* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Autonomic_notes
Long-term depression wikipedia , lookup
NMDA receptor wikipedia , lookup
Neuroanatomy wikipedia , lookup
Nervous system network models wikipedia , lookup
Biological neuron model wikipedia , lookup
Syncope (medicine) wikipedia , lookup
Neurotransmitter wikipedia , lookup
Synaptic gating wikipedia , lookup
Axon guidance wikipedia , lookup
Haemodynamic response wikipedia , lookup
End-plate potential wikipedia , lookup
Synaptogenesis wikipedia , lookup
Signal transduction wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Microneurography wikipedia , lookup
Circumventricular organs wikipedia , lookup
Neuromuscular junction wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
History of catecholamine research wikipedia , lookup
Autonomic Notes
The length of the notes for a section is not necessarily proportional to the number of test questions for a section.
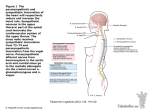
Autonomic nervous system (ANS) versus somatic nervous system: what are the similarities &
differences?
Sympathetic versus parasympathetic
Which spinal / cranial nerves does each division travel along?
(Sympathetic: spinal nerves from thoracic and high lumbar levels. Parasympathetic: some cranial nerves,
and spinal nerves from sacral levels.)
Where are the ganglia of the 2 divisions?
Side note: Some authors (incl. Marieb & Hoehn) call the “second” neuron in the autonomic
pathway the “post-ganglionic” neuron. Other authors (incl. Martini & Ober) call that neuron the
“ganglionic neuron”. Either way, it is the neuron “after” the pre-ganglionic neuron. The axon of a
(post)ganglionic neuron is called a post-ganglionic fiber by all sources I have seen. Be comfortable
with both usages.
When (in general) does each division become active?
(If using Martini & Ober text) What is the enteric division of ANS? How does it relate to
the sympathetic & parasympathetic divisions?
Sympathetic and parasympathetic organization
Where are the…
Sympathetic preganglionic neurons? (thoracic & upper lumbar segments of spinal cord, specifically
in lateral gray horn)
Sympathetic post-ganglionic neurons? (sympathetic chain ganglia, collateral ganglia, adrenal
medulla)
Sympathetic pathway: Axons of symp preganglionics (wich are mostly myelinated) exit
spinal cord in ventral root, follow ventral ramus, then follow white ramus communicans to
the sympathetic trunk (also called sympathetic chain ganglia). Preganglionic axon takes
on e of three courses: 1. Synpase at that level onto postganglionic. 2. Go up or down one
or two levels before synapsing onto postgangionic. 3. Pass through the sympathetic trunk
to the prevertebral plexus and synapse onto a postganglionic neuron there in the
prevertebral plexus. The axons (unmyelinated) of symp preganglionics whose somas are
in the symp trunk travel thorugh the gray ramus communicans then travel with mixed
nerves to their destination.
Sympathetic pre-ganglionic fiber versus post-ganglionic fiber length? (short, except to
adrenals; long)
How does adrenal gland relate? (see preceding)
General function of sympathetics? (Metabolism, alertness, blood pressure, heart rate all increase
during sympathetic activation; fight or flight.)
Where are the…
Parasympathetic preganglionic neurons? (brainstem, sacral segments of spinal cord)
Parasympathetic post-ganglionic neurons? (in ganglia near target organs, or in the target organs
themselves)
Parasympathetic pre-ganglionic versus post-ganglionic fiber length? (long, short)
General function of parasympathetics? (Promote relaxation, nutrient uptake, energy storage for
future use; rest and digest.)
Sympathetic & parasympathetic pathway details
Where do the nerves go and how do they get there?1
The following cranial nerves have preganglionic parasympathetic motor fibers in them:
III Oculomotor – has parasympathetic motor fibers to smooth muscles of the pupil and lens.
VII Facial – has parasympathetic motor fibers to lacrimal (tear) glands, two of the three salivary glands,
nasal glands
IX Glossopharyngeal – has parasympathetic motor fibers to the third salivary gland (parotid)
X
Vagus – has 75% to 90% (estimates vary) of all parasympathetic preganglionic fibers; branches go to
heart, lungs, GI tract, etc.
The above is just a partial answer to the question posed. See text and preceding portion of notes for more.
Sympathetic & parasympathetic physiology at cellular level
What neurotransmitters are involved?
(Epinephrine, norepinephrine, both of which are active in sympathetic division only. Acetylcholine, which
plays roles in sympathetic and parasympathetic divisions.)
1
Martini & Ober 14.4.1, 14.4.2 show epi binding to alpha receptors and norepi binding to beta receptors. This is
potentially misleading, since either ligand can bind to either receptor. However, it is well established that norepi
binds poorly to beta-2 receptors (Katzung 8th ed 2001).
Two types of adrenergic receptors; two types of cholinergic receptors. What are they and
how do they differ?
(Adrenergic receptors: alpha and beta types. Both types found on effector cells (muscle or gland)
receiving sympathetic innervation. Both types respond to norepinephrine (noradrenaline) and epinephrine
(adrenaline), which are released (mainly NE) by most sympathetic postganglionic fibers onto their target
organs.1 All adrenergic receptors act via second messengers in cytoplasm.
Blood-pressure-raising effects of sympathetic stimulation or adrenaline administration are mediated in part
by by alpha-1 receptors, whose activation causes blood vessel constriction in skin and viscera (but not in
skeletal muscle, which has few alpha receptors). Beta-1 receptors on heart make it beat faster/stronger
during same stimuli. Beta-2 receptors cause dilation of bronchioles (helps with increased breathing) and
skeletal muscle blood vessels (more blood flow to muscle, less to gut). Beta-3 receptors cause increased
lipolysis: release of fatty acids (needed as muscle fuel) from adipocytes.
Cholinergic receptors: nicotinic and muscarinic types. Natural ligand for both types is acetylcholine
(ACh); they are also activated by the drugs nicotine & muscarine respectively.
Nicotinic receptors: found on sympathetic and parasympathetic ganglionic neurons, stimulated by ACh
released by preganglionic neuron. Nicotinic cholinergic receptor also found on skeletal muscle cells,
responding to ACh released by somatic motoneurons. Nicotinic receptors are chemically gated ion channels
that open when ACh binds; this leads to target cell excitation.
Muscarinic receptors: found on effector cells (muscles or gland or other cell type) receiving
parasympathetic innervation. Muscarinic receptors are G-protein-coupled receptors which act via second
messengers. Effects are slow compared to nicotinic receptor activation; can be excitatory or inhibitory.
Muscarinic receptors are also found on cells receiving sympathetic cholinergic innervation - an unusual
and important exercise-related exception to the general rule that sympathetic postganglionic fibers release
NE. Skeletal muscle and eccrine sweat glands receive symp cholinergic innervation and are activated during
exercise. Activation causes blood vessel dilation and sweating.
Form and function of sympathetics & parasympathetics
Effects of activation of each system?
Symp: metabolism, alertness, blood pressure, heart rate all increase; fight or flight.
Parasymp: relaxation, nutrient uptake, energy storage for future use; rest and digest
Anatomical characteristics of each system, including different pre- & postganglionic fiber
lengths, different and in some cases same transmitters (depending on pre- versus postganglionic)?
Adrenal medulla versus other sympathetic ganglia?
ANS control of different body functions.
Example: heart rate control?
Symp activation causes heart rate up via beta adrenergic receptors; parasymp activation causes heart rate
down via muscarinic cholinergic receptors.
Visceral reflexes
Which nerves carry afferent fibers for the reflexes?
Afferents in nerves VII, IX, X (facial, glossopharyngeal vagus), and others. (You already know the efferent
pathways: the symp and parasymp motor outflow discussed above.)
Visceral reflex examples
Baroreceptors – what are they, how do they work, what are the pathways?
Baroreceptor = stretch receptor in wall of hollow organ such as blood vessel, lung, gut, bladder. Increased
pressure in organ causes more stretch causes more action potentials on afferent neuron. Example: “arterial
baroreceptors” in carotid artery and aortic arch (called aortic sinus by Martini & Ober) report arterial blood
pressure (BP). Afferent fibers in cranial nerve IX (carotid baroreceptor) and X (aortic baroreceptors).
Central processing in medulla (solitary tract nucleus=NTS) & other brainstem areas. Efferent pathway
involves sympathetic fibers & parasymp fibers to heart and to blood vessels. A change in blood pressure
leads to autonomic responses (symp & parasymp) that tend to compensate for, or correct, the change, such
as increased heart rate if BP falls, etc. Sympathetic nerve activity to heart increases rate and strength of
heart beats; parasympathetic (vagal) activity slows heart. Sympathetic activation constricts most blood
vessels, especially in gut and skin.
{Skip chemoreceptor reflexes.
Chemoreceptors – what are they, how do they work, what are the pathways?
Chemoreceptor = receptor which responds to a change in concentration of a chemical. Example: “arterial chemoreceptors” in
carotid artery and aortic arch report changes in blood pH and concentration of O2, CO2. Afferent fibers in cranial nerve IX
(carotid chemoreceptor) and X (aortic chemoreceptors). Central processing in solitary nucleus (=NTS) & other brainstem areas
that regulate respiration and blood delivery to tissues. Efferent pathway involves brainstem areas that control muscles of
respiration and cardiovascular system. Change in O2, CO2, pH lead to autonomic responses (symp & parasymp) that tend to
compensate for, or correct, the change, such as faster breathing if O2 falls, etc.
}
Higher level control of ANS
What higher brain centers control the ANS?
Hypothalamus oversees autonomic centers in pons (respiratory control) and medulla (many autonomic
functions including respiration, heart, blood vessels, swallow, cough, etc). Medulla controls autonomic
outflow from spinal cord and vagus nerve. Hypothalamus is controlled by higher brain areas including
cortex, limbic system (emotions).
___________________________
Concluding thoughts for students
Understand distinction between preganglionic (pre-G) and postganglionic neurons: Know
where the cells bodies of each type are found (for both symp and parasymp), and what
chemicals the different types use as their transmitters, and where are those chemicals released.
One thing that may be confusing is that the axons of the pre-Gs terminate in the ganglia, on
the somas of the post-Gs. Therefore the transmitters of the pre-Gs (which is always ACh) are
found in the ganglia.