* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Neurotoxicity
Activity-dependent plasticity wikipedia , lookup
Blood–brain barrier wikipedia , lookup
Nonsynaptic plasticity wikipedia , lookup
Holonomic brain theory wikipedia , lookup
Central pattern generator wikipedia , lookup
Cognitive neuroscience wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Electrophysiology wikipedia , lookup
Neural engineering wikipedia , lookup
Biological neuron model wikipedia , lookup
Signal transduction wikipedia , lookup
Aging brain wikipedia , lookup
Single-unit recording wikipedia , lookup
Biochemistry of Alzheimer's disease wikipedia , lookup
Metastability in the brain wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Development of the nervous system wikipedia , lookup
Optogenetics wikipedia , lookup
Synaptic gating wikipedia , lookup
Haemodynamic response wikipedia , lookup
Neuromuscular junction wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Axon guidance wikipedia , lookup
Node of Ranvier wikipedia , lookup
End-plate potential wikipedia , lookup
Channelrhodopsin wikipedia , lookup
Nervous system network models wikipedia , lookup
Synaptogenesis wikipedia , lookup
Neurotransmitter wikipedia , lookup
Circumventricular organs wikipedia , lookup
Neuroregeneration wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Neuroanatomy wikipedia , lookup
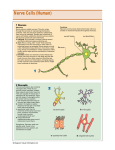
NERVOUS SYSTEM TOXICOLOGY DR. BASMA DAMIRI 173020 OUTLINE • Nervous system anatomy and physiology • Ways in which neurotoxic chemicals may impair nervous system function • Target of toxicity, Manifestations of neurotoxicity • • • • • Membrane Neuronopathies Axonopathies Myelinopathies Neurotransmission-associated anomalities • Prototypical toxicological agents • Methylmercury • Carbon disulfide • Lead • Nicotine • Organochlorine insectides • Organophosphorous insectides • Venoms Suggested Questions: 1. What are the chemicals that act on the neuron and cause disruption for it? 2. What are peripheral neurotoxicants and how do they affect neurons? 3. Describe in details the function of blood brain barrier in brain toxicity? 4. What is the relationship between the nervous system and the respiratory system (rule of anoxia in neurotoxicity)? 5. What is the site effect of nicotine on the nervous system (neurotoxicity)? NERVOUS SYSTEM ANATOMY NERVOUS SYSTEM ANATOMY Nerve cell (neuron): functional unit • Cell Body: makes proteins for all parts of neurone with central nucleus • Axons: long projections along which nerve impulses travel rapidly • Myelin sheath: fatty substance that insulates the axons and speeds up conduction • Post-synaptic membrane: nerve or muscle cell Nervous system as a target organ Structural damage to neuron • Lead – damages myelin sheath slowing nerve impulse transmissions • Mild symptoms – tiredness • Severe cases – peripheral neuropathy producing muscle weakness, often showing as ‘wrist drop’ or ‘foot drop’ • n-Hexane – causes swelling of axon and degeneration of axon and myelin sheath • Symptoms include muscular weakness and sensory motor loss particularly to hands and feet Nervous system as a target organ • Structural damage to neuron • Manganese – damages axon • Symptoms resemble Parkinson’s disease with tremor and difficulty in walking and speaking • Mercury – damages the sensory nerves • Symptoms include hearing, speech and vision problems. Also tremors and shaking and psychiatric disturbances • Organo-metallics (e.g. methyl mercury and tetra ethyl lead) – can readily reach the brain • Symptoms include irritability, memory loss, convulsions and psychiatric disturbances Nervous system as a target organ • Functional damage to nerve • Organic solvents – act as CNS depressants • High affinity for lipid rich tissues (e.g. myelin sheath) and absorb into it causing swelling and impairing nerve impulse transmission • Acute narcotic and anaesthetic effects: drowsiness, loss of feeling, unconsciousness, death • Chronic effects: possible long-term damage to neurons Nervous system as a target organ • Functional damage to nerve pesticides – depolarisation of axon is prolonged • Organo-chlorine polarisation and • Symptoms include tremors caused by nerves becoming hyper- excitable • Organo-phosphorous pesticides – interfere with chemical transmission across the synapse • Acetylcholine not hydrolysed by target cell enzymes leading to reactivation of target cell • Symptoms include excessive muscle contractions, convulsions and paralysis Response to neurotoxicants includes changes in: • Heart rate. • Sensory perception • Coordination • Mood and many other physiological, behavioral, cognitive, and emotional effect. Ways in which neurotoxic chemicals may impair nervous system function: 1. Permanent damage since neurons do not usually regenerate. 2. May disrupt the electrical impulse along the axon, either by harming the myelin sheath or membrane integrity or by impairing the synthesis function of proteins essential to axonal transport. 3. Chemicals may also inhibit the neurotransmitters by blocking their synthesis release or binding the receptors. 4. General protein synthesis impairment may have an effect not only on the neurotransmitters production, but also the production of important enzymes which break down neurotransmitters when they are no longer needed. The anatomical and physiological features that makes an axon a particular target for toxicants 1. Blood Brain Barrier a. Tight junctions of capillaries. b. Oligodendrites-glial as a 2nd layer. c. Astrocytes. d. The chemical to go there has to be a lipophilic or resemble a neurotransmitter. e. Site of toxicity –Circumventricular organs- spinal and autonomic ganglia. Less restrictive areas. NERVOUS SYSTEM ANATOMY BLOOD BRAIN BARRIER Blood Brain barrier • Selective barrier which protects most of brain against water soluble toxins • but permeable to lipid soluble toxins (e.g. organometals, solvents) • Matures 6 months after birth (consequence?) Most tissues Blood brain barrier 2- Importance of energy requirements of the brain: • High energy requirements the brain utilizes aerobic glycolysis and, therefore, it is extremely sensitive to even brief interruptions in the supply of oxygen ore glucose • anything inhibits aerobic respiration as cyanide or produces hypoxia such as CO will affect the brain and leads to the early signs of dysfunction in the myocardium and neurons. • Anoxia: the relationship between the nervous system and the respiratory system. • The high metabolic rate of neurons requires that they be well supplied with oxygen and a rapid waste transport system. • Damage to the NS under these conditions is a combination of direct toxic effects on neurons and secondary damage from systemic hypoxia or ischemia. Examples of sensitivity of neurons to energy depletion. • CO- may severely reduce the O2 supply to neurons and eventually causes their death by anoxia. Acute CO poisoning damage those structures in the CNS that are most vulnerable to hypoxia (e.g. the neurons in specific regions of basal ganglia and hippocampus, certain layers of the cerebral cortex, and the cerebellar Purkinje cells). CO may also produce white matter damage. Systemic hypotension is the best predictor of these lesions following CO poisoning. • H2S and Cn can irreversibly bind to cytochrome oxidase, an essential component of the respiratory electron transport chain, can affect autonomic nerves such as those controlling breathing and heart rate which lead to death. • 3-Nitropopronic acid (3-NP) naturally occurring mycotoxin irreversible inhibitor of succinate dehydrogenase that produces ATP depletion in cerebral cortical explants and associated wit motor disorders in livestock and humans that have ingested contaminated food. 3-Obstacle of the space: the longer the axon, the more likely to hit more places. a. b. Neuropathy: When the neuronal cells body has lethally injured, it degenerates, in a process called neuropathy no potential of regeneration Axonopathy: When the injury is on the level of the axon, it may degenerate while the neuronal cell continuous to survive Band of Bungner: if any part of the axon is damaged, another elongation or repair could occur. 4. Maintenance of an environment rich in lipids: Lipids wrap around the axon (myelin sheath, Schwan cells)- Exclude water-ions from the area-They have particular lipids different than other cells- there are certain toxicants that target these lipids. 5. Transmission of information across extracellular spaces –Synapse. MANIFESTATIONS OF NEUROTOXICITY MANIFESTATIONS OF NEUROTOXICITY • Motor • Sensory • Autonomic • Cognitive capabilities Mechanism of neurotoxicity Neuropathy Neuropathy Ethanol and methanol Pb Mn • The initial injury to neurons is followed by apoptosis is or necrosis leasing to permanent loss of the neurons: Al As Bismuth 6-amino nicotinamide inhibition of NADPH CO CCl4 Chloramphenicol CN Hg organic and inorganic Methyl bromide MPTP 3-NP Phenytoin Quinine Streptomycin Thallium Trimethyltin: plasticizer, antifungal agent, or pesticide. can cause hearing loss • The onset of neurotoxic problem may follow toxic exposure for many years. • The relationship between MPTP intoxication and Parkinsonism has stimulated investigations into the role that environmental and occupational exposure may play in the pathogenesis of Parkinson’s disease. • Herbicides , pesticides, metals risk factors • Dithiocarbamate paly important role • Alzheimer’s disease Al MANIFESTATIONS OF NEUROTOXICITY NEURONOPATHIES • Doxorubicin (adriamycin) A quinone-containing anthracycline antibiotic, is one of the most effective antimitotics in cancer chemotherapy. • Clinical application is limited by acute and chronic cardiotoxicity, injury to PNS. • It can intercalate into grooves of DNA preventing transcription • If the blood-brain barrier is temporarily opened by the use of mannitol, toxicity of Doxorubicin is ↑↑↑ • With injury in the neurons in the cortex and subcortical nuclei of the brain MERCURY • Vapor from degassing in earth’s crust • Methylated by microorganisms to CH3Hg • CH3Hg is most significant form of Hg in terms of toxicity from environmental exposure • Bioconcentration in aquatic food chain • 90 to 95% absorption in GIT • Crosses placenta MERCURY METHYL MERCURY • Neurotoxic effects lead to, • Paresthesia • Ataxia • Neurasthenia • Vision and hearing loss • Coma and death • Neurotoxic effects due to focal necrosis of neurons MERCURY METHYL MERCURY • The critical or lowest level of observed adverse health effect in adults is paresthesia • The average long-term intake associated with paresthesia calculated to be 300 μg/day for an adult • Poisoning therapy utilizes chelators such as cysteine, penicillamine, thiol resins • It is estimated that 3-4 million children live within a mile of at least one of the 13000+ active hazardous waste sites in USA. • Clinical picture of Methg poisoning varies both with severity of exposure and the age of individual at the time of exposure. • In adults, the most dramatic sites of injury are the neurons of cereberall cortex whose massive degeneration results in blindness and marked ataxia. • In children, developmental disabilities, retardation, and cognitive deficits occur. LEAD • Ubiquitous toxic metal • Primary route of exposure is by ingestion • Source is from lead-based paint, contaminated drinking water, lead-glazed pottery • Encephalopathy occurs at blood lead levels of 80-100 μg/dL LEAD • Symptoms of encephalopathy include lethargy, vomiting, irritability, loss of appetite, and dizziness • Progression of symptoms lead to ataxia, reduced level of consciousness, which may progress to coma and death • Recovery is often associated with life-long epilepsy, mental retardation, optic neuropathy, blindness LEAD • Chronic toxicity affects PNS; Schwann cell degeneration • Mechanisms of toxicity include, • Impairment of cell-cell connections • Alterations in neurotransmitter levels • Disrupts calcium metabolism Metaphyseal lead lines Basophilic Stippling • MPTP- a contaminant of synthetic heroin. Resemble dopamine and acts as mitochondrial toxicant- high lipid peroxidation- high ROS- release dopamine from the vesicles MANIFESTATIONS OF NEUROTOXICITY Membrane: • Chemicals that disrupt the membrane system can seriously impair nervous system function. • Solvents or cleaning agents like methanol, trichloroethylene, tetrachloroethylene. They are lipophilic and volatile MANIFESTATIONS OF NEUROTOXICITY AXONOPATHIES: dying –back neuropathy • The primary site of toxicity is the axon itself. Microtubules are usually the target. • Degeneration of axon, surrounding myelin, but cell body remains intact • Irreversible in CNS, but reversible in PNS • Caused by CS2, acrylamide, gold, organophosphorous esters, chlordecone (Kepone), Dapsone, Li, metronidazole, platinium, CS2 • CS2: the most significant exposures of humans to CS2 have • • • • • occurred in the vulcan rubber and viscose rayon industry distal axinopathy like n-hexane Used in the production of viscose rayon, cellophane, pesticides, as a solubilizer for waxes and oils Exposure is predominantly occupational Direct interaction with free amine and sulfhydryl groups Microsomal activation to reactive sulfur intermediates that bind macromolecules Produce neuronal degeneration in CNS; in PNS produce myelin swelling and fragmentation MANIFESTATIONS OF NEUROTOXICITY AXONOPATHIES Gamma- Diketones n-hexane Methyl n-butyl ketone • Sensorimotor polyneuropathy • Sensory numbness and paresthesia • Distal nerves affected first (distal axon swelling in both motor or sensory neurons) • Clinical signs often delayed for 6-12+ months • Axonal swelling and secondary demyelination • 2,5-hexanedione is common toxic metabolite • Gamma- Diketones react with amino groups on all proteins forming pyrolle adducts, an important step in developing axonopathy. • Pyrolles are oxidized and cross-linking occurs between microfilaments subunits. • Neurofilaments accumulate in the distal axon, usually just proximal to node of Rnvier, and forma massive axonal swellings leading to reactions of myelin from the nodes. Acrylamide • Vinyl monomer used widely in water purification, paper • • • • • manufacturing, mining, and waterproofing. It presents in many foods prepared at high temperatures. PNS Distal axonopathy multiple axonal swellings Large single dose or multiple smaller doses Repeated dosing results in more proximal axonopathy “dying back” process. MANIFESTATIONS OF NEUROTOXICITY MYELINOPATHIES • Attack myelen sheath or Schwan cells and oligodendritis • Metals such as lead, thallium, and triethyltin can be inhaled. • Decreases the ability of conduction, slow down impulses. • Increases the susceptibility to other damage. • Thallium: causes vision loss • Lead: impaired cognition MYELINOPATHIES • Intramyelinic edema • Demyelination • Remyelination in CNS occurs to a limited extent • Remyelination in PNS done by Schwann cells • Caused by amiodarone, disulfiram,Pb MANIFESTATIONS OF NEUROTOXICITY NEUROTRANSMISSION-ASSOCIATED ANOMALITIES • Interruption of impulse transmission • Blockade of transsynaptic communication • Inhibition of neurotransmitter uptake • Interference with second-messenger systems Nicotine bind cholinergic receptor amphetamines, methamphetamine alteration of dopaminergic, serotonergic, and cholinergic systems Cocaine infarcts and hemorrhage Atropine acts as adrenergic receptors, blocks cholinergic receptors Muscarine (mushroom) binds muscarinic receptor (cholinergic ) NICOTINE • Exposure from smoking • Binds to nicotinic cholinergic receptors (low-dose) stimulation; high-dose blocking • Increase in HR • Elevated BP • Acute overdose leads to excessive stimulation of nicotinic receptors leading to ganglionic paralysis Neurotransmission associated toxicity • Two main mechanisms of action: 1. Binds to receptors or channels such as organo- chlorine Insecticides. 2. Binds to enzymes and prevents the breakdown of neurotransmitters such as organo phosphorous insecticides ( OP) Parathion and carbamate. Toxicants that bind to receptors or channels: 1. DDT: Organochlorine insecticides 2. Cyclodienes: such as Chlordane, Kepone, Mirex, endosulfan 3. Nicotine binds to acetylcholine receptor (Ach) 4. Ethanol ORGANOCHLORINE INSECTICIDES • DDT, lindane, dieldrin • High lipid solubility, low degradation rate • Persistence in environment, bioconcentration and biomagnification in food chains • Produce disturbances in ion transport across axon leading to increased excitability and seizures 1- DDT cause tremors and seizure and increase sensitivity to stimuli 1. Binds Na-ATPase act as a neurotransmitter. 2. Binds Ca-ATPase, Ca is essential for diffusion of neurotransmitters to membrane. Inhibits Ca – modulin. Death occurs because of the continuous contraction in human diaphragm- no breathing. 3. Inhibits norepinephrine function and manganese which inhibits serotonin, norepinephrine, and dopamine function 2. Cyclodienes: such as Chlordane, Kepone, Mirex, endosulfan – act as antagonist for gama amino butyric acid (GABA), a neurotransmitter. 3. Nicotine binds to acetylcholine receptor (Ach), nicotinic receptors cause nicotine poisoning such as excitability, nausea, and increased heart rate followed by muscle relaxation, decreased heart rate, and sometimes coma and death. 4. Ethanol: impairs axonal signal transmission by disrupting the Na, and K channels. Neurotransmission associated toxicity • Two main mechanisms of action: 1. Binds to receptors or channels such as organo- chlorine Insecticides. 2. Binds to enzymes and prevents the breakdown of neurotransmitters such as organo phosphorous insecticides ( OP) Parathion and carbamate. Toxicants that bind to neurotransmitter enzymes and prevent breakdown of neurotransmitters • Anticholinesterase insecticides • Organ phosphorous insecticide (OPs). • Carbamate OPS : chemical intermediate, flame retardants, fuel additives, hydrolytic fluid, lubricants, pharmaceutical, plasticizers. Pesticide and nerve agents • Symptoms of carbamate toxicity similar to those of OPs but of shorter duration or milder severity. Pesticide Aging • we are removing the acetyl group –after choline is removed away, two alkyl groups are left on P. If one alkyl group was cleaved, the second group will be hydrolyzed so slow (few days). No possibility of second hydrolysis because of dealkylation. We have to regenerate the enzyme. • Second hydrolysis is very slow and takes days. The body will remake the enzymes than to hydrolyze it. • Aging will occur with ethyl (least likely to age), propyl or butyl (more likely to age). OPIDN - Organophosphate Induced Delayed Neuropathy Some of OP compounds, such as tri-o-cresyl phosphate (TOCP) are neuropathic and can cause a sever sensorimotor central peripheral distal axonopathy called OPIDN without inducing cholinergic toxicity called also delayed neuropathy or delayed polyneuropathy (OPIDP) USA contaminated alcohol, Morocco contaminated olive oil • Clinical signs • Ataxia and paralysis • Develop 10 to 14 days after exposure • Neuropathology • Wallerian-type degeneration • Mode of Action • Inhibition of neurotoxic esterase (NTE) is generally predictive Clinical signs related to excessive stimulation of nicotinic and muscarinic receptors 1. 2. 3. 4. 5. 6. 7. 8. 9. Muscle tremors CNS effects Respiratory paralysis (this is what causes death) Salivation, Lacrimation, Urination, and Defecation CNS signs Bronchospasm Bronchial secretions Miosis Bradycardia OPIDN - Organophosphate Induced Delayed Neuropathy • Clinical signs • Ataxia and paralysis • Develop 10 to 14 days after exposure • Neuropathology • Wallerian-type degeneration • Mode of Action • Inhibition of neurotoxic esterase (NTE) is generally predictive Chemical Treatment: • 1. Atropine – NEVER give 2-PAM as hydrolysis occur. • Hydrolysis: • Acetylcholine> atropine> carbamate • 1 sec > min to hrs • OP hydrolysis never occurs ORGANOPHOSPHOROUS PESTICIDES • Malathion, parathion, “nerve gases” • Inhibits acetylcholinesterase (AChE) leading to continuous stimulation • Neurobehavioral, cognitive, neuromuscular disturbances • Intermediate syndrome • Death from respiratory distress VENOMS ARACHNIDA • Scorpions, spiders • Contain low molecular weight proteins that affect ion transport along axon • Impairs action potential • Symptoms include tachycardia, respiratory distress