* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Neuropathology Review
Environmental enrichment wikipedia , lookup
Perivascular space wikipedia , lookup
Metastability in the brain wikipedia , lookup
Axon guidance wikipedia , lookup
Biochemistry of Alzheimer's disease wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Nervous system network models wikipedia , lookup
Aging brain wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Optogenetics wikipedia , lookup
Intracranial pressure wikipedia , lookup
Synaptogenesis wikipedia , lookup
Development of the nervous system wikipedia , lookup
Synaptic gating wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Neuroanatomy wikipedia , lookup
Subventricular zone wikipedia , lookup
Neuroregeneration wikipedia , lookup
Eyeblink conditioning wikipedia , lookup
Channelrhodopsin wikipedia , lookup
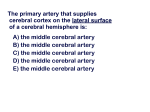
Neuropathology By: Vero Versari Pathologic Rxns in the CNS: Neuron: has a big nucleus and nucleolus. Nissl substance at soma and dendrites, but not at axon. The spectrum of reactions of neurons to disease: 1. Simple loss: Alzheimer 2. Ischemic change: Infarct 3. Central chromatolysis: Damage to axon 4. Mineralization (Ferrugination): Neuron calcifies w/ damage 5. Pathologic Inclusions Ischemic Neuron: Caused by infarct, cardiac arrest. Has pyknotic nuclei and red cytoplasm. Central Chromatolysis: The body of the neuron swells up and the nucleus and Nissl substance goes toward the periphery. The neuron is making 2x the amount of protein in order to recuperate. Axon Reaction: Chromatolysis: Production of protein until contact is established w/ the mm. W/ maintained insult, the neuron dies. Simple Chromatolysis: Non-specific change. Nucleus stays at center, but Nissl subs. goes toward periphery. Ferruginated Neurons: Mineralization. Calcification. Can see the triangular shape. Lewy Body: Inclusion in Parkinson’s Pt. @ Locus Ceruleus and Subs. Nigra. Must be correlated w/ clinical Sx to Dx Parkinson’s b/c could be due to aging. Pick Body: Found in Pick’s Dementia. Hirano Bodies: Cytoplasmic eosinophillic inclusions found in Alzheimer’s and senile Pts. Lafora Body: Found in Pts. w/ Myoclonic Epilepsy. Negri Bodies: Intracytoplasmic eosinophillic inclusions found in Rabies. Neurofibrillary Tangle: Neuronal degeneration found in Alzheimer’s and senile Pts. Tear drop shape. Seen w/ silver stain. Granulovacuolar Degeneration: Granule inside a vacuole due to neuronal degeneration. Glycogen: Accumulates @ cytoplasm in Pompe’s Disease. Mucopolysaccharides: Accumulate in Hurler’s Disease. Ganglioside: Tay-Sachs Disease. Neuromelanin: Non-pathological pigment found @ CNS (Subs. Nigra, Locus Ceruleus, Dorsal Vagal Nuclei) and PNS (Dorsal Root). Lipofuscin: Degenerated organelles. Cardiac mm also has it. Inc. w/ age. Children w/ Progeria have inc amnts. Axonal Swelling: W/ axonal damage. The axons look round, “spheroids”. On a silver stain slide, the axons were cut transversally and longitudinally (look like sausages). Cerebellar Axonal Swelling: Purkinje neurons. W/ damage, axons take torpedo shapes. Can see internal granular layer, Purkinje layer, and molecular layer. Astrocytes: Seen w/ gold stain. No processes are seen on H&E, except if there’s a tumor or gliosis). Fibrillary Astrocytes: Can see many processes. Gemistocytic Astrocytes: Have a lot of cytoplasm. Very pink (eosinophillic). Looks reactive or neoplastic. Pilocytic Astrocytes: Elongated nucleus (spindle shaped). Bipolar (only two processes). Found @ gliosis and tumors. Astrocytes maintain the hematoencephalic barrier. Electronic Microscopy: To detect the presence of tumors. You see Intermediate filaments. Immunostain Glial Fibrillary Acidic Protein (GFAP): Found in astrocytes and ependymal cells. Rosenthal Fibers: Degenerated Astrocyte processes seen in tumors and gliosis. So, its not Dx of neoplacia. Gliosis: The same as fibrosis in any other organ. A scar, due to collagen deposition. Will see a cavitation. The three etiologies of Rosenthal Fibers: Reactive, Neoplastic, Genetic/Metabolic. Reactive Astrocytes seen in hyperammonemic conditions: Alzheimer Type II Astrocytes: Related more to Hepatic Encephalopathy. Naked nucleus, no cytoplasm, clearing seen. Alzheimer Type I Astrocytes: Wilson’s dz.(copper), PML (progressive multifocal leukencephalopathy). Large nucleolus, clumped chromatin. Corpora Amylacea: Degenerated Astrocyte processes @ periventricular and subpial. Inc. w/ age. Oligodendrocytes: Look like fried eggs. Nucleus w/ a halo, which occurs when time elapses before the slide is fixated in formalin. Oligodendrocytes make myelin sheaths. Ependyma: Covers ventricles. +GFAP. Ependymal Granulation: Subglial cells which are under the ependymal cells that proliferate when there’s ependymal cell damage (i.e. meningitis), forming granulation to protect. Stenosis of the aqueduct: Caused by cellular proliferation. Damage after meningitis, causing aqueduct stenosis ----> hydrocephalus. Mesenchymal components of the CNS: Microglia, Monocytes, Macrophages. Microglia: are now accepted as monocytes - derived resident constituents of the reticuloendothelial system. Most convert into macrophages. Microglia are very small cells that unless they are activated it is hard to see them on microscope. They have few ramifications. Microglia Nodule: Occurs in viral dzs Microglia that form aggregates about small foci of tissue necrosis. Neuronophagia: Microglia that congregate around portions of dying neurons. Macrophages: Two sources: Bloodstream via diapedetic monocytes. Transformation of indigenous microglia. Meninges: Dura mater Leptomeninges: Pia Mater Arachnoid Vascular Disorders: Cerebrovascular Dz (CVD): Any abnormality of the brain resulting from a pathological process involving blood vessels, causing inadequate oxygenation of brain tissue. Neuronal death: Laminar necrosis. Piknotic nuclei, pink cytoplasm. Layers 3,5, & 6 of cortex. Selective Vulnerability: Certain areas have neurons which are more sensitive to changes due to: Local energy metabolism requirements, hemodynamic factors, and local neurotransmitters. The sensitive areas are: Hippocampus: CA 1 (Sommer’s Sector). The pyramidal layer of the hippocampus is divided into: CA 1, CA 4, CA 3, CA 2 (from least resistant to ischemia/hypoxia to most resistant). Cerebral Cortex: Layers 3,5,& 6 (Laminar necrosis) Cerebellum: Diffuse necrosis of Purkinje cells. Hippocampus sclerosis: Will have gliosis. Laminar Necrosis: Will have a thin cortex due to dead cells. The cortex can detach from the white matter. On microscope can see that the tissue loses the affinity for the stain and can see few cells. Bilateral necrosis of Globus Pallidum: Secondary to hypotension (blood doesn’t reach area). Risk factors for cerebral infarction: Atheroma, hypertension, serum lipids (obesity, diet), diabetes mellitus, heart dz, dz of neck artery, meds., smoking, hypothyroidism. Causes of brain infarction: Emboli: Mitral endocarditis-->emboli-->to brain-->lodge at distal branches of arteries. Middle Cerebral artery is the branch most commonly affected. Atheroma Compression: Uncal herniation-->infarct of posterior cerebral artery. Types of Cerebral Infarction: -Territoral: Major Territorial: Atheroma + Thrombosis or Emboli Minor Territorial: Emboli-->because they lodge at distal branches. Dural Herniation: PCA*, ACA -Border boundary zone: Hypotension -Focal / Multifocal: Vasculitis (multiple infarcts due to vasculitis). -Lacunar: Basal Ganglia. Hypertension + Lipohyalinosis. -Brainstem: Hypertension + Lipohyalinosis. -Transterritorial: Venous. Involves gray and white matter (artery only involves gray matter) Border Zone (watershed) Infarct: Atheroma-->hypotension-->diminished blood flow to distal branches -->Infarct. Has a hemorrhagic component: when pressure is normalized and irrigation returns, vessels are still damaged, so hemorrhage results. Can be seen betw. Anterior and Middle Cerebral arteries, or betw. Middle and Post Cerebral. Also @ Cerebellar arteries. There’s an area of the brain (temporoparietoccipital) where there’s part of Ant., Middle, and Post. Cerebral arteries that irrigate, so no infarct occurs. Ischemic Infarct (complete occlusion): Thrombus-->infarct @ arterial territory limited to that area where the thrombus was formed. A picture of a recent infarct shows ventricular obliteration, midline deviation, enlarged hemisphere, soft to touch. A CT scan shows the affected side darker than normal and midline deviation. A picture of an old infarct (mos-yrs) shows a cavity full of liquid w/ astrocytes (fibrillary reactive astrocytes) throwing threads from one side to the other. If the infarct occurs @ Brocca’s area, speech prblms. would result. Cerebral Infarction Histology: -6-12 hrs.: Diffuse reduction in staining intensity of tissues. Edema (white spaces. Shrunken neurons) -48 hrs.(2 days): Prominent blood vessels and some neutrophils. -72-96 hrs (3-4 days): Clusters of macrophages around blood vessels (max @ 2weeks). -2 weeks: Prominent astrocytosis; eventually results in fibrillary gliosis. Sequence of microscopic changes and the evolution of the cerebral infarct: Normal neurons-->shrunken, red neurons and PMN leukocytes (hrs-3dys)->Macrophages (3-5dys)-->encrusted neurons, astrocytes, cystic cavity (wks-mos.) Infarct can affect the cerebral peduncles, making them look smaller, there is degeneration of fibers going down on the SAME SIDE as the infarct, b/c haven’t crossed yet at this point. Sx are CONTRALATERAL. Hemorrhagic Infarct (embolus, pressure): Emboli-->ischemia, vessel damage->emboli moves-->blood flow resored-->extravasation. Cerebral Embolism: 30-60% of strokes are embolic in nature. Most thru Middle Cerebral artery. Most produce transient occlusion only. Sources: Heart Dz, Dz of extracranial neck arteries (Carotids), Cardiac surgery, Systemic Embolism of fat (pt. w/ fracture of femur) or venous gases (pt. who gives birth) Post. Cerebral Hemorrhagic infarct due to uncal herniation, which compresses. Not known why it is hemorrhagic. Old Hemorrhagic Infarct: Orange color. Hemosiderin pigment inside macrophages. Can see w/ an iron stain. Cerebral Venous Thrombosis (CVT): Causes: Infxns. (intracranial, facial, head injury, neurosurgical procedures and neoplasm). Risk Factors: Preg. and puerperium, oral contraceptives, congential heart dz, hematologic abnormalities, severe dehydration (baby w/ severe diarreah-->thrombosis of Sup. Sagital Sinus. Affects both gray and white matter due to retrograde flow. Global Ischemia: When the heart stops (cardiac arrest). Prolonged entubation. No viable cells. Cortex has a dirty gray color. Arteriolosclerosis - Lipohyalinosis: Diabetics / HBP. Hyalination of wall, occluding the lumen. Lacunar Infarct: <1.5cm diameter. @ Basal Ganglia mostly, but seen also @ thalamus, Pons. Hypertension, Lipohyalinosis, deep gray matter. Intracranial Hemorrhage: Risk Factors: Hypertension, rupture of Saccular Aneurism (Berry Aneurism), Thrombocytopenia, Mycotic Aneurism, vascular malformation, tumor, Amyloid (congophilic) angiopathy (@ meningeal vessels get amyloid deposits-->break and bleed). Types of Intracranial Hemorrhage: -Cerebral Hemorrhage: Hypertensive hemorrhages -Subarachnoid Hemorrhage: Ruptured Saccular Aneurysm -Epidural and Subdural Hemorrhage: Trauma -Mixed: Vascular malformations Hypertensive Hemorrhages: 1. Basal ganglia - Putamen 2. Thalamus 3. White matter (lobar) 4. Pons 5. Cerebellum Microaneurism: Charcot-Bouchard Aneurism Old Hemorrhage: The blood is reabsorbed and a flat, regular cavity remains (Infarcts are irregular). Saccular Aneurism: Frequent cause of subarachnoid hemorrhage. Aged young and middle age adults. 90% Ant. circulation (Ant. Comm.). Formed at bifurcations, where the wall is weaker. Can break thru the subarach. space and reach the ventricle. Can go to subdural space (Infarcts compress, herniation). Multiple Aneurisms: Related to Fibrocystic Kidney Dz. Fusiform Aneurism: Caused by Arteriosclerosis Infective aneurism: Used to be called Mycotic Aneurism. Bacteria @ vessel->debilitation -->rupture-->hemorrhage. CNS Vascular Malformations: -Arteriovenous: Trichome stain. Collection of abnormal bv’s interposed betw. feeding arteries and draining veins. Males. Bleeding in age 10-30, rare after 60. Spinal cord. -Venous Angioma: Trichome stain. -Capillary Telangiectasia: Small vessels, look like capillaries. -Cavernous Hemangioma: No parenchyma betw. vessels. CNS Neoplasms: WHO Grading System: -GRADE I: Pilocytic Astrocytoma -GRADE II: Diffuse Astrocytomas -Fibrillary -Protoplasmic -Gemistocytic -GRADE III: Anaplastic Astrocytoma -GRADE IV: Glioblastoma Multiforme p53 mutation-->neoplastic cell-->Astrocytoma-->p16 gene-->Anaplastic Astrocytoma-->chr. 10 loss-->Glioblastoma Pilocytic Astrocytoma: W/ Medulloblastoma it’s the most common in children. Circumscribed. From Optic nerve to conus medullaris. Slow growing. Bipolar w/ elongated nuclei. Malignancy rare. NF 1. No p53 mutation. Good Px. - Cerebellar Astrocytoma: Cystic w/ a mural nodule on CT scan. Surgery radiation. Children in 1st 2 decades. 10-25 yr. survival. Rosenthal fibers. Microcystic degeneration (microcysts unite forming a large one). Non-malignant vessel proliferation. Diffuse Astrocytoma: 30-40yrs. Seizures. p53 mutation. @cerebral hemisphere, brainstem. 6-8 yr. survival. Cortical fading. Not much nuclear pleomorphism, no necrosis. Anaplastic Astrocytoma: 41 yrs. Seizures. @cerebral hemisphere. Nuclear atypia, mitotic activity, proliferation of bv’s. No necrosis or perifocal edema. Glioblastoma Multiforme: Most frequent tumor of CNS after metastasis. 45-70 yrs. p53 mutation. Nuclear atypia, mitotic activity, microvascular proliferation, glomeruloid shape of vessels, pseudopalisading, pleomorphism, giant cells, multinucleation. Ct scan shows ring like enhancement w/ central necrosis. Affinity for corpus callosum, crossing to other hemisphere (“Butterfly Sign”). 9 mo survival. Oligodendroglial Tumors: -Oligodendroglioma: WHO GRADE II -Anaplastic Oligodendroglioma: WHO GRADE III Oligodendroglioma: 35-40 yrs. chr19 & 1. @cerebral white matter. Seizure & HA. Multifocal Calcifications. No pleomorphism or necrosis, round nuclei w/ halo, fibrovascular septas. 3-5 yr survival Anaplastic Oligodendroglioma: Necrosis, pleomorphism, vascular proliferation, enlarged nuclei, mitosis. Central Neurocytomas: Similar to Oligodendroglioma. Differentiated by sinaptomycin which tells if it’s neuronal origin (central neurocytoma) Young adults. Midline neoplasm, close to septum pellucidum. Hydrocephalus. Ependymal Tumors: -Ependymoma: WHO GRADE II -Anaplastic Ependymoma: WHO GRADE III -Myxopapillary Ependymoma: WHO GRADE I -Subependymoma: WHO GRADE I @ 4th ventricle Ependymoma: 6yrs and 30-40yrs. chr22. @ 4th ventricle, lat. ventricle, spinal cord. Circumscribed. Post. Fossa. N/V, HA sec. to hydrocephalus. 3-5 yr. survival. *Perivascular pseudorossette, Ependymal true rossette. Anaplastic Ependymoma: Necrosis, pleomorphism, pushing parenchyma. Myxopapillary Ependymoma: 36yrs. @conus-cauda-filum terminale. 14yr(subtotal)-19(total removal) survival. Mucus accumulation, many vessels. Choroid Plexus Tumors: 1yr. @epi. of choroid plexus. SV 40, DNA viruses. -Choroid Plexus Papilloma: WHO GRADE I. Coliflower. Sec to hydrocephalus. Total removal. One layered, no necrosis. -Choroid Plexus CA: WHO GRADE III. Pseudostratified, no papilas. Mitosis. Pineal Parenchymal Tumors: -Pineocytes: photosensory and neuroendocrine functions -Pineocytoma: WHO GRADE II. All ages. Slow growth. Parinaud’s Synd. (vertical gaze paralysis). 5yr survival. Normal pineal architecture. -Pineoblastoma: WHO GRADE IV. Children. Craniospinal seeding, metastasis to lungs. Poor Px. Embryonal Tumors: -Central Neuroblastoma: WHO GRADE IV -Medulloblastoma: WHO GRADE IV -Ependymoblastoma -Supratentorial PNET’s Central Neuroblastoma: 25% 2yrs, 50% 5yrs, 30% 1st decade. @Cerebrum. CSF dissemination. Extraneural metastasis. Homer-Wright pseudorossettes. Hyperchromatic oval nuclei. Medullobastoma: 7yrs, 21-40yrs. chr17q &1. Invasive embryonal tumor of the cerebellar vermis. Truncal ataxia, disturbed gait, intracranial HBP, HA, N/morning V. Ext. granular layer. CSF seeding to ventricles and spinal cord . Icing. Like Neuroblastoma. Pyknotic nuclei, carrot shaped cells. Homer-Wright pseudorossettes. Cranial and peripheral nerve tumors: -Schwannoma: WHO GRADE I -Neurofibroma: WHO GRADE I -Malignant Periph. Nerve Sheath Tumor: WHO GRADE III or IV -Neurofibroma grows inside the nerve separating the fibers, but Schwannoma grows next to the nerve. Schwannoma: 40-60yrs. NF 2. Encapsulated benign tumor. @vestibular div. CN8, cerebellopontine angle. Tinnitus, hearing difficulty. Antoni A(compact, fusiform cells, makes Verocay body) and B(loose) patterns. Verocay bodies. Can have cystic degeneration, hemorrhage, involve CN5&7 if not removed early. Neurofibroma: All ages. NF 1. Solitary nodule. Loose mucinous tumor w/ wavy fibers. @cutaneous or major trunk nerve. Good Px. Meningioma: WHO GRADE I(whorls), II, III. Middle age & elderly. chr.22del. From neoplastic arachnoidal cells. @ 1. Parafalcine 2. Lateral sulcus 3. Orbitofrontal cortex 4. Cerebellopontine angle. Hyperostosis. Atypical Meningioma: WHO GRADE II. Mitosis, focal necrosis, pleomorphism, hypercellularity Anaplastic Meningioma: WHO GRADE III. Necrosis, mitosis, neural tissue invasion, inside parenchyma. Psamomma bodies: whorls that degenerate and calcify. Neurocutaneous Syndromes (Phakomatoses): Inherited disorders w/ hamartomas (bv tumor) @ NS & skin. NF 1: chr17q11. Pilocytic Astrocytoma, MPNST, Optic Nerve Glioma & Neurofibroma, Iris Hamartomas, Osseous lesions, Pheochromocytoma, Leuk. Cafe au lait spots, axillary freckling. 1st degree relative w/ NF1. Glial Hamartomas (Leisch Nodules). NF2: Bil. Vestibular Schwanommas, Meningioma, Spinal ependymomas, Neurofibroma. 1st degree relative w/ NF2. Post. subcapsular lens opacity, cerebral calcification. Von Hippel Landau Dz (VHL): VHL gene, chr3p25. Nervous System, Retina hemangioblastoma, Renal Cell CA, Pheo., Visceral cysts. Life expectancy 49yrs. @ cerebellum. Nodular or cystic. Like Cystic Astrocytoma (differ by age b/c Astro pts. are children). Mural nodule w/ myelin stain. -Hemangioblastoma: Reticulin fibers, stromal cells, bv’s. Tuberous Sclerosis: TSC1 chr9 and TSC2 chr16 genes. Subependymal giant cell astrocytoma(Hamartomatous lesions, “candle guttering“), Cortical Tubers. Adenoma Sebaceum (cutaneous angiofibroma), peau chagrin, subungal fibromas. *Triad: Angiofibromas, Seizures, and Mental Retardation. CNS Metastases: Lung 50%, Breast 5%, Malignant Melanoma 10.5% Hemorrhage as 1st manifestation of CNS Metastasis: -Malignant Melanoma: inc. affinity to CNS, to cauda equina -Renal Cell CA -ChorioCA Metastatic tumor mostly betw. cortex and white matter. Primary Lymphoma of the Brain: Male. At risk: Immsupp & post. transplant. Immunoblastic variant most common. B cell Lymphomas. Dx: bv wall affinity, reactive lymphocytes, reticulin fibers. Goes to brain thru meninges. Poor Px.