* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Mild Traumatic Brain Injury 9th Annual Fall
Neuroscience and intelligence wikipedia , lookup
Blood–brain barrier wikipedia , lookup
Emotional lateralization wikipedia , lookup
Limbic system wikipedia , lookup
Human multitasking wikipedia , lookup
Haemodynamic response wikipedia , lookup
Selfish brain theory wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Neuroinformatics wikipedia , lookup
Embodied cognitive science wikipedia , lookup
Neuroanatomy wikipedia , lookup
Time perception wikipedia , lookup
Neurolinguistics wikipedia , lookup
Neuroeconomics wikipedia , lookup
Brain morphometry wikipedia , lookup
Dual consciousness wikipedia , lookup
Human brain wikipedia , lookup
Neuroesthetics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Brain Rules wikipedia , lookup
Holonomic brain theory wikipedia , lookup
Neurophilosophy wikipedia , lookup
History of neuroimaging wikipedia , lookup
Impact of health on intelligence wikipedia , lookup
Neuroplasticity wikipedia , lookup
Cognitive neuroscience wikipedia , lookup
Aging brain wikipedia , lookup
Neuropsychology wikipedia , lookup
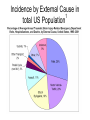
Mild Traumatic Brain Injury 9th Annual Fall Nursing Symposium-9/17/2008 Robert G. Kohn D.O. Neurology, Psychiatry, Neuropsychiatry 815 344 7951 www.drrobertkohn.com Goals • 1. Familiarize the audience with the scope of mTBI • 2. Explain relevant brain anatomy and function impacted by TBI • 3. Provide a guideline for initial evaluation and ongoing treatment with practical resourses available in the community Overview • Part I-Mild TBI, Epidemiology, Brain anatomy and function • Part II- Evaluation Process of TBI • Part III- Approach to Treatment; An Integrated Bio-Psycho-Social Model SPECT normal vs TBI Normal 3-D Surface Image Traumatic Brain Injury Traumatic Brain Injury- TBI • …with or without skull fracture is an insult to the brain caused by external physical force that may produce a diminished or altered state of consciousness. – Acquired Brain injury- not hereditary or present at birth or degenerative condition that may be due to a stroke, toxic ( alcohol, cocaine, etc ), anoxic-hypoxic ( cardiac, sepsis, metabolic, etc ). –www.biail.org fact sheet page 1 Mild TBI • A concussion or event that may leave a person dazed or cause a brief loss of consciousness • Any period of LOC of < 30 minutes and a GCS of 13-15 • Any loss of memory for events immediately before or after an accident with PTA <24 hours • Any alteration in mental state ( dazed, confused, disoriented ) at the time of the accident • Focal neurological deficits that may or may not be transient Post Concussion Syndrome • May follow from the injury that includes a spectrum of deficits – Headache – Dizziness – Dysequilibrium – Mild mental slowing – Fatigue Epidemiology of TBI Prevalence in total US Population • 1.4 million people sustain a TBI each year • Distribution of Average incidence of hospitalizations, emergency department visits, and deaths between 1995-2001 • As a cumulative result of TBI, an estimated 5.3 million Americans are living with a permanent disability 1 Deaths 4% Hospitaliz ations 17% ED visits 79% TBI Incidence by Severity in U.S. Population15 • Mild TBI- 131 cases/100,000 people (397,700) • Moderate TBI- 15 cases/100,000 people 9% 9% Mild Moderate Severe (45,540) • Severe TBI- 14 cases/100,000 people (42,500) • Mortality rates: – severe TBI 33% – moderate TBI 2.5% 82% Incidence by External Cause in 1 total US Population Some Statistics about brain injury • 1.5 million Americans sustain TBI annually • 80,000 Americans experience LTDisability • 5.3 million Americans-2% pop have TBI LTD • MVA cause 44%, Falls 26%,Assualts and Firearms 17%, sports and recreation13% • 50,000 children TBI from bicycle • 200,000 children hospitalized and 30,000 are permanent TBI injuries U.S. Military Incidence and Prevalence (OEF/OIF) • Head/neck injuries: 15-20% of all battle injuries2,3 • Up to 28% of all war fighters4 • Defense and Veterans Brain Injury Center (DVBIC) at Walter Reed Army Medical Center among OIF/OEF veterans5– 30% had traumatic brain injury (greater percentage meeting TBI criteria when injury was blast related) • 56% have moderate to severe TBI • 44% have mild TBI (MTBI) – 10–20% of combat veterans meet the criteria for MTBI on postdeployment screening 44% 56% Mild Mod/Severe How does TBI happen- mechanism Bicycle fall head injury Helmet Protection Bicycle TBI proposed mechanisms • Shearing forces from rapid accelerationdeceleration disrupt molecular bonds that hold white matter fibers together • Decrease in rCBF • Decrease in Glucose availability to neurons • Cytotoxicity from Glutamate release • Thalamus injury alters pacemaker generation fails to gate cortical-subcortical firing patterns White matter disruption-axonal shearing & Thalamus injury Brain Anatomy and FunctionLobes-F,P,T,O,Cb Cortex lobes and function – Frontal lobe-central executive, emotional executive; planning, decision making, time management, organziation, motivation,drive and reward systems for behavior, taste, smell – Temporal lobe-”what systems” for attention and language, brain dictionary, “memory” for declarative and emotional recordshippocampus and amygdala Cortex lobes-function – Parietal lobe-sensory-motor cortex for visual-spatial processing, “ where” attention system and “ How “ systems for motor planning- praxis and language – Occipital lobe- primary, secondary and tertiary visual processing- faces, color, shapes, movement, etc Cortex, Subcortex and brainstem • Cerebellum- balance and coordination of trunk, limbs, eye movements,” time keeper” for data sequencing- cognitive dysmetria. • Basal Ganglia • Cingulate lobe • Insula • Thalamus • Brainstem- origination of NE, 5HT,DA projection pathways, sleep circuits, etc Brain regions Brain Stem Spinal Cord Limbic System properties • Mental content; linking mental content to autonomic, hormonal, immunological states; coordination of affiliative behaviors related to social cohesion • Channeling emotion; drives to extrapersonal events • Includes perception of taste, smell, taste Cortical-Subcortical Loops: Thalamo-Cortical-Striatal Anatomy Cortex Thalamus Striatum Japanese Cherry Blossoms Evaluation Process of TBI • Patient Narrative- observe, listen and ensure an open minded, patient centered space for each person to report their story • Obtain Pre and Post Injury report of functionality from patient and family, partner, children, etc • Broad framework of observation from patient report of symptoms to systems involved. Assist information gathering • Provide rating forms for patient and family before patient is seen • Include – TBI patient and care giver rating form – MINI- NIMH form assessment screen for Depression, Panic, Anxiety and Substance abuse – Consider PTSD and substance screening forms Collaborative History • Obtain records from other professionals if available; ie hospital emergency room • Legal status; ie litigation pending or implemented • If child or young adult get school report cards • Assure time to obtain collaborative history from significant others in patient’s life 5 Regions of Impairment to evaluate-SCABS • Sleep- fatigue, insomnia, restfullness, emergent OSA • Cognition-short term memory, attention states, processing speed, mental stamina, distractability, focus • Affective-observed mood changes, vegetative symptoms of depression, anxiety, fears, anger,suicidality • Behavior-disinhibition leading to property or physical destruction, aggression, agitation, safety status • Somatic-pain symptoms, headache, dizziness, balance difficulties,etc Office Evaluation • MSE -include digit span, WLG, categorical naming, read, writing, math, drawing,etc • Physical attention to pain • Neurological attention to general versus focal deficits; test for smell and taste, balance and coordination, weakness and power, vision and pupil reaction, deep tendon reflexes, sensory gradients with vibration, position, graphesthesia,etc • Attention testing; CPT- IVA, Quotient tests against ADHD data set, personality w NEO5 factor inventory- CANOE Additional Testing • EEG- awake and asleep study for post traumatic epilepsy • QEEG- spectral analysis of brain wave frequency distribution; localized slowing, etc • SPECT-nuclear medicine test for regional or focal hypoperfusion • 3T MRI- done at centers using higher resolution than 1.5 T evalute white matter tracts and cortex • fMRI- functional testing; ie language based protocol evaluate networks activated or delayed; www.cmrr.uic.edu • Event Related Potentials-EEG based pattern of visual, auditory or cognitive processing QEEG Temporal lobe slowing +3sd Visual relaxation Autumn Winter Summer Imagination Approach to Treatment- An Integrated Model • Define the Problem-Biological, Psychological, Social Perspectives • Patient focus- fears? Loss? Anger? Transient. • System view- family acknowledgement or disbelief?, partner intimacy loss?, employment risk or continuity? • Search for Meaning the event holds • • • • Legal issues to recover costs or seek financial gain Religious beliefs to sustain recovery Hidden expectations from parents, siblings, family, partner Temperment profile and capacity to process injury Time Framework • Initial evaluation• prepare patient before hand for paperwork, records, define initial expectations. Arrive earlier to complete. • Access willingness and resources; what is the capacity of the patient to particpate? Are injury deficits limiting information flow or emotional capacity? • Provide written list of the next steps in the evaluation; where to go, testing orders, contacts. • Provide timely follow up to assure compliance and answer questions from the patient. Do this before the next visit or reschedule follow up. Treatment Plan • Build a treatment team • Family, care giver role reversals • Case management • Referral resources for cognitive evaluation and rehabilitation ( neuropsychology ), for individual and marital therapy, for physical therapy • Medications, Alternative Therapies – Osteopathic, Chiropractic, Accupuncure, Nutritional Treatment Plan • Target specific measureable results: • Overview of SCABS • Sleep- consider sleep study or risk of etoh or sedativehypnotic rx from other source for self medication • Cognition- consider Neuropsychology evaluation, Cognitive rehabilitation, Medication, • Affect- consider medication, individual therapy or marital therapy referral. • Behavior- discuss risks and benefit of medications • Somatic- discuss importance of pain specialist and risk of narcotic diversion-dependence to self medicate mood Medications • Medication can improve: – Attention- stimulants used for ADHD tx such as ritalin, Concerta, Focalin, Adderall, etc – Working memory-Amantadine, Aricept, Exelon ( patch ), Reminyl – Mood stability- Depakote, other AED’s – Self control-impulsivity-atypical antipsychotics such as Abilify, Seroquel, Risperidal,etc – Pain Non medication treatment • EEG Neurofeedback- brain wave reinforcement programs • Osteopathic and Chiropractic- help muscloskeletal components of pain and redirect somatic forces of imbalance • Massage- help soft tissue injuries • Accupuncture- help pain • Physical Therapy- help pain, confidence Time is fleeting Summary • MTBI has many faces of impairment • The evaluation process requires a broad framework of knowledge and resource allocation • Significant recovery is the RULE not the Exception but the time frame and expectations vary • An ounce of Prevention is worth a pound of cure…. Thank you. HAPPY FAMILY