia , lookup
Synaptic gating wikipedia , lookup
Basal ganglia wikipedia , lookup
Cerebral cortex wikipedia , lookup
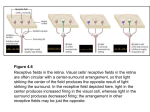
Key Points: Neuroscience Exam #2 Lecture 16 and 17: Development of the NS I and II see David’s study guide Day 18: prechordal plate and notochord signal overlying ectoderm to differentiate into neuroepithelia cells o Begins at the CRANIAL end of the embryo and proceeds caudally o Forms the neural plate every NS structure is derived from the neural plate and formation ends at the end of the 4th week o Neural groove will become the ventricular system of brain and central canal of SC Day 22: neural plate invaginates in the midline to form the neural groove o Cells in the lateral lip of the neural groove will proliferate in a process known as neuralation o As the neural plate cells proliferate, they create folds lateral to the neural groove (these grow upward and inward) As the neural fold develop, neural crest cells begin to differentiate at the crest of the folds these will migrate out and form many structures of the PNS as well as others DRG and sympathetic chain ganglia and enteric ganglia allows you to interact with you environment Teath, CT around the eye, cilliary muscles, septum in the heart, pharyngeal arch cartilage (hyoid), dermis and hypodermis of the face and neck, adrenal medulla (sympathetic chain ganglia-like), schwann cells, enteric ganglia, arachnoid and pia matter, melanocytes o Albinism is caused by defect in neural crest migration o o They eventually meet in the midline at day 22 in the region that the 1st 5 somites The closure forms a hollow tube: neural tube (ectoderm) the closure proceeds cranially and caudally in both directions Day 24: cranial neuropore closes Day 28: caudal neuropore closes; both neural tubes are closed o Closure of the neuropores coincides with the establishment of a vascular circulation for the neural tube. The walls of the neural tube thicken to form the brain and spinal cord o Anytime the neuropores do not close, you end up with an open NS and parts can be missing th 4 week (29 days): embryo undergoes flexure of the cranial region to define developing brain regions (only regions bc they have not differentiated yet) o Prosencephalon= forebrain o Mesencephalon= midbrain o Rhombencephalon= hindbrain Brain development: Certain transcription factors (Shh, BMP) determine how the NS will be spatially organized The neural tube must form and close appropriately for things to develop in the right places o The neural tube in the spinal cord region keep dividing inward until all that is left is the small central canal 3 primary brain vesicles: o Prosencephalon= forebrain o Mesencephalon= midbrain o Rhombencephalon= hindbrain o As the brain starts to develop, certain flexures form and separate the compartments Cervical flexure between spinal cord and medulla Medulla= not as distinct as the SC tela choroidia forms roof of 4th ventricle o General and special somatic and visceral afferent nuclei form o General and special somatic and visceral efferent nuclei form Not special somatic efferent o Sulcus limitans separates 4th ventricle and medulla Pontine flexure Midbrain flexure between midbrain region and forebrain Patterning: there are opposing gradients that give your ventral and dorsal segments of the spinal cord this is how we get functionally efficient organization of the SC makes sure axons go in the right place o Alar= dorsal (sensory) BMP mainly o Basal= ventral (motor) Shh mainly Lecture 18: Sensory receptors and pathways Sensory receptor types, functions, associated axonal fiber types (e.g., Aβ), rapidly adapting vs. slowly adapting mechanoreceptors o Mechanoreceptors are stimulated by mechanical displacement of some tissue of the body which includes both tactile and position sensations One continues the on and offset of stimuli and one is doing continued presence Rapidly adapting (RA) mechanoreceptors adapt quickly and signal a change in a stimulus (e.g., onset or offset) or movement Meissner corpuscles (touch; flutter) Pacinian corpuscles (pressure; vibration) Slowly adapting (SA) mechanoreceptors signal the continued presence, and intensity, of a stimulus Merkel disks (touch) Ruffini endings (detects steady pressure) Thermoreceptors detect heat and cold (changes in temperature – thermal) Nociceptors (pain receptors) are activated by any factor that damages the tissue (noxious stimuli) o Proprioceptors: knowledge of joint/limb position; information on muscle length, position and tension Proprioceptors found in the muscle spindles and GTO not found in skin A-alpha and beta fiber types o Non-hairy skin o Hairy skin (Glabrous) Thick epidermis Thin epidermis Sweat glands Sebaceous glands. Meissner corpuscles Hair follicle receptors Higher receptor density Ruffini endings Lower receptor density o See slides for fiber types: A-beta= (mechanoreceptors of skin) meisner’s corpuscles, merkel receptor for superficial touch AND pacinian corpuscles and ruffini endings for deep touch and vibration A-delt= (thermo and nocioceptors for skin) free nerve endings for pain and temp (cool) C-fibers= free nerve endings for pain, temp(warm), and itch o Free nerve endings in the skin are modality specific and can detect either pain or touch or pressure or temperature Receptor potentials 2-point discrimination and receptive fields o Receptive fields: the area that would stimulate one nerve would constitue its receptive field o 2-point discrimination: determines how sensitive an area of your body is how far apart do they have to be in order to determine that there are two stimuli On your back, there is a greater distance than in the finger and tongue Larger distance= less dense sensory innervation Smaller distance= more sensitive o o Know your pathways – I could lesion anything Brown Sequard syndrome Lecture #19: Spinal reflexes- Atance Intro to reflexes: Reflex= reaction of muscles or glands to a stimulus mediated by simple neuronal circuits consisting of a sensory neuron, one or more interneurons, and a motor neuron o Interneuron relays the info to the motor neuron to withdraw from the stimulus Types of reflexes: o Somatic reflex: skeletal muscle Innate reflexes= patellar reflex Developed reflexes= learned over time driving, hitting a baseball o Autonomic reflex (visceral): increase HR, sweating, etc Processing site: interneurons can be in the spinal cord or in the brain Purpose of reflexes: Reflexes are automatic, stereotyped responses that prevent us from having to think about all the little details required from day to day living o Posture, locomotion, protection, visceral activity Spinal reflexes: Delayed awareness: spinal reflexes occur without immediate conscious awareness you will feel pain later bc it has to go up to higher centers Reflex suppression: reflexes can be suppressed by conscious thought (higher centers) o You can hold on to a pot of boiling water in order to save a child from getting burnt Purpose of spinal reflexes: o Once you make a decision to walk, we no longer need to use higher centers to continue walking perpetuation of activity is via central pattern generators (rhythmic patterns) o Reflexes work to continue to maintain balance and reestablish your walking pattern o Decerebrate animals (where brain and spinal cord has been cut) can still walk due to reflexes and central pattern generator o Clinical: testing reflexes can determine level of the lesion (hyper or hypo-reflexive) Muscle spindles give info about length of muscle and GTO give info about the tension on the muscle o provide continuous, subconscious feedback to the spinal cord, cerebellum, and cortex o they also play a role in proprioception (where your body is in space) knowledge of the position of your fingers on an object give you a better idea of what the object is easier than just brushing it across your fingers o Muscle spindle anatomy Extrafusal fibers allow the muscle to contract Intrafusal fibers are involved in sensation and on the inside of the muscle spindle Spindle is encapsulated Gamma motor neurons supply the intrafusal fibers and alpha motor neurons innervate the extrafusal fibers Two types of γ-motor neurons supply the contractile regions of the intrafusal fibers Dynamic γ-motor neurons supply the bag fibers (arranged randomly) Static γ-motor neurons supply the chain fibers (arranged in a chain) o Muscle spindle function: sensory Providing info on the length of the muscle by determining how much the muscle is stretched Determine info based on dynamic and static stretch response o Static= measure of the amount of stretch Type II are sensitive to the amount of stretch but not the rate; when tension is released, these are quite of AP o Dynamic= how fast is the stretch occurring Type Ia are sensitive to change in rate of stretch o Muscle spindle function: motor If a muscle gets stretched, the immediate response is going to want to contract If there is a contraction reflexively of the extrafusal fibers via alpha motor neuron in response to the stretch in the intrafusal fibers, there must be a co-activating contraction from gamma motor neurons of the intrafusal fibers in order to continue to monitor stretch in that muscle If there was not a concurrent contraction, then the intrafusal fibers could no longer monitor stretch in that muscle this is why gamma motor neuron activation is so important to allow the intrafusal fibers to do their stretchsensing work o Stretch reflex Reciprocal inhibition of the antagonist must occur so that the reflex can work properly Dynamic vs static Type I= dynamic initial contraction Type II= static to slow the reflex down and control it after the initial response If the muscle spindles are damaged, the muscle contraction is not as smooth and controlled o Goli tendon organs: encapsulated and embedded in the tendon will serve 10-15 muscle fibers Type IB serves the GTO determines the amount of tension based on the amount on the amount of collagen fiber displacement These are inflexible and non-adapting There is an interneuron in the SC and there is an inhibitory neuron that causes reflexive relaxation Relaxation of a muscle in response to a buildup of tension The GTO is also working to balance out the stretch and relax inputs Flexor-relfex o You must have a counterbalance between withdraw and maintaining balance Called crossed extensor reflex: One would flex to withdraw and the other leg extensors would contract to keep balance o After-discharge= allows you to maintain withdraw bc the spinal reflex fatigues very quickly o Reverberatory Circuits= allows you to stay away from a stimulus after withdrawing initially Lecture #20: Cortical brainstem control of motor function Primary motor cortex, premotor area, and supplementary motor area function. o PMA: intention to perform a movement and selection of a movement based on external events o SMA: involved in programming complex sequences of movements and coordinating bilateral movements, especially selecting movements based on remembered sequences of movements. o Premotor & supplementary motor areas help in planning movement; precise control of complex sequences of voluntary movements. Receive projections from: Prefrontal cortex (decision making) Parietal association areas (spatial relationships between body & external world) o The brainstem also comes into play through a collective group of tracts that give inputs to body movements Vestibular nuclear complex (balance: lateral subdivision; positioning of head & neck: medial subdivision) Reticular formation (affects the body position, coordination) Red nucleus (exerts control over tone of distal flexor muscles) Superior colliculus (initiates orienting movements of the head and eyes; saccades) Alpha and gamma motor neurons. o Alpha MN supply the extrafusal fibers in muscle; they contact them directly and are called lower motor neurons Means by which the NS can exert control over body movements o Gamma MN supply contractile portions of the intrafusal fibers inside the muscle spindle Alpha-gamma coactivation helps sense changes in load during movement UMN vs. LMS: what are they, what lesions of each would result in. o UMN= where the command for movement begins (precentral gyrus) until it synapses with LMN in the ventral horn of the SC o LMN= after synapse in the ventral horn, the nerves exit the SC and travel to the effector Sign UMN lesions: CP, TBI, stroke, MS, LMN lesions: poliomyelitis, lesions corticospinal tract injury near spinal cord weakness YES YES atrophy No Yes fasiculations no Yes reflexes Increased: hyperreflexia Decreased: hyporeflexia tone Increased: hypertonia Decreased: flaccid o Fasciculation: abnormal muscle twitches due to spontaneous muscle activity o Increased resistance to passive stretching of muscles (spasticity, hypertonia) vs. reduced resistance to passive stretching (hypotonia) Medial and lateral motor systems: Location of termination within the spinal cord, general function of each in motor control. Pathway Site of origin Site of termination Function in motor control Primary motor cortex and supplementary area Medial VST: med and inf vestibular nuclei Lateral VST: lat vestibular nucleus Pontine and medullary reticular formation Cervical and thoracic cord – sends out bilateral projections Med VST: cervical and upper thoracic Lat VST: entire cord Control of bilateral axial and girdle muscles Reticulospinal Superior colliculus Cervical cord Lateral systems Lateral corticospinal Precentral gyrus Entire cord Rubrospinal Red nucleus Cervical cord Medial systems Anterior corticospinal Vestibulospinal Tectospinal Entire cord Med VST: positioning of the head and neck Lat VST: balance **maintain position Automatic posture and gait-related movements Orientation based on auditory stimuli Movement of contralateral limbs Movement of contralateral limbs; tone of distal flexor muscles o Somatotopy in the ventral horn: most medial= axial muscles posterior= flexors most lateral= limbs anterior= extensors Motor functions of the cranial nerves, what lesions of each would result in. o Motor nuclei are more medially and sensory nuclei are more lateral o CN 3 (oculomotor), 7 (facial), 9 (glossopharyngeal), and 10 (vagus) are involved with the parasympathetics o Somatic motor: extraocular muscles and intrinsic tongue muscles Occulomotor, trochlear, abducens, and hypoglossal nerves and brainstem nuclei o Brachial motor: muscles of mastication, facial expression, middle ear, pharynx (swallowing), larynx (voicebox), SCM, upper portion of trap Brainstem nuclei and CN: Motor nucleus of CN 5 (trigeminal), facial nucleus (CN 7facial), nucleus ambiguous (CN 9, 10- glossopharyngeal, vagus), accessory spinal nucleus (CN 11- accessory) o Corticobulbar tract= leads to the motor neurons in the brainstem nuclei (5, 7, 12) Nuclei stimulate muscles of the face that are under the finest control (lip and tongue muscles) and muscles of the jaw and pharynx Distributes bilaterally exception= facial nucleus for lower face which receives contralateral projections (causes Bell’s palsy findings) CN Oculomotor (3), trochlear (4), abducens (6) Function 3= most eye movements; PS pupil constriction/lens 4= down and out Lesion 3= eye tracking problems; pupil dilation 4= would deviate up and in **Trigeminal motor (5) Facial nerve (7) Glossopharyngeal (9) 6= Abducts the eye lat in a horizontal direction Brachial motor root supplies muscles of mastication- bilateral projections Brachial motor controlling muscles of facial expression- contralateral projection Stylopharyngeus elevates the pharynx during talking and swallowing, and contributes (with CN X) to the gag reflex Brachial motor= all pharyngeal muscles of the larynx Recurrent laryngeal nerve= intrinsic laryngeal muscles (almost all) Supplies SCM (rotates to opp side) and upper trap 6= eye would deviate medially Weakness of the jaw can be partially compensated for due to bilateral projections UMN lesion= muscle weaknessforehead spared LMN lesion= muscle weakness of entire half of face Dysphagia, speech difficulties Danger of injury during surgery causes temporary voice disturbance and laryngeal spasm ** Hoarseness after surgery is a sign Spinal Accessory (11) Pt would have weakness turning head away from lesion and couldn’t shrug shoulders (ipsalateral weakness) Hypoglossal (12) Tongue movements Tongue would deviate toward side of lesion; contra=UMN, ipsa=LMN ** UMN control reaching the trigeminal motor nucleus is bilateral meaning that unilateral lesions in the motor cortex or corticobulbar tract usually cause little deficit in the jaw movement bc it is partially compensated for Vagus (10) Upper vs. lower motor neuron facial weakness. o Facial nucleus has two divisions: upper face= bilateral projections and lower face= contralateral projections o UMN lesions spare the forehead due to bilateral projections of the UMN to the forehead and orbicularis oculi Orbicularis oculi muscle closes the eyelid o LMN lesions affect the entire half of the face and do not spare the forehead because there is no longer some ipsilateral cortical input remaining to help innervate (and spare) the forehead Any clinically relevant details mentioned. Lecture #21: Basal Ganglia Know the components of the basal ganglia, functional relevance, and circuitry involved o Basal ganglia are a collection of gray matter nuclei located deep in the white matter of the cerebral hemispheres Basal ganglia + Thalamus Movement Cognition Emotion Motivation o Striatum= caudate and putamen Receives all input to the basal ganglia Cortico-striate fibers run from the cortex to the striatum Putamen= Mainly motor and somatosensory cortex Movements, bodily positions Caudate= Mainly association cortex Cognition Bilateral damage of the head of the caudate nucleus= can completely change someone’s personality caudate is closely associated to the association cortexes Ventral striatum (nucleus accumbens) Limbic cortex, hippocampus, amygdala Initiating drive-related behaviors o Lenticular nucleus= globus pallidus and putamen Globus pallidus has an internum (medial) and externum (lateral) o Subthalamic nucleus (diencephalon) o Substantia nigra (rostral midbrain) Pars compacta: (closely packed) widespread modulatory dopaminergic inputs to BG INPUT CENTER Pars reticulata: (loosely packed) BG output OUTPUT CENTER Associated vasculature o ACA= nucleus acumbens and head of caudate nucleus o Anterior choroidal artery= globus pallidus o Perforating branches of the MCA= striatum o Perforating branches of PCA and post communicating= substantia nigra and subthalamic nucleus Direct and indirect pathways involving the basal ganglia o Inputs to the BG: Corticostriatal cortex to striatum motor, somatosensory, association, and limbic cortex Putamen= most important input nucleus for motor control pathways o Most are excitatory and use glutamate Substantia nigra pars compacta another important input Dopaminergic nigrostriatal pathway (substantia nigra to striatum)= excitatory to some cells and inhibitory to others o Outputs to the BG: Substantia nigra pars reticulata conveys info for the head and neck Internal segment of the globus pallidus conveys info for the rest of the body These pathways are inhibitory and use GABA There is a constant tonic inhibition by these output systems Both pathways go to the thalamus (ventral lateral nucleus- VL and ventral anterior nucleus- VA) via thalamic fasciculus o Internal connections in the BG: go from striatum to the internal segment of the globus pallidus (GPi) or substantia nigra pars reticulata (SNPr) Direct: straight from striatum GPi or SNPr Free the thalamus from its state of tonic inhibition by GPi and SNPr Net effect= excitation of the thalamus Indirect (takes a detour): striatum external segment of globus pallidus (GPe) subthalamic nucleus GPi or SNPr o Net effect= inhibition of the thalamus (resulting in inhibition of movements through connections back to the cortex 4 main categories of internal connections: mostly inhibitory o Disinhibition= striatum inhibits GPi and SNPr through excitation from the cortex which inhibits the tonic inhibition by GPi and SNPr on the thalamus thus the net effect is excitation of the thalamus Know the movement disorders, including Parkinson’s disease, Huntingdon’s chorea, Sydenham’s chorea, chorea, athetosis, and hemiballism. o BG disorders can produce either hypokinetic or hyperkinetic movement disorders o Parkinson’s disease (hypokinetic): rigidity, slowness, and marked difficulty initiating movements Loss of dopaminergic neurons in the SNPc (nigrostriatal projections) Ultimately results in decerased input from the thalamus (VL) to the cortex o o o hypokinetic (direct pathway problems) Characterized by asymmetrical “pill-rolling”, resting tremor, and bradykinesia (extreme slowness of movement), rigidity, and shuffling, stooped, flat-footed gait Tremor diminishes during voluntary movement and increases during emotional stress SNPc D1 and D2 are degenerated causes more tonic inhibition of the GPi causes decreased excitation of the thalamus to the cortex hypokinetic disorder Rx= administer levodopa (L-dopa) to help alleiviate some sx Deep brain stimulation= implantation of electrodes to the GPi or subthalamic nuclei to help replace abnormal activity with normal activity Huntington’s disease (hyperkinetic): uncontrolled involuntary movements producing a random pattern of jerks and twists Can’t produce coordinated movement; progressive - usually choreiform (irregular, spasmodic, involuntary movements of the limbs or facial muscles) - movement disorder, dementia, and psychiatric disturbances, ultimately leading to death. CAG repeats in tandem The pathologic hallmark is progressive atrophy of the striatum, especially involving the caudate nucleus (degenerated). Caudate nucleus degenerated decreasing inhibitory influence on GPe and that makes its own inhibitory inputs more active less excitatory input from subthalamic nucleus and more inhibitory from GPe causes inhibition of GPi (tonic inhibition) less tonic inhibition= excitation of the thalamus increased excitation of the cortex= hyperkinetic disorder Rigidity from BG disorders is called “lead pipe rigidity” bc the spasticity is more continuous throughout attempts to bend the limb Look through other disorders briefly not tested Lecture #22: Pathophysiology of genetic neuronal diseases Know the signs & symptoms of each disorder discussed Know the genetic mutation involved, what issues this causes, and how Know the inheritance of each disorder Disease Signs and Sx Fabry Disease Think: dark skin spots and eye issues Episodes of pain (hands and feet), clusters of dark spots on skin (Angiokeratomas), decreased ability to sweat, corneal opacity, retinal and conjuctival issues, GI issues, tinnitus, hearing loss SAUSAGE-LIKE vessels in conj Along with associated conditions… Dystonia, chorea, flailing of limbs, inability to walk, behavioral disturbances (selfmutilation) The infant’s diapers= orange-colored crystal-like deposits (“orange sand”), pink or reddish urine (hematuria), kidney stones/failure, dysphagia, aspiration, aggressiveness Lesch-Nyhan Syndrome Think: behavioral problems and high uric acid NiemannPick Disease Think: Lipids and enlarged spleen/liver Maple Syrup Urine Disease Think: poor feeding, AA build-up, brain toxicity B= non-neurological A= neuro deterioration C= seizures Hepatosplenomegaly, macular cherry red spots, foamy cytoplasm histologically due to lipids Poor feeding, vomiting, lethargy, developmental delay, seizures, hypotonia, intramyelinic edema, vasogenic edema Genetic mutation GLA gene that responsible for making alphagalactosidase A Mutation causes… Inheritance build-up of a particular type of fat (globotriaosylceramide, or GL3) in the body's cells can eventually lead to MI, kidney damage, and stroke X-linked HPRT1 gene: a severe deficiency of the enzyme hypoxanthine phosphoribosyl transferase 1 (HPRT1) Purines are broken down but NOT recycled: overproduction X-linked recessive Type A and B= SMPD1 Type C= NPC1 or NPC2 abnormal lipid metabolism causes harmful amounts of lipids to accumulate in the spleen, liver, lungs, bone marrow, and brain Autosomal recessive BCKDHA, BCKDHB, DBT, and DLD genes Abnormal AA processing and prevent breakdown of leucine, isoleucine, and valine (toxic to brain) Autosomal recessive and accumulation of uric acid which can cause can cause gouty arthritis (arthritis caused by an accumulation of uric acid in the joints), kidney stones, and bladder stones; low levels of dopamine Lecture #23: hypothalamus Identify the structure of the hypothalamus, including the major hypothalamic nuclei and areas. o Lowest level of the diencephalon, situated below the thalamus Bilaterally symmetric structure split by the 3rd ventricle Region sitting right below the thalamus Connects through the infundibulum to the pituitary Pituitary tumors can compress a part of the optic chiasm and cause bitemporal hemianopia o Parts of the hypothalamus based on what is below it: Preoptic (most rostral) before being above the optic chiasm ACA and ant com art Supraoptic= above the optic chiasm ACA and ant com art Area above the tuber cinereum PCA and post com art Posterior part= above the mammillary bodies most caudal PCA and post com art Lateral hypothalamus= supplied by lenticulostriate art from MCA and choroidial branches Outline the major functions of the hypothalamus and its nuclei/areas. o Major functions: HEAL Homeostasis, endocrine control, autonomic control, limbic mechanisms Neural and neurohumoral (direct hormone control) functions The hypothalamus serves as an integrator of autonomic, endocrine, emotional, and somatic functions Nodal point in pathways concerned with homeostasis Coordinates drive-related behaviors o Afferent connections (things coming in) Hippocampus to hypothalamus (periventricular nucleus and mammillary body) via fornix important for limbic system Afferent fibers from olfactory areas to preoptic nucleus and dorsomedial nuclei via medial forebrain bundle Amygdala to hypothalamus via stria terminalis emotion, fear Visceral afferent fibers to hypothalamus via peduncle of mammillary bodies o Efferent connections (things leaving) Dorsal longitudinal fasciculus to parasympathetic nuclei Mamillotegmental tract to tegmentum of midbrain Then relayed to midbrain reticular formation Mediates autonomic info between hypothalamus, CN nuclei, and SC Hypothalamic-hypophyseal tract to pituitary Anterior (adenohypophysis outgrowth of the ectodermal cells of pharynx) o Direct vascular link to directly release hormones Could be releasing hormones or inhibiting hormones) o Optic chiasm in front of it Posterior (neurohypophysis buds down from diencephalon) o Needs a neuronal signal and then can release hormones no direct release o o o Mammillary bodies on the posterior end Supraoptic and paraventricular (on either side of the lateral ventricle) have large neurosecratory cells that produce two hormones depending on need ADH or vasopressin: increase the reabsorption of water in the kidney and decrease production of urine Neurotransmitter function: helps in controlling circadian rhythms Oxytocin: Causes contraction of uterine and mammary smooth muscle; important in parturition and milk letdown Hypothalamic nuclei Medial has three subdivisions (anterior-supraoptic, middle-tuberal, and posterior-mammillary) and lateral has one o Parasympathetic= anterior and med o Sympathetic= lateral and posteromedial o o o o o Circadian rhythms= suprachiasmatic nucleus ant and med Master clock for circadian rhythms, direct retinal projections (getting info about daylight), melatonin receptors Temperature Preoptic (ant-medial): lowers body temp anterior= A/C helps to cool you down Promotes heat loss (sweating, behavioral) and prevent heat production Lesion= hyperthermia in a warm environment Posterior nuclei= raises body temp Promote heat production (shivering, behavioral) and prevent heat loss Lesion= hypothermia in cold environments Feeding and thirst Lateral= initiate feeding based on glucose levels and thirst when dehydrating Lesion= loss of desire to eat (aphasia) possible underlying cause to anorexia and very little fluid intake (adipsia) Medial- tuberal zone= satiety center inhibits food intake stimulated by high glucose levels Lesion= compulsive overeating (hyperphagia) or overdrinking (polydipsia) Sexual behaviors Medial-preoptic nucleus= control sexual dimorphism involving hormonal influences on maturation Contains high density of GNRH producing neurons which synthesize large peptides that are directed at target cells in the anterior pituitary Oxytocin/vasopressin Medial-supraoptic Paraventricular and Supraoptic Nuclei Neurosecretory cells whose axons project to posterior pituitary Secrete oxytocin and vasopressin Systemic feedback to hypothalamus via circumventricular Organs (OVLT, Organum Vaculosum Lamina Terminalis, and SFO, subfornical organ) Predict the role and mechanisms of the hypothalamus as it relates to thirst, hunger, temperature regulation, and the defense mechanism. Distinguish some of the basic disorders associated with hypothalamic dysfunctions Lecture #24: thalamus diencephalon thalamus= major subdivision of the diencephalon (hugging the third ventricle) Thalamic anatomy o Boundries: Most rostral= lamina terminalis (contains organum vasculosum which regulates osmolarity of blood Rostral and dorsal= anterior comminsure Caudal= posterior commissure Anterior pole= interventricular foramen Lateral boundry= internal capsule that divides it from the putamen medial edge= 3rd ventricle caudal to post commissure on top of tectum= pineal gland above/dorsal= lateral ventricle below/ventral= roof of hypothalamus o Medial to lateral in horizontal section: Third ventricle, thalamus, internal capsule, putamen o Caudate and putamen hugging thalamus in horizontal section o Massa intermedia= connects right and left thalamus o Hypothalamic sulcus= separates thalamus and hypo Describe the thalamic nuclei and their functional significance o Thalamus= gateway to the cortex Gateway that has some transforming properties can modulate signals based on inputs from many sources o Internal medullary lamina= Y shaped white matter tract that divides the thalamus into the medial, anterior, and lateral groups 1. Intralaminar nucleus: Central median nucleus= part of ARAS o Afferents from globus pallidus, reticular formation, and sensory pathways o Efferents to stratium (caudate and putamen) Parafascicular nucleus= similar connections o Nonspecific: Connect with cortical areas that have broader functional implications such as association and limbic cortices 2. Anterior nuclear group Main connectivity to cingulate cortex 3. Medial nuclear group (whole group is dorsal medial group 4. Lateral nuclear group (has dorsal and ventral tier and lateral and medial geniculate nucleus Lateral dorsal nucleus and o Also connectivity to cingulate cortex Lateral posterior nucleus o Connectivity to sensory association cortex of parietal lobes Pulvinar: huge chunk of posterior thalamus o largest thalamic nucleus in humans and has extensive connections with parietal-occipital-temporal (POT) association cortex Visual cortical areas Posterior parietal cortex Cingulate, posterior parietal, premotor and prefrontal cortex The pulvinar also has extensive input from the superior colliculus important in the initiation of saccades, regulation of visual attention, and orientation behavior Describe the major “inputs” and “outputs” of the “specific” thalamic nuclei o Specific nuclei: from the ventral tier of the lateral nuclear group and lateral and medial and lateral geniculate nuclei Almost all projections are ipsalateral when going to the cortex (more on the specific nuclei) Ventral tier Ventral anterior nucleus (association motor) o Receive inputs from BG and originate in the GPi and also SNPr o Motor projects to premotor and supplementary motor cortex VA nucleus is an important part of the mechanism by which the BG exerts influence on normal movement Ventral lateral nucleus motor info o Receives inputs from BG and originate in the GPi and also SNPr Also receives input from the dentate nucleus of the cerebellum o Motor projects to primary motor cortex (precentral gyrus) Ventral posterior nucleus sensory info o Lateral subdivision (VPL) Receives inputs from PCML and spinothalamic inputs from LE and UE and projects to primary sensory cortex (postcentral gyrus) Fine touch and proprioception (PCML) Pain and temp (spinothalamic) o Medial subdivision (VPM) Receives input from the face from the trigeminal nucleus and projects to primary sensory cortex (postcentral gyrus) Fine touch and proprioception from face (principle sensory nucleus) Pain and temp (spinal trigeminal nucleus) Lateral geniculate nucleus visual Projects to primary visual cortex (upper and lower banks of the calcarene sulcus) Medial geniculate nucleus auditory Projects to auditory cortex of temporal lobe o Also receives input from inferior colliculus of midbrain via inferior brachium Review and describe the arterial blood supply to the thalamus o MCA and PCA send up perforating branches to regions of the thalamus Thalamic lesions & related functional deficits o The deficits are related to which nuclei is affected o Posterior lesion: sensory defects, abnormal sensation o Thalamic (Dejerine-Roussy) syndrome: thalamic stroke leads to innocuous stimulus perceived as very painful (allodynia) – severe contralateral pain. Can be worsened by emotional distress. o VA/VL lesion: motor disturbances due to connections with globus pallidus, cerebellum o Dorsomedial, Anterior lesions: disorders of consciousness, alterations in personality, decreased motivation, indifference to pain (less specific deficits) Lecture #25: limbic system Big picture: o Fornix: From hippocampus to hypothalamus, mammillary bodies and septal nuclei o Stria Terminalis (ST): from Amygdala to red nucleus, septal nuclei & nucleus accumbens o cingulum loop: fibers run around the cingulum into parahippocampal cortex then into hippocampus o Limbic structures handle both conscious and unconscious processes related to emotion, memory, and basic drives (hunger, thirst, sex, etc.) Clinically relevant points o *Note damage to hippocampus, fornix and mammillary bodies all cause memory loss o Korsakoff’s psychosis:Damage to mammillary bodies (hippocampus->fornix->MBs) and Dorsomedial nuclei of thalamus Chronic alcoholics Vitamin B1 defficiency Anterograde amnesia Inability to form new declarative memories Make up answers as they go along to conceal memory loss (confabulatory syndrome) o Kluver-Bucy: bilateral temporal lobe damage hypersexuality, absence of emotional reactions and fear Man with child porn after surgery for seizures Know the major limbic structures and functions described. o Cingulate gyrus Stimulation elicits: Autonomic responses Aggression if anterior cingulate involved Damage results in: o o o o Greatly diminished emotional responses and may result in problems remembering the order of events, or akinetic mutism (looks and acts like a coma but you aren’t) Subgenual (knee of the corpus collosum) cingulate Active during sadness Hyperactive in major depression Medial Prefrontal cortex Executive functions, working memory, planning, emotion regulation, foresight. Reciprocal inhibitory connections with the amygdala Amygdala can see with a coronal section through the uncus Associated with fear conditioning in animals Stimulation in humans generates predominantly negative emotions (sadness, fear and anxiety) but also some positive Links perception of objects with appropriate emotional responses, particularly in types of danger snowman video Sensory cortex and thalamus inform amygdala about the outside world Lesions= bilateral destruction memory deficit that impairs ability to learn/remember an appropriate emotional response; have difficulty recognizing fear or understanding the concept of fear They are not afraid and their body won’t react as if they are afraid Hypothalamus When stimulated in the lab: Medial hypo= panic attack sx in humans Lateral= predatory aggression in cats Dorsal-medial= stress response activated Mammillary bodies Receive majority of input from the hippocampus (memory area) through the fornix damage= impairs memory Hippocampus: HM and memory Bilateral removal= sever anterograde amnesia and some retrograde Amnesia only in declarative memories and not in learning new skills/procedures Involved in moving some types of memory from short to long-term storage Hippocampus is a curved sheet of cortex folded into the medial surface of the temporal lobe in three distinct zones: Dentate gyrus (looks like teeth) Hippocampus proper o Dentate gyrus and hipp prop look like 2 interlocking Cs Subiculum Alveus= hippocampal equivalent of subcortical white matter) Contains inputs and outputs to/from hippocampus Form a fiber bundle called the fimbria (“fringe”) of the hippocampus Fimbria in turn becomes the crus (“leg”) of the fornix Parahippocampal gyrus o Fornix: he leg of each fimbria joins at the midline to form the body of the fornix Travels out of the hippcampus, loops around, then heads anterior and dives down to form columns of fornix, heading to mammillary bodies, septal nuclei, and nucleus accumbens Damage to fonix causes impairment of spatial memory Receives projections from the hippocampus through the fornix and from the amygdala through the stria terminalis. Projects to the Ventral Tegmental Area (reward pathway). Also sends return projections to the hippocampus and amygdala o Septal nuclei: stimulation causes varying degrees of sexual arousal and compulsion to masturbate o Dorsomedial, anterior nuclei of the thalamus Hippocampus projects to anterior nucleus via the cingulum, Amygdala to Dorsomedial Nucleus via the Ventral Amygdalaofugal pathway Input-output relationships of limbic structures, focusing on amygdala, hippocampus o Amygdala Major nuclei: Central: Connected with hypothalamus, brainstem nuclei (e.g., PAG) o Emotional responses Basolateral: continuous with parahippocampal cortex, extensively connected with other cortical areas (prefrontal, insula, entorhinal, etc.) o motor response to fear based on learned associations Medial: Connected with olfactory system (bulb & cortex), relatively small in humans Inputs: Central: Visceral sensory inputs o Hypothalamus, septum,PAG, project to central nucleus Basolateral: sensory info from thalamus, visual, auditory, somatosensory, and gustatory project BL nucleus o Levels of physical/emotional comfort/discomfort in the anterior cingulate and insula project to basolateral nucleus Medial: Olfactory bulb & cortex project to medial nucleus through olfactory tract Major Inputs arrive via: o stria terminalis (from hypothalamus and septal nuclei to central nucleus) o ventral amygdalofugal pathway (from thalamus, anterior cingulate cortex to basolateral; from hypothalamus to central nucleus) o directly from temporal lobe cortex and hippocampus (to BL) (not pictured) o From the olfactory bulb to the central nucleus and medial nucleus Outputs: Fibers leave through Stria Terminalis and Ventralamygdalofugal pathway to reach many of the same areas Stria terminalis= connects amygdala to septal nuclei in the hypothalamus VAF= connects amygdala to septum, PAG, brainstem, DM thalamus, and substantia inomonata Amygdala connections to hypothalamus, brainstem initiate emotional responses such as fear and aggression Outputs to ventral striatum, modulate reward seeking, modulates reproductive drives. No time for romance when you are being chased by a bear Outputs to sensory cortical areas heighten awareness Outputs to PAG and spinal cord prime defensive reflexes o Hippocampus: Outputs: through fornix to the hypothalamus, mammilary body and septal nuclei Mainly arise in the subiculum or hipp proper and mainly project diretly back to entorhinal cortex/parahippocampal cortex (most anatomically prominent pathway is through the fornix) Near the interventricular foramen, some fibers branch off in front of the anterior commissure and are called the pre-commissural fornix, terminating in septal nuclei Remaining fibers (post-commissural fornix) terminate in, mammillary body, anterior thalamic nucleus, and hypothalamus Inputs (afferents): Primary source of afferents to hippocampus is entorhinal cortex (parahippocampal cortex) o EC receives some olfactory inputs, lots of association cortex inputs (posterior cingulate gyrus,orbital cortex, multimodal areas of frontal, parietal, temporal lobes) Modulatory cholinergic inputs from septal nuclei (S) reach hipp through fornix o Also direct inputs from amygdala Hippocampal commissure connects contralateral hippocampus to share info between one another Describe the components and flow of information in the Papez circuit o Hippocampus through fornix mammillary bodies (memory processing) ant nucleus of thalamus cingulate gyrus Lecture #26: Cerebellum Clinically relevant details Cerebellum has NO DIRECT connections to LMN’s indirect effect of LMN (higher center) Lesions of cerebellum, association cortex, and BG would be problems with coordination (ataxia) rather than weakness (as with problems in the motor cortices) Ataxia that you see will be ipsalateral to the side of the lesion (double cross) Midline lesions of the cerebellar vermis or flocculonodular lobes mainly cause unsteady gait (truncal ataxia) and eye movement abnormalities Lesions lateral to the cerebellar vermis mainly cause ataxia of the limbs (appendicular ataxia) Cerebellum receives inputs and error signals and the cerebellum can correct them based on the input it receives Primarily motor even though it receives a lot of sensory input as well Tests to determine cerebellar lesions: o Finger-nose test tests for intact cerebellum Can be done to determine if someone is drunk o Complex movements involves in speaking can also be affected: scanning speech (normal flow/rhythm disrupted; successive syllables emerge slowly, separated) o Rebound Phenomenon Patient, with eyes closed, told to move arm against resistance of examiner Examiner releases arm, forcefully “rebounds” toward patient (hypermetria) o Truncal Ataxia: Lesions confined to the cerebellar vermis affect primarily the medial motor systems. Patients with such lesions therefore often have a wide-based, unsteady “drunklike” gait o Appendicular ataxia: Lesions of the intermediate and lateral portions of the cerebellar hemisphere affect the lateral motor systems. Therefore, these patients have ataxia on movement of the extremities Vascular supply to cerebellum: o o AICA is where the peduncles are Major cerebellar anatomical regions, layers, excitatory vs. inhibitory parts of circuitry o Folia= folds in cerebellum (similar to gyri in cortex) o o o o o o 1. 2. Anterior lobe Posterior lobe Primary fissure= separates ant and post lobes (seen on mid-sagital cut) Flocculonodular lobe= shown in ventral view includes flocculus and nodular lobes Posterolateral fissure= separates Flocculonodular lobes Left hemisphere and Right hemisphere Lateral hemisphere= motor planning in extremities lat corticospinal tract Paravermis (intermediate hemispheres)= intermediate portion of the lateral hemisphere a. Distal limb corrdination lat CS and rubrospinal tracts 3. Vermis= midline structure that connects the two hemispheres o Middle, superior, and inferior peduncles= for the cortex to communicate with the cerebellum Cerebellar nuclei: Don’t Eat Greasy Food (lateral to medial) o Dentate nucleus (only one that you can see grossly) Receive projections from the lateral cerebellar hemispheres Active just before voluntary movements motor planning o Emboliform nucleus and Globose nucleus (connected functionally) Receives inputs from intermediate part of the lateral hemisphere Active during and in relation to that movement error correction system (a way to get better at a task) o Fastigial nucleus Receives inputs from the vermi Major inputs/outputs o Key points: Inputs arrive to cerebellar cortex (green, excitatory) Cerebellar cortex projects to deep cerebellar nuclei (red, inhibitory) Deep nuclei project to output targets (green, excitatory) o Cerebellar cortex: MPG (from outside to inside) Molecular layer Mostly composed of axons and dendrites Purkinje cell layer: only output from the cerebellar cortex Inhibitory in their projections: GABA They have intricate dendritic trees that branch out to the cortex Granule cell layer Each sends out a projection through the parallel fibers and can then project to the dendritic trees of the purkinje cells (transversely oriented) o Cerebellar cortex: Climbing fibers: associated ONLY with inferior olive in a question, CF are linked with inferior olive A single climbing fiber winds around the dendritic tree of each Purkinje cell making thousands of excitatory synapses Most powerful excitatory input in the nervous system CFs arise ONLY from contralateral inferior olivary nucleus Destruction of inferior olive has acute effects similar to destruction of the entire (contralateral) cerebellar hemisphere Mossy fibers: everything that doesn’t come from inf olivary nucleus will come in via mossy fibers o Mossy fibers terminate on dendrites of granule cells – less direct effect on Purkinje cells bc they reach out to granule cells first o Order to reach purkinje cells: Mossy fiber granule cell parallel fiber Purkinje cell All of the input into the purkinje fibers are excitatory (ignore GABA to purkinje) and all output carried by purkinje fibers to the efferent connections is inhibitory Cerebellar inputs: Pontocerebellar tract: Cerebral cortex (motor/premotor/ somatosensory cortex) projects to cerebellum via pontine nuclei Pontine nuclei receive inputs from ipsilateral cerebral cortex (orange), project to contralateral cerebellum through massive MCP Can see the middle cerebellar peduncles and pontocerebellar fibers in the mid pons section Gives the cortex some feedback as to what action it should perform next Spinocerebellar pathway (anterior and posterior) Particularly vulnerable to damage bc they travel on the lateral-most edge of the SC Post= inferior cerebellar peduncle Ant= superior cerebellar peduncle Lesion= Friedreich’s ataxia intention tremor from spinocerebellar tract problems o o Intention tremor= over and under-correcting movement and not direct movement finger-to-nose test Cerebellar outputs: Major output= superior cerebellar peduncle to the ventrolateral nuclei of thalamus (bc it has to go through this in the thalamus to go to the motor cortex) Dentate nucleus superior cerebellar peduncle at superior cerebellar peduncle decussation VL nucleus of thalamus primary motor cortex LMN in ventral horn of spinal cord Deficits would be ipsalateral bc inputs to the cortex and back down cross twice cerebellum to cortex crosses then cortex to SC (corticospinal) crosses again Involved in motor planning Cerebellum gives extra info so that we can generate better motor outputs Interposed nuclei (Emboliform and Globose nucleus) superior cerebellar peduncle VL nucleus of thalamus motor cortex Deals with error-correction (golf game) controlling ongoing movements of extremities Fastigial nucleus (don’t worry about details of pathway) goes to VL and cortex also eventually Proximal trunk movements and eye movements Bilateral projections allows for compensation with lesions Lecture #27: Cerebrum Lobes of the cerebral hemispheres and the functions of each o Frontal: voluntary motor and personality (Broca’s area) The frontal cortex is involved in “executive” function, i.e., the process of making decisions about how an individual will conduct themselves. Phineus Gage o Parietal: Postcentral Gyrus; tactile and proprioceptive inputs Inferior parietal lobule: language comprehension; Wernicke’s area Remainder of parietal cortex: spatial orientation, directing attention o Temporal: learning, memory, hearing (primary auditory cortex) In the 50’s; HM had progressively worse seizures; experimental (bilateral) removal of medial temporal lobe, including amygdala, most of hippocampus and parahippocampal gyrus Profound anterograde amnesia Unable to add new words to his vocabulary, remember people after 1953, or recall events after surgery Ability to keep track of his internal state was impaired (amygdala) After eating/drinking he remained hungry/thirsty o Occipital: visual info o Limbic: motivation, emotion, arousal, memory o Insular cortex: Involved in taste, emotion, consciousness, homeostatic regulation, perception, motor control, self-awareness, cognition, interpersonal experience Histological organization of the cortex (which cortical regions are characterized by particularly prominent cortical layers, e.g., layer V for motor cortex). o Small pyramidal neurons (layer III) have axons that terminate in the cortex. These form “association” fibers. o Layer IV is the granular layer – receives thalamic inputs, so this is the layer where large sensory tracts terminate (e.g., DCML/PCML, spinothalamic/anterolateral). o Large pyramidal neurons project out of the cortex. These form the fibers of, for example, corticobulbar and corticospinal tracts – layer V Type of information/BA Prefrontal association (46) Primary visual cortex (4) Primary motor cortex (17) Primary/largest layer Layer III Layer IV Layer V Main connections Cortical-cortical Inputs from thalamus Sends outputs to subcortical structures Know main Brodmann’s areas. o Brodmann’s areas are different based on what the section looks like histologically o Area 4 = primary motor cortex o Areas 1, 2, 3 = primary somatosensory cortex o Areas 41, 42 = primary auditory cortex o Area 17 = primary visual cortex hugging calcarene sulcus o Area 44, 45 (left hemisphere) = Broca’s speech and language area opercularis and triangularis near inferior frontal gyrus o Area 22 (left hemisphere) = Wernicke’s area posterior portion of superior temporal gyrus Somatotopic organization of the somatosensory cortex and primary motor cortex; cortical vascular supply. o Density of distribution of sensory receptors determines the representation in the somatosensory cortex Different types of receptors can give us an overall picture of our environment o Imaging of the brain for professionals and amateurs: more diverse and random for amateurs and more focal and practiced for professionals Basal ganglia location, vascular supply o BG considered part of the cerebrum: group of subcortical nuclei o Largest components include: caudate nucleus, putamen, globus pallidus (internum and externum) Caudate hugs the lateral ventricle From lateral to medial: putamen, globus pallidus, internal capsule, thalamus Ant limb of IC separates head of caudate from putamen Post limb of IC separates thalamus from putamen and globus pallidus o Exert indirect effects on motor control, e.g., via VA and VL thalamic nuclei, reticular formation of brainstem Important in facilitating appropriate motor actions, inhibiting unwanted movements Determines how much excitation the cortex will have by controlling motor output o Main categories of white matter fiber tracts that connect cortical areas. 1. U (arcuate) fibers: connect two adjacent gyri 2. Association fibers: span and connect several gyri Playing the piano would require many different inputs from many different areas shows the need for association fibers 3. Commissural fibers: travel to the opposite hemisphere, terminate in functionally related cortex Ant and post division Corpus collosum 4. Projections fibers: leave the cortex (e.g., corticospinal fibers) Internal capsule Corticobulbar (motor innervation to the face) pass through the genu Corticospinal and somatosensory fibers pass through the posterior limb Recognize the somatotopic organization of fibers traversing the internal capsule (above); vascular supply o MCA in particular dives out from the insula and provides supply (putamen and globus pallidus and a ton of cortex) o PCA and ACA (caudate) also play a role Vasculature MCA ACA Anterior choroidal PCA Areas impacted Putamen and globus pallidus and a ton of cortex (face representation in postcentral gyrus) Caudate and ant limb of IC Post limb and genu of IC thalamus Lecture #28: physiology of sleep Lesion would cause… Movements and body position (GP); sensory deficits in face, trunk, arm Cognition; sensory deficits in the leg Corticospinal and corticobulbar pathway deficits (motor weakness in extremities and face) Tons of deficits depending on nuclei effected Lecture #30: Motor pathways integration Know your lesions! Given a set of symptoms, be able to localize a lesion based on some process of elimination and associated symptoms. These give clues. Your patient is like a mystery you have to solve. Know whether you’d be ipsi/contra (whether the lesion is on the same side or opposite side of the body relative to the motor deficits observed). Know UMN (upper motor neuron) lesion signs versus LMN (lower motor neuron) lesion signs (slide 5) Sign weakness atrophy fasiculations reflexes tone UMN lesions: CP, TBI, stroke, MS, corticospinal tract injury YES No no Increased: hyperreflexia Increased: hypertonia LMN lesions: poliomyelitis, lesions near spinal cord YES Yes Yes Decreased: hyporeflexia Decreased: flaccid Know where corticobulbar and corticospinal tracts are running within the internal capsule. o Corticobulbar (facial motor)= genu o Corticospinal= post limb Know the vasculature that would be associated with a given lesion. o Anterior choroidal artery post limb and genu of IC corticospinal affected Is the lesion a vascular event or a tumor? (fast, acute onset vs. slow, gradually worsening) Know the terminology of slide 27/28. Also, do NOT memorize slide 8. o Plegia= total paralysis quadri= all 4 limbs, para= both legs or both arms, hemi= one side o Paresis= motor weakness quadri, para, hemi o Thrombosis= occlusion of vessels o Infarction= area of tissue undergoing necrosis due to restricted blood and O2 o Hemorrhage= bleeding into nervous tissue o Acute event vascular o Tumor chronic o Relapsing and remitting something like MS (can show up in a different part of the body) For the descending lateral and medial pathways, still know the main function for each and where each would be located in a C7 cross-section of the spinal cord (i.e., if given a lesion, what would be impacted). o Lateral systems: descending pathways descend contralaterally deficits tend to show marked deficits on one side Lateral corticospinal: pre-central gyrus post limb of IC through cerebral peduncle through basal pons through pyramid pyramidal decussation at the spinomedullary junction descends through lat corticospinal tract synapses in ventral horn of SC Rubrospinal: tone over flexor muscles red nucleus (this is the origin bc there are several inputs coming into the red nucleus to create this descending pathway) crosses immediately at o ventral tegmental decussation in midbrain travels through rubrospinal tract LMN in ventral horn Medial systems: mainly descend ipsalaterally or bilaterally less obvious defects when lesioned bc they have bilateral projections Ant corticospinal: trunk muscles Motor cortex ant CS tract terminates bilaterally at the level of the effector Vestibulospinal: postural adjustments; positioning of head and neck Balance: Lateral vestibular nucleus in pons descends ipsalaterally Travels through ventral part of lateral funiculus excitatory projections to ventral horn of entire spinal cord Position of head and neck: medial V nucleus in the medulla descends bilaterally Bilateral projections to cervical, upper thoracic spinal cord (head and neck) Reticulospinal: Posture, gait-related movements Reticular formation at pons (medial) or medulla (lateral) ipsilaterally through reticulospinal tract Terminates in ventral horn Tectospinal: orient head and eyes to (only contralateral medial system!) Superior colliculus crosses immediately through the dorsal tegmental decussation, in midbrain tectospinal tract ventral horn Lecture #31: Sensory pathways integration Know these pathways: o PCML pathway: proprioception and discriminative touch DRG dorsal horn travels up medial gracile (LE) or lateral cuneate (UE) decussates at internal arcuate fibers in medulla becomes the medial lemniscus pathway and travels through pons and midbrain thalamus (VPL) postcentral gyrus in parietal lobe (medial for LE and lateral for UE) o Anterior and lateral spinothalamic tracts: Ant= pressure and crude touch Lat= pain and temp DRG ventral horn decussated immediately through ventral white commissure and joins contralateral spinothalamic tract VPL of thalamus postcentral gyrus o Trigeminothalamic pathway: sensory info from face CN 5 fine touch and proprioception enters via principle sensory nucleus at mid-pons decussate and travel to VPM in the thalamus Spinal trigeminal nucleus at caudal pons brings in pain and temp from face VPM in thalamus o Spinocerebellar (ant and lat): unconscious proprioception lesions= ataxia Ant= decussate immediately LE info ascends contralaterally to enter cerebellum through sup cerebellar peduncle Post= synapse in Clark’s nucleus ascend ipsalaterally and enter cerebellum through inf cerebellar peduncle Lecture #29: higher cortical function Functions (and the effects of lesions to) primary motor, supplementary motor, premotor areas, frontal eye fields Corticospinal pathway, and UMN vs. LMN damage Know Brodmann’s areas for visual, auditory, somatic sensory, motor, and speech areas Recognize the cortical areas important for language. Compare and contrast Broca’s, Wernicke’s, conduction, and global aphasias, etc., and know the vascular lesion likely to produce each deficit. Recall the cortical area important for spatial relations, and hemispatial neglect (hemineglect). Identify the functions of the prefrontal association cortex. Any other clinically relevant details (e.g., prosopagnosia) Compare the major differences in hemispheric function in humans