* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download M555 Medical Neuroscience
Neuroregeneration wikipedia , lookup
Proprioception wikipedia , lookup
Axon guidance wikipedia , lookup
Metastability in the brain wikipedia , lookup
Subventricular zone wikipedia , lookup
Caridoid escape reaction wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Neural engineering wikipedia , lookup
Nervous system network models wikipedia , lookup
Embodied language processing wikipedia , lookup
Haemodynamic response wikipedia , lookup
Central pattern generator wikipedia , lookup
Synaptic gating wikipedia , lookup
Neuromuscular junction wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Microneurography wikipedia , lookup
Synaptogenesis wikipedia , lookup
Premovement neuronal activity wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Circumventricular organs wikipedia , lookup
Optogenetics wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Development of the nervous system wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Neuroanatomy wikipedia , lookup
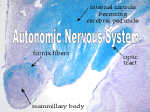
M555 Medical Neuroscience Motor Systems - Autonomic Motor Comparing Autonomic Motor and Somatic Motor Systems motor neurons Somatic Motor CNS effector Autonomic Motor CNS effector effectors Somatic Motor CNS Autonomic Motor autonomic ganglion CNS preganglionic neuron postganglionic neuron action of motor neurons on effectors Somatic Motor CNS effector agonist epibatidine antagonists alpha-bungarotoxin gallamine pancuronium succinylcholine tubocurarine Autonomic Motor CNS effector Somatic and Autonomic Motor Systems sensory input motor output reflexes descending control and modulation from brain supplemental motor cortex premotor cortex primarymotor cortex somatic somatosensory cortex thalamus (VPL) sensory afferents interneurons somatic motor neurons skeletal muscle cells somatosensory cortex cigulate cortex autonomic hypothalamus thalamus (VPL) sensory afferents interneurons preganglionic autonomic motor neurons postganglionic autonomic motor neurons cardiac muscle cells smooth muscle cells gland cells Autonomic Motor System Major Divisions sympathetic parasympathetic enteric Sympathetic and Parasympathetic Divisions origin - location of preganglionic neurons Sympathetic spinal cord T1 - L3 Parasympathetic brain stem midbrain pons medulla spinal cord S2-S4 efferent pathway Sympathetic paraverterbral chain ganglia spinal nerve gray ramus white ramus preverterbral ganglia efferent pathway Parasympathetic brain stem ganglia EWN midbrain SSN pons ISN NA medulla DVMN spinal cord S2-S4 neurotransmitters and receptors PreG: preganglionic neuron Parasympathetic PostG: postganglionic neuron cns PreG PostG target ganglion Sympathetic cns PreG PostG target ganglion Special Case for Sympathetic Autonomic smooth muscle cells in some blood vessels secretory cells in sweat glands cns PreG chromaffin cells in adrenal medulla adrenal capillary Neurotransmitters/Receptors at Cholinergic Synapses Nicotinic - neuromuscular junctions SMNs >>> skeletal muscle cells - preganglionic autonomic neurons >>> postganglionic neurons Muscarinic - postganglionic neurons >>> effectors at Adrenergic Synapses Alpha (includes subtypes 1 and 2) alpha 1 are found on smooth muscle cells in walls of arterioles in most organs activation of alpha 1 receptors contracts smooth muscle and produces vasoconstriction Beta (includes subtypes 1, 2) beta 1 receptors are found on pacemaker and contractile cardiac muscle cells activation of beta 1 receptors increases heart rate and contractility beta 1 agonists increase cardiac output; “beta blockers” ease work demands on the heart beta 2 receptors are also found on smooth muscle cells in walls of bronchioles activation of beta 2 receptors relaxes smooth mucle cells and produces bronchiole dilation beta 2 agonists help increase bronchiole diameter effect on target cells, tissues and organs Sympathetic Parasympathetic normal in dark Autonomic Reflexes and Disorders Pupillary Light Reflex eye normal in light eye constrictor muscle in iris postganglionic axons in ciliary nerves normal response optic nerve spot of light ciliary ganglion preganglionic axons in CN III optic tract damage to retina or optic nerve on side of “X” X X spot of light E-W pretectum E-W oculomotor nucleus spot of light partial damage to retina or optic nerve on side of “X” X X pretectum spot of light spot of light relative afferent pupillary defect (Marcus-Gunn pupil) from figure 17- 38 E-W = Edinger-Westphal nucleus Argyll Robertson pupil damage to optic tract or pretectum on side of “X” X X spot of light spot of light damage to optic tract or pretectum on side of “X” damage to oculomotor nerve on side of “X” light no constriction direct or consensual in response to light X light damage to oculomotor nerve on side of “X” X constriction during accommodation-convergence spot of light X spot of light Autonomic Reflexes and Disorders Horner’s Syndrome hypothalamus tarsal muscle eye eyelid dilator in iris dilator in iris brain stem superior cervical ganglion eyelid tarsal muscle cervical spinal cord sweat glands smooth muscle cells in blood vessels thoracic spinal cord paravertebral sympathetic ganglia (not to scale) signs/symptoms preganglionic or postganglionic? place a few drops of peredrine in affected eye peredrine - an amphetamine derivative enhances release of norepinephrine from axon terminals before peredrine after peredrine after peredrine baroreceptor reflex sensory afferents carotid artery brain stem sensory afferents CN X preganglionic parasympathetic neurons aorta spinal cord heart postganglionic sympathetic neurons systemic arterioles preganglionic sympathetic neurons thoracic levels Autonomic Reflexes and Disorders Case A T.F is 30-years-old and is currently being treated for hypertension. For no apparent reason, T.F. sometimes experiences feelings of anxiety. He also complains of headaches, nausea, abdominal pains and feeling hot. He notes that he’s lost some weight since the onset of his problems. During certain “episodes,” T.F.’s heart races, he sweats profusely and exhibits nervous tremors. His physician schedules a MRI and a urinalysis to check for higher-than-normal levels of catecholamines. Although a final diagnosis await the results of the imaging and lab tests, T.F.’s physician suspects an autonomic problem is at the root of his disorder and that surgery will ultimately be an important part of the treatment. Case B A developmental abnormality involving the neural crest has lead to serious difficulties in the lower gastrointestinal tract for newborns like J.G. This disorder involves the autonomic/enteric nervous systems and is one of the most common congenital anorectal malformations (1/5,500 births, four times more frequent in males). Neural crest may have failed to migrate toward the developing colon and rectum. Alternatively, neural crest cells reached the colon but failed to survive and differentiate. As a result, enteric neurons in one or more of the plexuses are missing along a variable section of the distal GI tract. Extrinsic (sympathetic and parasympathetic) inputs to the colon and rectum proliferate. The absence of the enteric neurons and the over-abundance of extrinsic inputs disrupt peristalsis and affect smooth muscle tone. Continuous spasm in the aganglionic segment causes a stenosis and diminished motility; massive distention of the normal proximal colon develops secondarily. There is retention of fecal matter in the distended colon. The untreated disease has a mortality rate as high as 80%. Surgical removal of the aganglionic portion of the GI tract is an important part of the treatment regimen. Case C Several serious and debilitating problems affect R.K., age 67 years. The primary sign of the disorder is orthostatic hypotension. In fact, blood pressure regulation overall is faulty. Sometimes while reclining, R.K.’s blood pressure rises dramatically. R.K. also experience irregular heartbeat, constipation, incontinence and dimished ability to control body temperature. In addition, there are signs such as bradykinesia, rigidity, impaired balance and unsteady gait. R.K. complains of double visison and occassional breathing difficulty. His wife notes that he is becoming more confused. The disease is clearly progressing. Images of the brain suggest atrophy at several points - the basal ganglia, cerebellum and portions of the brain stem. There is no cure for this disorder; management of the symptoms is possible to some degree.