* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download History of the Nervous System Cells of the Nervous System
Cognitive neuroscience wikipedia , lookup
Multielectrode array wikipedia , lookup
History of neuroimaging wikipedia , lookup
Neuropsychology wikipedia , lookup
Neuroplasticity wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Optogenetics wikipedia , lookup
Intracranial pressure wikipedia , lookup
Axon guidance wikipedia , lookup
Node of Ranvier wikipedia , lookup
Holonomic brain theory wikipedia , lookup
Neural engineering wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Anatomy of the cerebellum wikipedia , lookup
Hydrocephalus wikipedia , lookup
Nervous system network models wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Circumventricular organs wikipedia , lookup
Subventricular zone wikipedia , lookup
Metastability in the brain wikipedia , lookup
Sports-related traumatic brain injury wikipedia , lookup
Haemodynamic response wikipedia , lookup
Neuroregeneration wikipedia , lookup
Synaptogenesis wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Channelrhodopsin wikipedia , lookup
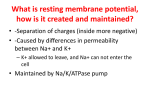
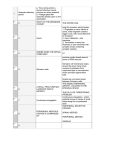
History of the Nervous System Cells of the Nervous System 2 Types: o Neurons Cannot divide; however, they have the capacity to undifferentiated and then divide, becoming tumors. Classification of Neurons Multipolar Many processes Common for motor neurons Unipolar Common for sensory neurons of PNS Bipolar Found in sense organs One process from axon to soma Axon and dendrite make up two processes o Glia (means glue) Can divide! May also become tumors as well 6 Types of Glia: Ependymal Cells: Line the ventricles Have cilia Anaxonic Can’t tell axon and dendrites apart Microglia: Specialized immune cell… will proliferate if pathogen is present Have phagocytic properties Astrocytes: Most common in CNS Mediator b/w blood and the neuron… decides what the neuron gets from the blood This helps form the Blood Brain Barrier! Also, repair damaged tissue o Can lead to gliosis = scar formation from massive proliferation of astrocytes o white area in brain Two types: o Fibrous associated w/ axons o fibrous astrocytes o Protoplasmic associated w/ soma protoplasmic Oligiodendrocytes Myelinate segments of several axons In CNS Schwann Cell In PNS Myelinate segment of one axon Assist in axon repair by acting like a tunnel for it to grow back through Satellite Cell In ganglia b/c associated w/ cell bodies Regulate environ and provide nutrients to soma o Glia Limitans Purpose is to regulate movement of molecules into and out of the brain External: Outermost layer of neural tissue (b/w pia and brain) Formed by the feet of the astrocytes Internal: Also formed by astrocyte foot processes B/w brain and ventricular CSF o Ependymal cells associated w/ it o Myelin A lipoprotein made up of either schwann or oligiodendrocyte membrane Increases the speed of the AP o Neuropil Synaptically dense region containing dendrites, glia and unmyelinated axons Neuron Histology Soma (cell body): o Contains same organelles as normal cells… Nucleus (nucleolus = all the dark spots in pic. below) RER (Nissl bodies) They give off the gray color in gray matter Golgi, mitochondria, lysosomes Storage vesicles May contain lipofuscin, which is brown/yellow pigment of fatty residues left over from lysosomal digestion Result of aging Axon Hillock (AH) clear area (b/c no RER) that signifies we are going into an axon This is where membrane potentials are summated before entering the axon Dendrites o Increase neuron surface area and allow for more synapses o Shape is formed by actin filament o o Dendritic spines (DS) are dynamic protrusions at the synapse. They form as you gain new experiences… trippy… B/c of this learning is associated w/ formation of DS. Alcohol reverses this problem and thus Fetal Alcohol Syndrome causes problems Axon o One axon per one neuron! o Purpose is to transmit action potential to an effector cell (every cell except a neuron) or a neuron. o o The cytoskeleton in axons create the Axoplasmic Flow: Anterograde Axoplasmic Transport Retrograde Axoplasmic Transport Cell body axon synaptic terminal Synaptic terminal axon cell body Kinesin Dynein Brings Neurotransmitters to synapse How rabies gets into CNS… picks up the toxin and carries it to the cell body then to the CNS. This is why there is a short window of time in order to deal w/ it. Axon Terminal (Synaptic Boutons) o Site of Neurotransmitter (NT) release o Has synaptic vesicles (w/ NT) and mitochondria o o Chemical Synapse: Presynaptic membrane, synaptic cleft, and postsynaptic membrane o Electrical Synapse: Ions flow through gap junctions o Types of Synapses o PNS – Ganglia CT of PNS goes epineurium perineurium endoneurium OVERALL Afferent = peripheral central o sensory Efferent = central peripheral (exits the CNS) o motor Gray matter = region of cell bodies, unmyelinated axons and dendrites o Gray due to Nissl bodies (RER) White matter = region of axons, myelinated and unmyelinated axons o White b/c of the phospholipids from the cell membranes of glia (myelin sheath) In brain white matter is deep and gray is superficial In spinal cord white matter is superficial and gray is deep Oligiodendrocytes = CNS Schwann = PNS Myelinated neurons = very large diameter, faster impulse Unmyelinated neurons = very small diameter, slower impulse Group of Axons Group of Cell Bodies Neural Tube Defects CNS PNS Tract Nucleus Nerve Ganglion CNS Malformations Occur when a part of the neural tube fails to close OR a part of the tube can reopen after it has fully closed Inadequate folate during initial weeks of gestation is a huge risk factor for these defects! Diagnosis base on ultrasound and maternal blood screening of elevated alpha-fetoprotein Spina Bifida Occulta Asymptomatic bony defect Meningocele -Meninges and CSF protrude out through spina bifida defect Note: occult spinal dysraphism (OSD) is hair/birthmark over the spina bifida occulta defect and sometimes can also have protrusion of meninges/spinal cord Neural Tube Defects Myelomeningocele Encephalocele -Spinal cord, meninges, and CSF protrude out through spina bifida defect -Most common form and usually happens in the lumbosacral region -Present w/ problems w/ lower extremity motor skills and bowel/bladder control -Malformation of cranium causing brain to protrude -Usually in the posterior fossa or through the cribiform plate in the anterior fossa (may be mistaken for a nasal glioma) Anencephaly -Malformation of anterior end of neural tube -Absence of brain and calvarium -The forebrain does not develop at day 28. -All that is there is the area cerebrovasculosa (flattened remnant of disorganized brain tissue) Note: Spina bifida (aka split spine) is a broad category that encompasses spina bifida occult, occult spinal dysraphism, meningocele, and myelomeningocele. Forebrain Anomalies Abnormalities in generation and migration of neurons = forebrain malformations o Either effects part of the forebrain or the whole thing Megalencephaly Microencephaly -Brain is abnormally large -Brain is abnormally small -More common than megalencephaly -Can be caused by chromosome abnormalities, fetal alcohol syndrome, or HIV-1 infection Lissencephaly -Few or no gyri (agyria) Two Patterns: Smooth surface Mutations w/ signaling for migration and cytoskeleton motor proteins Results in inability of neuroblasts to migrate Rough/cobblestoned surface Mutations that disrupt the stop signal for migration Forebrain Anomalies Polymicrogyria -Small, numerous gyri -Entrapment of meningeal tissue in the 4 layers of gray matter leads to an irregular cortical surface Neuronal Heterotopias Holoprosencephaly Agenesis of corpus callosum -Migrational disorders associated w/ epilepsy -Collections of neurons in the wrong places along migrational pathways -Commonly found along the ventricular surface -Periventricular heterotopias = mut. in filamin A (responsible for creating meshwork of filaments) -Incomplete separation of cerebral hemispheres -Result in midline facial abnormalities (cyclopia) -Arrhin-encephaly = absence of CN 1 -Associated w/ trisomy 13 -Common -absence of corpus callosum -Batwing deformity = misshapen lateral ventricles -May be either asymptomatic or lead to mental retardation Posterior Fossa Anomalies Malformations that affect the brainstem and the cerebellum Dandy-Walker Malformation -Enlarged posterior fossa -Cerebellar vermis is absent (associated w/ posture and locomotion) -Large midline cyst lined w/ ependymal and contiguous w/ leptomeninges represents the 4th ventricle and replaces the cerebellar vermis Posterior Fossa Abnormalities Chiari Type II (Arnold-Chiari) -Small posterior fossa, misshapen midline cerebellum, and downward extension of vermis through foramen magnum -Usually also has hydrocephalus and lumbar myelomeningocele Chiari Type I -Low cerebellar tonsils extend into vertebral canal Syringomyelia Hydromyelia -Cystic cavities that occur around the central canal that is NOT lined w/ ependymal cells -Associated w/ Chiari I, intraspinal tumors, or traumatic injury -Dilation of the central canal of the spinal cord that is lined w/ ependymal cells -Sometimes this dilation can connect w/ the fourth ventricle -Called syringobulbia if cavity extends to the brainstem Note: both of these cause a syrinx (fluid filled cavity in spinal cord) and result in the same symptoms isolated loss of pain and temperature sensation in the upper extremities b/c anterolateral spinal tract can’t cross the ventral commissure in the cervical area Ataxia Telangectasia Sturge-Weber Syndrome -Autosomal recessive -Beginning in early childhood, loss of full control of body movements (ataxia) and subsequent development of dilation of capillaries (telangiectasia) in the conjunctiva and eye. Also, immunodeficient. -Mutated ATM gene on chromosome 11q22-q23 kinase responsible for cellular response to dsDNA breaks… they continue to replicate damaged DNA -Abnormalities in cerebellum (loss of Purkinje and granule cells) -Degeneration of dorsal columns, spinocerebellar tracts, anterior horn cells, and peripheral neuropathy Clinical: -Very progressive, early death -Initial recurrent sinopulmonary infections and unsteady walking -Rare congenital disorder -Venous angiomatous masses in cortical leptomeninges w/ ipsilateral facial port wine nevi Basically, malformation of the veins that drain the brain -Associated w/ mental retardation, seizures, hemiplegia Tuberous Sclerosis -Autosomal dominant 1/6000 births -Hamartomas (benign neoplasm that represents tissue of origin) Take form of cortical tubers (abnormal development of brain) o Cause epilepsy And subependymal nodules o Subependymal giant cell astrocytomas -Associated w/ benign neoplasms in other organs of the body (liver, kidney, pancreas, lung, heart) -TSC1 encodes hamartin -TSC2 encodes tuberin -Hamartin and tuberin bind inhibit mTOR kinase (key regulator in protein synthesis) -Later difficulty talking and moving eyes -Usually develop T-cell leukemias Metabolic Diseases of the Nervous System Neuronal Storage Diseases Autosomal recessive deficiency of a specific enzyme for catabolism of sphingolipids, mucopolysaccharides, or mucolipids causes accumulation of the substrate for deficient enzyme in lysosomes of neurons neuronal death If occurs in cortical neurons loss of cognitive function and possibly seizures Neuronal Storage Diseases Neuronal Ceroid Lipofuscinoses Tay-Sachs Disease Accumulation of lipofuscin Accumulation of Gm2 gangliosides Neuronal dysfunction blindness, mental and motor deterioration, and seizures Def. in hexosaminidase A Characterized by age of onset or pattern of inclusion on electron microscopy Infantile INCL Late Infantile LINCL Juvenile JNCL Adult ANCL Kuf dz Leukodystrophies Autosomal recessive Myelin abnormalities w/ synthesis or turnover causes progressive degeneration of white matter o Adrenoleukodystrophy is x-linked!! Do NOT have neuronal storage defects If problem in white matter deterioration in motor skills, spasticity, hypotonia, or ataxia Krabbe Disease Leukodystrophies Metachromatic Leukodystrophy Adrenoleukodystrophy Autosomal recessive Autosomal recessive X-linked Definiciency of galactocerebroside betagalactosidase (galactosylceramidase) does catabolism of galactocerebroside to ceramide and galactose Deficiency of arysulfatase A… a lysosomal enzyme accumulation of sulfatide (cerebroside sulfate) Progressive dz w/ symptoms of myelin loss from the CNS and PNS and adrenal insufficiency (atrophy of adrenal cortex) Distal end of chromosome 22q ALD gene on chromosome X (g28) ATPbinding cassette transporter ABCD1 Chromosome 14q31 Excess galactocerebroside becomes galactosylsphingosine cytotoxic compound that causes oligodendrocyte injury Clinical Motor stiffness and weakness Gradual feeding difficulties Rapidly progressive survival beyond 2 y.o. uncommon Clinical Late infantile form most common Juvenile form Both child forms present w/ progressive motor symptoms death in 5-10 years Adult form Psychiatric/cognitive symptoms then motor symptoms Inability to catabolize very long chain fatty acids in peroxisomes elevated VLCFA in blood Clinical Earlier onset more rapid course Child w/ neurological symptoms and adrenal insufficiency rapidly progressive and fatal Later onset more protracted Peripheral n. involvement slowly progressive Mitochondrial Encephalomyopathies Problem w/ oxidative phosphorylation can’t produce ATP mutations in mitochondrial DNA involves gray matter (CNS) and skeletal muscle Usually presents as muscles diseases Mitochondrial Encephalomyopathy, Lactic Acidosis, and Strokelike Episodes (MELAS) Mitochondrial Encephalomyopathies Myoclonic Epilepsy and Ragged Red Fibers (MERRF) Most common type! Maternally transmitted Mutation in tRNAs Mutation in tRNAs diff. from MELAS Recurrent episodes of everything it says in the name + muscle weakness Myoclonus seizure disorder w/ myopathy Areas of infarction w/ vascular proliferation and focal calcification Leigh Syndrome (Subacute Necrotizing Encephalopathy) Early childhood dz of Lactic academia, lack of psychomotor development, feeding problems, seuizures, extra-ocular palsies, and weakness w/ hypotonia Death w/in 1 to 2 years Ataxia w/ neuronal loss from cerebellum system (inferior olive, cerebellar cortex, and deep nuclei) Mutations mitochondrial genome components for oxidative phosphorylation and tRNAs Acquired Metabolic Diseases Thiamine (Vit. B1) Disorder Beriberi cardiac failure Wernicke encephalopathy Psychotic symptoms or ophthalmoplegia w/ sudden onset Korsakoff syndrome memory disturbances Vitamin B12 Deficiency Anemia can be the cause of neurological symptoms numbness, tingling, ataxia in lower extremities can progress to spastic weakness and complete paraplegia Hypoglycemia Low blood glucose not good b/c glucose is the fuel for the brain Pyramidal neurons, hippocampus, and purkinje cells are especially sensitive to this Hyperglycemia Most commonly found in inadequately controlled diabetes mellitus Associated w/ ketoacidosis or hyperosmolar coma Paraplegia usually the only thing that cannot be recovered Wernicke-Korsakoff syndrome usually used b/c the two syndromes are closely linked -Result of chronic alcoholism Toxic Disorders Carbon Monoxide Methanol Hypoxia from altered oxygen-carrying capacity of hemoglobin Usually affects the retina degeneration of retinal ganglion cells blindness Injury to neurons of layers 3 and 5 of the cerebral cortex Sommer sector of hippocampus and purkinje cells Severe bilateral putamenal necrosis and focal white-matter necrosis Bilateral necrosis of the globus pallidus Ethanol Chronic alcohol abuse Cerebellar dysfunction truncal ataxia, unsteady gait, nystagmus Lysosomal Storage Diseases Lysosomal enzymes (acid hydrolases) synthesized in ER transported to golgi post-translation modifications attachment of mannose-6-phosphate lysosomal enzymes w/ mannose-6-P pinch of golgi in a vesicle Lysosomal enzymes break down things from autophagy (metabolic turnover of intracellular organelles) of heterophagy (stuff acquired from outside the cells by phagocytosis) Lysosomal storage diseases are a deficiency in a lysosomal enzyme leads to build up of insoluble metabolite w/in lysosome lysosome enlarges w/ this stuff Tay Sachs Dz Hexosaminidase A (alpha subunit) Gm2 gangliosidoses Morphology -hexosaminidase A is absent in all tissue Gm2 gangliosidoses accumulations every where mostly in neurons of CNS and ANS and retina Lysosomal Storage Diseases Neimann-Pick Dz types A Gaucher Dz and B Inherited def. in sphingomyelinase accum. of lysosomal sphingomyelin (usually in mononuclear phagocyte system) Chromosome 11p15.4 Type A -Severe infantile form -Extensive neurologic involvement -Visceral accumulations of sphingomyelin -Progressive wasting and early death w/in 3 years of life -Missense mut. almost complete deficiency of sphingomyelinase -Infants w/ big belly hepatosplenomegaly -Progressive deterioration of psychomotor function Autosomal recessive mut. in glucocerebrosidase (cleaves glucose from ceramide) accum. of glucocerebroside in phagocytes and CNS Pathology from accumulations and activation of MO’s secretion of IL-1, IL-6 and TNF 3 Subtypes -Type 1, Chronic nonneuronopathic form Most common Glucocerebrosides only in mononuclear phagocytes Splenic and skeletal involements… NO brain Detectable enzyme Jews Mucopolysachharidoses Autosomal recessive def. in lysosomal enzymes that degrade mucopolysaccharides (glycosaminoglycans) Hunter syndrome is an Xlinked recessive trait Glycosaminoglycans include: Dermatan sulfate, heparan sulfate, keratan sulface, and chondroitin sulfate Mucopolysaccharides are a part of proteoglycans abundant in ground substance of connective tissue Accumulations of mucopolysaccharides are found in Type B -Organomegaly but NO CNS involvement Morphology -“Foam cells” -Found in spleen (massive enlargement), liver, lymph nodes, bone marrow, tonsils, GI tract, and lung -In brain gyri shrunken and sulci widened diffuse neuronal involvement -Retinal cherry-red spot seen here too Clinical -Symptoms at 6 months old -Relentless motor and mental deterioration -Cherry-red spot in macula of eye -Death at 2-3 y.o. Other Gm2 gangliosidosis -Sandhoff dz beta subunit defect -Gm2 activator deficiency -Same clinical manisfestations as TaySachs -Type 2, Acute neuronopathic Infantile acute cerebral pattern No detectable enzyme Splenomegaly but mostly CNS involvement No Jews -Type 3 Intermediate b/w type 1 and 2 Systemic involvement like type 1, but progressive CNS like type 2 Morphology -Spleen, liver, bone marrow, lymph nodes, tonsils, thymus and Peyer’s patch mononuclear phagocytic cells, endothelial cells, smooth muscle cells and fibroblasts. Usually in the spleen, liver, bone marrow, lymph nodes, blood vessels, and heart Clinical -Hepatosplenomegaly -Skeletal deformities -Valvular lesions -Subendothelial arterial deposits myocardial ischemia myocardial infarction and cardiac decompensation death MPS 1 Hurler syndrome Def. in alpha-1iduronidase Very severe, affects children MPS 2 Hunter syndrome X-linked Absence of corneal clouding and milder clinical course Tay Sachs and Niemann-Pick dz are both common among Ashkenazi Jews Peripheral Nerve Tumors Tumors of the peripheral nerves can arise from Schwann cells, perineurial cells, and fibroblasts Schwannoma Benign tumor that arises in Schwann cells that arise from the neural crest Well encapsulated easily separated from the nerve Peripheral Nerve Tumors Neurofibroma Benign nerve sheath tumors Neoplastic schwann cells mixed w/ perineuriallike cells, fibroblasts, mast cells and CD34+ spindle cells Malignant Peripheral Nerve Sheath Tumor ½ arise in NF1 PT’s probably from malignant transformation of a plexiform neurofibroma Usually in larger peripheral nerves of chest, abdomen, pelvis, neck or limb-girdle Common component of neurofibromatosis 2 Inactivating mutations in the NF2 gene on chromosome 22 Loss of expression of merlin Normally restricts the cell-surface expression of growth factor receptors (EGFR) W/o it cells hyperproliferate in response to GF’s Morphology -Antoni A moderate to high cellularity -Verocay bodies nuclear free zones -Antoni B less densely cellular May either be sporadic or NF1-associated Exhibit complex chromosomal aberrations Distinguished by growth pattern: Superficial cutaneous neurofibromas Unencapsulated nodular lesions Neurofibromatosis Type 1 -Common autosomal dominant LOF mut. in NF1 gene no neurofibromin RAS is on -Systemic dz w/ nonneoplastic manifestations -Mental retardation, seizures, skeletal defects - Pigmented nodules of the iris (Lisch nodules) Diffuse neurofibromas Plaque on skin Plexiform neurofibromas -Grow in nerve fascicles entrapping axons -“Bag of worms” expanded, ropy thickening of multiple nerve fascicles -Collagen looks like “shredded carrot” -Not possible to separate tumor from nerve -Loss of NF1 function no neurofibromin (tumor suppressor that -Cutaneous hyperpigmented macules (café au lait spots) -Elephant man Neurofibromatosis Type 2 inhibits RAS) Presence of multiple neurofibromas or plexiform neurofibromas neurofibromatosis type 1 Clinical -Usually at the cerebellopontine angle attach to vestibular branch of CN 8 tinnitus and hearing loss aka acoustic neuroma -Autosomal dominant -Bilateral CN 8 schwannomas and multiple meningiomas -W/in dura sensory nerves, CN 5, and dorsal roots -Extradural where motor and sensory nerve fibers mixed Skull Fractures CNS Trauma Fall while awake usually occipital bone fracture Fall w/ loss of consciousness usually frontal bone fracture Diastatic fracture fracture that crosses sutures Displaced (depressed) Bone displaced into cranial cavity by a distance greater than the thickness of the bone Ex: PT struck by hard object… like a hammer Skull Fractures Linear/curvilinear Basilar (basal) Can have branching fractures off of the main fracture Usually skull fractures are linear fractures of the calvarium Ex: PT fallen and hit their head on a hard surface… like concrete Fracture of the base of the skull Suspicion of this if symptoms from cranial nerves in the cervicomedullary region and orbital or mastoid hematomas Ring Occurs at base of skull where fracture encircles the foramen magnum When head forcibly pushed inferiorly or vertebral column forcibly pushed superiorly Ex: someone jumping from a great height and lands on feet Ex: impact to occiput or sides of head CSF discharge from nose or ear and meningitis may follow Parenchymal Injuries Concussion Types of Parenchymal Injuries Direct Parenchymal Injury Altered consciousness after a head injury Laceration tearing of brain tissue Symptoms -Instantaneous onset of transient neurologic dysfx -Loss of consciousness -Temporary respiratory arrest -Loss of reflexes Contusion bruising of brain tissue -Blow to surface of the brain transmitted through the skull -Crests of gyri most susceptible Diffuse Axonal Injury Damage in the form of extensive lesions in white matter tracts occurs over a widespread area Damage to axon at the node of Ranvier that alters axoplasmic flow Can be caused by angular acceleration in the absence of impact 50% of coma PT have this Common sites frontal lobes along the orbital ridges and temporal lobes Uncommon sites occipital lobes, brainstem, cerebellum Fracture contusions may occur here though Types of Contusions Coup injury develops a contusion at the point of contact Countrecoup injury develops a contusion opposite to point of contact Traumatic Vascular Injuries Epidural Hematoma temporal skull fracture middle meningeal a. ruptured neurosurgical emergency o Subdural Hematoma lateral aspects of cerebral hemispheres tear in bridging veins at point where they penetrate the dura slowly progressive neurologic deterioration o Subarachnoid and intraparenchymal compartment hemorrhages usually happen at the same time if there has been brain trauma Gunshot Wounds Something weird /(funny…?) to wake you up to keep studying Penetrating into but not through the head Perforating through the head Entrance Wounds round to ovoid w/ marginal abrasion Exit Wounds create tears in skin and irregular margins Contact Gunshot Wound Muzzle stamp or soot deposition Close-range Soot and searing of skin Medium range Some soot around the entrance wound Distance range no gunpowder Child Abuse Scalp contusions, subdural hematoma, perioptic nerve hemorrhages, retinal hemorrhages (shaken baby syndrome) o Sequelae of Brain Trauma Post-traumatic hydrocephalus obstruction of CSF resorption from hemorrhage into subarachnoid spaces Post-traumatic dementia and punch drunk syndrome repeated head trauma Post-traumatic epilepsy, tumor, infectious dz, psychiatric disorders Spinal Cord Trauma Thoracic vertebrae or below paraplegia Cervical lesions quadriplegia Above C4 respiratory compromise from paralysis of diaphragm Principal cause of neurological deficits is from damaging the tracts in the spinal cord and disconnecting them from its cortical connections in the cerebrum and brain stem Cerebral Edema, Hydrocephalus, Raised Intracranial Pressure (ICP), and Herniation Cerebral Edema Brain edema, increased CSF, and focally expanding mass lesions can cause ICP Generalized both vasogenic and cytotoxic edema Gyri flattened. Sulci narrowed. Ventricals compressed. can result in herniation if too much ICP o Interstitial edema (hydrocephalic edema) around lateral ventricles from increase in intravascular pressure that causes intraventricular CSF to cross the ependymal lining into the white matter Types of Cerebral Edema Vasogenic Cytotoxic BBB disruption and increased vascular permeability intercellular spaces of the brain edema is b/w the cells Increase in intracellular fluid secondary to neuronal, glial, or endothelial cell membrane injury edema is in the cells themselves Fluid accumulated in the intercellular spaces b/c brain has limited lymphatics, therefore lack of resorption Can result from hypoxic/ischemic insult or metabolic damage that prevents maintenance of the membrane ionic gradient Can be either localized (inflammation/neoplasms) or generalized Hydrocephalus Excess CSP in the ventricles usually from impaired flow/resorption or rarely overproduction (tumors of the choroid plexus) CSF Circulation: Choroid plexus ventricles foramina of luschka (lateral aperture) and magendie (median aperture) cisterna magna subarachnoid space arachnoid granulations venous blood back to bodies circulation o Infancy enlargement of head increase in head circumference b/c sutures aren’t closed. Adult enlargement of ventricles w/ ICP w/o change in head circumference. Non-communicating Hydrocephalus Only a portion of ventricles enlarged Possibly from mass in 3rd ventricle Types of Hydrocephalus Communicating Hydrocephalus All of the ventricles are enlarged Hydrocephalus ex vacuo Dilation of ventricles w/ incease in CSF volume due to a loss of brain parenchyma Raised Intracranial Pressure and Herniation Occurs if CSF and Venous drainage cannot compensate for all of the extra fluid Diffuse like generalized brain edema Focal tumors, abscesses, or hemorrhages ICP can cause restriction of vessels exacerbated cerebral edema b/c can’t drain the fluid out if vessel closed off The dural folds of the brain (flax cerebri, tentorium cerebelli, and falx cerebelli) can cause herniation of the cerebrum/cerebellum if bad enough then you can get herniation syndrome Types of Herniation Syndromes Subfalcine (Cingulate) Herniation Transtentorial (Uncinate, Mesial Tonsillar Herniation Temporal) Hernation Unilateral or asymmetric expansion of a cerebral hemisphere displaces the cingulate gyrus under the falx cerebri Can cause compression of the anterior cerebral a. Medial aspect of the temporal lobe is compressed against the tentorium cerebelli Displacement of the cerebellar tonsils through the foramen magnum Can cause problems w/ CN 3 pupillary dilation and inability to move eye on the same side as the lesion Life-threatening due to brainstem compression of respiratory and cardiac centers in the medulla Can cause compression of the posterior cerebral a. hypoperfusion to primary visual cortex Kemohan’s notch Contralateral cerebral peduncle may be compressed hemiparesis on same side of the herniation Secondary brainstem (duret) hemorrhages hemorrhagic lesions in the midbrain and pons due to the herniation