* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 楈瑳汯杯捩污传杲湡穩瑡潩景琠敨䌠牥扥慲潃瑲硥
Cognitive neuroscience wikipedia , lookup
Executive functions wikipedia , lookup
Holonomic brain theory wikipedia , lookup
Microneurography wikipedia , lookup
Affective neuroscience wikipedia , lookup
Persistent vegetative state wikipedia , lookup
Expressive aphasia wikipedia , lookup
Environmental enrichment wikipedia , lookup
Lateralization of brain function wikipedia , lookup
Visual selective attention in dementia wikipedia , lookup
Synaptic gating wikipedia , lookup
Broca's area wikipedia , lookup
Embodied language processing wikipedia , lookup
Aging brain wikipedia , lookup
Dual consciousness wikipedia , lookup
Emotional lateralization wikipedia , lookup
Neuroesthetics wikipedia , lookup
Human brain wikipedia , lookup
Neuroeconomics wikipedia , lookup
Neuroplasticity wikipedia , lookup
Cortical cooling wikipedia , lookup
Eyeblink conditioning wikipedia , lookup
Anatomy of the cerebellum wikipedia , lookup
Premovement neuronal activity wikipedia , lookup
Time perception wikipedia , lookup
Neuroanatomy of memory wikipedia , lookup
Cognitive neuroscience of music wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Motor cortex wikipedia , lookup
Neural correlates of consciousness wikipedia , lookup
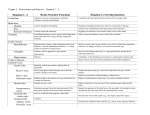
MINISTRY OF HEALTH OF UKRAINE VINNYTSIA NATIONAL MEDICAL UNIVERSITY NAMED AFTER M.I.PIROGOV NEUROLOGY DEPARTMENT Stomatology Faculty Lesson #5 Cerebrum. Cerebral Cortex. Higher Cortical Functions. Consciousness. 1. Goals: 1.1. To study the Anatomical fundamentals of the Cerebral Gray and White Matter. 1.2. To study the Functional peculiarities of the Higher Brain Centers and their anatomical localisations. 1.3. To study the Neurological fundamentals of the Consciousness and its changes in different Neurological conditions. 2. Basic questions: 2.1. Anatomical Fundamentals: 2.1.1. Cerebral cortex. Cortical Layers . 2.1.2. Cerebral White Matter. Fibers. 2.2. Functional Localisations in the Cerebral Cortex: 2.2.1. Primary Somatosensory and Motor Cortical Areas. 2.2.2. Primary Visual Cortex. 2.2.3. Primary Gustatory Cortex. 2.2.4. Primary Vestibular Cortex. 2.2.5. Association Areas. 2.3. Higher Cortical Functions and Their Impairment by Cortical Lesions 2.3.1. Aphasia. 2.3.2. Apraxia. 2.3.3. Agnosia. 2.4. Consciousness. 2.4.1. Morphological and functional substrate of Consciousness. 2.4.2. Impaired Consciousness. Coma. Glasgow Coma Scale. Literature: Mathias Baehr, M.D., Michael Frotscher, M.D. Duus’ Topical Diagnosis in Neurology. – P.349-400 Mark Mumenthaler, M.D., Heinrich Mattle, M.D. Fundamentals of Neurology. – P.39-42. Histological Organization of the Cerebral Cortex The folded surface of the brain is made up of the gray matter of the cerebral cortex, which is gray because of the very high density of neurons within it. The cortex varies in thickness from 1.5mm (visual cortex) to 4.55mm (precentral gyrus); it is generally thicker on the crown of a gyrus than in the depths of the neighboring sulci. The internal structure of the six-layered isocortex is depicted in Fig. 9.12. In an anatomical section perpendicular to the brain surface, the following layers can be distinguished, from outside to inside (i.e., from the pial surface to the subcortical white matter). 1. Molecular layer (zonal layer). This layer is relatively poor in cells. In addition to the distal dendritic trees (apical tuft) of lower-lying pyramidal cells and the axons that make synaptic contact with them, this layer contains mostly small neurons (Cajal-Retzius cells), whose dendrites run tangentially within the layer. The 2. External granular layer. This layer contains many granule cells (“nonpyramidal cells”) and a few pyramidal cells whose dendrites branch out both within the external granular layer and upward into the molecular layer. The nonpyramidal cells are mostly GABAergic inhibitory neurons, while the pyramidal cells are excitatory and use glutamate as their neurotransmitter. 3. External pyramidal layer. As its name implies, this layer contains many pyramidal cells, which, however, are smaller than those of the deeper cortical layers. These cells are oriented with their bases toward the subcortical white matter. 4. Internal granular layer. Like the external granular layer, this layer contains many nonpyramidal cells. These granule cells mainly receive afferent input from thalamic neurons by way of the thalamocortical projection. 5. Internal pyramidal layer. This layer contains medium-sized and large pyramidal cells. The largest cells of this layer (Betz cells) are found only in the region of the precentral gyrus. The especially thickly myelinated neurites of these cells form the corticonuclear and corticospinal tracts. 6. Multiform layer. This layer of polymorph cells is subdivided into an inner, less dense layer containing smaller cells, and an outer layer containing larger cells. Cerebral White Matter Each hemisphere contains a large amount of subcortical white matter, which is composed of myelinated nerve fibers of varying thickness and neuroglia (mainly oligodendrocytes, the cells that form myelin sheaths). The subcortical white matter is bounded by the cerebral cortex, the lateral ventricles, and the striatum. Its nerve fibers are of three types: 1 Projection fibers 2 Association fibers 3 Commissural fibers Projection Fibers Projection fibers connect different parts of the central nervous system with each other over long distances. Association Fibers The association fibers (Figs. 9.15 and 9.16) make up most of the subcortical white matter. These fibers connect neighboring distant cortical areas of the same hemisphere with each other. The cerebral cortex is able to carry out its diverse associative and integrative functions only because all of its functionally important areas are tightly interconnected and neural impulses can travel easily from one cortical area to another. These extensive fiber connections between cortical areas may also be an important anatomical substrate for the partial recovery of function often seen in the aftermath of cortical injury (e. g., after trauma or stroke). Over time, as the individual practices the impaired activities, performance may improve because the corresponding neural impulses have been redirected along the remaining, intact pathways. Commissural Fibers Fibers linking cortical regions with their counterparts in the opposite cerebral hemisphere are called commissural fibers (Fig. 9.16c, d) and are found in the corpus callosum and the anterior commissure. Functional Localization in the Cerebral Cortex A patho-anatomically oriented functional analysis of cortical structures was supplemented, from 1870 onward, by experiments with direct electrical or chemical stimulation of the cerebral cortex, both in animals and in humans. Later techniques, including stereotaxy, electroencephalography, and microelectrode recording of potentials from individual neurons and nerve fibers, yielded ever more detailed functional “maps” of the brain (Fig. 9.17). The original idea of the “localizability” of brain function remains valid after a century and a half of study, especially with respect to the primary cortical areas, described further below. Primary Cortical Fields Primary Somatosensory and Motor Cortical Areas Localization and function. The primary somatosensory cortex (areas 3, 2, and 1, Fig. 9.18) roughly corresponds to the postcentral gyrus of the parietal lobe and a portion of the precentral gyrus. It extends upward onto the medial surface of the hemisphere, where it occupies the posterior portion of the paracentral lobule. The primary somatosensory cortex is responsible for the conscious perception of pain and temperature as well as somatic sensation and proprioception, mainly from the contralateral half of the body and face. Its afferent input is derived from the ventral posterolateral and posteromedial nuclei of the thalamus (Fig. 6.4, p. 266). Even though some sensory stimuli, particularly painful stimuli, may already be vaguely perceived at the thalamic level, more recise differentiation in terms of localization, intensity, and type of stimulus cannot occur until impulses reach the somatosensory cortex. The conscious perception of vibration and position is not possible without the participation of the cortex. The primary motor cortex (area 4) roughly corresponds to the precentral gyrus of the frontal lobe, including the anterior wall of the central sulcus, and extends upward into the anterior portion of the paracentral lobule on the medial surface of the hemisphere. The fifth cortical layer in area 4 contains the characteristic Betz pyramidal cells, which give off the rapidly conducting, thickly myelinated fibers of the pyramidal tract. Area 4 is thus considered the site of origin of voluntary movement, sending motor impulses to the muscles by way of the pyramidal tract and anterior horn cells of the spinal cord. It receives afferent input from other areas of the brain that participate in the planning and initiation of voluntary movement, particularly the ventro-oral posterior nucleus of the thalamus, the premotor areas 6 and 8, and the somatosensory areas. A lesion of the primary somatosensory cortex impairs or abolishes the sensations of touch, pressure, pain, and temperature, as well as two-point discrimination and position sense, in a corresponding area on the opposite side of the body (contralateral hemihypesthesia or hemianesthesia). A lesion in area 4 produces contralateral flaccid hemiparesis. Additional damage of the adjacent premotor area and the underlying fiber tracts is necessary to produce spastic hemiparesis, which reflects the interruption of nonpyramidal as well as pyramidal pathways. Focal epileptic seizures restricted to the somatosensory cortex are characterized by repetitive motor phenomena, such as twitching, or by paresthesia/dysesthesia on the opposite side of the body or face (motor or sensory jacksonian seizures). Primary Visual Cortex Localization and retinotopy. The primary visual cortex corresponds to area 17 of the occipital lobe (Figs. 9.17, 9.18). It is located in the depths of the calcarine sulcus, and in the gyri immediately above and below this sulcus on the medial surface of the hemisphere, and it extends only slightly beyond the occipital pole. It is also called the striate (“striped”) cortex because of the white stripe of Gennari, which is grossly visible within it in a perpendicular anatomical section. The visual cortex receives input by way of the optic radiation from the lateral geniculate body, in orderly, retinotopic fashion: the visual cortex of one side receives visual information from the temporal half of the ipsilateral retina and the nasal half of the contralateral retina. Thus, the right visual cortex subserves the left half of the visual field, and vice versa. Visual information from the macula lutea is conveyed to the posterior part of area 17, i.e., the area around the occipital pole. A unilateral lesion of area 17 produces contralateral hemianopsia; a partial lesion produces quadrantanopsia in the part of the visual field that corresponds to the site of the lesion. Central vision is unimpaired as long as the lesion spares the posterior end of the calcarine fissure at the occipital pole. Primary Auditory Cortex Localization. The primary auditory cortex is located in the transverse gyri of Heschl (area 41), which form part of the upper surface of the superior temporal gyrus (Figs. 9.17, 9.18). It receives its afferent input from the medial geniculate body, which, in turn, receives auditory impulses from both organs of Corti byway of the lateral lemnisci. Thus, the primary auditory cortex of each side processes impulses arising in both ears (bilateral projection). Unilateral lesions of the primary auditory cortex cause only subtle hearing loss because of the bilateral projections in the auditory pathway. The impairment mainly concerns directed hearing, and the ability to distinguish simple from complex sounds of the same frequency and intensity. Primary Gustatory Cortex Taste-related impulses are processed first in the rostral nucleus of the tractus solitarius in the brainstem and then conducted, by way of the central tegmental tract, to a relay station in the ventral posteromedial nucleus of the thalamus (parvocellular part). They then travel onward through the posterior limb of the internal capsule to the primary gustatory cortex, which is located in the pars opercularis of the inferior frontal gyrus, ventral to the somatosensory cortex and above the lateral sulcus (area 43, Fig. 9.18). Primary Vestibular Cortex Neurons of the vestibular nuclei in the brainstem project bilaterally to the ventralposterolateral and posteroinferior nuclei of the thalamus, as well as to its posterior nuclear group near the lateral geniculate body. Vestibular impulses are conducted from these sites to area 2v in the parietal lobe, which lies at the base of the intraparietal sulcus, directly posterior to the hand and mouth areas of the postcentral gyrus. Electrical stimulation of area 2v in humans induces a sensation of movement and vertigo. Area 2v neurons are excited by head movement. They receive visual and proprioceptive as well as vestibular input. Another cortical area receiving vestibular input is area 3a, at the base of the central sulcus adjacent to the motor cortex. The function of area 3a neurons is probably to integrate somatosensory, special sensory, and motor information for the control of head and body position. Large lesions of area 2v in humans can impair spatial orientation. Association Areas Unimodal Association Areas The unimodal association areas of the cortex are located next to the primary cortical areas. Their function, in very general terms, is to provide an initial interpretation of the sensory impulses that are processed in relatively raw form in the primary cortical areas. Sensory information transmitted to the association areas is compared with previously stored information, so that a meaning can be assigned to it. The visual association areas are areas 18 and 19 (Fig. 9.18), which are adjacent to the primary visual cortex (area 17). These areas receive relatively basic visual information from area 17 and use it to perform a higher-level analysis of the visualworld. The somatosensory association cortex lies just behind the primary somatosensory cortex in area 5, and the auditory association cortex is part of the superior temporal gyrus (area 22) (Fig. 9.18). The unimodal association areas receive their neural input through association fibers from the corresponding primary cortical fields. They receive no direct input from the thalamus. Multimodal Association Areas Unlike the unimodal association areas, the multimodal association areas are not tightly linked to any single primary cortical field. They make afferent and efferent connections with many different areas of the brain and process information from multiple somatosensory and special sensory modalities (Fig. 9.26). They are the areas in which motor and linguistic concepts are first drafted, and in which neural representations are formed that do not directly depend on sensory input. The largest multimodal association area is the multimodal portion of the frontal lobe (to be described further below), accounting for 20% of the entire neocortex. Another important multimodal association area is found in the posterior portion of the parietal lobe. While the anterior portion of the parietal lobe processes somatosensory information (areas 1, 2, 3, and 5), its posterior portion integrates somatosensory with visual information to enable the performance of complex movements. Frontal Lobe The frontal lobe can be divided into three major components: the primary motor cortex (area 4), which has already been described, the premotor cortex (area 6), and the prefrontal region, a large expanse of cortex consisting of multimodal association areas (Fig. 9.18). The primary motor cortex and the premotor cortex form a functional system for the planning and control of movement. The prefrontal cortex is primarily concerned with cognitive tasks and the control of behavior. Premotor cortex. The premotor cortex (area 6) is a higher-order center for the planning and selection of motor programs, which are then executed by the primary motor cortex. Just as the unimodal association areas adjacent to the primary somatosensory, visual, and auditory cortices are thought to store sensory impressions, so too the premotor cortex is thought to store learned motor processes, acting in cooperation with the cerebellum and basal ganglia. The stored “motor engrams” can be called up again for use as needed. Even tasks performed with a single hand activate the premotor cortex of both hemispheres. Another important function of the premotor cortex is the planning and initiation of eye movements by the frontal eye fields (area 8; Figs. 9.17, 9.18, and 9.21). Unilateral stimulation of area 8 induces conjugate movement of both eyes to the opposite side. Lesions of area 8 that diminish its activity produce conjugate gaze deviation to the side of the lesion through the preponderant activity of the contralateral area 8 (deviation conjugate, e. g., in stroke—“the patient looks toward the lesion”). Higher Cortical Functions and Their Impairment by Cortical Lesions Aphasia Language is one of the more important and complex activities of the human brain. In most individuals (ca. 95%), language-related areas are located in the frontal and temporoparietal association cortices of the left hemisphere, which is usually contralateral to the dominant (right) hand. Some important aspects of language, however, including its emotional (affective) component, are subserved by the right hemisphere. The major speech centers are in the basal region of the left frontal lobe (Broca’s area, area 44) and in the posterior portion of the temporal lobe at its junction with the parietal lobe (Wernicke’s area, area 22) (Fig. 9.26). These areas are spatially distinct from the primary sensory and motor cortical areas responsible for purely auditory perception (auditory cortex, transverse gyri of Heschl), purely visual perception (visual cortex), and the motor performance of the act of speaking (primary motor cortex). Broca’s area is activated when an individual speaks, and even during “silent speech,” i.e., when words and sentences are formulated without actually being spoken. Pure word repetition, on the other hand, is associated with activation in the insula. Wernicke’s area is primarily concerned with the analysis of heard sounds that are classified as words. Aphasia. A disturbance of language function is called aphasia (different subtypes of aphasia are sometimes collectively termed “the aphasias”). Some types of aphasia exclusively affect speech, writing (dysgraphia or agraphia), or reading (dyslexia or alexia). Aphasia is distinct from impairment of the physical act of speaking, which is called dysarthria or anarthria (caused, for example, by lesions of the pyramidal tract, cerebellar fiber pathways, the brainstem motor neurons innervating the muscles of speech, e. g., in bulbar paralysis, or the muscles themselves). Dysarthria and anarthria affect articulation and phonation, i.e., speech, rather than language production per se (grammar, morphology, syntax, etc.). Aphasia is called fluent or nonfluent, depending on whether the patient speaks easily and rapidly, or only hesitantly and with abnormal effort. The more important types of aphasia, their distinguishing features, and their cortical localization are summarized in Table 9.1. Global aphasia involves all aspects of language and severely impairs spoken communication. The patient cannot speak spontaneously or can only do so with great effort, producing no more than fragments of words. Speech comprehension is usually absent; at best, patients may recognize a few words, including their own name. Perseveration (persistent repetition of a single word/subject) and neologisms are prominent, and the ability to repeat heardwords is markedly impaired. Patients have great difficulty naming objects, reading, writing, and copying letters or words. Their ability to name objects, read, and write, except for the ability to copy letters of the alphabet or isolated words, is greatly impaired. Language automatism (repetition of gibberish) is a characteristic feature. Site of lesion: Entire distribution of the middle cerebral artery, including both Broca’s and Wernicke’s areas. Broca’s aphasia (also called anterior, motor, or expressive aphasia) is characterized by the absence or severe impairment of spontaneous speech, while comprehension is only mildly impaired. The patient can speak only with great effort, producing only faltering, nonfluent, garbled words. Phonemic paraphasic errors are made, and sentences are of simple construction, often with isolated words that are not grammatically linked (agrammatism, “telegraphic” speech). Naming, repetition, reading out loud, and writing are also impaired. Site of lesion: Broca area; may be due to infarction in the distribution of the prerolandic artery (artery of the precentral sulcus). Wernicke’s aphasia (also called posterior, sensory, or receptive aphasia) is characterized by severe impairment of comprehension. Spontaneous speech remains fluent and normally paced, but paragrammatism, paraphasia, and neologisms make the patient’s speech partially or totally incomprehensible (word salad, jargon aphasia). Naming, repetition of heard words, reading, and writing are also markedly impaired. Site of lesion: Wernicke’s area (area 22). May be due to infarction in the distribution of the posterior temporal artery. Transcortical aphasia. Heard words can be repeated, but other linguistic functions are impaired: spontaneous speech in transcortical motor aphasia (syndrome similar to Broca’s aphasia), language comprehension in transcortical sensory aphasia (syndrome similar to Wernicke’s aphasia). Site of lesion: Motor type, left frontal lobe bordering on Broca’s area; sensory type, left temporo-occipital junction dorsal to Wernicke’s area. Watershed infarction is the most common cause. Amnestic (anomic) aphasia. This type of aphasia is characterized by impaired naming and word finding. Spontaneous speech is fluent but permeated with word-finding difficulty and paraphrasing. The ability to repeat, comprehend, and write words is essentially normal. Site of lesion: Temporoparietal cortex or subcortical white matter. Conduction aphasia. Repetition is severely impaired; fluent, spontaneous speech is interrupted by pauses to search for words and by phonemic paraphasia. Language comprehension is only mildly impaired. Site of lesion: Arcuate fasciculus or insular region. Agraphia Agraphia. Agraphia is the acquired inability to write. Agraphia may be isolated (due to a lesion located in area 6, the superior parietal lobule, or elsewhere) or accompanied by other disturbances: aphasic agraphia is fluent or nonfluent, depending on the accompanying aphasia; apraxic agraphia is due to a lesion of the dominant parietal lobe; spatial agraphia, in which the patient has difficulty writing on a line and only writes on the right side of the paper, is due to a lesion of the nondominant parietal lobe; alexia with agraphia may be seen in the absence of aphasia. Micrographia (abnormally small handwriting) is found in Parkinson disease and is not pathogenetically related to agraphia. Various forms of agraphia are common in Alzheimer disease. Examination: The patient is asked to write sentences, long words, or series of numbers to dictation, to spell words, and to copy written words. Alexia Alexia. Alexia is the acquired inability to read. In isolated alexia (alexia without agraphia), the patient cannot recognize entire words or read them quickly, but can decipher them letter by letter, and can understand verbally spelled words. The ability to write is unaffected. The responsible lesion is typically in the left temporooccipital region with involvement of the visual pathway and of callosal fibers. Anterior alexia (difficulty and errors in reading aloud; impaired ability to write, spell, and copy words) is usually associated with Broca’s aphasia. Central alexia (combination of alexia and agraphia) is usually accompanied by right-left disorientation, finger agnosia, agraphia, and acalculia (Gerstmann syndrome; lesions of the angular and supramarginal gyri), or by Wernicke’s aphasia. Other features include the inability to understand written language or to spell, write, or copy words. Examination: The patient is asked to read aloud and to read individual words, letters, and numbers; the understanding of spelled words and instructions is tested. Acalculia Acalculia. Acalculia is an acquired inability to use numbers or perform simple arithmetical calculations. Patients have difficulty counting change, using a thermometer, or filling out a check. Lesions of various types may cause acalculia. Examination: The patient is asked to perform simple arithmetical calculations and to read numbers. Apraxia Apraxia, in general, is a complex disturbance of voluntary movement that does not result from weakness or other dysfunction of the primary motor areas, or from the patient’s lack of motivation or failure to comprehend the task. It manifests itself as an inability to combine individual, elementary movements into complex movement sequences, or to assemble these sequences themselves into still higher-order motor behaviors. The individual movements themselves, however, can still be carried out. Motor apraxia. A patient with severe motor apraxia cannot execute basic sequences of movements, such as reaching out and grasping an object, even though isolated testing of the individual muscle groups involved reveals no weakness in the arm or hand. Ideomotor apraxia results from lesions of the language-dominant (left) hemisphere, either in the motor association areas or in the association and commissural fibers by which they are innervated and interconnected. A typical clinical finding is the omission, or premature termination, of individual components of a sequence of movements. Individual components can also be unnecessarily repeated (motor perseveration), so that they start at inappropriate times and thereby impede or interrupt the course of the next movement. Patients with motor apraxia whose lesions lie in the parietal lobe cannot correctly imitate the examiner’s movements (e. g., a military salute). These patients can often still copy facial expressions, while patients with left frontal lobe lesions can copy complex arm movements, but not facial expressions. Ideational apraxia. In this rarer type of apraxia, a temporoparietal lesion in the language-dominant (left) hemisphere impairs the planning and initiation of complex motor activities. The patient remains able, in principle, to carry out a complex sequence of movements, but seems not to comprehend its meaning or purpose. The patient either fails to initiate the movement or terminates it prematurely. Construction apraxia. Patients with construction apraxia have difficulty drawing spatial constructions such as geometrical figures or objects. This disturbance usually results from a lesion in the parietal lobe of the non-languagedominant (right) hemisphere. Most apraxic patients are also aphasic. Patients can suffer from ideomotor, ideational, and constructive apraxia simultaneously, depending on the site and extent of the lesion. Agnosia and Neglect The anterior portion of the parietal lobe processes somatosensory signals, while its posterior portion and the visual association cortices are concerned with the integration of somatosensory, visual, and motor information. Complex activities, such as pouring a drink while carrying on a conversation, require the simultaneous integration of many different perceptual and motor processes: the objects handled (glass, bottle) must be recognized, which requires conjugate eye movements and visual processing; reaching, grasping, and pouring movements must be smoothly executed; and, at the same time, language must be heard, understood, formulated, and spoken. In order to perform these tasks, the brain needs internal representations of the body, information about the positions of the limbs, and a conception of the outside world. These representations must, in turn, be linked to incoming visual and auditory signals, and to the brain’s plans for intended movement. The association cortices and the posterior portion of the parietal lobe play an essential role in these complex integrative processes. As an illustration of this role, the posterior portion of the parietal lobe is activated not only by intended grasping movements induced by visual stimuli, but also by palpation of an unseen object. Lesions of the visual association cortices and the parietal lobe can produce many different types of agnosia, i.e., complex disturbances of perception. A patient with agnosia cannot recognize objects or spatiotemporal contexts despite intact primary perception (normal vision, hearing, and somatic sensation) and motor function (absence of weakness). Agnosia can be visual, auditory, somatosensory, or spatial. Visual object agnosia. If the visual association areas are damaged, the patient can still comprehend the spatial structure of familiar objects, but can no longer identify them. A bottle, for example, can be correctly drawn, but cannot be identified as a bottle. Other, more complex types of visual agnosia include prosopagnosia (the inability to recognize faces) and alexia (the inability to read). Somatosensory agnosias. Astereognosia is the inability to recognize an object by touch alone, even though sensation is intact and objects can otherwise be named without difficulty. Asomatognosia is a generally diminished, or even absent, ability to perceive one’s own body. Gerstmann syndrome consists of the inability to name one’s own fingers (finger agnosia) along with an impairment of writing (dysgraphia or agraphia), calculation (dyscalculia or acalculia), and the ability to distinguish right from left. Gerstmann first described these findings in 1924 in a patient with an ischemic stroke in the territory of the middle cerebral artery affecting the left parietal lobe. Neglect. Patients sometimes pay less attention to the side of the body or visual field opposite a cortical lesion, or ignore it altogether; this is called neglect. There is often an accompanying unawareness of the deficit (anosognosia). Neglect usually involves vision, hearing, somatic sensation, spatial perception, and movement simultaneously. The causative lesion is usually in the parietal lobe of the non-languagedominant (right) hemisphere. A patient with motor neglect moves one side of the body very little, or not at all, even though it is not paralyzed. Normal and Impaired Control of Behavior, Including Social Behavior Prefrontal cortex. Cognition and the control of behavior are the main functions of the multimodal association areas in the frontal lobe that constitute the prefrontal cortex (Fig. 9.18). Experimental electrical stimulation of the prefrontal cortex does not induce any motor response. This portion of the frontal lobe is extraordinarily enlarged in primates, and particularly in humans; thus, it has long been presumed to be the seat of higher mental functioning. The frontal cortical fields make reciprocal connections with the medial nucleus of the thalamus, through which they receive input from the hypothalamus. They also make very extensive connections with all other areas of the cerebral cortex. The task of the prefrontal cortex is the rapid storage and analysis of objective and temporal information. The dorsolateral prefrontal cortex plays an essential role in the planning and control of behavior, and the orbital prefrontal cortex does the same in the planning and control of sexual behavior. Lesions of the prefrontal convexity. Patients with bilateral prefrontal lesions can barely concentrate on a task and are extremely easy to distract with any new stimulus. They can carry out complex tasks only in part, or not at all. They have no sense of advance planning and take no account of future events or of possible problems in the execution of a task. They often stick rigidly to an idea and fail to adapt to changing circumstances. In extreme cases, they manifest perseveration, i.e., they perform the same task again and again, always with the same mistakes. This deficit is strikingly brought out by the Wisconsin Card Sorting Test, in which the patient sorts cards bearing various symbols and colors according to some criterion (e. g., shape), after seeing the examiner do so. Performance in the first round is usually relatively normal. The examiner confirms the patient’s success, then changes the sorting criterion (e. g., to color) without explicitly saying so. A patient with a prefrontal lesion realizes about as rapidly as a normal individual that the task has changed, yet keeps sorting according to the old criterion, despite being immediately informed of each mistake. Markedly reduced drive and lack of spontaneity are also characteristic clinical signs of prefrontal dysfunction. These deficits are revealed by very poor performance on the Word Fluency Test, in which the patient is given a short period of time to say as manywords as possible that begin with a particular letter of the alphabet. Patients with prefrontal lesions do badly despite relatively normal verbal memory. They do badly on nonverbal tests as well: normal subjects can draw about 35 pictures in five minutes, patients with left frontal lesions 24, patients with right frontal lesions 15. Because they lack spontaneity in all forms of communication, these patients seem lazy, lethargic, and unmotivated. They neglect many activities of daily life, spend the morning in bed, fail to wash or groom themselves or to get dressed without help, and do no regular work. Nonetheless, their formal IQ and long-term memory are largely intact! Fronto-orbital lesions. Social and sexual behavior are controlled and regulated by highly complex processes. Behavior of these types, too, is abnormal in patients with frontal lobe lesions. Fronto-orbital lesions, in particular, produce two characteristic types of personality disturbance. Pseudo-depressive patients are apathetic and indifferent and display markedly reduced drive, diminished sexual desire, and little or no variation in their emotional state. Pseudo-psychopathic patients, on the other hand, are hypomanic and restless in their movements, fail to keep an appropriate distance from others, and lack normal kinds of inhibition. They display markedly increased drive and sexual desire. They are unwilling or unable to hold to the same normal conventions of behavior that they followed unquestioningly before becoming ill. Consciousness Consciousness is an active processwith multiple individual components, including wakefulness, arousal, perception of oneself and the environment, attention, memory, motivation, speech, mood, abstract/logical thinking, and goaldirected action. Clinical assessment of consciousness tests the patients’ perception of themselves and their environment, behavior, and responses to external stimuli. Findings are expressed in terms of three categories: level of consciousness (state/clarity of consciousness, quantitative level of consciousness, vigilance, alertness, arousability); content of consciousness (quality of consciousness, awareness); and wakefulness. Changes in any of these categories tend to affect the others aswell. Morphologically, the level of consciousness is associated with the reticular activating system (RAS). This network is found along the entire length of the brain stem reticular formation, from the medulla to the intralaminar nuclei of the thalamus. The RAS has extensive bilateral projections to the cerebral cortex; the cortex also projects back to the RAS. Neurotransmission in these systems is predominantly with acetylcholine, monoamines (norepinephrine, dopamine, serotonin), GABA (inhibitory), and glutamate (excitatory). In the normal state of consciousness, the individual is fully conscious, oriented, and awake. All of these categories undergo circadian variation (depending on the time of day, a person may be fully awake or drowsy, more or less concentrated, with organized or disorganized thinking), but normal consciousness with full wakefulness can always be restored by a vigorous stimulus. Acute Disturbances of Consciousness Confusion affects the content of consciousness - attention, concentration, thought, memory, spatiotemporal orientation, and perception (lack of recognition). It may also be associated with changes in the level of consciousness (fluctuation between agitation and somnolence) and in wakefulness (impaired sleep–wake cycle with nocturnal agitation and daytime somnolence). Delirium is characterized by visual hallucinations, restlessness, suggestibility, and autonomic disturbances (tachycardia, blood pressure fluctuations, hyperhidrosis). Somnolence is a mild reduction of the level of consciousness (drowsiness, reduced spontaneous movement, psychomotor sluggishness, and delayed response to verbal stimuli) while the patient remains arousable: he or she is easily awakened by a stimulus, but falls back asleep once it is removed. The patient responds to noxious stimuli with direct and goal-directed defensive behavior. Orientation and attention aremildly impaired but improve on stimulation. Stupor is a significant reduction of the level of consciousness. These patients require vigorous and repeated stimulation before they open their eyes and look at the examiner. They answer questions slowly and inadequately, or not at all. They may lie motionless or display restless or stereotyped movements. Confusion reflects concomitant impairment of the content of consciousness Disorders of arousal. Wakefulness normally follows a circadian rhythm. Sleep apnea syndrome, narcolepsy, and parasomnia are disorders of arousal. Hypersomnia is caused by bilateral paramedian thalamic infarcts, tumors in the third ventricular region, and lesions of the midbrain tegmentum. The level and content of consciousness may also be affected. In patients with bilateral paramedian thalamic infarction, for example, there may be a sudden onset of confusion, followed by somnolence and coma. After recovery from the acute phase, these patients are apathetic and their memory is impaired (“thalamic dementia”). Coma (from the Greek for “deep sleep”) is a state of unconsciousness in which the individual lies motionless, with eyes closed, and cannot be aroused even by vigorous stimulation. Coma reflects a loss of the structural or functional integrity of the RAS or the areas to which it projects. Coma may be produced by an extensive brain stem lesion or by extensive bihemispheric cerebral lesions, as well as by metabolic, hypoxic/ischemic, toxic, or endocrine disturbances. In the syndrome of transtentorial herniation, a large unihemispheric lesion can cause coma by compressing the midbrain and the diencephalic RAS. Even without herniation, however, large unihemispheric lesions can transiently impair consciousness. Coma Staging The degree of impairment of consciousness is correlated with the extent of the causative lesion. The severity and prognosis of coma are judged from the patient’s response to stimuli. There is no universally accepted grading system for coma. Proper documentation involves an exact description of the stimuli given and the responses elicited, rather than isolated items of information such as “somnolent” or “GCS 10.” Coma scales (e. g., the Glasgow Coma Scale) are useful for the standardization of data for statistical purposes but do not replace a detailed documentation of the state of consciousness. Spontaneous movement. Assessment of motor function yields clues to the site of the lesion and the etiology of coma. The examiner should note the pattern of breathing, any utterances, yawning, swallowing, coughing, and movements of the limbs (twitching of the face or hands may indicate epileptic activity; there may be myoclonus or flexion/extension movements). Stimuli. Lesions of the midbrain or lower diencephalon produce the decerebration syndrome (arm/leg extension with adduction and internal rotation of the arms, pronation and flexion of the hands), while extensive bilateral lesions at higher levels produce the decortication syndrome (arm/hand flexion, arm supination, leg extension). These pathological flexion and extension movements occur spontaneously or in response to external stimuli (verbal stimulation, tickling around the nose, pressure on the knuckles or other bones) whether the cause of coma is structural or metabolic. Withdrawal of the limb from the stimulus usually means that the pyramidal pathway for the affected limb is intact. Stereotyped flexion or extension movements are usually seen in patients with severe damage to the pyramidal tract. Brainstem reflexes. Structural lesions of the brain stem usually impair the function of the internal and external eye muscles, while supratentorial lesions generally do not, unless they secondarily affect the brain stem. Coma in a patient with intact brainstemreflexes is likely to be due to severe bihemispheric dysfunction (if no further objective deficit is found, coma may be psychogenic or factitious). Physicians should be aware that coma due to intoxication or drug overdose may be difficult to distinguish from that due to structural damage by clinical examination alone. Preservation of the vestibulo-ocular reflex (VOR) and of the doll’s eyes reflex is compatible with either a bihemispheric lesion or a toxic or metabolic disorder. The VOR induces conjugate eye movement only if its brain stem pathway is intact (from the cervical spinal cord to the oculomotor nucleus). Nonetheless, the VOR may be absent in some cases of toxic coma (due to, e. g., alcohol, barbiturates, ). Abnormalities of the respiratory pattern are of limited localizing value. Cheyne–Stokes respiration is characterized by regular waxing and waning of the tidal volume, punctuated by apneic pauses. It has a number of causes, including bihemispheric lesions and metabolic disorders. Slow, shallow respiration usually reflects a metabolic or toxic disorder. Rapid, deep respiration (Kussmaul’s respiration) usually reflects a pontine or mid brain lesion, or metabolic acidosis. Medullary lesions and extensive supratentorial damage produce ataxic, cluster, or gasping respiration.