* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PNS Terminology
Metastability in the brain wikipedia , lookup
Activity-dependent plasticity wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Single-unit recording wikipedia , lookup
Neural coding wikipedia , lookup
Biological neuron model wikipedia , lookup
Mirror neuron wikipedia , lookup
Neurotransmitter wikipedia , lookup
End-plate potential wikipedia , lookup
Proprioception wikipedia , lookup
Axon guidance wikipedia , lookup
Optogenetics wikipedia , lookup
Neuroregeneration wikipedia , lookup
Embodied language processing wikipedia , lookup
Caridoid escape reaction wikipedia , lookup
Development of the nervous system wikipedia , lookup
Channelrhodopsin wikipedia , lookup
Microneurography wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Circumventricular organs wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Nervous system network models wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Central pattern generator wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Synaptic gating wikipedia , lookup
Synaptogenesis wikipedia , lookup
Neuroanatomy wikipedia , lookup
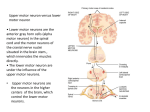
Divisions of the nervous system CNS PNS EFFERENT Somatic Skeletal muscle -voluntary ANS Cardiac & smooth muscles Glands -involuntary AFFERENT Somatic Visceral Cardiac & Skeletal muscle, tendons smooth muscles Glands joints PNS Terminology • Ganglia – neuron cell bodies • Peripheral nerves – neuronal axons • PNS neuroglia – Satellite cells • Enclose neuron cell bodies in ganglia – Schwann cells • Cover peripheral axons Efferent Division of the PNS • the somatic nervous system and part of the autonomic nervous system • the somatic – control of skeletal muscle • the ANS – involuntary control over cardiac and smooth muscle + gland secretion I - Olfactory II - Optic III - Oculomotor IV-Trochlear V - Trigeminal VI - Abducens VII - Facial VIII - Acoustic IX - Glossopharyngeal X - Vagus XI - Accessory XII - Hypoglossal -cranial nerves – 12 pairs -considered part of the peripheral nervous system (PNS) -olfactory & optic contain only sensory axons = sensory nerves -remaining are motor or mixed nerves (both motor and sensory axons) Spinal Nerve •after passing through intervertebral foramina the spinal nerve branches = ramus/rami •Dorsal ramus Sensory/motor innervation to skin and muscles of back •Ventral ramus -Ventrolateral body surface, body wall structures, muscles of the upper and lower limbs •in addition to these rami - the spinal nerves also give off a meningeal branch reenters the vertebral canal and supplies the vertebrae, vertebral ligaments and meninges • rami communicantes = branches from the spinal nerve -defined as a connection between a spinal nerve and the sympathetic trunk of the ANS -two types: 1. gray rami communicantes – unmyelinated post-ganglionic axons 2. white rami communicantes – myelinated preganglionic axons sympathetic trunk Somatic Nervous System • considered the voluntary aspect of the PNS – but the muscles of posture and balance are controlled involuntarily by the lower brain centers (brain stem, cerebellum) • cell bodies located in the ventral gray horn of the spinal cord • the axon of a motor neuron extends from the CNS continuously to its skeletal muscle target – ANS usually requires two neurons • terminals release acetylcholine – contraction • can only stimulate its target – whereas the ANS can either stimulate or inhibit its target Somatic Nervous System - somatic/motor commands emerge from the ventral horn and travel through the: – dorsal ramus to target the muscles of the back – ventral ramus to target the muscles of the limps and body wall Somatic Nervous System • motor neurons receive incoming information from many converging presynaptic neurons – both excitatory and inhibitory on these motor neurons – some information are part of reflexes originating in the spinal cord – other information can come in from areas of the brain via the descending white matter tracts • motor areas of the cerebral cortex, the basal nuclei and the cerebellum – synapse with the motor neurons in the ventral horn and regulate their activity • activation – impulse sent to muscles • inhibition – no impulse, no contraction • level of activity of a motor neuron is the balance between the EPSPs/activation and the IPSPs/inhibition of the incoming synapsing neurons • therefore motor neurons are considered the final common pathway – considered the only way any other part of the nervous system can influence muscle activity Somatic Motor pathways • all excitatory and inhibitory signals that control movement converge on the motor neurons that extend from the brain stem and SC to innervate the skeletal muscles – called lower motor neurons (LMNs) – have their cell bodies in the brain stem and SC (anterior gray horn) – their axons extend through the cranial and spinal nerves to skeletal muscle – only LMNs provide output from the CNS to skeletal muscle fibers = final common pathway – damage to the LMNs produces flaccid paralysis on the same side as the damage – loss of reflex action, motor tone and voluntary contraction • neurons in four distinct circuits control movement by providing input to these LMNs – – – – 1. local circuit neurons 2. upper motor neurons (UMNs) 3. basal ganglial neurons 4. cerebellar neurons • • Somatic Motor pathways 1. local circuit – input arrives at LMNs from nearby interneurons called local circuit neurons – receive input from somatic sensory receptors and higher centers of the brain – help coordinate rhythmic activities in muscle groups 2. UMNs – Interneurons that provide input to the local circuit and LMNs – essential for planning, initiating and directing sequences of voluntary movements – extend from the brain to the LMNs via two types of somatic motor pathways • 1. direct motor pathways: nerve impulses for precise voluntary movement – lateral corticospinal, anterior corticospinal and corticobulbar – cell bodies are located in motor cortex and travel down the spinal cord (corticospinal tracts) or through the brain stem (corticobulbar) – about 90% decussate within the medulla oblongata (lateral corticospinal) • 2. indirect motor pathways: or extrapyramidal pathways – nerve impulses follow complicated circuits that involve the cortex, basal ganglia, thalamus and brain stem Somatic Motor pathways • 3. Basal ganglia – assist movement by providing input to the UMNs – also suppresses unwanted movements by inhibiting thalmic activity – the production of dopamine by the substantia nigra also effects muscle tone – major pathway (cortex – basal ganglia – thalamus – cortex – UMN LMN) • Globus pallidus and substantia nigra involved • this circuit may function in initiating and terminating movements • caudate nucleus and putamen receive imput from sensory, association and motor areas of the cortex and from the substantia nigra – UMNs of this pathway form the reticulospinal, rubrospinal and vestibulospinal tracts • 4. Cerebellar – function involves four activities • 1. monitoring intentions for movement • 2. monitoring actual movement • 3. comparing the command (intention and movement) with sensory information • 4. provides correction – to UMNs – travels via the thalamus to the UMNs in the cerebral cortex – or can go directly to the UMNs that originate in the brain stem Medical application: Lou Gehrig’s Disease -Amyotrophic lateral sclerosis: Lou Gehrig’s disease -unknown cause -attacks motor areas of the cortex, axons of motor neurons in the spinal cord and motor neuron cell bodies -muscle weakness and atrophy -begins in regions of the SC that affect hands and arms and then spreads -specific destruction of the axons of UMNs in the corticospinal (direct UMN) and rubrospinal (indirect UMN) tracts plus the cell bodies of LMNs -about 15% of cases are inherited = familial ALS -non-inherited cases have implicating factors -buildup in the synaptic cleft of the NT glutamate – released by motor neurons because the gene controlling the recycling of this NT is mutated -excess glutamate causes motor neuron malfunction and death -drug – riluzole – may help by reducing damage to these neurons by decreasing glutamate concentration -also roles for free radicals, autoimmune, viral infections??? The Neuromuscular Junction • end of neuron (synaptic terminal or axon bulb) in very close association with a muscle fiber/cell • distance between the bulb and the folded sarcolemma = synaptic cleft • nerve impulse leads to release of neurotransmitter (acetylcholine) •this release will result in activation of the muscle cell and contraction •therefore the NMJ is ALWAYS excitatory •the only way inhibition can take place is through the inhibition of the neuron “connecting” with the muscle http://www.blackwellpublishing.com/matthews/neurotrans.html Medical Application • black widow – – – – • botulism – – – • triggers an explosive release of ACh also at other sites other than the NMJ (i.e. neurons that release ACh = cholinergic neurons) prolonged depolarization of target paralysis of the diaphragm – respiratory failure blocks release of ACh from the neuron at the NMJ from Clostridium botulinum bacteria – toxin death due to respiratory failure curare – – reversibly binds to the muscle cell but doesn’t trigger the opening of Na channels – no contraction • • ACh antagonist myasthenia gravis – – – – – – – disease of the NMJ - autoimmune extreme muscle weakness antibodies are produced against the AcH receptors at the NMJ (sodium channel) so AcH cannot bind to the muscle cell and trigger a contraction as a result Acetylcholinesterase destroys the released AcH before it has a chance to interact at the NMJ treatment – neostigmine – AchE inhibitor this temporarily increasing the chance ACh can find and bind its receptor at the NMJ – Na influx etc….. contraction Motor Units • • • • • Each skeletal fiber has only ONE NMJ MU = Somatic neuron + all the skeletal muscle fibers it innervates Number and size indicate precision of muscle control Muscle twitch – Single momentary contraction – Response to a single stimulus All-or-none theory – Either contracts completely or not at all • Motor units in a whole muscle fire asynchronously some fibers are active others are relaxed delays muscle fatigue so contraction can be sustained • Muscle fibers of different motor units are intermingled so that net distribution of force applied to the tendon remains constant even when individual muscle groups cycle between contraction and relaxation. ANS • involuntary motor commands and sensory information • supplies cardiac and smooth muscle, glands (i.e. viscera) • comprised of two neurons – preganglionic and postganglionic – preganglionic synapses with the cell body of the postganglionic within the ganglion • therefore the collection of their cell bodies forms the ganglion itself!!! – the pregang and postgang neurotransmitters can differ – the postganglionic neuron is unmyelinated ANS • two divisions that innervate the same organs • efferent branch regulates “visceral” activities (motor commands, involuntary, organs) • also has an afferent branch that receives sensory information from these areas – called the visceral division of the CNS Parasympathetic Division • cell bodies of the preG neurons are located in the four cranial nerves III, VII, IX and X (brain stem) and in the lateral gray horns of the sacral spinal nerves 2 through 4 • emerge as part of the cranial or spinal nerve • parasympathetic ganglia: called terminal ganglia – located close to the wall of a visceral organ – the preG fibers are very long because they must extend from the CNS to an organ – synapse with postG within the terminal ganglia – four major TGs – located close to the organ they innervate • otic, submandibular, pterygopalatine, ciliary • • • • • cell bodies of the preG neurons are located in the lateral gray horns of T1 to L2 sympathetic ganglia – site of the synapse between the preG and postG neurons – two groups: 1. sympathetic trunk ganglia: -vertical row lateral to the vertebral column -short preG lead into these ganglia -3 cervical, 11 or 12 thoracic, 4 or 5 lumbar and 4 or 5 sacral -3 cervical have specific names (superior, middle, inferior) 2. prevertebral ganglia: -close to the large abdominal arteries -postG neurons innervate the abdominal organs -three major prevertebral ganglia: celiac, superior mesenteric and inferior mesenteric axons exit the lateral gray horn through the ventral (anterior) root of the thoracic spinal nerve along with somatic motor nerve axons and parasympathetic preG axons form part of the spinal nerve they then enter a white rami communicantes and pass to the nearest sympathetic trunk ganglion– visceral motor Sympathetic Division celiac ganglion *** whether it is sympathetic or parasympathetic – the preG neurons release AcH Sympathetic Dominance • fight or flight • protective response • elevated heart rate, blood pressure, respiration rate • increase blood flow to skeletal muscles, lungs, heart, brain • decrease blood flow to digestive, reproductive and urinary organs Parasympathetic Dominance • “rest and digest” response • dominates in quiet, stress-free situations • resets the system after sympathetic stimulation – e.g. slow the heart rate and lower blood pressure ANS Neurotransmitters • specific neurons release specific NTs – have distinct names • cholinergic neurons and AcH – include all preG neurons from sympathetic and parasympathetic neurons – sympathetic postG that innervate the sweat glands – all parasympathetic postG neurons – two types of receptors • 1. nicotinic • 2. muscarinic • adrenergic neurons and NE – most sympathetic postG – two types of receptors • 1. alpha – a1 and a2 • 2. beta – b1 and b2 and b3 ANS receptors • the NTs released by the ANS can either stimulate or inhibit its target – depends on the receptors located in the target 1. Cholinergic receptors – respond to AcH • a. nicotinic – named because they are activated by nicotine – – – – found in the ganglia of the symp. and parasymp. division (all ANS ganglia) respond to AcH release from symp and parasymp preG fibers binding opens channels for the movement of Na and K more Na enters the target neurons within the ganglion – depolarization and initiation of an AP by the postG neurons adrenergic R nicotinic R muscarinic R • b. muscarinic receptors • can bind either Ach or muscarene (Amanita muscaria mushroom) • expressed on tissues “downstream” of post-ganglionic neurons – at the target tissue – e.g. neuromuscular junction (ligand-gated sodium channel) adrenergic R nicotinic R muscarinic R 2. Adrenergic receptors – respond to NE/Epi • alpha and beta classes – a1, a2, b1, b2, b3 • distributed in a specific pattern and respond to either NE or Epi or both • respond to activation by activating G proteins -> second messangers (cAMP or Ca) • therefore they are called G protein coupled receptors adrenergic R nicotinic R muscarinic R • Somatic • ANS Reflex arc •Neural “wiring” of reflex •Requires 5 functional components: 1. sensory receptor, 2. sensory neuron, 3. intergrating center (SC or BS), 4. motor neuron, & 5. effector • By development – Innate, acquired • Where information is processed – Spinal, cranial • Motor response – Somatic, visceral • Complexity of neural circuit – Monosynaptic Classification of Reflexes • Stretch reflex is monosynaptic - causes contraction in response to stretch • Regulates skeletal muscle length and tone • all monosynaptic reflexes are ipsilateral reflexes - input and output on same side • only one synapse in the CNS - between ad single sensory and motor neuron • Sensory receptors are found in muscle spindles – e.g. Patellar reflex – muscle spindles in the quadriceps muscles, hit with a mallet stretches the quadriceps and its tendon - results in contraction Spinal Reflexes •Tendon reflexes - polysynaptic •controls muscle tension by causing muscle relaxation before muscle contraction rips tendons •Generally polysynaptic - more than one CNS synapse involved between more than two different neurons •sensory synapses with 2 interneurons - one inhibitory IN synapses with motor neurons and causes inhibition and relaxation of one set of muscles, the other stimulatory IN synapses with motor neurons and causes contraction of the antagonistic muscle Spinal Reflexes -Postural reflexes - maintain upright position •e.g flexor (withdrawl) reflex polysynaptic •sensory input -> interneuron -> motor neuron which contracts muscles and pulls limb away •PLUS synapses with motor neurons in adjacent SC segments -> contracts muscle •known as an intersegmental reflex arc •IN ADDITION - the sensory input can cross to the other side of the SC (via the gray commisure) where it synapses with and interneuron and motor neuron to contract the antagonistic muscle group and maintains balance = Intersegmental and Crossed extensor reflexes involved withdrawl crossed extensor Reflexes – Laboratory Exercise • • • achilles tendon – also called the ankle-jerk reflex – occurs when the Achilles tendon is tapped while the foot is dorsi-flexed – results in plantar flexion (pointing of toes) – checks if the S1 and S2 nerve roots are intact – Absence: sciatic nerve pathology or disc herniations at L5-S1 level. – Diminshed: hypothyroidism or peripheral neuropathy patellar tendon – also called knee jerk reflex – deep tendon or stretch reflex – tests the function of the femoral nerve and spinal cord segments L2-L4. – Absence or decrease of this reflex is known as Westphal's sign • receptor damage, peripheral nerve disease, involving the dorsal(sensory) columns of the spinal cord • cerebellar lesions • lesions present within the motor cortex of the brain • complete interruption of sensory and/or motor impulse transmission in the femoral nerve • is often known as a characteristic finding in tabes dorsalis, a type of neuro-syphilis triceps – deep tendon or stretch reflex – elicits involuntary contraction of the triceps brachii muscle – initiated by the Cervical spinal nerve 7 nerve root – tested as part of the neurologica examination to assess the sensory and motor pathways within the C7 and C8 spinal nerves. – Absence: essential to try again with reinforcement, with the patient clenching his or her teeth just as the reflex hammer strikes. – Hyper-reflexia: Indicates a potential upper motor neuron lesion. • biceps: – examines the function of the C5 reflex arc and to a lesser degree the C6 reflex arc – activates the stretch receptors inside the biceps brachii muscle which communicates mainly with the C5 spinal nerve and partially with the C6 spinal nerve – induces a reflex contraction of the biceps muscle and jerk of the forearm – strong contraction = 'Brisk' reflex = lesion of upper motor neuron – absent reflex = 'diminished‘ reflex = lower motor neuroe lesions. – change to the biceps reflex indicates pathology at the level of C5/6 or at some point above it in the spinal cord or brain • Babinski – – – – – – – – Joseph Babinski identifies disease of the spinal cord and brain also exists as a primitive reflex in infants. When non-pathological it is Babinski's sign refers to its pathological form three responses possible: Flexion: the toes curve inward and the foot everts - seen in healthy adults. Indifferent: there is no response. Extension of the hallux other toes fan out - the Babinski's sign indicating damage to the central nervous system (usually a lesion on a neuron or neurons) – BUT: Babinski response is normal while asleep and after a long period of walking.