* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Impulsivity-related brain volume deficits in schizophrenia
Executive dysfunction wikipedia , lookup
Neuroesthetics wikipedia , lookup
Cognitive neuroscience of music wikipedia , lookup
Neurogenomics wikipedia , lookup
Environmental enrichment wikipedia , lookup
Dual consciousness wikipedia , lookup
Executive functions wikipedia , lookup
Metastability in the brain wikipedia , lookup
Human brain wikipedia , lookup
Neurophilosophy wikipedia , lookup
Neuropsychology wikipedia , lookup
Emotional lateralization wikipedia , lookup
Neuroeconomics wikipedia , lookup
Persistent vegetative state wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Orbitofrontal cortex wikipedia , lookup
Neuroplasticity wikipedia , lookup
Visual selective attention in dementia wikipedia , lookup
Biology of depression wikipedia , lookup
Cognitive neuroscience wikipedia , lookup
Impact of health on intelligence wikipedia , lookup
Time perception wikipedia , lookup
Brain morphometry wikipedia , lookup
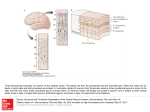
doi:10.1093/brain/awq153 Brain 2010: 133; 3093–3103 | 3093 BRAIN A JOURNAL OF NEUROLOGY Impulsivity-related brain volume deficits in schizophrenia-addiction comorbidity Boris Schiffer,1 Bernhard W. Müller,2 Norbert Scherbaum,2 Michael Forsting,3 Jens Wiltfang,2 Norbert Leygraf1 and Elke R. Gizewski3,4 1 2 3 4 Department Department Department Department of of of of Forensic Psychiatry, University of Duisburg-Essen, Germany Psychiatry and Psychotherapy, University of Duisburg-Essen, Germany Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, Germany Neuroradiology, University Hospital Giessen, Germany Correspondence to: Boris Schiffer, Department of Forensic Psychiatry, University of Duisburg-Essen, Virchow str. 174; 45147 Essen, Germany E-mail: [email protected] Despite a high prevalence of schizophrenia patients with comorbid substance abuse, little is known about possible impacts on the brain. Hence, our goal was to determine whether addicted and non-addicted schizophrenic patients suffer from different brain deficits. We were especially interested to determine if grey matter volumes were affected by impulsivity. We hypothesized that (comorbid) substance abuse would be associated with enhanced impulsivity and that this enhanced impulsivity would be related to grey matter volume deficits in prefrontal areas. We employed a voxel-based morphometry approach as well as neuropsychological assessment of executive functions and trait impulsivity in 51 participants (age range 23–55). The schizophrenia group comprised 24 patients (12 patients with paranoid schizophrenia and 12 with additional comorbid substance use disorders). The comparison group comprised 27 non-schizophrenic individuals, matched by age and education (14 healthy individuals and 13 patients with substance use disorders). Total grey matter volume deficits were found in all patient groups as compared with healthy controls but were largest (8%) in both addicted groups. While grey matter volume losses in lateral orbitofrontal and temporal regions were affected by schizophrenia, volume decreases of the medial orbitofrontal, anterior cingulate and frontopolar cortex were associated with addiction. Compared with non-addicted schizophrenics, comorbid patients showed significant volume decreases in anterior cingulate, frontopolar and superior parietal regions. Additionally, they showed an increased non-planning impulsivity that was negatively related to grey matter volumes in the same regions, except for parietal ones. The present study indicates severe grey matter volume and functional executive deficits in schizophrenia, which were only partially exacerbated by comorbid addiction. However, the relationship between non-planning impulsivity and anterior cingulate and frontopolar grey matter volumes points to a specific structure–function relationship that seems to be impaired in schizophrenia-addiction comorbidity. Keywords: schizophrenia; addiction; structural imaging; executive control; impulsivity Abbreviations: BA = Brodmann area; BIS = Barratt Impulsiveness Scale; DSM = Diagnostic and Statistical Manual of Mental Disorders; FDR = false discovery rate; SZ = non-addicted schizophrenic patients; SZ+A = comorbid patients (addicted schizophrenics); WCST = Wisconsin card sorting task Received February 1, 2010. Revised April 29, 2010. Accepted May 6, 2010. Advance Access publication July 20, 2010 ß The Author (2010). Published by Oxford University Press on behalf of the Guarantors of Brain. All rights reserved. For Permissions, please email: [email protected] 3094 | Brain 2010: 133; 3093–3103 Introduction Comorbid substance abuse in patients with schizophrenia is very common. Approximately 50% of these patients fulfil the criteria for both schizophrenia and substance use disorder over their lifetime (Regier et al., 1990). However, persisting comorbid substance abuse is associated with a negative outcome. This includes an overall reduced quality of life, more frequent and longer periods of hospitalization, higher relapse rates, less treatment compliance and higher incidence of violent behaviour (Fazel et al., 2009). Despite these adverse outcomes in schizophrenia-addiction comorbidity, little is known about its actual impacts on the brain or their functional relevance. However, structural brain abnormalities in schizophrenia were identified by using voxel-based morphometry that revealed impairments, especially in frontotemporal cortices (Davatzikos et al., 2005; Honea et al., 2005; Williams, 2008). Most voxel-based morphometry studies to date have focused on chronic patients and showed rather consistent volume decreases in superior and medial temporal cortices (Honea et al., 2005; Williams, 2008). Moreover, there is accumulating evidence for volume reductions in frontal brain regions (Williams, 2008) resulting from meta-analyses of studies regarding first-episode schizophrenia and other high-risk groups, such as first-degree relatives. Apart from alcohol misuse, substances commonly abused in schizophrenic patients include nicotine, cocaine and cannabis (Winklbaur et al., 2006). These substances are reinforced by an increased dopaminergic activity, particularly in the mesolimbic dopamine system (Gerdeman et al., 2003). As substance abuse increases the mesolimbic dopamine activity (Gerdeman et al., 2003) and leads to neurotoxic damage within frontosubcortical circuits in the long term (Spanagel and Heilig, 2005), it may exacerbate the presumed pre-existing dysregulation of the dopamine system and cause an additional disruption within frontosubcortical circuits in patients with schizophrenia (Siever and Davis, 2004). Furthermore, recent structural magnetic resonance imaging (MRI) studies documented morphological changes in the frontal lobe of patients suffering from different types of drug addiction (Jernigan et al., 1991; Liu et al., 1998; Chanraud et al., 2007). Unfortunately, only a few studies on brain dysmorphology in addicted and non-addicted schizophrenic patients have been carried through and these have mainly focused on alcohol abuse. Furthermore, their results were partly inconclusive. While a recent study did not show significant differences between schizophrenic patients with and without comorbid alcoholism (Wobrock et al., 2009), the largest study (Mathalon et al., 2003) at hand documented a compounding, additive effect in schizophreniaalcoholism comorbidity in prefrontal cortex areas, important for cognitive functioning. Regarding cognition, both schizophrenia and substance use disorders are related to functional impairment (Bowie and Harvey, 2005; Lundqvist, 2005; Minzenberg et al., 2009). However, little is known about the status of cognitive and executive functions in comorbid patients. Executive functions represent supervisory cognitive coordination processes allowing for flexible, goal-directed behaviour, particularly in novel situations (Norman and Shallice, B. Schiffer et al. 1986). They depend upon the functional integrity of frontosubcortical circuits that are affected both in schizophrenia (Camchong et al., 2006) and substance use disorders (Garavan and Stout, 2005). It has been suggested that goal-directed behaviours of addicted patients in addiction relevant situations are mainly driven by automatic processes and that their ability to interrupt the maladaptive automatic schemata is disturbed (Tiffany, 1990). Continuing abstinence requires the ability to inhibit automatic response routines leading to drug consumption and the ability to shift the cognitive focus to alternative behaviours and goals. Accordingly, poor response inhibition, as part of the impulsivity concept, has been found to predict problem drinking and illegal drug use (Nigg et al., 2006). Thus, the impulsivity construct is of central importance for substance use disorders or schizophrenia-addiction comorbidity (Moeller et al., 2002). It can be conceptualized as a personality trait, characterized by acting quickly and without planning in order to satisfy a desire (Kreek et al., 2005). Hence, impulsivity is a complex, multifaceted construct including cognitive, personality and behavioural components (e.g. risk taking, sensation seeking and behavioural disinhibition) (Nigg, 2000). Impulsivity has been related to an early use of illegal substances, a high susceptibility to developing a substance use disorder (Tarter et al., 2003) and a decrease of local grey matter volumes, particularly in orbito-frontal regions (Matsuo et al., 2009). These findings indicate that comorbid patients should show more distinct executive deficits and in particular, higher trait impulsivity than non-addicted schizophrenics. Yet, while studies regarding impulsivity are still lacking, studies regarding executive functions revealed inconclusive results (Addington and Addington, 1997; Pencer and Addington, 2003; Herman, 2004; Bowie et al., 2005). The present investigation therefore sought to determine whether executive functions and trait impulsivity show different impairments in patients with schizophrenia, with and without comorbid substance use disorder, and especially, whether or how brain volumes are associated with impulsivity. We hypothesized that (comorbid) substance abuse would be associated with enhanced trait impulsivity and that this enhanced impulsivity would be correlated with grey matter volume deficits in prefrontal areas or frontosubcortical circuits, relevant for executive control. Methods Subjects A total of 51 male individuals (age range 23–55 years) were recruited for this study. The schizophrenia group comprised 24 chronic patients, diagnosed as having Diagnostic and Statistical Manual of Mental Disorders, fourth edition paranoid schizophrenia (DSM IV: 295.30) and was subdivided into two subsamples. The comorbid sample (SZ+A) comprised 12 paranoid schizophrenic patients who had a history of alcohol dependence (DSM IV: 303.90) and a misuse of substances other than alcohol: cannabis (n = 3; DSM IV: 305.20), medicinal drugs (n = 1; DSM IV: 305.40), stimulants (n = 1; DSM IV: 305.70) or multiple substances (n = 5; DSM IV: 304.80). The ‘SZ’ sample comprised 12 patients with paranoid schizophrenia without VBM in schizophrenia-addiction comorbidity current or lifetime alcohol or other substance problems, except for nicotine. Patients were recruited from the outpatient care of the Department of Psychiatry and Psychotherapy, University of Duisburg-Essen, and underwent medical screening and psychiatric assessment. Diagnosis was based on consensus between a research psychologist conducting a clinical interview and a trained research assistant implementing the Structured Clinical Interview for DSMIV (SCID-I and SCID-II) (Wittchen et al., 1996). Symptom severity was evaluated using the Positive and Negative Syndrome Scale (Kay et al., 1987), executed by two raters with an established inter-rater reliability (mean Pearson’s correlation: 0.758). All schizophrenic patients were taking antipsychotic medication [typical (n = 1), atypical (n = 12), typical and atypical (n = 11)] and were physically healthy at the time of scanning and testing. The comparison group comprised 27 non-schizophrenic individuals and was also subdivided into two subsamples. The addicted patients sample comprised 13 patients with a history of alcohol dependence (DSM IV: 303.90) and was matched with the comorbid sample regarding other substances than alcohol abused over their lifetime: cannabis (n = 4; DSM IV: 305.20), opiates (n = 1; DSM IV: 305.50), stimulants (n = 1; DSM IV: 305.70), multiple substances (n = 5; DSM IV: 304.80). They were recruited from specialized aftercare facilities in Essen. The healthy control group sample (n = 14), recruited by advertisement and local employment agencies, was screened via telephone and then assessed by implementing structured psychiatric SCID interviews. The healthy control group was excluded for Axis I psychopathology or lifetime history of substance abuse. Both non-schizophrenic groups were matched by age, education level and duration of substance abuse or dependence, where appropriate. They did not have a first-degree relative with psychotic episodes. Eighty-three percent (n = 20) of the schizophrenic patients and 78% (n = 21) of the non-schizophrenic group smoked. General exclusion criteria included a history of significant medical or neurological illness, head injury resulting in loss of consciousness (430 min), inadequate knowledge of the German language, left-handedness and mental retardation (IQ 590), which was tested with a multiple choice vocabulary test (Mehrfachwahl–WortschatzIntelligenztest-B, an indicator of pre-morbid abilities) (Lehrl et al., 1995). All patients with a history of substance abuse had not consumed any substances for at least 1 year (supported by urine analysis). Table 1 (upper half) presents demographic and clinical characteristics of the study participants. The study was approved by the local Committee on Medical Ethics of the Medical Faculty of the University of Duisburg-Essen, Germany and was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki, amended by the 55th WMA General Assembly, Tokyo, 2004). After a detailed description of the study, written informed consent was obtained from all participants. Assessment of addiction severity The Michigan Alcohol Screening Test (Selzer, 1971) and the Drug Abuse Screening Test-20 (Skinner, 1982) were used to quantify the exposure to alcohol and illegal drugs. The Michigan Alcohol Screening Test was developed as a quick and effective screening method for lifetime alcohol-related problems and alcoholism, and consists of 25 items. The Drug Abuse Screening Test-20, a shortened version of the 28-item Drug Abuse Screening Test, designed to identify drug-use related problems, was also used as a lifetime measure. Brain 2010: 133; 3093–3103 | 3095 Cognition and impulsivity assessments All participants underwent neuropsychological assessments to explore different executive domains (cognitive flexibility, response inhibition, planning and visuospatial memory) and trait impulsivity. The Trail Making Test (Reitan and Wolfson, 1985) and a computerized version of the modified Wisconsin Card Sorting Task (WCST) (Nelson, 1976) were used to assess the ability to alter a behavioural response mode in case of changing contingencies [reactive cognitive flexibility (set-shifting)]. Furthermore, a test of verbal fluency was applied to measure spontaneous cognitive flexibility and speed of access to semantic information (in this study, animals with a given time period of 60 s). The Corsi block tapping Test (Schellig, 1997) and the visual reproduction task from the Wechsler Memory Scale, Revised (Wechsler, 1987) were applied to assess visuospatial memory. Inhibition performance was assessed by the number of perseverative errors in the WCST and a Go/No-go task, taken from a German standard battery (Zimmermann and Fimm, 2009). A computerized Tower of London task (Schall et al., 2003), an adaptation of the Tower of Hanoi, was used to measure the planning behaviour of our study participants. And finally, to quantify impulsivity, we used the Barratt Impulsiveness Scale (BIS-11) (Barratt, 1994), which is regarded as the most commonly used self-report measure of impulsivity. In its revised form, it results in a total score and three subscale scores: attention, motor and non-planning impulsivity (Patton et al., 1995). Cognitive and impulsivity measures and their relationship to local grey matter volumes To characterize the patients and test our hypothesis regarding impulsivity, we had to aggregate the information derived from the comprehensive test battery comprising many different dependent variables. Based on theoretical assumptions and validated by factor analysis, we therefore subsumed selected variables under five domains of executive functions (as described below) and computed positively connoted (i.e. the higher the value, the better the performance) mean zscores for each, which according to our prior hypothesis were partly used as covariates in the voxel-based morphometry analyses: (i) Reactive cognitive flexibility: WCST number of categories achieved, WCST total number of errors [with reversed signs (wrs)], Trail Making Test–B mean reaction time (wrs) and Trail Making Test set shifting costs (wrs). (ii) Spontaneous cognitive flexibility: category fluency number of words and number of perseverations (wrs). (iii) Visuospatial memory: Corsi block span, Wechsler Memory Scale, revised visual reproduction (immediate recall). (iv) Inhibition: WCST number of perseverative errors (wrs) and number of errors in the Go/No-go task (wrs); (v) Planning: Tower of London number of correct solutions and mean first reaction time for each trial (wrs). Image acquisition Brain images were acquired on a 1.5T MRI system (Siemens Sonata, Erlangen, Germany) using a 3D T1-weighted sequence (magnetization prepared rapid gradient echo) with the following parameters: repetition time = 1900 ms; echo time = 3.93 ms; flip angle = 15 ; 160 3096 | Brain 2010: 133; 3093–3103 B. Schiffer et al. Table 1 Demographic, clinical, executive, impulsivity and brain volume measures of study participants Healthy controls (n = 14) Addicted patients (n = 13) Schizophrenic patients (n = 12) Co-morbid patients (n = 12) Overall statistical test P-value Post hoc comparison (P _ 0.05, Bonferroni-adjusted) Age (years) 36.7 11.4 37.3 7.9 37.8 9.0 37.2 7.3 ANOVA 0.96 NA School education (years) 9.93 0.99 9.69 1.44 9.33 1.44 9.75 1.66 ANOVA 0.91 NA Age at schizophrenia onset (years) NA NA 21.0 5.3 25.5 4.9 t-test 0.04 NA Duration of illness (years) NA NA 16.8 7.2 11.6 6.8 t-test 0.08 NA Measure Demographic Clinical Chlorpromazine equiv. (mg/day) NA NA 672.3 383 608.8 392 t-test 0.69 NA PANSS positive NA NA 14.6 4.1 16.0 4.8 t-test 0.45 NA PANSS negative NA NA 20.5 4.5 18.7 5.0 t-test 0.36 NA PANSS general NA NA 31.9 5.9 35.8 7.5 t-test 0.18 NA Michigan alcohol screening test 1.6 2.3 14.2 6.9 3.7 3.9 13.1 6.6 ANOVA 0.00 SZ + A = SUD 4 HC = SZ Drug abuse screening test 0.9 0.9 12.8 6.3 3.8 3.9 9.7 6.2 ANOVA 0.00 SZ + A = SUD 4 HC = SZ Duration of substance abuse (years) NA 11.2 5.3 NA 13.0 5.0 t-test 0.39 NA Abstinence duration (years) NA 1.6 0.5 NA 3.2 2.4 t-test 0.04 NA 109.9 11.7 106.4 6.0 102.2 8.2 102.7 9.4 ANOVA 0.12 NA Premorbid IQ (MWT-B) Executive functions (z-scores) Reactive cognitive flexibility 0.49 0.39 0.28 0.65 0.54 0.95 0.33 0.99 ANOVA 0.00 HC 4 SZ+A = SZ; SUD 4 SZ Spontaneous cognitive flexibility 0.29 0.89 0.47 1.17 0.41 0.76 0.44 0.88 ANOVA 0.03 HC = SUD 4 SZ = SZ + A Visuospatial working memory 0.52 0.30 0.07 0.31 0.77 1.34 0.09 0.82 ANOVA 0.00 HC = SUD = SZ+A4SZ Inhibition 0.29 0.19 0.02 0.37 0.03 0.40 ANOVA 0.05 HC 4 SUD Planning 0.47 0.37 0.20 0.52 ANOVA 0.00 HC = SUD 4 SZ+A BIS-11 total score 63.3 6.8 69.8 7.1 65.7 8.5 72.8 11.0 ANOVA 0.05 SZ + A = SUD 4 HC BIS-11 motor 23.6 3.6 23.4 3.0 22.5 3.6 24.8 4.3 ANOVA 0.59 NA BIS-11 attention 15.0 2.7 18.6 3.5 18.4 3.4 18.8 3.7 ANOVA 0.04 SZ + A = SZ = SUD 4 HC BIS-11 non-planning 24.7 4.3 27.9 3.1 24.9 4.6 29.2 4.9 ANOVA 0.03 SZ + A4HC = SZ 0.32 0.61 0.17 0.81 0.60 0.75 Impulsivity Global volume measure (cm3) Total brain volume 1767.4 181.4 1753.5 77.2 1782.2 184.3 1747.9 136.7 ANOVA 0.95 NA Total grey matter volume 713.6 59.7 649.8 56.4 696.8 59.6 654.4 76.3 ANOVA 0.03 HC4SUD = SZ+A Adjusted grey matter volumea 712.8 39.0 652.8 55.7 690.5 41.7 659.1 58.6 ANOVA 0.01 HC4SUD = SZ+A Total white matter volume 529.4 80.6 517.1 36.9 539.0 59.7 512.9 49.4 ANOVA 0.73 NA Total CSF volume 524.4 77.4 586.7 78.3 546.4 113.6 580.7 76.1 ANOVA 0.24 NA Data are mean SD. HC = healthy controls; SUD = non-schizophrenic addicted patients; NA = not applicable; PANSS = Positive and Negative Syndrome Scale; MWT-B = multiple choice vocabulary test. a Grey matter volume adjusted by brain-size (i.e. each individual’s total brain volume). Significant P-values are stated in bold type. contiguous 1 mm sagittal slices; field of view = 240 mm 240 mm, matrix size = 240 240, voxel size = 1.0 0.9 1.0 mm. Voxel-based grey matter volume analysis (local approach) Data were processed using the SPM5 software (Welcome Department of Imaging Neuroscience Group, London, UK; http://www.fil.ion.ucl. ac.uk/spm). We applied voxel-based morphometry standard routines and default parameters implemented in the voxel-based morphometry 5 toolbox (http://dbm.neuro.uni-jena.de/vbm.html). Images were bias field corrected, tissue classified and registered using linear (12-parameter affine) and non-linear transformations (warping) within the same generative model (Ashburner and Friston, 2005). Analyses were performed on grey matter segments, which were multiplied by the non-linear components derived from the normalization matrix in order to preserve actual grey matter values locally (modulated grey matter volumes). Grey matter segments were not multiplied by the linear components of the registration in order to account for individual differences in brain orientation, alignment and size globally. Finally, the modulated grey matter volumes were smoothed with a Gaussian kernel of 14 mm full width at half maximum. These smoothed, modulated grey matter volumes are referred to as grey matter. Total brain and grey matter volume analysis (global approach) Using the tissue-classified partitions from the voxel-based morphometry analysis [i.e. grey matter, white matter and cerebrospinal fluid (CSF)], overall volumes were determined in cm3 as the sum of voxels representing grey matter + white matter + CSF (total brain volume), total grey matter volume, total white matter volume and total CSF volume. VBM in schizophrenia-addiction comorbidity Statistical analysis Group differences for all demographic, clinical, executive, impulsivity and total volume measures were analysed by means of t-tests and ANOVAs, followed by post hoc analyses with Bonferroni corrections. Voxel-wise grey matter differences between single groups (healthy controls versus all clinical groups and all clinical groups with each other) were examined by using independent-sample t-tests. In order to avoid possible edge effects between different tissue types, we excluded all voxels with grey matter values of 50.1 (absolute threshold masking). Statistical outcomes for the effects of the full-factorial model, the independent-sample t-tests and the correlation analyses were corrected, unless stated otherwise, using false discovery rate (FDR) corrections for multiple comparisons. All significant outcomes were restricted to clusters exceeding different numbers of voxels (spatial extent threshold) in order to decrease the risk of detecting spurious effects due to noise. The spatial extent threshold corresponds to the expected number of voxels per cluster, calculated according to the theory of Gaussian random fields. Although all four groups were carefully matched by age, we conducted all voxel-based morphometry analyses while co-varying for age to rule out according effects. In order to test our hypothesis that impulsivity would be related to substance abuse as well as grey matter volume decreases in prefrontal areas, we used the mean z-scores of all behavioural impulsivity-related executive measures (i.e. planning and inhibition) and all BIS scores as separate covariates in full-factorial models. We computed a correlation analysis for each, i.e. we performed post hoc Pearson correlations between these variables and the non-adjusted grey matter estimates of co-varying regions. Due to the numerous statistical comparisons or correlation analyses, we considered only those with a type one error of P50.01 in order to minimize the probability to detect false positives. In absence of specific refutable a priori hypothesis for all other executive domains, these were used only to characterize the groups. Results Demographic and clinical data One way ANOVAs of the demographic and clinical variables (Table 1) across the four groups did not yield significant differences for age, education or any relevant clinical measure, except illness onset. Further, as indicated by post hoc analysis, the severity of alcohol consumption (Michigan Alcohol Screening Test) and illegal drug use (Drug Abuse Screening Test) of both addicted groups exceeded that of non-addicted subjects but was comparable between addicted subjects. Executive functioning and impulsivity data While the pre-morbid IQ did not differ between groups, significant group differences were found for all executive measures (Table 1). A significant schizophrenia effect was found for reactive and spontaneous cognitive flexibility. As indicated by the post hoc analysis, both schizophrenic groups showed weaker performances on both measures compared with healthy controls. Brain 2010: 133; 3093–3103 | 3097 We found a significant group effect between addicted (non-schizophrenic) patients and healthy controls for the inhibition domain. The post hoc analysis revealed that addicted patients differed significantly from healthy individuals and showed the largest deficit in this domain. However, the most distinct deficit in comorbid patients was observed for the planning domain. Comorbid patients, compared with non-schizophrenic subjects, showed significantly weaker performances. Regarding BIS-11 impulsivity measures, we found significant between-group differences in all scales, except for motor impulsivity (Table 1). As shown in the post hoc analysis, the BIS total score showed that both addicted groups achieved comparable values but significantly higher ones than the healthy subjects. Corresponding to the cognitive domain planning, the BIS non-planning scale showed the most distinct deficit in comorbid patients. Comorbid patients achieved significantly higher nonplanning impulsivity than healthy controls and non-addicted schizophrenics, but did not differ from addicted patients. Global volume measures Groups did not differ with respect to total brain volume, white matter or CSF but in total grey matter volume (Table 1). However, both addicted groups, compared with the healthy control group, showed a significant, and 8% (SZ+A = 7.5%, addicted patients = 8.4%) decreased brain-size adjusted grey matter volume (i.e. adjusted by each individuals’ total brain volume). Nonaddicted schizophrenics showed a 3.1% decrease. Local grey matter volumes In order to identify relevant group differences, we performed separate two sample t-tests between healthy subjects and all clinical groups (Fig. 1, Table 2) as well as between all clinical groups (Table 3). All three clinical groups revealed grey matter volume decreases in several frontotemporal clusters as compared with healthy controls. Moreover, addicted patients, compared with healthy controls (healthy controls 4 addicted patients), showed large additional grey matter volume decreases in the anterior cingulate cortex and the frontopolar region. The comorbid patients showed similar but less severe deficits than the addicted patients, whereas non-addicted schizophrenics did not show any decreases (Table 2). Both schizophrenia groups differed significantly in four areas (Table 3; Fig. 2). Corresponding to the healthy controls 4 SZ+A contrast, the SZ 4 SZ+A contrast revealed significant grey matter volume differences in the anterior cingulate cortex, the left frontopolar region and the left superior parietal lobule. However, the reversed contrast (SZ+A4SZ) revealed significant differences only in the right temporopolar cortex [Brodmann area (BA) 38]. Due to the age matching procedure in both schizophrenic groups and their differences in illness onsets, we found between-group differences in illness durations. In order to take these into account we calculated an additional model with illness duration as a covariate. The results showed that the anterior cingulate volume difference lost its significance, at least when FDR 3098 | Brain 2010: 133; 3093–3103 B. Schiffer et al. Figure 1 Areas of decreased grey matter volume in addicted patients (red), non-addicted schizophrenic patients (blue) and comorbid patients (green) as compared with healthy controls. Decreased grey matter volumes in all clinical groups, compared with healthy controls, co-varied for age [corrected for multiple comparisons, FDR P50.05; t44.13; extent threshold of 200 (healthy controls 4 addicted patients = 198; healthy controls 4 SZ = 170; healthy controls 4 SZ+A = 212) = expected voxels per cluster] as resulted from the independent sample t-tests between healthy controls and the three clinical groups. The results are visualized with the MRIcroN software by C. Rohden, 2009 (http://www.cabiatl.com/mricro). Areas of decreased grey matter volumes in the three clinical groups compared with healthy controls are overlaid in different colours on a standard T1-template embedded in the MRIcroN software and presented in neurological convention (right is right). corrected for multiple comparisons. However, the influence of illness duration was small as the trend remained (FDR P50.068). Correlation analyses between local grey matter volumes and impulsivity-related measures (executive domains: inhibition, planning and BIS scores) Regarding the executive domain inhibition, correlation analyses revealed a common positive relationship between inhibition performance and left frontopolar (BA 10), left anterior cingulate cortex (BA 32), medial orbitofrontal cortex (BA 11) and superior temporal cortex (BA 38) volumes for all groups. This result corresponds with our finding that addicted patients showed the most distinct volume decreases in these areas and also revealed the largest performance deficit in this domain. The planning performance, which was largely impaired in comorbid patients, was positively correlated with left medial orbitofrontal cortex (BA 11) and right anterior cingulate cortex (BA 24, 32) volumes in all groups. This result partly corresponds with the finding that comorbid patients also showed volume decreases in orbitofrontal cortex and anterior cingulate cortex volumes, compared with non-addicted schizophrenics and/or healthy controls. Regarding the correlative relationships between BIS impulsivity measures and local grey matter volumes, the most distinct associations could be observed for the left dorsolateral prefrontal cortex volumes (BA 9, Montreal Neurological Institute coordinates: 56, 22, 33), which were negatively correlated with the BIS total score (k = 53, FDR P50.03; r = 0.439, P50.01) and all BIS subscales (motor impulsivity: k = 161, FDR P50.02; r = 0.454, P50.01; non-planning impulsivity: k = 479, FDR P50.05; r = 0.466, P50.01) except attentional impulsivity. However, the attentional impulsivity was negatively correlated with the left supplementary motor cortex volume (BA 6, Montreal Neurological Institute coordinates: 23; 17; 61, k = 123, FDR P50.05; r = 0.478, P50.01). Besides the dorsolateral prefrontal cortex volume correlations, the motor impulsivity was additionally negatively correlated with right medial orbitofrontal cortex volumes (BA 11, Montreal Neurological Institute coordinates: 17; 42; 28, k = 74, FDR P50.02; r = 0.438, P50.01) and the non-planning impulsivity showed an additional negative correlation with left frontopolar volumes (BA 10). This corresponds to the finding that compared with healthy controls and non-addicted schizophrenics, addicted groups showed both the highest non-planning impulsivity and grey matter volume decreases. Scatter plots illustrating the correlation patterns between local grey matter volumes and inhibition and planning performance as well as non-planning impulsivity are provided in Supplementary Fig. 1. VBM in schizophrenia-addiction comorbidity Brain 2010: 133; 3093–3103 | 3099 Table 2 Grey matter volume differences between healthy controls and clinical groups (n = 51) as demonstrated by separate two sample t-tests (t44.13) covaried for age Group Brain region BA MNI coordinates x HC Medial orbitofrontal cortex Lateral orbitofrontal cortex Ventrolateral prefrontal cortex Dorsolateral prefrontal cortex Anterior cingulate cortex Frontopolar cortex Parahippocampal gyrus Middle temporal cortex Inferior temporal cortex Superior temporal cortex Angular gyrus Superior parietal lobule Cuneus Middle occipital cortex 11,47 11,47 47 47 47 45,47 6,8 6,8 6 24,32 24,32 9,10 10 10 10 27,30 28,35 39 20,21 20 20 20 20 38 38 39 7,19 18 18,19 19 y 13 13 35 42 51 52 14 11 7 7 2 8 24 13 30 13 22 49 65 34 57 33 60 31 45 35 35 5 10 40 Side Z 29 26 25 27 24 27 33 35 6 37 33 53 56 60 51 40 20 71 38 14 31 8 21 4 5 75 72 83 91 81 4 SUD 4 SZ P Cluster size 24 26 15 20 6 2 52 54 73 22 19 27 25 16 11 0 19 8 4 32 28 44 34 43 17 33 48 8 22 10 L R R R L L R L R R L R R L L R L L R R L L L R R L L L R R 3476 714 Cluster size 4 SZ+A P 0.005* 0.006* 823 13136 0.006* 0.005* 0.005* 615 1000 205 2395 498 452 0.009* 0.009* 0.008* 0.008* 0.005* 0.005* 0.006* 231 209 0.008* 0.008* 390 0.005* 13748 0.005* 0.005* 0.005* 2584 3131 3675 0.033 0.033 237 0.033 489 334 0.033 0.033 990 221 0.033 0.033 217 1291 171 517 0.033 0.033 0.033 0.033 Cluster size P 539 1002 498 312 0.021 0.021 0.021 0.022 214 0.024 974 636 261 234 0.020 0.038 0.040 0.040 337 0.034 327 9534 0.022 0.013 719 0.021 957 0.021 HC = healthy controls; SUD = non-schizophrenic addicted patients; MNI = Montreal Neurological Institute. *FWEcorrected P50.05. For the reversed contrasts (SUD 4 HC, SZ 4 HC and SZ+A 4 HC) significant differences were absent. Table 3 Grey matter volume differences between all clinical groups (n = 37) as demonstrated by separate two sample t-tests co-varied for age Contrast Brain regions Side BA MNI coordinates x SZ 4 SZ+A Superior parietal lobule Anterior cingulate cortex L L 7 32 SZ+A 4 SZ Frontopolar cortex Superior temporal cortex L R 10 38 SUD 4 SZ+A SZ+A 4 SUD No region Frontopolar cortex SUD 4 SZ SZ 4 SUD Superior temporal cortex Frontopolar cortex Dorsolateral prefrontal cortex Lingual gyrus Cuneus Supplementary motor cortex y Cluster size *P 647 187 152 282 385 0.042 0.047 0.048 0.025 0.048 z 37 7 15 41 32 65 17 31 59 4 54 45 27 12 50 R 10 9 60 4 511 0.038 R R R R L L R R L 38 10 46 9 46 18 18 6 6 32 41 45 36 49 9 2 5 1 3 53 37 46 36 69 90 21 28 45 6 19 34 9 0 12 68 67 455 397 722 624 731 686 360 387 282 0.044 0.039 0.039 0.039 0.039 0.039 0.039 0.039 0.039 SUD = non-schizophrenic addicted patients; MNI = Montreal Neurological Institute. *FDRcorrected P50.05. 3100 | Brain 2010: 133; 3093–3103 B. Schiffer et al. Figure 2 Grey matter volume differences between schizophrenic patients with and without comorbid substance use disorder covaried for age (corrected for multiple comparisons, FDR P50.05; extent threshold = 113 = expected voxels per cluster), as resulted from the independent sample t-test. The colour intensity represents t-statistic values at the voxel level. The results are visualized on standard normalized T1-weighted images in selected slices and displayed in neurological convention (right is right). Discussion While previous studies assessing brain volumes in schizophreniaaddiction comorbidity focused on structural effects, here we also examined the structure–function relationship between local grey matter volumes and impulsivity. Grey matter volume deficits were found in all clinical groups compared with healthy controls, but were largest in both addicted groups (8%). However, while temporal and lateral orbitofrontal cortex deficits rather correspond to the schizophrenia diagnosis, the medial orbitofrontal cortex, anterior cingulate cortex, dorsolateral prefrontal cortex and frontopolar volume decreases show more corresponding elements with addiction. Furthermore, as hypothesized, we observed enhanced addiction-related impulsivity which was correlated mainly with the same local grey matter volumes as addiction-related decreased. In accordance with this, comorbid patients compared with non-addicted schizophrenics showed significant volume decreases in the left anterior cingulate cortex and frontopolar cortex. Additionally, and in line with previous studies (Matsuo et al., 2009), the medial orbitofrontal cortex, which showed volume decreases in both addicted groups compared with healthy controls, was also correlated with most of the impulsivity-related measures. As indicated by both the self-report measure (BIS score: non-planning impulsivity) and the behaviourally assessed executive domain planning, comorbid patients showed the largest abnormality regarding non-planning impulsivity. These were, except the dorsolateral prefrontal cortex, related to the same grey matter volumes as the inhibition performance, where the addicted patients group showed their largest impairments: orbitofrontal cortex, anterior cingulate cortex and frontopolar volumes (Matsuo et al., 2009; Minzenberg et al., 2009). However, the result that both addicted groups showed significant structural decreases implies a structure–function relationship between these areas and two dimensions of impulsivity (disinhibition and non-planning) which seem to be strongly related to addiction, as has been reported previously for drug abuse (Jentsch and Taylor, 1999). All of these areas are part of different behaviourally relevant frontosubcortical circuits, the superior medial frontosubcortical circuit (anterior cingulate and frontopolar cortex) and the medial orbitofrontal cortex frontosubcortical circuit (Chow and Cummings, 2007). Each of these interconnected networks comprises projections to the ventral striatum (including ventromedial caudate, ventral putamen, nucleus accumbens), globus pallidus and substantia nigra as well as ventroanterior and dorsomedial nuclei of the thalamus, and closes with projections back to the anterior cingulate cortex and the medial orbitofrontal cortex. While the medial orbitofrontal cortex frontosubcortical circuit was associated with dysregulation of affect, social behaviour and impulsivity in previous studies (Chow and Cummings, 2007), the superior medial frontosubcortical circuit, especially the anterior cingulate cortex, is known to be of central importance for cognitive control (Kerns et al., 2004; Ridderinkhof et al., 2004) and apathy or amotivational syndrome (Chow and Cummings, 2007). As suggested previously (Spanagel and Heilig, 2005) the disruption of parts of the frontosubcortical circuits in (comorbid) addiction might contribute to the more negative outcome in terms of enhanced impulsivity and antisocial/violent behaviours in addicted and dual-diagnosis patients (Fazel et al., 2009). Although not significant, comorbid patients had increased grey matter total volumes compared with addicted non-schizophrenic patients. This might be due to the fact that compared with patients with dual diagnosis, addicted non-schizophrenic patients showed a more severe substance use problem, especially with illegal drugs, and were abstinent only for half as long as comorbid VBM in schizophrenia-addiction comorbidity patients. This, in combination with the fact that both addicted groups in the present study had not used substances for at least one year, may also explain the differences between our results and those reported previously (Mathalon et al., 2003), where this was not a prerequisite (abstinence duration: alcoholics median = 33 days, comorbid patients = none abstinent). In the present study, the addicted patients group showed the largest volume decreases, thus contrasting with the results of Mathalon et al. (2003), which showed that the comorbid group suffered from the largest volume decreases. It is known that alcohol-induced volume decreases partially recover after a 6–9 month period after cessation of drinking (Cardenas et al., 2007), thus showing early effects of abstinence (after a few weeks) (Bartsch et al., 2007). However, it is questionable whether complete brain regeneration is possible after having been abstinent for a longer period, or whether the brain recovers from long-term illegal drug use. To clarify this issue, we conducted additional correlation analyses between local grey matter volumes and substance abuse related measures that, except for dependency duration, failed to show significant relationships. Even though the sample size was small, our results indicate a progressive process of grey matter volume losses in frontopolar, middle temporal and cerebellar regions over dependency duration. Additionally, in absence of a positive correlation between abstinence duration and grey matter volumes, they also indicate a steady recovery state in both addicted groups after cessation of drinking or consuming illegal drugs within at least one year. In agreement with previous findings (Honea et al. 2005), the most consistent grey matter volume reduction in patients with chronic schizophrenia was found in the right superior temporal cortex (including the temporal pole). However, non-addicted schizophrenics, compared with healthy subjects (healthy controls 4 SZ) and with comorbid patients (SZ+A 4 SZ), showed a significant volume decrease in the temporal pole known to be crucial for theory of mind or social cognition (Frith and Frith, 2003). While structural and theory of mind-related functional abnormalities in the temporal poles have been previously observed in schizophrenia (Benedetti et al., 2009), the absence of such theory of mind-related structural impairments in comorbid patients might indicate that comorbid addiction would be associated with preserved mentalizing abilities in schizophrenia, especially as there is evidence showing that dual-diagnosis patients have better social skills than non-addicted schizophrenic patients (Carey et al. 2003). Yet, some methodological concerns of this study should be considered. Firstly, with respect to correlation analyses in voxel-based morphometry studies, performance in specific cognitive domains may only be modulated in part by structural alterations. Secondly, the sample sizes of the subgroups in our experiment were rather small and the variation of substance categories may contribute variation in some measures (e.g. neuropsychological performance). While this design enables the conjoined analysis of two major clinical dimensions, the variations of substance categories may preclude replication of some effects of comorbidity noted from the existing literature and to that extent have to be replicated in larger samples without such a variation. A further specific characteristic of our sample was that both addicted groups had been abstinent Brain 2010: 133; 3093–3103 | 3101 for at least 1 year. Assuming that major recovery processes occur within the first year of abstinence, our results suggest a larger stability over time compared with results of patient groups that had been abstinent for shorter periods. Therefore, the reported grey matter volume decreases in these groups are limited to those that persist in spite of abstinence for longer than at least 1 year. Conclusions As hypothesized, the results of the present study indicate an increased non-planning impulsivity in addicted, especially dual-diagnosis patients, which is related to grey matter volume losses in medial orbitofrontal cortex, dorsolateral prefrontal cortex, anterior cingulate cortex and frontopolar regions. However, in contrast to non-addicted schizophrenics, comorbid patients showed exacerbated volume decreases only in the anterior cingulate cortex and frontopolar region but not in the medial orbitofrontal cortex or the dorsolateral prefrontal cortex. The previously reported finding, that substance abuse comorbidity represents the main risk factor of schizophrenic patients to become violent (Fazel et al., 2009), corresponds to the hypothesis that violence is associated with impulsivity that was increased in both addicted groups. Finding this structural relationship between substance abuse, non-planning impulsivity and anterior cingulate and frontopolar volumes in dual-diagnosis patients is of clinical importance and requires further investigation with functional MRI approaches. Acknowledgements Christina Pawliczek, MSc, and Alexander Wormit, cand. med., assisted with the data collection and analysis. Funding This work was supported by a grant from the Landschaftsverband Rheinland, Germany (Dr Schiffer). The Landschaftsverband Rheinland participated in the design and conduct of the study and the collection and analysis of the data with the support of Dr Schiffer. Supplementary material Supplementary material is available at Brain online. References Addington J, Addington D. Substance abuse and cognitive functioning in schizophrenia. J Psychiatry Neurosci 1997; 22: 99–104. Ashburner J, Friston KJ. Unified segmentation. Neuroimage 2005; 26: 839–51. 3102 | Brain 2010: 133; 3093–3103 Barratt ES. Impulsiveness and aggression. In: Monahan J, Steadman HJ, editors. Developments in risk assessment. Chicago: University of Chicago Press; 1994. p. 61–79. Bartsch AJ, Homola G, Biller A, et al. Manifestations of early brain recovery associated with abstinence from alcoholism. Brain 2007; 130: 36–47. Benedetti F, Bernasconi A, Bosia M, et al. Functional and structural brain correlates of theory of mind and empathy deficits in schizophrenia. Schizophr Res 2009; 114: 154–60. Bowie CR, Harvey PD. Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr Clin North Am 2005; 28: 613–33, 626. Bowie CR, Serper MR, Riggio S, Harvey PD. Neurocognition, symptomatology, and functional skills in older alcohol-abusing schizophrenia patients. Schizophr Bull 2005; 31: 175–82. Camchong J, Dyckman KA, Chapman CE, Yanasak NE, McDowell JE. Basal ganglia-thalamocortical circuitry disruptions in schizophrenia during delayed response tasks. Biol Psychiatry 2006; 60: 235–41. Cardenas VA, Studholme C, Gazdzinski S, Durazzo TC, Meyerhoff DJ. Deformation-based morphometry of brain changes in alcohol dependence and abstinence. Neuroimage 2007; 34: 879–87. Carey KB, Carey MP, Simons JS. Correlates of substance use disorder among psychiatric outpatients: focus on cognition, social role functioning, and psychiatric status. J Nerv Ment Dis 2003; 191: 300–8. Chanraud S, Martelli C, Delain F, et al. Brain morphometry and cognitive performance in detoxified alcohol-dependents with preserved psychosocial functioning. Neuropsychopharmacology 2007; 32: 429–38. Chow TW, Cummings JL. Frontal-subcortical circuits. In: Miller BL, Cummings JL, editors. The Human Frontal Lobes - Functions and Disorders. New York: Guilford Press; 2007. p. 25–43. Davatzikos C, Shen D, Gur RC, et al. Whole-brain morphometric study of schizophrenia revealing a spatially complex set of focal abnormalities. Arch Gen Psychiatry 2005; 62: 1218–27. Fazel S, Langstroem N, Hjern A, Grann M, Lichtenstein P. Schizophrenia, substance abuse, and violent crime. JAMA 2009; 301: 2016–23. Frith U, Frith CD. Development and neurophysiology of mentalizing. Philos Trans R Soc Lond B Biol Sci 2003; 358: 459–73. Garavan H, Stout JC. Neurocognitive insights into substance abuse. Trends Cogn Sci 2005; 9: 195–201. Gerdeman GL, Partridge JG, Lupica CR, Lovinger DM. It could be habit forming: drugs of abuse and striatal synaptic plasticity. Trends Neurosci 2003; 26: 184–92. Herman M. Neurocognitive functioning and quality of life among dually diagnosed and non-substance abusing schizophrenia inpatients. Int J Ment Health Nurs 2004; 13: 282–91. Honea R, Crow TJ, Passingham D, Mackay CE. Regional deficits in brain volume in schizophrenia: a meta-analysis of voxel-based morphometry studies. Am J Psychiatry 2005; 162: 2233–45. Jentsch JD, Taylor JR. Impulsivity resulting from frontostriatal dysfunction in drug abuse: implications for the control of behavior by rewardrelated stimuli. Psychopharmacology 1999; 146: 373–390. Jernigan TL, Butters N, DiTraglia G, et al. Reduced cerebral grey matter observed in alcoholics using magnetic resonance imaging. Alcohol Clin Exp Res 1991; 15: 418–27. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13: 261–76. Kerns JG, Cohen JD, MacDonald AW, Cho RY, Stenger VA, Carter CS. Anterior cingulate conflict monitoring and adjustments in control. Science 2004; 303: 1023–6. Kreek MJ, Nielsen DA, Butelman ER, LaForge KS. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nat Neurosci 2005; 8: 1450–7. Lehrl S, Triebig G, Fischer B. Multiple choice vocabulary test MWT as a valid and short test to estimate premorbid intelligence. Acta Neurol Scand 1995; 91: 335–45. B. Schiffer et al. Liu X, Matochik JA, Cadet JL, London ED. Smaller volume of prefrontal lobe in polysubstance abusers: a magnetic resonance imaging study. Neuropsychopharmacology 1998; 18: 243–52. Lundqvist T. Cognitive consequences of cannabis use: comparison with abuse of stimulants and heroin with regard to attention, memory and executive functions. Pharmacol Biochem Behav 2005; 81: 319–30. Mathalon DH, Pfefferbaum A, Lim KO, Rosenbloom MJ, Sullivan EV. Compounded brain volume deficits in schizophrenia-alcoholism comorbidity. Arch Gen Psychiatry 2003; 60: 245–52. Matsuo K, Nicoletti M, Nemoto K, et al. A voxel-based morphometry study of frontal gray matter correlates of impulsivity. Hum Brain Mapp 2009; 30: 1188–95. Minzenberg MJ, Laird AR, Thelen S, Carter CS, Glahn DC. Meta-analysis of 41 functional neuroimaging studies of executive function in schizophrenia. Arch Gen Psychiatry 2009; 66: 811–22. Moeller FG, Dougherty DM, Barratt ES, et al. Increased impulsivity in cocaine dependent subjects independent of antisocial personality disorder and aggression. Drug Alcohol Depend 2002; 68: 105–11. Nelson HE. A modified card sorting test sensitive to frontal lobe defects. Cortex 1976; 12: 313–24. Nigg JT. On inhibition/disinhibition in developmental psychopathology: views from cognitive and personality psychology and a working inhibition taxonomy. Psychol Bull 2000; 126: 220–46. Nigg JT, Wong MM, Martel MM, et al. Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. J Am Acad Child Adolesc Psychiatry 2006; 45: 468–75. Norman DA, Shallice T. Attention to action: willed and automatic control of behaviour. In: Davison RJ, Schwartz GE, Shapiro D, editors. Consciousness and self-regulation. New York: Plentum; 1986. p. 1–18. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol 1995; 51: 768–774. Pencer A, Addington J. Substance use and cognition in early psychosis. J Psychiatry Neurosci 2003; 28: 48–54. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA 1990; 264: 2511–8. Reitan RM, Wolfson D. The Halstead-Reitan neuropsychological test battery: theory and clinical interpretation. Tucson, AZ: Neuropsychology Press; 1985. Ridderinkhof KR, Ullsperger M, Crone EA, Nieuwenhuis S. The role of the medial frontal cortex in cognitive control. Science 2004; 306: 443–7. Schall U, Johnston P, Lagopoulos J, et al. Functional brain maps of Tower of London performance: a positron emission tomography and functional magnetic resonance imaging study. Neuroimage 2003; 20: 1154–61. Schellig D. Block Tapping Test—Testhandbuch. Frankfurt: Swets and Zeitlinger; 1997. Selzer ML. The Michigan alcoholism screening test: the quest for a new diagnostic instrument. Am J Psychiatry 1971; 127: 1653–8. Siever LJ, Davis KL. The pathophysiology of schizophrenia disorders: perspectives from the spectrum. Am J Psychiatry 2004; 161: 398–413. Skinner HA. The drug abuse screening test. Addict Behav 1982; 7: 363–71. Spanagel R, Heilig M. Addiction and its brain science. Addiction 2005; 100: 1813–22. Tarter RE, Kirisci L, Mezzich A, et al. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am J Psychiatry 2003; 160: 1078–85. Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev 1990; 97: 147–68. Wechsler D. Wechsler Memory Scale–revised. New York: The Psychological Corporation; 1987. VBM in schizophrenia-addiction comorbidity Williams LM. Voxel-based morphometry in schizophrenia: implications for neurodevelopmental connectivity models, cognition and affect. Expert Rev Neurother 2008; 8: 1049–65. Winklbaur B, Ebner N, Sachs G, Thau K, Fischer G. Substance abuse in patients with schizophrenia. Dialogues Clin Neurosci 2006; 8: 37–43. Wittchen HU, Wunderlich U, Gruschwitz S, Zaudig M. Strukturiertes Klinisches Interview für DSM-IV (SKID). Göttingen: Beltz-Test 1996. Brain 2010: 133; 3093–3103 | 3103 Wobrock T, Sittinger H, Behrendt B, D’Amelio R, Falkai P. Comorbid substance abuse and brain morphology in recent-onset psychosis. Eur Arch Psychiatry Clin Neurosci 2009; 259: 28–36. Zimmermann P, Fimm B. A test battery for attention performance. In: Leclercq M, Zimmermann P, editors. Applied neuropsychology of attention. Theory, diagnosis and rehabilitation. New York: Psychology Press; 2009. p. 110–51.