* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Medical Biochemistry Review #2 By
Basal metabolic rate wikipedia , lookup
Gaseous signaling molecules wikipedia , lookup
Ultrasensitivity wikipedia , lookup
Metalloprotein wikipedia , lookup
Signal transduction wikipedia , lookup
Enzyme inhibitor wikipedia , lookup
Lipid signaling wikipedia , lookup
Photosynthesis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Lactate dehydrogenase wikipedia , lookup
Mitogen-activated protein kinase wikipedia , lookup
Paracrine signalling wikipedia , lookup
Photosynthetic reaction centre wikipedia , lookup
Biosynthesis wikipedia , lookup
Mitochondrion wikipedia , lookup
Nicotinamide adenine dinucleotide wikipedia , lookup
Blood sugar level wikipedia , lookup
Biochemical cascade wikipedia , lookup
Microbial metabolism wikipedia , lookup
Light-dependent reactions wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Electron transport chain wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
NADH:ubiquinone oxidoreductase (H+-translocating) wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Biochemistry wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
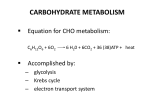
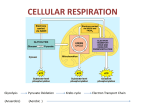
Medical Biochemistry Review #2 By Jason Elmer [email protected] Obi Ekwenna [email protected] YOUR EXAM • • • • • Lectures 14-24 ~44 questions (4 questions per lecture) Take a calculator to the exam Exam on Monday October 4th. DO THE STUDY QUESTIONS; if nothing else read the answers!!!!!!!!!! • Of course TLEs are highly recommended! It is impossible to memorize every possible bit of biochemistry trivia. ‘They’ simply know way too much about metabolism for a single person to be able to regurgitate it all. • Do not rely on passive reading and highlighting/underlining of the textbook. • Do not sit and stare at the handouts • Do not try to read 50 review books. (Make your own review book instead!) • Do focus on identifying key concepts • Do actively draw and redraw pathways and connections • Do learn to identify relevant information Do prioritize: • • • • • • What is the purpose of a pathway? What are the starting and ending molecules? Where is the pathway (in the cell, in a tissue, in an organ system)? How does the pathway connect to other pathways? What metabolic conditions turn the pathway on and off? What are the control points for regulating the pathway? – reactants, products and enzyme name of each regulatory step – additional regulatory molecules involved (vitamins, cofactors) – make sure you know every step that makes or uses ATP • What structural features are important for the function and interaction of specific regulatory molecules in a pathway? • What biochemical techniques are used to study these pathways? • What specific drugs or diseases associated with the pathway? METABOLIC PATHWAYS • • • • • • • • Glycolysis Gluconeogenesis Citric Acid Cycle (Krebs Cycle) Glycogen Metabolism Hexose Interconversions Electron Transport Chain Oxidative Phosphorylation Pentose-Phosphate Shunt GLYCOLYSIS • Oxidation of glucose is known as Glycolysis. – Either AerobicPyruvate – Anaerobic Lactic Acid – Occurs in the Cytosol Overall Rxn: Glucose + 2 ADP + 2 NAD+ + 2 Pi 2 Pyruvate + 2 ATP + 2 NADH + 2 H+ NADH generated during glycolysis is used to fuel mitochondrial ATP synthesis via oxidative phosphorylation. Does not pass through mitochondrial membrane 2 ATP generated glycerol phosphate shuttle 3 ATP generated malate-aspartate shuttle If used to transport the electrons from cytoplasm NADH into the mitochondria. Key Reactions • Hexokinase – Found in the cytosol of most tissues – Low specificity: it’s a “hoe” for hexoses – Low Km: high affinity for glucose – Inhibited by Glucose-6-phosphate Glucokinase: Found in the Liver and pancreatic b cells Also a ‘hexokinase’ High specificity for glucose High Km inhibited by fructose-6-phosphate Regulation of Glycolysis • Hexokinase, PFK-1 and PK all proceed with a relatively large free energy decrease. These nonequilibrium reactions of glycolysis would be ideal candidates for regulation of the flux through glycolysis. • Hexokinase is not key because of G6P is generated by glycogenolysis • PK reaction is reversed in Gluconeogenesis • Therefore rate limiting step in glycolysis is the reaction catalyzed by PFK-1. • PFK-1 is a tetrameric enzyme that exist in two conformational states termed R and T that are in equilibrium. • ATP is both a substrate and an allosteric inhibitor of PFK-1. F6P is the other substrate for PFK-1 and it also binds preferentially to the R state enzyme. ATP binds the T state. • The inhibition of PFK-1 by ATP is overcome by AMP which binds to the R state of the enzyme and, therefore, stabilizes the conformation of the enzyme capable of binding F6P. • The most important allosteric regulator of both glycolysis and gluconeogenesis is fructose 2,6bisphosphate, F2,6BP, which is not an intermediate in glycolysis or in gluconeogenesis. • Also important to note that Insulin/Glucagon ratio i.e. fed/starve state, regulate Pyruvate Kinase activity. The last enzyme in the pathway. • Glucagon: high in starvation, b/cos blood glucose levels are low, therefore it favors gluconeogenesis in Liver. • Insulin: on the contrary favors glycolysis. Glycolysis Glycolysis • Key points about the Shuttle System: – Malate-Asparate shuttle is the primary system – By default Glycerol shuttle is secondary • Two enzymes are involved in this shuttle: 1.cytosolic version of the enzyme glycerol-3-phosphate dehydrogenase (glycerol-3-PDH) which has as one substrate, NADH. 2.mitochondrial form of the enzyme which has as one of its' substrates, FAD+. Since the electrons from mitochondrial FADH2 feed into the oxidative phosphorylation pathway at coenzyme Q (as opposed to NADH-ubiquinone oxidoreductase [complex I]) only 2 moles of ATP will be generated from glycolysis. G3PDH is glyceraldehyde-3-phoshate dehydrogenase. Glycolysis • Malate -Asp Shuttle – The electrons are "carried" into the mitochondria in the form of malate. Cytoplasmic malate dehydrogenase (MDH) reduces oxaloacetate (OAA) to malate while oxidizing NADH to NAD+ – Cytoplasmic malate dehydrogenase (MDH) reduces oxaloacetate (OAA) to malate while oxidizing NADH to NAD+. – Malate then enters the mitochondria where the reverse reaction is carried out by mitochondrial MDH – mitochondrial OAA goes to the cytoplasm to maintain this cycle ; must be transaminated to aspartate (Asp) with the amino group being donated by glutamate (Glu). The Asp then leaves the mitochodria and enters the cytoplasm. The deamination of glutamate generates a-ketoglutarate (a-KG) which leaves the mitochondria for the cytoplasm. – When the energy level of the cell rises, the rate of mitochondrial oxidation of NADH to NAD+ declines and therefore, the shuttle slows. • The synthesis of F2,6BP is catalyzed by the bifunctional enzyme phosphofructokinase-2/fructose-2,6bisphosphatase (PFK-2/F-2,6-BPase). • In the nonphosphorylated form the enzyme is known as PFK-2 and serves to catalyze the synthesis of F2,6BP by phosphorylating fructose 6-phosphate. • The result is that the activity of PFK-1 is greatly stimulated and the activity of F-1,6-BPase is greatly inhibited. More glycolysis! • When the bifunctional enzyme is phosphorylated it no longer exhibits kinase activity, but a new active site hydrolyzes F2,6BP to F6P and inorganic phosphate. • This enzyme is regulated by ProteinKinase A, which is a cyclic AMP dependent enzyme. cAMP is generated depending on the hormonal changes in the body. Eg. With Glucagon, high cAMP thus PKA is active thus less glycolysis. • In addition to these Pyruvate Kinase is activated by F1,6BP and inhibited by ATP. G l u c o n e o genesis Substrates for Gluconeogenesis: Lactate, pyruvate, glycerol, propionny-CoA and certain Amino Acids but never FAT!!! •The Cori cycle involves the utilization of lactate, produced by glycolysis in nonhepatic tissues, (such as muscle and erythrocytes) as a carbon source for hepatic gluconeogenesis. In this way the liver can convert the anaerobic byproduct of glycolysis, lactate, back into more glucose for reuse by non-hepatic tissues. Note that the gluconeogenic leg of the cycle (on its own) is a net consumer of energy, costing the body 4 moles of ATP more than are produced during glycolysis. Therefore, the cycle cannot be sustained indefinitely. The glucose-alanine cycle is used primarily as a mechanism for skeletal muscle to eliminate nitrogen while replenishing its energy supply. Glucose oxidation produces pyruvate which can undergo transamination to alanine. This reaction is catalyzed by glutamate-pyruvate transaminase, GPT (also called alanine transaminase, ALT in Figure). • Regulation of Gluconeogenesis • See regulation of Glycolysis via F2,6 P • Do not forget Hormonal regulations: Insulin and Glucagon • Other things to keep in mind – Pyruvate carboxylase is present in mitochondria, requires Biotin as a cofactor to convert Pyruvate OAA – MDH present in mitochondria, OAA to malate, then MDH present in cytosol converts malate back to OAA – OAA is then converted to PEP, as shown in the previous slide. Pyruvate Carboxylase: inhibited by ADP and activated Acetyl CoA PEP Carboxykinase in the cytosol is inhibited by ADP TCA /Citric Acid/KREBS Cycle • The cycle is located in the mitochondria • All cells have a mitochondria except RBCs • This is the Final common pathway of oxidative metabolism • Acetyl coenzyme A condenses with OAA to begin the cycle. Catabolism of CHO, Fats and Proteins provide the acetyl CoA • The bulk of ATP used by many cells to maintain homeostasis is produced by the oxidation of pyruvate in the TCA cycle • During this oxidation process, reduced NADH and reduced FADH2 are generated. The NADH and FADH2 are principally used to drive the processes of oxidative phosphorylation, which are responsible for converting the reducing potential of NADH and FADH2 to the high energy phosphate in ATP The PDH complex requires 5 different coenzymes: CoA, NAD+, FAD+, lipoic acid and thiamine pyrophosphate (TPP) . Three of the coenzymes of the complex are tightly bound to enzymes of the complex (TPP, lipoic acid and FAD+) and two are employed as carriers of the products of PDH complex activity (CoA and NAD+). pyruvate + CoA + NAD+ CO2 + acetyl-CoA + NADH + H+ The TCA cycle showing enzymes, substrates and products. The abbreviated enzymes are: IDH = isocitrate dehydrogenase and a-KGDH = a-ketoglutarate dehydrogenase. The GTP generated during the succinate thiokinase (succinyl-CoA synthetase) reaction is equivalent to a mole of ATP by virtue of the presence of nucleoside diphosphokinase. The 3 moles of NADH and 1 mole of FADH2 generated during each round of the cycle feed into the oxidative phosphorylation pathway. Each mole of NADH leads to 3 moles of ATP and each mole of FADH2 leads to 2 moles of ATP. Overall Stoichiometry of TCA • • acetyl-CoA + 3NAD+ + FAD + GDP + Pi + 2H2O ----> 2CO2 + 3NADH + FADH2 + GTP + 2H+ + HSCoA The GTP generated by Succinyl CoA SYNTHETASE IS VIA SUBSTRATE LEVEL PHOSPORYLATION. • Regulation of TCA: Regulation of the TCA cycle like that of glycolysis, occurs at both the level of entry of substrates into the cycle as well as at the key reactions of the cycle. Fuel enters the TCA cycle primarily as acetyl-CoA. The generation of acetyl-CoA from carbohydrates is a major control point of the cycle. This is the reaction catalyzed by the PDH complex – PDH complex is inhibited by acetyl-CoA, ATP, and NADH – PDH activated by non-acetylated CoA (CoASH) and NAD+. – The pyruvate dehydrogenase activities of the PDH complex are regulated by their state of phosphorylation. This modification is carried out by a specific kinase (PDH kinase) and the phosphates are removed by a specific phosphatase (PDH phosphatase). – The phosphorylation of PDH inhibits its activity which leads to decreased oxidation of pyruvate. – PDH kinase is activated by NADH and acetyl-CoA and inhibited by pyruvate, ADP, CoASH, Ca2+ and Mg2+. The PDH phosphatase, in contrast, is activated by Mg2+ and Ca2+ Citrate Synthase: inhibited by ATP and citrate Isocitrate Dehydrogenase: Isocitrate, AMP, ADP activates, ATP and NADH inhibits A-ketoglutarate dehydrogenase: succinoyl CoA and NADH inhibits CindyIsKinkySoSheFornicatesMoreOften ELECTRON TRANSPORT AND OXIDATIVE PHOSPHORYLATION • Each turn of TCA cycle generates 3NADH and 1 FADH2 • Electron transport and oxophos occurs in the mitochondria • NADH and FADH2 ultimately pass electrons to O2 and produce H2O. – NADH + (1/2)O2 + H+ -->NAD+ + H2O ~ -52.6kcal/mol – ADP + PATP ~ +7.3kcal/mol – Energy from NADH can be used to drive synthesis of ATP several times. Important again to remember this is an oxidation-reduction reaction thus our friend Nerst is back: DeltaG' = -nFDE' Electron Transport is coupled to Oxidative Phosphorylation • The idea of coupling is explained by Mitchell’s CHEMIOSMOTIC HYPOTHESIS – Basically coupling electron flow through the ETC to ATP synthesis – The Respiratory complexes are proton pumps. As electrons pass through complexes I, III, and IV, hydrogen ions are pumped across the inner mitochondrial membrane into the intermembrane space. – The proton concentration in the intermembrane space increases relative to the mitochondrial matrix – This generates a proton-motive force as a result of 2 factors: 1) Difference in pH and 2) Difference in electrical potential, delta si, between intermembrane space and the mitochondrial matrix. – ATP synthetase complex (complex V): Hydrogen ions pass back into the matrix through V, this drives ATP synthesis. • NADH 3ATP • FADH2 2 ATP: note bypass of Complex 1 ATP synthesized in the matrix is transported out of the matrix via an ATP/ADP translocase (an antiport) also coupled to proton motive force. Inhibitors of Oxidative Phosphorylation • • • • • • • • • • • Rotenone: e- transport inhibitor Complex I Amytal: e- transport inhibitor Complex I Antimycin: A e- transport inhibitor Complex III Cyanide: e- transport inhibitor Complex IV Carbon Monoxide: e- transport inhibitor Complex IV Azide e- transport inhibitor Complex IV 2,4,-dinitrophenol: Uncoupling agent transmembrane H+ carrier Pentachlorophenol: Uncoupling agent transmembrane H+ carrier Oligomycin: Inhibits ATP synthase Thermogenin: also an uncoupler, component of brown fat Malonate inhibits Complex II There are others in your handout take a look at them. SOME MORE STUFF • TCA cycle is regulated by the ratio of ADP, Pi/ ATP – Under resting conditions, with a high cell energy charge, the demand for new synthesis of ATP is limited and, although the Proton Motive Force is high, flow of protons back into the mitochondria through ATP synthetase is minimal. When energy demands are increased, such as during vigorous muscle activity, cytosolic ADP rises and is exchanged with intramitochondrial ATP via the transmembrane adenine nucleotide carrier ADP/ATP translocase. Increased intramitochondrial concentrations of ADP cause the Proton Motive Force to become discharged as protons pour through ATP synthetase, regenerating the ATP pool. – The rate of electron transport is dependent on the PMF – ANY BLOCKADE AT ANY POINT IN THE ELECTRON TRANSPORT CHAIN STOPS ATP SYNTHESIS!!!!!!!!! SAMPLE QUESTIONS • Choose the INCORRECT statement concerning the ATP-ADP cycle and the study of bioenergetics in the human body: • a. One half of the ATP-ADP cycle involves the coupling the energy derived from the hydrolysis of the high energy phosphate bonds of ATP to endergonic reactions so that they will occur spontaneously. b. The work that requires energy derived from ATP hydrolysis includes the transport of electrons down the electron transport chain. c. One half of the ATP-ADP cycle involves the generation of ATP that starts with the formation of reduced coenzymes like NADH and FADH2and the ultimate transfer of their electrons to oxygen d. An important part of oxidative phosphorylation and ATP biosynthesis is the generation of an electrochemical gradient across the inner membrane of the mitochondria. Many catabolic reactions, like the TCA cycle and fatty acid oxidation, provide the reduced coenzymes for the start of oxidative phosphorylation and ATP biosynthesis • • • • • Since electron transport and oxidative phosphorylation are tightly coupled, which one of the following mechanisms BEST explains how ADP regulates the rate of electron transport during oxidative phosphorylation? • a. AMP concentrations are increased as ADP concentrations fall • b. Low [ADP] accelerates the Krebs (TCA) cycle reaction rates, thereby providing more NADH to activate electron transport • c. The transmembrane proton gradient is dissipated with low [ADP] • d. The ATP/ADP antiport system is not functional when mitochondrial [ADP] is low • e. Proton translocation across the inner mitochondrial membrane is decreased when ATP-synthase lacks bound ADP and Pi, secondarily retarding electron transport • You isolate mitochondria from a group of patients that present with lactic acidosis and muscle weakness, and show that they are unable to: (1) oxidize reduced coenzyme Q, (2) translocate protons across their mitochondrial membranes to the intennembrane space against a concentration gradient with succinate added as the substrate, and (3) reduce cytochrome c. The biochemical defect in these patients most likely resides in their ... ? • A. Complex I (NADH dehydrogenase) • B. Complex II (succinate-Q reductase) • C. Complex III (cytochrome b-c1) • D. Complex IV (cytochrome oxidase) • E. Complex V (F1F0 ATPase) • Which of the following orderings #1 - #5 of the various components of the electron transport chain and oxidative phosphorylation will effectively allow the development of an electrochemical potential sufficient to drive the generation of high energy phosphate bonds between ADP and Pi? • 1. FMN, NADH dehydrogenase, ubiquinone, cytochrome c, cytochrome oxidase, F1F0-ATPase • 2. Complex I, Complex III, ubiquinone, cytochrome a1-a3, cytochrome c, Complex IV, Complex V • 3. FAD(2H)/succinate dehydrogenase, Coenzyme Q, cytochrome b-cl, cytochrome c, cytochrome a1-a3, F1F0-ATPase • 4. NADH dehydrogenase, CoQ, cytochrome b-cl, cytochrome c, cytochrome oxidase, ATP synthase • 5, NADH dehydrogenase, CoQ, cytochrome c, cytochrome oxidase, cytochrome b-cl, F1F0-ATPase • a. Both #1 and #2 • b. Both #3 and #4 • c. Only #4 • d. Only #3 • e. None of the above • As a skilled cell biologist and biochemist, you cleverly devise a method for experimentally separating the F1 portion of ATP synthase from the membrane-bound Fo fragment in intact mitochondria. Which of the following metabolic effects do you observe? • a. Electron transport and oxygen consumption are inhibited • b. Electron transport and phosphorylation of ADP remain tightly coupled • c. The inner mitochondrial membrane remains impermeable to protons • d. Protons pass through the membrane-bound Fo fragment, but they do not sustain any ATP formation • e. The F1 fragment forms ATP at an accelerated rate until ADP is depleted or the proton gradient is dissipated • Which of the following groups of enzymatic reactions, enzymes and substrates comprise important anaplerotic pathways for 4-carbon intermediates critical to the citric acid (TCA) cycle in the liver, muscle and nervous tissues? • a. conversion of pyruvate to acetyl CoA via pyruvate dehydrogenase and glutamate to a-ketoglutarate via transaminases • b. conversion of cc-ketoglutarate to glutamate and GABA • c. production of ketone bodies (acetoacetate and Phydroxybutyrate) • d. conversion of pyruvate to oxaloacetate via pyruvate carboxylase, biotin, bicarbonate ion, and ATP • e. both (A) and (D) • Regulation of tricarboxylic acid cycle activity in vivo may involve the concentration of all of the following EXCEPT: • • • • • acetyl CoA ADP. ATP. CoA. oxygen. • NAD+ can be regenerated in the cytoplasm if NADH reacts with any of the following EXCEPT: • • • • • pyruvate. dihydroxyacetone phosphate. oxaloacetate. the flavin bound to NADH dehydrogenase. phosphoglycerate kinase. • Glucokinase: • has a Km considerably greater than the normal blood glucose concentration.. • is found in muscle. • is inhibited by glucose 6-phosphate. • is also known as the GLUT-2 protein. • has glucose 6-phosphatase activity as well as kinase activity. • A 7yr old female presents with anxiety, dizziness, sweating and nausea following brief periods of exercise. The symptoms are relieved by eating and do not occur if the patient is frequently fed small meals. Blood analysis indicates she is hypoglycemic following brief period of fasting, alanine fails to increase blood sugar, fructose or glycerol administration restores glucose to normal? • What Pathway is affected, which enzyme could it be? How would you confirm your speculation? • After the BIOCHEM exam you and your friends decided to only drink “liquid-fire” (Bacardi 151) for the rest of the evening. The next morning you manage to wakeup with terrible ‘hangover’. Which of these molecules is most responsible for your hangover? • Lactic Acid • Pyruvate • Acetate • Acetyladehyde • Ethanol • ADH alcohol dehydrogenase • AcDH acetyladehyde dehydrogenase • Acetaldehyde forms adducts with Proteins, nucleic acids, and other compounds results in hangover. • NADH/NAD+ imbalance causes Liver to over work. • Diversion of gluconeogenesis by Lactic Acid dehydrogenase decreases ability of Liver to deliver glucose to the blood. • In addition, there is increased synthesis of FAT. Acetate + CoA gives you acetyl-CoA which is a precursor for Fatty acid sythesis. You already have enough NADH to go to work. So let the FATTYLIVER BEGIN! HepatoMEGALLY! Lets go! CLINICAL CORRELATIONS • Riboflavin Deficiency – FMN and FAD are both synthesized from riboflavin, which contains the electronaccepting ring structure of FAD – Severe Riboflavin deficiency decreases the ability of mitochondria to generate ATP via oxidative phosphorylation – In general, impairment of Complex I (NADH Dehydrogenase) induces formation of mitochondria with structural abnormalities. • Iron Deficiency Anemia – Characterized by decreased levels of Hb and other heme containing proteins in blood. – Iron-containing cytochromes and Fe-S centers of ETC are decreased as well. – Fatigue partly due to impaired ETC for ATP generation • ETC inhibitors at specific sites – Rotenone and Amytal block Complex I – Antimycin blocks cytochrome b1 in Complex III – Cyanide blocks cytochrome a/a3 in Complex IV. Prevents reduction of e- from reduced cytochrome c. – CO binds to reduced iron of cytochrome oxidase • Cyanide Poisoning – CN- causes a rapid and extensive inhibition of ETC at the cytochrome oxidase step. Prevents O2 from serving as the final e- acceptor. – Mitochondrial respiration and energy production cease, resulting in cell death – Occurs from tissue asphyxiation, most notably in the Nervous System – Treatment: nitrites administered to convert oxyHb to MetheHb, which can then compete with cytochrome a,a3 for the CN-, forming a complex. • Oxidative Phosphorylation II “the uncoupling of ETC and Ox-Phos” • Uncoupling of ETC with Ox-Phos – Proton gradient from ETC coupled to ATP production from Oxidative Phosphorylation. If uncoupled and proton gradient dissipated, ATP and ADP concentrations lose their ability to regulate the rate of e- transport. – Uncouplers: proton ionophores, which rapidly transport H+ from cytosolic to matrix side of inner mitochondiral membrane • DNP – picks up H+ on cyto side, drops H+ on matrix side – Oligomycin: inhibits F1F0-ATPase…ATP synthesis stops. • Respiration and transport are blocked • Addition of an uncoupler (DNP) induces initiation of O2 consumption…ETC continues but w/o ATP synthesis since the pathways are uncoupled. • Brown Adipose Tissue and Thermogenesis – Large deposits of brown fat around vital organs (in human infants)…specialized for ‘non-shivering thermogenesis.’ – Cold or excessive food intake stimulates NE release – Then Thermogenin, proton conductance uncoupler, is activated, pumping H+ back into mitochondria…dissipating the gradient. – ETC is induced, increasing rate of NADH and FADH2 oxidation, which generates more heat = biological heating pad • • Hyperthyroidism – Grave’s Disease – Thyroid hormone influences bioenergetics via actions on mitochondrial ox phos. – In Hyperthyroidism, energy derived from ox. Phos is significantly less than normal. – Thryoid causes ‘uncoupling’ of Ox Phos. – Results in increased heat production – patients complain of feeling hot and sweaty. • Salicylate (aspirin) poisoning – At high concentrations, salicylate can partially uncouple mitochondrial Ox Phos. – Decreased ATP [ ] and increased cytosolic AMP induce glycolysis – Results in increased blood pyruvate and lactate and metabolic acidosis and fever • Myoclonic Epileptic Ragged Red Fiber Disease (MERRF) – Debilitating, progressive spontaneous muscle jerking – Mitochondrial myopathy with enlarged, abnormal mitochondria – Neurosensory hearing loss, dementia, hypoventilation, mild cardiomyopathy – Maternal inheritance (sex linked) – Impaired energy metabolism….lactic acidosis • Pentose Phosphate Pathway • Hemolysis caused by Reactive Oxygen Species (ROS) – G6PD deficiency in pentose phosphate pathway – Causes increased production of radicals from GSH, since can’t produce sufficient NADPH to re-reduce glutathione….result in hemolysis • Heinz Bodies in RBCs – Due to G6PD deficiency – RBCs need the enzyme to re-reduce glutathione with NADPH to protect against oxidative stress – ROS peroxidation of membrane lipids lyses the RBC membrane • G6PD Mediterranean disease most severe G6PD deficiency • Lecture 21 – Monosaccharides and interconversion of sugars • Classical Galactosemia – Deficiency of Galactosyl-1-P uridylyltransferase – Accumulation of G-1-P in tissues and inhibition of glycogen metabolism, which require UDP-sugars – Higher level of galactose in blood and urine – More serious form • Non-Classical Galactosemia – Galactokinase deficiency – Unable to convert galactose to galactose-1-P • • Glycogen Synthesis Glucose Toxicity – Dysfunction of glycogen synthase – Due to hyperglycemia…produces insulin resistance – Due to production of hexosamines that inhibit hexokinase, protein phosphatase 1, and glycogen synthase. • • Lecture 23 – Glycogen Degradation Von Gierke’s Disease – – – – • • Defective G-6-Phosphatase enzyme Increased amount of glycogen, normal structure Affects liver and kidney Massive enlargement of the liver. Severe hypoglycemia, ketosis, hyperuricemia, hyperlipemia. Lecture 24 – Glucose/Glycogen Regulation Type I – Insulin-dependent diabetes mellitus – Hyperglycemic – Continuous glucagon expression causes ketogenesis, lipolysis, and gluconeogenesis. – Hyperchylomicronemia occurs (liver TG syn and VLDL transport faster than adipose LPL breakdown of TG) – Risk of ketoacidosis • Type II – Noninsulin-dependent Diabetes Mellitus – Hyperglycemic – Peripheral tissues insulin resistant – Glucose accumulates in blood due to poor uptake by peripheral tissues, particularly muscles – Hypertriacylglycerolemia, which results from increase of VLDL without hyperchylomicronemia. New FA and VLDL synthesized in liver instead of increased delivery of fatty acids from adipose tissue. Pentose Phosphate Pathway What is the PPP and why is it important? Pentose Phosphate Pathway What is the PPP and why is it important? The pentose phosphate pathway is primarily an anabolic pathway that utilizes the 6 carbons of glucose to generate 5 carbon sugars and reducing equivalents Pentose Phosphate Pathway • To generate reducing equivalents, in the form of NADPH, for reductive biosynthesis reactions within cells • To provide the cell with ribose-5-phosphate (R5P) for the synthesis of the nucleotides and nucleic acids • Although not a significant function of the PPP, it can operate to metabolize dietary pentose sugars derived from the digestion of nucleic acids as well as to rearrange the carbon skeletons of dietary carbohydrates into glycolytic/gluconeogenic intermediates Pentose Phosphate Pathway • The reactions of fatty acid biosynthesis and steroid biosynthesis utilize large amounts of NADPH. As a consequence, cells of the liver, adipose tissue, adrenal cortex, testis and lactating mammary gland have high levels of the PPP enzymes. • Erythrocytes utilize the reactions of the PPP to generate large amounts of NADPH used in the reduction of glutathione • The conversion of ribonucleotides to deoxyribonucleotides (through the action of ribonucleotide reductase) requires NADPH as the electron source, therefore, any rapidly proliferating cell needs large quantities of NADPH Pentose Phosphate Pathway Oxidative Pathway The reactions of the PPP operate exclusively in the cytoplasm. From this perspective it is understandable that fatty acid synthesis (as opposed to oxidation) takes place in the cytoplasm The oxidation steps, utilizing glucose-6-phosphate (G6P) as the substrate, occur at the beginning of the pathway and are the reactions that generate NADPH Reactions catalyzed by glucose-6-phosphate dehydrogenase and 6phosphogluconate dehydrogenase generate one mole of NADPH each for every mole of glucose-6-phosphate (G6P) that enters the PPP Pentose Phosphate Pathway Non-oxidative Pathway Non-oxidative reactions are to convert dietary 5 carbon sugars into both 6 (fructose-6phosphate) and 3 (glyceraldehyde-3-phosphate) carbon sugars which can then be utilized by the pathways of glycolysis The primary enzymes involved in the non-oxidative steps of the PPP are transaldolase and transketolase Transketolase functions to transfer 2 carbon groups from substrates of the PPP, thus rearranging the carbon atoms that enter this pathway. Like other enzymes that transfer 2 carbon groups, transketolase requires thiamine pyrophosphate (TPP) as a cofactor in the transfer reaction Transaldolase transfers 3 carbon groups and thus is also involved in a rearrangement of the carbon skeletons of the substrates of the PPP. The transaldolase reaction involves Schiff base formation between the substrate and a lysine residue in the enzyme Pentose Phosphate Pathway What’s the point? Pentose Phosphate Pathway What’s the point? R5P production Oxidation of G6P, a 6 carbon sugar, into a 5 carbon sugar Generation of NADPH 3 carbon sugar generated is glyceraldehyde-3-phsphate which can be shunted to glycolysis and oxidized to pyruvate OR it can be utilized by the gluconeogenic enzymes to generate more 6 carbon sugars (fructose-6-phosphate or glucose-6-phosphate) Pentose Phosphate Pathway RBCs and the PPP Predominant pathways of carbohydrate metabolism in the red blood cell (RBC) are glycolysis, the PPP and 2,3-bisphosphogylcerate (2,3-BPG) Glycolysis provides ATP for membrane ion pumps and NADH for re-oxidation of methemoglobin The PPP supplies the RBC with NADPH to maintain the reduced state of glutathione (Glutathione can reduce disulfides nonenzymatically) Oxidative stress generates peroxides that in turn can be reduced by glutathione to generate water Inability to maintain reduced glutathione in RBCs leads to increased accumulation of peroxides, predominantly H2O2, that in turn results in a weakening of the cell wall and concomitant hemolysis Glutathione removes peroxides via the action of glutathione peroxidase. The PPP in erythrocytes is essentially the only pathway for these cells to produce NADPH Glycogen Metabolism CH2OH CH2OH O H H OH H H OH H O OH CH2OH H H OH H H OH H H OH CH2OH O H OH O H OH H H O O H OH H H OH H H O 4 glycogen H 1 O 6 CH2 5 H OH 3 H CH2OH O H 2 OH H H 1 O CH2OH O H 4 OH H H H H O OH O H OH H H OH H OH Glycogen is a polymer of glucose residues linked by a(14) glycosidic bonds, mainly a(16) glycosidic bonds, at branch points Glycogen chains & branches are longer than shown Glucose is stored as glycogen predominantly in liver and muscle cells. CH2OH Glycogen catabolism (breakdown): H O H OH H H OH OH H OPO32 glucose-1-phosphate Glycogen Phosphorylase catalyzes phosphorolytic cleavage of the a(14) glycosidic linkages of glycogen, releasing glucose-1-phosphate as reaction product. glycogen(n residues) + Pi glycogen (n–1 residues) + glucose-1-phosphate Commonly used terminology: "a" is the form of the enzyme that tends to be active, and independent of allosteric regulators (in the case of Glycogen Phosphorylase, when phosphorylated). "b" is the form of the enzyme that is dependent on local allosteric controls (in the case of Glycogen Phosphorylase when dephosphorylated). Glycogen catabolism Most people don’t know… The relative activity of the un-modified phosphorylase enzyme (phosphorylase-b) is sufficient to generate enough glucose-1phosphate for entry into glycolysis for the production of sufficient ATP to maintain the normal resting activity of the cell; This is true in both liver and muscle cells Glycogen Phosphorylase in muscle is subject to allosteric regulation by AMP, ATP, and glucose-6phosphate. A separate isozyme of Phosphorylase expressed in liver is less sensitive to these allosteric controls. AMP (present significantly when ATP is depleted) activates Phosphorylase, promoting the relaxed conformation. ATP & glucose-6-phosphate, which both have binding sites that overlap that of AMP, inhibit Phosphorylase, promoting the tense conformation. Thus glycogen breakdown is inhibited when ATP and glucose-6-phosphate are plentiful. Regulation by covalent modification (phosphorylation): The hormones glucagon and epinephrine activate Gprotein coupled receptors to trigger cAMP cascades. Both hormones are produced in response to low blood sugar. Glucagon, which is synthesized by a-cells of the pancreas, activates cAMP formation in liver. Epinephrine activates cAMP formation in muscle. Glycogen catabolism •In response to lowered blood glucose the a cells of the pancreas secrete glucagon which binds to cell surface receptors on liver and several other cells; Liver cells are the primary target for the action of this peptide hormone •Activation of the enzyme adenylate cyclase which leads to a large increase in the formation of cAMP •cAMP binds to an enzyme called cAMP-dependent protein kinase, PKA. This leads to PKA-mediated phosphorylation of phosphorylase kinase Phosphorylase kinase activates the enzyme which in turn phosphorylates the b form of phosphorylase •Phosphorylation of phosphorylase-b greatly enhances its activity towards glycogen breakdown (phosphorylase-a) • The net result is an extremely large induction of glycogen breakdown in response to glucagon binding to cell surface receptors Hormone (epinephrine or glucagon) via G Protein (Ga-GTP) Adenylate cyclase (inactive) Adenylate cyclase (active) catalysis ATP cyclic AMP + PPi Activation Signal cascade by which Glycogen Phosphorylase is activated. Phosphodiesterase AMP Protein kinase A (inactive) Protein kinase A (active) ATP ADP Phosphorylase kinase (b-inactive) Phosphatase Phosphorylase kinase (P) (a-active) ATP Pi ADP Phosphorylase (b-allosteric) Phosphorylase (P) (a-active) Phosphatase Pi The cAMP cascade results in phosphorylation of a serine hydroxyl of Glycogen Phosphorylase, which promotes transition to the active (relaxed) state. The phosphorylated enzyme is less sensitive to allosteric inhibitors. Thus, even if cellular ATP & glucose-6-phosphate are high, Phosphorylase will be active. The glucose-1-phosphate produced from glycogen in liver may be converted to free glucose for release to the blood. With this hormone-activated regulation, the needs of the organism take precedence over needs of the cell. Glycogen catabolism This identical cascade of events occurs in skeletal muscle cells However, in these cells the induction of the cascade is the result of epinephrine binding to receptors on the surface of muscle cells (Ca2+ ion-mediated pathway to phosphorylase kinase activation is through activation of a-adrenergic receptors by epinephrine) Epinephrine is released from the adrenal glands in response to neural signals indicating an immediate need for enhanced glucose utilization in muscle, the so called fight or flight response Muscle cells lack glucagon receptors. The presence of glucagon receptors on muscle cells would be futile anyway since the role of glucagon release is to increase blood glucose concentrations and muscle glycogen stores cannot contribute to blood glucose levels…why? Glycogen catabolism – Regulation of phosphorylase kinase activity is also affected by two distinct mechanisms involving Ca2+ ions – The ability of Ca2+ ions to regulate phosphorylase kinase is through the ubiquitous protein, calmodulin – Calmodulin is a calcium binding protein; binding induces a conformational change in calmodulin which in turn enhances the catalytic activity of the phosphorylase kinase towards its substrate, phosphorylase-b. – This activity is crucial to the enhancement of glycogenolysis in muscle cells where muscle contraction is induced via acetylcholine stimulation at the neuromuscular junction – The effect of acetylcholine release from nerve terminals at a neuromuscular junction is to depolarize the muscle cell leading to increased release of sarcoplasmic reticulum stored Ca2+, thereby activating phosphorylase kinase – Thus, not only does the increased intracellular calcium increase the rate of muscle contraction it increases glycogenolysis which provides the muscle cell with the increased ATP it also needs for contraction Phosphorylase Kinase inactive ++ Phosphorylase Kinase-Ca partly active P-Phosphorylase Kinase-Ca++ fully active Phosphorylase Kinase in muscle includes calmodulin as its d subunit. Phosphorylase Kinase is partly activated by binding of Ca++ to this subunit Phosphorylation of the enzyme, via a cAMP cascade induced by epinephrine, results in further activation These regulatory processes ensure release of phosphorylated glucose from glycogen, for entry into Glycolysis to provide ATP needed for muscle contraction. Pyridoxal phosphate (PLP), a derivative of vitamin B6, serves as prosthetic group for Glycogen Phosphorylase. H O O P O O C H2 C OH O N H CH3 pyridoxal phosphate (PLP) A class of drugs developed for treating the hyperglycemia of diabetes (chloroindolecarboxamides), inhibit liver Phosphorylase allosterically. These inhibitors bind at the dimer interface, stabilizing the inactive (tense) conformation. PLP GlcNAc inhibitor GlcNAc Human Liver Glycogen Phosphorylase PLP PDB 1EM6 Question: Why would an inhibitor of Glycogen Phosphorylase be a suitable treatment for diabetes? Debranching enzyme has 2 independent active sites, consisting of residues in different segments of a single polypeptide chain: The transferase of the debranching enzyme transfers 3 glucose residues from a 4-residue limit branch to the end of another branch, diminishing the limit branch to a single glucose residue The a(16) glucosidase moiety of the debranching enzyme then catalyzes hydrolysis of the a(16) linkage, yielding free glucose. This is a minor fraction of glucose released from glycogen The major product of glycogen breakdown is glucose-1phosphate, from Phosphorylase activity. Enzyme-Ser-OPO32 CH2OPO32 CH 2OH H O H OH H OH H Enzyme-Ser-OPO32 Enzyme-Ser-OH H OPO32 OH glucose-1-phosphate H O H OH H OH H OH CH 2OPO32 H OPO32 H O H OH H H OH OH H OH glucose-6-phosphate Phosphoglucomutase catalyzes this reversible reaction Glycogen Glucose-1-P Glucose Hexokinase or Glucokinase Glucose-6-Pase Glucose-6-P Glucose + Pi Glycolysis Pathway Pyruvate Glucose metabolism in liver. The product glucose-6-phosphate may enter Glycolysis or (in liver) be dephosphorylated for release to the blood Liver Glucose-6-phosphatase catalyzes the following, essential to the liver's role in maintaining blood glucose: glucose-6-phosphate + H2O glucose + Pi Most other tissues lack this enzyme…why?? O CH2OH Glycogen synthesis HN O H H OH H O H O OH H OH UDP-glucose P O O O O P O CH2 O N O H H OH H OH H Uridine diphosphate glucose (UDP-glucose) is the immediate precursor for glycogen synthesis As glucose residues are added to glycogen, UDP-glucose is the substrate and UDP is released as a reaction product. O UDP-Glucose Pyrophosphorylase CH2OH HN O H H OH H O H H O P O OH O + O O OH O P O O P O O O O CH2OH H OH HN H O H O OH H OH O UTP PPi O P P O O O O UDP-glucose P O CH2 O N O H H OH H OH H CH2 O glucose-1-phosphate H O N O H H OH H OH H UDP-glucose is formed from glucose-1-phosphate: glucose-1-phosphate + UTP UDP-glucose + PPi PPi + H2O 2 Pi Overall: glucose-1-phosphate + UTP UDP-glucose + 2 Pi Spontaneous hydrolysis of the ~P bond in PPi (P~P) drives the overall reaction Cleavage of PPi is the only energy cost for glycogen synthesis (one ~P bond per glucose residue). Glycogenin initiates glycogen synthesis. Glycogenin is an enzyme that catalyzes glycosylation of one of its own tyrosine residues. 6 CH 2OH H 4 OH 5 O H OH H H O O C 1 O 3 tyrosine residue of Glycogenin UDP-glucose P O P O Uridine HO C CH H2 NH 2 H O OH O 6 CH 2OH O-linked glucose H residue 4 OH 5 O H OH H H C 1 O 3 2 H O OH C CH H2 NH + UDP CH OH CH OH 2 A glycosidic bond is formed2 between the anomeric C1 of the O O H H from UDP-glucose Hglucose moiety Hderived and the hydroxyl H H C O H oxygen of a tyrosine side-chain of Glycogenin. H OH OH O C CH O a product. OH UDP is released as H 2 H OH H OH NH O 6 CH 2OH O-linked glucose H residue 4 5 O H OH OH UDP-glucose 1 OH O H H H OH H + UDP OH a(14) linkage H C H O O OH H C CH H2 NH 2 H O CH2OH O H OH C O 3 CH2OH H H H H OH C CH H2 NH O + UDP Glycosylation at C4 of the O-linked glucose product yields an O-linked disaccharide with a(14) glycosidic linkage. UDP-glucose is again the glucose donor This is repeated until a short linear glucose polymer with a(14) glycosidic linkages is built up on Glycogenin Glycogen Synthase catalyzes transfer of the glucose moiety of UDP-glucose to the hydroxyl at C4 of the terminal residue of a glycogen chain to form an a(1 4) glycosidic linkage: glycogen(n residues) + UDP-glucose glycogen(n +1 residues) + UDP A separate branching enzyme transfers a segment from the end of a glycogen chain to the C6 hydroxyl of a glucose residue of glycogen to yield a branch with an a(16) linkage. Glycogen Synthesis UTP UDP + 2 Pi glycogen(n) + glucose-1-P glycogen(n + 1) Glycogen Phosphorylase Pi Both synthesis & breakdown of glycogen are spontaneous If both pathways were active simultaneously in a cell, there would be a "futile cycle" with cleavage of one ~P bond per cycle (in forming UDP-glucose) To prevent such a futile cycle, Glycogen Synthase and Glycogen Phosphorylase are reciprocally regulated, by allosteric effectors and by phosphorylation. Glycogen Glucose-1-P Glucose Hexokinase or Glucokinase Glucose-6-Pase Glucose-6-P Glucose + Pi Glycolysis Pathway Pyruvate Glucose metabolism in liver. Glycogen Synthase is allosterically activated by glucose-6-P (opposite of effect on Phosphorylase) Thus Glycogen Synthase is active when high blood glucose leads to elevated intracellular glucose-6-P It is useful to a cell to store glucose as glycogen when the input to Glycolysis (glucose-6-P), and the main product of Glycolysis (ATP), are adequate. Glycogen Glucose-1-P Glucose Hexokinase or Glucokinase Glucose-6-Pase Glucose-6-P Glucose + Pi Glycolysis Pathway Pyruvate Glucose metabolism in liver. High cytosolic glucose-6-phosphate, which would result when blood glucose is high, turns off the signal with regard to glycogen synthesis The conformation of Glycogen Synthase induced by the allosteric activator glucose-6-phosphate is susceptible to dephosphorylation by Protein Phosphatase (PP1) The cAMP cascade induced in liver by glucagon or epinephrine has the opposite effect on glycogen synthesis. Glycogen Synthase is phosphorylated by Protein Kinase A as well as by Phosphorylase Kinase. Phosphorylation of Glycogen Synthase promotes the "b" (less active) conformation. The cAMP cascade thus inhibits glycogen synthesis. Instead of being converted to glycogen, glucose-1-P in liver may be converted to glucose-6-P, and dephosphorylated for release to the blood. Insulin, produced in response to high blood glucose, triggers a separate signal cascade that leads to activation of Phosphoprotein Phosphatase This phosphatase catalyzes removal of regulatory phosphate residues from Phosphorylase, Phosphorylase Kinase, & Glycogen Synthase enzymes Thus insulin antagonizes effects of the cAMP cascade induced by glucagon & epinephrine Glycogen Storage Diseases are genetic enzyme deficiencies associated with excessive glycogen accumulation within cells Some enzymes whose deficiency leads to glycogen accumulation are part of the inter-connected pathways shown here glycogen glucose-1-P Glucose-6-Phosphatase glucose-6-P glucose + Pi fructose-6-P Phosphofructokinase fructose-1,6-bisP Glycolysis continued When an enzyme defect affects mainly glycogen storage in liver, a common symptom is hypoglycemia, relating to impaired mobilization of glucose for release to the blood during fasting. When the defect is in muscle tissue, weakness & difficulty with exercise result from inability to increase glucose entry into Glycolysis during exercise. Additional symptoms depend on the particular enzyme that is deficient. Glycogen Storage Disease Symptoms, in addition to glycogen accumulation Type I, liver deficiency of Glucose-6-phosphatase (von Gierke's disease) hypoglycemia (low blood glucose) when fasting, liver enlargement. Type IV, deficiency of branching enzyme in various organs, including liver (Andersen's disease) liver dysfunction and early death. Type V, muscle deficiency of Glycogen Phosphorylase (McArdle's disease) muscle cramps with exercise. Type VII, muscle deficiency of Phosphofructokinase. inability to exercise. Summary