* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download (B) rosiglitazone
Biological neuron model wikipedia , lookup
Multielectrode array wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Neural oscillation wikipedia , lookup
Metastability in the brain wikipedia , lookup
Selfish brain theory wikipedia , lookup
Development of the nervous system wikipedia , lookup
Environmental enrichment wikipedia , lookup
Haemodynamic response wikipedia , lookup
Caridoid escape reaction wikipedia , lookup
Mirror neuron wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Central pattern generator wikipedia , lookup
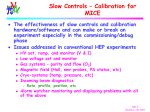
Single-unit recording wikipedia , lookup
Neural coding wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Premovement neuronal activity wikipedia , lookup
Neuroanatomy wikipedia , lookup
Biochemistry of Alzheimer's disease wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Hypothalamus wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Nervous system network models wikipedia , lookup
Pre-Bötzinger complex wikipedia , lookup
Circumventricular organs wikipedia , lookup
Synaptic gating wikipedia , lookup
Journal Club 2007年10月11日 8:20-8:50 B棟8階 カンファレンス室 亀田メディカルセンター 糖尿病内分泌内科 Diabetes and Endocrine Department, Kameda Medical Center 松田 昌文 Matsuda, Masafumi Figure 1: Search strategy profile Table 1: Characteristics of trials and participants RECORD intrim PROactive Figure 2: Overall risk for congestive heart failure with (A) TZDs; (B) rosiglitazone; and (C) pioglitazone TZDs Figure 2: Overall risk for congestive heart failure with (A) TZDs; (B) rosiglitazone; and (C) pioglitazone rosiglitazone Figure 2: Overall risk for congestive heart failure with (A) TZDs; (B) rosiglitazone; and (C) pioglitazone pioglitazone Figure 3: Overall risk for cardiovascular death with (A) TZDs; (B) rosiglitazone; and (C) pioglitazone trials TZDs Figure 3: Overall risk for cardiovascular death with (A) TZDs; (B) rosiglitazone; and (C) pioglitazone trials rosiglitazone Figure 3: Overall risk for cardiovascular death with (A) TZDs; (B) rosiglitazone; and (C) pioglitazone trials pioglitazone Figure 4: Comparison of risk of congestive heart failure (A) and cardiovascular death (B) for rosiglitazone and pioglitazone Table 2: Congestive heart failure events reported in the thiazolidinedione trials Table 3: Congestive heart failure and cardiovascular deaths by type of thiazolidinedione ? Note We did not include the smaller trials available for either rosiglitazone or pioglitazone, since they might not have had long enough observation times to accurately measure the risk for congestive heart failure and cardiovascular death. A recent meta-analysis showed that patients given rosiglitazone had a higher risk of myocardial infarction than controls; they also had a higher risk of cardiovascular death, although this was not significant. Interpretation Longer followup and better characterisation of such patients is needed to determine the effect of TZDs on overall cardiovascular outcome. 1Department of Medicine, Division of Endocrinology, Beth Israel Deaconess Medical Center and Harvard Medical School, 99 Brookline Avenue, Boston, Massachusetts 02215, USA. 2Department of Internal Medicine, Center for Hypothalamic Research, The University of Texas Southwestern Medical Center, 5323Harry Hines Boulevard, Dallas, Texas 75390-9077, USA. 3Division of Neuroscience, Oregon National Primate Research Center, Oregon Health & Science University, 505 NW185th Avenue, Beaverton, Oregon 97006, USA. 4State Key Laboratory of Pharmaceutical Biotechnology, School of Life Sciences, Nanjing University, Nanjing 210093, China. “Chinese remedmy treats diabetes ???” Mechanisms for the development of diabetes mellitus • Impairment of insulin secretion • Impairment of insulin sensitivity Impairment of glucose sensing in the brain (tasting?) Thrifty Gene Theory Abnormality in the hypothalamus in the brain Brain Hypothalamus Abnormality in the Fat tissue Obesity (Energy Storage) Muscle insulin resistance + Delayed & Hyper insulin secretion Neel JV: Diabetes mellitus: a ‘thrifty’ genotype rendered detrimental by “progress”? Am J Hum Genet 14:353–362, 1962 fMRI Response Matsuda, M. et al Diabetes 48:1801-1806, 1999 Nature 405:1058-1062, 2000 SUR1-Kir6.2 on pancreatic beta cells Background Mutant Kir6.2 forms functional KATP channels that are 250 times less sensitive to closure by ATP and, when expressed in pancreatic b-cells, causes impaired glucose induced insulin secretion and diabetes. Journal club Aug 3, 2006 Leptin → Lean : stop appetite, increase energy exp. (increased sympathetic NS) Insulin → Lean Increase POMC/CART decrease NPY/AgRP IRS aMSH MC4Receptors Hypothesis to be proved The POMC-mut-Kir6.2 mice expressed the transgene only in POMC neurons has impairment in the whole-body response to a systemic glucose load. Glucose sensing by POMC neurons became defective in obese mice on a highfat diet. Figure 1 | Glucose sensing is lost in POMC-mut-Kir6.2 neurons a, Structure of the Kir6.2[DN2–30,K185Q]–GFP transgene. Mice. For generation of POMC-mut-Kir6.2 mice, the mut-Kir6.2 cassette (Kir[D2–30,K185Q]–GFP)7 was inserted into a POMC BAC genomic clone so that the ATG codon replaced that of POMC, as described previously. POMC-mut-Kir6.2 BAC DNA was prepared using a commercially available kit (Qiagen) and microinjected into pronuclei of fertilized one-cell-stage embryos of FVB mice (Jackson Laboratories), resulting in the generation of two POMC-mut-Kir6.2 lines that were maintained on an FVB inbred background. POMC-GFP and NPY-GFP mice were generated by insertion of hrGFP into a POMC or NPY BAC, respectively, as described above. Ucp2-/- mice were used as described previously. To generate POMC-GFP;Ucp2-/- mice, heterozygous POMC-GFP transgenic mice were crossed with heterozygous Ucp2-/- mice. For high fat diet feeding experiments, mice were placed on a high-fat rodent diet (45% kcal from fat; Research Diets Inc; D12451) at four weeks of age for a total of 20 weeks (or 8 weeks for electrophysiological studies). b, Double immunofluorescence staining for GFP (green) and b-endorphin (yellow) in the arcuate nucleus of POMC-mut-Kir6.2 mice. Arrows indicate neurons containing both b-endorphin and Kir6.2[DN2–30,K185Q]–GFP. The carboxy (C)-terminal end of the mutant Kir6.2 contains a green fluorescent protein (GFP) tag that does not alter the function of the channel but makes it possible to visualize cells expressing mutant Kir6.2 (mut-Kir6.2). b-endorphin (a marker for POMC neurons) c, Loose patch recordings of POMC neurons from wild-type (WT, POMC-GFP) and POMC-mut-Kir6.2 transgenic mice. Recordings were made for 5–10 min in aCSF solution containing 5mM glucose. Once stable activities were observed, the recording chamber was perfused with aCSF solution containing 3mM glucose for 5–15 min, then switched back to 5mM glucose for a further 5–10 min. Panels show a representative time course of firing rate of a glucose-excited wild-type neuron (left) and a glucose-insensitive POMCmut-Kir6.2 neuron (middle). Each bar represents the average firing rate for a 20-s interval; AP, action potential. The right panel shows the percentage of neurons activated by 5mM glucose (recordings were obtained from 22 wild-type mice and 12 POMC-mut-Kir6.2 mice, with 2–4 POMC neurons recorded per animal). OGTT 1g/kg BW d, aMSH release from hypothalamic slices of wild-type and POMC-mutKir6.2 mice (n=3 hypothalamic slices per data point, ±s.e.m.). e, Representative glucose tolerance curves from eight-week old male wild-type and POMC-mut-Kir6.2 littermates (n=8–10 mice per genotype, ±s.e.m.). Asterisk, P<0.05; two asterisks, P<0.01 compared with wild-type at a given time point. Leptin → Lean : stop appetite, increase energy exp. (increased sympathetic NS) Insulin → Lean Increase POMC/CART decrease NPY/AgRP IRS aMSH MC4Receptors Figure 2 | Glucose-sensing is lost in POMC neurons of mice on a high-fat diet a, Glucose-induced aMSH release from hypothalamic slices of wildtype C57BL/6 mice fed chow or a high-fat diet for 20 weeks (mean ± s.e.m.). b, Bar chart showing the percentage of POMC neurons activated by 5mM glucose in loose-patch recordings from POMC-GFP mice fed either chow or a high-fat diet (HFD) for eight weeks. c, In situ hybridization of Ucp2 mRNA in wild-type mice (dark field photomicrograph of 35S-silvergrains). VMH, ventromedial hypothalamus; Arc, arcuate nucleus. d, Double immunohistochemistry and in situ hybridization detecting b-endorphin protein and Ucp2 mRNA, respectively, in coronal sections from wild-type mice. Arrows indicate the presence of b-endorphin neurons co-localized with Ucp2 mRNA. 3V, third ventricle. Ucp2 In pancreatic b-cells, glucose sensing is negatively controlled by the mitochondrial protein UCP2. UCP2 mediates proton leak across the inner mitochondrial membrane, decreasing the yield of ATP from glucose. UCP2 activity is increased in b-cells of animal models for type 2 diabetes, and various studies have provided evidence that this increase in UCP2 activity has a role in the development of b-cell dysfunction. UCP2 is also expressed in the brain, including in the arcuate nucleus. e, f, Relative hypothalamic Ucp2 mRNA expression in wild-type mice on a high-fat diet (e, n=12; ±s.e.m.) and ob/ob (f, n=6; ±s.e.m.) mice. Two asterisks, P<0.01; three asterisks, P<0.001 compared to wild type (WT). Figure 3 | Genipin activates glucose-excited POMC neurons. Representative time course of firing rates of loose-patch recordings on POMC neurons from wild-type (WT) (a, b), Ucp2-/- (c), and POMC-mut-Kir6.2 (d) mice. Recordings were made for 5–10 min in aCSF solution containing 5mM glucose. Once stable firing rates were observed, the recording chamber was perfused with aCSF solution containing 3mM glucose for 5–10 min, and then genipin (20 mM) was added as indicated by the arrow. a, A glucose-excited POMC neuron activated by genipin, representative of 16 out of 22 glucose-excited neurons recorded. b, A glucose-insensitive POMC neuron not activated by genipin, representative of 12 out of 13 glucose-insensitive neurons recorded. Genipin We have recently identified a membranepermeant molecule, genipin, which inhibits UCP2-mediated proton leak. Geniposide, which is found in the fruit of Gardenia jasminoides Ellis, in Tsumura TJ-135 [茵チン蒿湯], used for liver diseases, is metabolized to genipin. “Chinese remedmy treats diabetes” (BBC news June 6, 2006) c, A glucose-excited POMCUcp2-/- neuron not activated by genipin, representative of 11 out of 12 glucose-excited Ucp2-/- neurons recorded. d, A POMC-mut-Kir6.2 neuron not activated by genipin, representing 13 out of 14 neurons recorded. e, Bar chart showing the percentage of neurons activated by genipin. Figure 4 | Acute inhibition or genetic deletion of UCP2 restores or prevents loss of glucose sensing in POMC neurons as a result of obesity induced by a high-fat diet. a, b, aMSH secretion from hypothalamic slices from wild-type (a, WT) and Ucp2-/- (b) mice in response to glucose, with or without genipin (20 mM). Data are presented as mean ± s.e.m., n=6 mice for each experimental condition. Asterisk, P<0.05. a, b, aMSH secretion from hypothalamic slices from wild-type (a, WT) and Ucp2-/- (b) mice in response to glucose, with or without genipin (20 mM). Data are presented as mean ± s.e.m., n=6 mice for each experimental condition. Asterisk, P<0.05. Messages First, we have shown that glucose sensing in POMC neurons has an important role in controlling systemic glucose homeostasis. Second, glucose sensing in these neurons is lost with obesity linked to a high-fat diet. Finally, UCP2 is involved in this loss of glucose sensing, perhaps by decreasing ATP production in POMC neurons. As POMC neurons represent only a fraction of all glucoseexcited neurons in the brain (which include melaninconcentrating hormone (MCH) neurons in the lateral hypothalamus, neurons in the ventromedial hypothalamus, and neurons in the hindbrain), we suggest that UCP2mediated loss of glucose sensing in glucose-excited neurons could be an important pathogenic component of type 2 diabetes.