* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Central neural control of the cardiovascular system
Neurolinguistics wikipedia , lookup
Selfish brain theory wikipedia , lookup
Neuroesthetics wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Nervous system network models wikipedia , lookup
Brain Rules wikipedia , lookup
Premovement neuronal activity wikipedia , lookup
Neuroeconomics wikipedia , lookup
Development of the nervous system wikipedia , lookup
Functional magnetic resonance imaging wikipedia , lookup
Neural oscillation wikipedia , lookup
Neurobiological effects of physical exercise wikipedia , lookup
Neuroplasticity wikipedia , lookup
Emotional lateralization wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Syncope (medicine) wikipedia , lookup
History of neuroimaging wikipedia , lookup
Intracranial pressure wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Activity-dependent plasticity wikipedia , lookup
Synaptic gating wikipedia , lookup
Aging brain wikipedia , lookup
Neuroanatomy wikipedia , lookup
Optogenetics wikipedia , lookup
Microneurography wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Metastability in the brain wikipedia , lookup
Hypothalamus wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Pre-Bötzinger complex wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Cushing reflex wikipedia , lookup
Haemodynamic response wikipedia , lookup
Adv Physiol Educ 40: 283–296, 2016;
doi:10.1152/advan.00027.2016.
Refresher Course
Central neural control of the cardiovascular system: current perspectives
Roger A. L. Dampney
School of Medical Sciences (Physiology) and Bosch Institute, The University of Sydney, Sydney, New South Wales, Australia
Submitted 3 February 2016; accepted in final form 23 May 2016
cardiovascular reflexes; central command; autonomic nervous system;
hypothalamus; brain stem
can be defined as the maintenance of the physical
and chemical properties of the extracellular fluid in all body
tissues. It is dependent, among other things, on effective
cardiovascular and respiratory regulatory mechanisms that ensure that the delivery of O2 to all regions of the body is
sufficient to match the metabolic demands of each region. This
is particularly critical in the case of the heart and skeletal
muscles, whose metabolic activity can vary greatly in different
circumstances. For example, during maximal exercise in humans, O2 demand can increase to a level up to 50-fold greater
than resting levels (49). This is achieved by an enormous
increase in blood flow (up to 20-fold) together with a 2- to
3-fold increase in O2 extraction from the blood (49). These
effects are produced by a combination of local and neural
mechanisms, as shown in Fig. 1. Local mechanisms, which
include metabolic, endothelial, and myogenic components
(49), result in vasodilation in metabolically active skeletal
muscle vascular beds, leading to large increases in local blood
flow provided the perfusion pressure (arterial pressure) is
maintained or increased. Similarly, the increase in O2 extraction from the blood also depends on both local factors (e.g.,
local acidosis, which shifts the hemoglobin-oxygen saturation
HOMEOSTASIS
Address for reprint requests and other correspondence: R. A. L. Dampney, School of Medical Sciences (Physiology) and Bosch Institute, The
Univ. of Sydney, Sydney, NSW 2006, Australia (e-mail: roger.dampney
@sydney.edu.au).
curve to the right) (49) as well as central regulatory mechanisms that maintain the arterial blood PO2 (PaO2) despite large
changes in metabolic activity (1).
Apart from physical exercise, coordinated cardiovascular
and respiratory mechanisms regulate the O2 supply to all tissue
during other behaviors, such as defensive behavior or sleep. In
addition, such regulatory mechanisms are also required to
maintain homeostasis in the face of challenges such as hypoxia, dehydration, or changes in ambient temperature. In this
review, I shall focus primarily on the central neural mechanisms that regulate cardiovascular function, although I shall
also discuss, where relevant, how these mechanisms are coordinated with respiratory regulatory mechanisms.
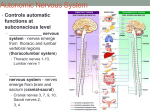
As shown in Fig. 1, arterial blood pressure is regulated by
autonomic nerves, consisting of sympathetic nerves that innervate the heart and blood vessels, and vagal parasympathetic
nerves, which innervate the heart. Sympathetic outflow, in turn,
is regulated by sympathetic premotor neurons located in the
lower brain stem and hypothalamus, whereas vagal cardiac
outflow originates primarily from the nucleus ambiguus in the
medulla oblongata. The activity of the sympathetic premotor
neurons and cardiac vagal neurons is controlled by two general
mechanisms: 1) reflex effects arising from stimulation of a
wide variety of peripheral receptors and 2) feedforward control, or “central command,” from descending inputs arising
from higher centers in the brain (Fig. 1).
One of the most important cardiovascular reflexes is the
baroreceptor reflex, and an example of its operation is shown in
Fig. 2A. In this example, recordings were made of mean
arterial pressure, heart rate, and renal sympathetic nerve activity in a conscious rat during treadmill exercise (35). Changes in
arterial pressure were induced by systemic injection of a
vasoconstrictor (phenylephrine) and a vasodilator (sodium nitroprusside), resulting in reflex changes in heart rate and renal
sympathetic nerve activity.
In contrast to reflex or feedback control, feedforward control
(central command) does not require inputs from peripheral
receptors. A classic example of such control is shown in Fig.
2B. Recordings of arterial pressure and heart rate were made in
a paralyzed, mechanically ventilated, but conscious, human
subject, who was asked to attempt to contract leg muscles (18).
The numbers indicate the effort as a percentage of the maximum. Note that there were graded increases in arterial pressure
and heart rate according to the degree of effort, despite the lack
of any afferent feedback from the paralyzed muscles.
These two general mechanisms of feedback and feedforward
control are not, however, entirely independent. In particular, as
shall be described in more detail below, cardiovascular reflexes
such as the baroreceptor reflex can be powerfully modulated by
central command signals arising from the forebrain or midbrain.
1043-4046/16 Copyright © 2016 The American Physiological Society
283
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
Dampney RA. Central neural control of the cardiovascular system:
current perspectives. Adv Physiol Educ 40: 283–296, 2016;
doi:10.1152/advan.00027.2016.—This brief review, which is based
on a lecture presented at the American Physiological Society Teaching Refresher Course on the Brain and Systems Control as part of the
Experimental Biology meeting in 2015, aims to summarize current
concepts of the principal mechanisms in the brain that regulate the
autonomic outflow to the cardiovascular system. Such cardiovascular
regulatory mechanisms do not operate in isolation but are closely
coordinated with respiratory and other regulatory mechanisms to
maintain homeostasis. The brain regulates the cardiovascular system
by two general means: 1) feedforward regulation, often referred to as
“central command,” and 2) feedback or reflex regulation. In most
situations (e.g., during exercise, defensive behavior, sleep, etc.), both
of these general mechanisms contribute to overall cardiovascular
homeostasis. The review first describes the mechanisms and central
circuitry subserving the baroreceptor, chemoreceptor, and other reflexes that work together to regulate an appropriate level of blood
pressure and blood oxygenation and then considers the brain mechanisms that defend the body against more complex environmental
challenges, using dehydration and cold and heat stress as examples.
The last section of the review considers the central mechanisms
regulating cardiovascular function associated with different behaviors,
with a specific focus on defensive behavior and exercise.
Refresher Course
284
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
Extrinsic inputs (e.g.
sight, sound, odor)
Forebrain & midbrain
Central command
Motor outflow to
respiratory muscles
Respiratory
activity
Metabolic,
myogenic &
endothelial
factors
Lower brainstem
Symp outflow to
skeletal muscle
vascular bed
Symp outflow to
other vascular
beds & heart
Other intrinsic inputs
(from chemoreceptors,
skeletal muscle
receptors etc.)
Vagal outflow
to the heart
Baroreceptor
inputs
Skeletal muscle
vascular
resistance
Blood flow to
skeletal muscle
O2 supply
Fig. 1. Flow diagram illustrating how feedforward (central command) and
feedback (reflex) mechanisms operate together to regulate the O2 supply to
particular regions (skeletal muscle in this example) to match the metabolic
demands of that region and thus maintain homeostasis.
A
MAP
(mmHg)
140
100
Central Mechanisms Subserving Homeostatic Reflexes
To maintain cardiovascular homeostasis, several key physiological variables must be regulated: arterial blood pressure,
the O2 content of the blood, blood volume, and body temperature. The following sections will briefly describe the reflex
mechanisms that regulate these variables.
Blood pressure. The baroreceptor reflex is the principal
mechanism regulating arterial pressure, at least in the short
term. For example, a decrease in arterial pressure is sensed by
baroreceptors located in the walls of the carotid sinus and
aortic arch (Fig. 3A). The baroreceptors are stretch receptors
located on the terminal arborizations of afferent fibers, so a
decrease in arterial pressure results in a decreased firing rate of
baroreceptor afferent fibers. Inputs from baroreceptor afferent
fibers reflexly inhibit the sympathetic outflow to the heart and
blood vessels and reflexly excite the cardiac vagal outflow via
central pathways in the brain stem and spinal cord (described
in more detail below). Therefore, a decrease in baroreceptor
firing rate results in a reflex increase in sympathetic vasomotor
activity, which increases total vascular resistance, and an
increase in sympathetic cardiac activity together with a reflex
decrease in cardiac vagal activity, which together results in an
increase in heart rate and cardiac contractility, and thus cardiac
output (Fig. 3A). The reflex increases in total peripheral
resistance and cardiac output together help to restore arterial
pressure (Fig. 3A). The most important component of the
reflex response is the reflex change in total peripheral
resistance, which accounts for ⬃80% of the reflex change in
arterial pressure at rest and virtually 100% during exercise
(Fig. 3B) (44).
The functional properties of the baroreceptor reflex in any
particular situation can be represented by a sigmoidal curve
that shows the input-output relationship for the reflex, where
the input is the mean arterial pressure and the output is the
reflexly controlled variable, e.g., renal sympathetic activity
or heart rate (Fig. 4). To determine this curve, changes in
mean arterial pressure are induced (e.g., by infusing a
vasodilator or vasoconstrictor drug, as shown in Fig. 2A),
180
HR
(bpm)
700
550
400
RSNA
( V)
250
0
-250
2 min
PE
B
HR
(bpm)
SNP
150
130
110
200
150
Arterial
pressure
(mmHg)
100
50
100%
50%
25%
0%
(Numbers indicate %maximum effort)
0
0
100
200
300
400
500
Time (s)
Fig. 2. A: example of baroreflex control of the cardiovascular system. Changes
in mean arterial pressure (MAP) were induced in a conscious exercising rat by
systemic injection of the vasoconstrictor phenylephrine (PE) or the vasodilator
sodium nitroprusside (SNP), resulting in reflex changes in heart rate (HR) and
renal sympathetic nerve activity (RSNA). [Modified from Miki et al. (35) with
permission.] B: example of central command. Recordings of arterial pressure
and HR [in beats/min (bpm)] were made in a paralyzed, mechanically ventilated, but conscious human subject, who was asked to attempt to contract leg
muscles. The numbers indicate the effort as a percentage of the maximum.
Note that there were graded increases in arterial pressure and HR according to
the degree of effort, despite the lack of any afferent feedback from the
paralyzed muscle. [Modified from Gandevia et al. (18) with permission.]
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
Arterial blood PO2
Arterial pressure
and reflex changes in the output (e.g., renal sympathetic
activity or heart rate) are then measured. The sigmoidal
curve that best fits the relationship between the input and
output is then determined (e.g., Fig. 4B).
The precise characteristics of the sigmoidal baroreflex function curve are defined by 1) the maximum and minimum values
of the reflexly controlled output; 2) the maximum gain or
sensitivity of the reflex, i.e., where the slope of the curve is
maximal; and 3) the operating range of the reflex, which is
defined as the range of mean arterial pressure over which
changes in pressure can produce significant reflex changes in
the output (Fig. 4A) (30).
The baroreceptor reflex is operational at all times, although
the functional properties of the reflex can vary under different
behavioral conditions. For example, the maximum gain of the
baroreceptor-sympathetic reflex is increased both during exer-
Refresher Course
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
A
B
Arterial pressure
285
Contribution (% total) of
cardiac output (CO) and total
peripheral resistance (TPR)
to reflex changes in
arterial pressure
Baroreceptor firing rate
TPR
Brainstem centers
Fig. 3. A: flow diagram showing the sequence of
events after a decrease in arterial pressure, leading
to a reflex compensatory restoration of arterial pressure. B: histogram showing that the reflex increase
in total peripheral resistance (TPR) is the major
factor contributing to the reflex response both at rest
and during exercise. CO, cardiac output. [Modified
from Raven et al. (44) with permission.]
CO
100
Sympathetic
vasomotor
activity
Sympathetic
cardiac
activity
Vagal cardiac
activity
Vascular
resistance
Cardiac
contractility
Heart rate
50
At
rest
cise (Fig. 5A) and psychological stress (Fig. 5B). Furthermore,
the reflex is reset so that it operates over a higher range of mean
arterial pressure and sympathetic activity during exercise and
stress (Fig. 5, A and B) (25, 35). Similarly, the baroreceptorheart rate reflex is reset to a higher operating range of both
mean arterial pressure and heart rate during exercise (Fig. 5C),
with little change in gain (41). The effect of such baroreflex
resetting is that during behaviors where an increase in arterial
pressure is physiologically advantageous (e.g., exercise or
defensive behavior), the baroreflex continues to be highly
effective in regulating arterial pressure at this increased level.
It is well known that mean arterial pressure and heart rate
show parallel diurnal variations, such that, in humans, both of
these variables tend to be minimal during the early hours of the
morning (i.e., during the sleep phase) and maximal after
A
Operating range
During
exercise
waking during the morning period (54). These variations in
arterial pressure and heart rate can be explained as a continuous
modulation or resetting of the baroreflex, which thus serves to
regulate arterial pressure at a level that is optimal for each
phase of the sleep-wake or activity cycle.
Studies over the last 35 yr have identified the essential
central pathways that mediate the baroreceptor reflex (13, 19),
and these are shown in Fig. 6. Primary afferent fibers from
arterial baroreceptors located in the carotid sinus and aortic
arch, which run in the glossopharyngeal nerve (cranial nerve
IX) and vagus nerve (cranial nerve X), respectively, terminate
in the nucleus tractus solitarius (NTS) in the dorsomedial
medulla. From the NTS, second-order neurons project directly
to cardiac vagal motoneurons in the nucleus ambiguus or to
interneurons in the caudal ventrolateral medulla (CVLM). The
B
Y value
RSNA (% baseline)
150
Point of
maximum
gain
Thr
X value
100
50
0
Sat
60
80
100
120
140
160
MAP (mmHg)
Fig. 4. A: the standard sigmoidal curve that is used to represent the input-output relationship for the baroreceptor reflex. The curve represents the following
function: Y ⫽ A1/{1 ⫹ exp[A2(X ⫺ A3)]} ⫹ A4, where X is the input (typically MAP) and Y is the output (e.g., sympathetic activity or HR) and A1, A2, A3, and
A4 are the parameters that define the specific curve in any particular situation. The gain or sensitivity of the reflex at any value of X is represented by the slope
of the curve and is maximal at the midpoint of the Y range (i.e., between the maximum and minimum values of Y). The threshold (Thr) value of X is the point
at which the value of Y is 5% of the Y range below the maximum value of Y, and the saturation (Sat) value of X is the point at which the value of Y is 5% of
the Y range above the minimum value of Y. The operating range of X lies between the Thr and Sat values and is thus the range of X over which changes in X
evoke significant reflex changes in Y. [Modified from McDowall et al. (30).] B: example of a baroreflex sigmoidal function curve that best fits the reflex
relationship between MAP and RSNA. In this experiment, changes in MAP were induced by injections of vasoconstrictor and vasodilator drugs, and the
corresponding reflex changes in RSNA were measured (solid circles). [Modified from McDowall et al. (31).]
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
0
Cardiac
output
Arterial pressure
Refresher Course
286
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
A
500
RSNA
(% baseline)
400
300
exercise
200
100
rest
0
60
80
RSNA
(% baseline)
120
140
160
180
160
180
400
300
stress
200
rest
100
0
60
80
100
120
140
MAP (mmHg)
90
C
80
HR (bpm)
exercise
70
60
rest
carotid sinus
50
60
80
100
120
140
160
180
MAP (mmHg)
Fig. 5. A: baroreflex function curves showing the relationship between MAP
and RSNA in conscious rats at rest and during exercise. Note that the
maximum gain is increased and the operating range is shifted to higher values
of MAP during exercise. [Modified from Miki et al. (35) with permission.] B:
baroreflex function curves showing the relationship between MAP and RSNA
in conscious rats at rest and during psychological stress (air jet stress). Note
that the maximum gain is increased and the operating range is shifted to higher
values of MAP during psychological stress, similar to the changes observed in
exercise. [Modified from Kanbar et al. (25).] C: baroreflex function curves
showing the relationship between MAP and HR in human subjects at rest and
during exercise. Note that the operating range of the reflex is shifted to higher
values of MAP during exercise but with little change in the maximum gain of
the reflex. [Modified from Ogoh et al. (41) with permission.]
latter group are GABAergic neurons, which project to and
inhibit sympathetic premotor neurons in the rostral ventrolateral medulla (RVLM). RVLM sympathetic premotor neurons
are tonically active, and their tonic activity is critical in
maintaining sympathetic vasomotor tone and resting arterial
pressure (13, 19). Furthermore, the tonic activity of RVLM
IX
NTS
IML
X
NA
CVLM
RVLM
heart and
blood vessels
heart
excitatory synapse
inhibitory (GABAergic) synapse
Fig. 6. Schematic diagram showing the essential pathways within the lower
brain stem that subserve the baroreflex control of the sympathetic outflow to
the heart and blood vessels and of the vagal parasympathetic outflow to the
heart. CVLM, caudal ventrolateral medulla; IML, imtermediolateral cell column; NA, nucleus ambiguus; NTS, nucleus tractus solitarius; RVLM, rostral
ventrolateral medulla; X, vagus nerve. [Modified from Dampney et al. (11).]
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
500
B
100
MAP (mmHg)
sympathetic premotor neurons under resting conditions also
permits both reflex decreases and increases in sympathetic
activity in response to altered input from the arterial baroreceptors.
Some of the neurons within the baroreflex circuitry shown in
Fig. 6 receive inputs from nuclei at higher levels of the brain,
including the midbrain periaqueductal gray (PAG), dorsomedial and paraventricular nuclei in the hypothalamus, central
nucleus of the amygdala, medial prefrontal cortex, and insular
cortex (13, 53). Although the precise functions of these inputs
has not been determined, it is likely that they include inputs
that reset the baroreceptor reflex during different behaviors.
Blood O2 level. Nearly all O2 in the blood is attached to
hemoglobin. In arterial blood, ⬎95% of hemoglobin molecules
are bound to O2, forming oxyhemoglobin, provided the PaO2 is
⬎90 mmHg. The principal mechanism that helps to maintain
PaO2 under hypoxic conditions (e.g., when atmospheric PO2 is
reduced at high altitudes or when normal breathing is prevented, such as during submersion in diving animals) is the
arterial chemoreceptor reflex. Chemoreceptors located in the
carotid and aortic bodies are activated primarily by a decrease
in PaO2 (Fig. 7A) (4). The main reflex effects of chemoreceptor
activation are 1) an increase in respiratory rate and depth that
increases alveolar ventilation and 2) cardiovascular effects that
reduce blood flow to peripheral tissues and that also decrease
heart rate and thus cardiac work, thus conserving the available
O2 (Fig. 7B).
Under resting conditions, carotid body chemoreceptor activity and the reflex ventilatory response do not start to increase
markedly until PaO2 decreases to ⬃60 mmHg (Fig. 7, A and C).
This corresponds to the point at which the percentage of
hemoglobin binding O2 also starts to decrease rapidly (23), so
the result is that the chemoreflex ventilatory response reflects
Refresher Course
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
A
100
B
287
Hypoxia
Chemoreceptor
Activity (units)
75
Chemoreceptor
afferent activity
50
25
Respiratory
activity
0
40
0
C
80
120
PaO2 (mmHg)
Cardiac
vagal activity
40
Ventilation
30
20
10
Vasoconstriction
Heart rate &
cardiac work
Moderate exercise
Rest
Oxygen uptake
Oxygen conservation
0
40
80
120
PaO2 (mmHg)
the degree of hypoxia of arterial blood. The reflex ventilatory
response to chemoreceptor stimulation is not constant but is
enhanced during exercise (Fig. 7C), as a consequence of
increased peripheral chemosensitivity (56). This is a further
example of reflex operating properties being altered according
to the behavioral state.
The essential central pathways mediating the chemoreceptor
reflex are shown in Fig. 8. Chemoreceptor primary afferent
carotid body
NTS
IML
Dorsolateral
pons
PreB
heart and
blood vessels
RVLM
A5 cell group
excitatory synapse
inhibitory synapse
Fig. 8. Schematic diagram showing the essential pathways within the lower
brain stem that subserve the chemoreflex control of the sympathetic outflow to
the heart and blood vessels. The solid lines indicate direct connections that
have been clearly identified, whereas the dashed lines may be direct or indirect.
PreB, pre-Bötzinger cell group. For other abbreviations, see Fig. 6. [Modified
from Dampney et al. (11).]
fibers arising from the carotid and aortic bodies, which run in
cranial nerves IX and X, respectively, terminate on secondary
interneurons in the NTS (13, 19, 20). The secondary interneurons, in turn, project to a number of targets, including respiratory neurons that drive the ventilatory response as well as
sympathetic premotor neurons in the RVLM that drive the
sympathetic component of the reflex (13, 19, 20). In regard to
the latter, there is now strong evidence that chemoreflex
sympathoexcitation is mediated by both a direct input from the
NTS to sympathetic premotor neurons in the RVLM as well as
by indirect inputs via neurons within the central respiratory
network, including respiratory neurons in the preBötzinger
complex and dorsolateral pons (Fig. 8) [for a detailed review,
see Guyenet (20)].
Apart from the chemoreceptor reflex, all air-breathing vertebrates have a diving reflex (also called nasopharyngeal reflex), which is another reflex that acts to conserve the available
O2 (42). This reflex is particularly powerful in diving animals
(Fig. 9A). The reflex is triggered by activation of nasopharyngeal receptors, which leads to a reflex apnea, intense widespread peripheral vasoconstriction (except in the brain and
heart), and a profound bradycardia (Fig. 9B). The cardiovascular reflex effects conserve the available O2, which is thus
preferentially provided to the brain and heart, two critical
regions that cannot sustain an O2 debt. The same pattern of
reflex respiratory and cardiovascular effects is also evoked in
nondiving animals, in response to stimulation of nasopharyngeal receptors by a noxious substance, such as smoke (57).
Under those circumstances, cessation of ventilation combined
with O2 conservation will also increase the probability of
survival.
Interactions between reflexes. In most situations, more than
one reflex is activated in response to a particular challenge, and
hypoxia is a good example of this. For example, in diving
animals, the first effect of submersion is the activation of
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
Ventilation
(liters/min)
Sympathetic
vasomotor
activity
Fig. 7. A: curve showing the relationship between the arterial blood PO2 (PaO2) and the
activity of a single carotid body chemoreceptor afferent fiber. [Modified from Biscoe et al.
(4) with permission.] B: flow diagram showing the reflex effects of chemoreceptor stimulation by arterial hypoxia, leading to an increase in ventilation (provided that respiratory
activity can increase, as during exposure to
high altitude) as well as cardiovascular reflex
changes that tend to conserve the available
O2. C: curve showing the chemoreflex relationship between PaO2 and alveolar ventilation at rest and exercise in human subjects.
Note that the reflex effects on ventilation are
enhanced during exercise. [Modified from
Weil et al. (56).]
Refresher Course
288
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
A
Arterial pressure
(mmHg)
160
120
80
5s
Diving period
B
Nasopharyngeal
receptor activity
Apnea
Sympathetic
vasomotor
activity
Cardiac
vagal activity
Intense peripheral
vasoconstriction (except
in brain & heart)
Heart rate &
cardiac work
Oxygen conservation
Fig. 9. A: example of the extreme bradycardia evoked during voluntary diving
in a rat. Note that despite the extreme bradycardia (decrease in HR of ⬃80%),
the arterial pressure is maintained, due to intense vasoconstriction. [Modified
from Panneton et al. (42).] B: flow diagram showing the reflex effects of
nasopharyngeal stimulation submersion, leading to cardiovascular reflex
changes that conserve the available O2.
nasopharyngeal receptors that then trigger the diving reflex,
including apnea as well as the cardiovascular effects described
above. The resultant hypoxia, in turn, triggers the chemoreceptor reflex (Fig. 10). The interaction between the two reflexes
reinforces the vasoconstriction and bradycardia, but the normal
ventilatory response to chemoreceptor stimulation is suppressed by inputs from nasopharyngeal receptors (Fig. 10).
In contrast, under conditions where hypoxia occurs without
activation of nasopharyngeal receptors, (e.g., high altitude),
chemoreceptor activation does reflexly increase ventilation,
which then activates another reflex arising from pulmonary
stretch receptors, innervated by afferent vagal fibers. The
pulmonary stretch receptor reflex tends to increase heart rate
and decrease vascular resistance, opposing the primary effects
of chemoreceptor stimulation (Fig. 10). Thus, the net effect on
cardiovascular and respiratory function depends on interactions
between a number of reflexes, which ensures that the pattern of
Fig. 10. Flow diagram illustrating the interaction between reflexes arising
from inputs from arterial chemoreceptors, pulmonary stretch receptors, and
nasopharyngeal receptors. When hypoxia occurs under conditions where respiratory activity can increase (e.g., exposure to a high altitude), the reflex
decrease in HR and the reflex increase in vascular resistance (in skeletal
muscle and visceral beds) is opposed by the secondary reflex effects arising
from the activation of pulmonary stretch receptors, which tends to increase O2
uptake. In contrast, when hypoxia occurs under conditions when respiratory
activity cannot increase (e.g., during submersion), the primary reflex response
to chemoreceptor stimulation is not opposed by these secondary effects.
Furthermore, under such conditions, nasopharyngeal receptors may be
stimulated, triggering reflex effects that reinforce the primary effects of
chemoreceptor stimulation, leading to greater reflex bradycardia and peripheral vasoconstriction and thus a greater degree of O2 conservation.
[From Dampney (11).]
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
Submersion
reflex cardiovascular and respiratory responses is optimal for
the particular environmental challenge faced by the animal.
As shown in Fig. 11, the NTS and RVLM are key components of the central pathways mediating the nasopharyngeal
reflex as well as baroreceptor and chemoreceptor reflexes (see
above) (42). Furthermore, inputs from a wide range of receptors that reflexly affect cardiovascular function also project to
the NTS, either directly or indirectly via other relay nuclei (Fig.
11). These receptors include cardiopulmonary receptors (that
respond primarily to changes in blood volume), vestibular
receptors that are critical for othostatic reflexes, receptors in
skeletal muscle that are activated during exercise (sometimes
called “ergoreceptors”), and skin nociceptors (11, 13). In
addition, inputs from some of these receptors also project to the
RVLM via other pathways that bypass the RVLM (Fig. 11)
(38, 42, 59). Ultimately, however, all of the inputs from the
receptors shown in Fig. 11 converge on sympathetic premotor
neurons in the RVLM. Thus, the RVLM is a major site at
which interactions between different inputs regulating sympathetic activity occurs. In addition, it is a likely site, together
with the NTS, at which inputs from higher centers modulate
baroreceptor, chemoreceptor, and other cardiovascular reflexes
(Fig. 11) (13, 19).
The reflex effects of activation of these various inputs on the
sympathetic outflow are not uniform (Fig. 12). For example,
baroreceptor stimulation results in reflex vasodilation in skeletal muscle vascular beds and a modest vasodilator effect on
the skin blood vessels, whereas chemoreceptor stimulation has
a similar effect on skin blood vessels, but evokes a powerful
vasoconstrictor effect on skeletal muscle vascular beds (24).
Refresher Course
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
Direct projections
Higher brain
regions
Direct and indirect
projections
Arterial
baroreceptors
Arterial
chemoreceptors
Nucleus of solitary
tract (NTS)
Cardiopulmonary
receptors
Nasopharyngeal
receptors
Medullary
trigeminal (V)
nucleus
Vestibular
receptors
Medullary
vestibular (VIII)
nucleus
Skin nociceptors
Dorsal horn of
spinal cord
Sympathetic outflow
Heart
Skin blood
vessels
Renal blood
vessels
Skeletal muscle
blood vessels
Fig. 11. Schematic diagram summarizing the essential central connections
within the brain stem of different reflexes regulating the sympathetic vasomotor outflow. Note that there are direct inputs from all receptors to the NTS and
that the RVLM is also a site of convergence of signals from all receptors,
which are conveyed by direct inputs or indirect inputs via the NTS. There are
also inputs to the NTS and RVLM from higher brain regions, which can
modify the reflex responses arising from the various peripheral receptors.
Finally, note that there are separate descending outputs from the RVLM, each
of which exclusively or preferentially regulates the sympathetic outflow to
blood vessels in different regions. This allows for a differentiated control of the
sympathetic outflow according to the pattern of inputs from peripheral receptors and higher brain regions.
Such differentiated effects on the sympathetic outflows to
different vascular beds reflect the fact that there are subgroups
of sympathetic premotor neurons in the RVLM that preferentially or exclusively control different sympathetic outflows
(Fig. 11) (13, 29).
Blood volume. The essential central pathways subserving the
reflexes described above are contained within the lower brain
stem, although they can be powerfully modulated by descending inputs from higher brain regions. In contrast, the central
regulatory mechanisms defending the body against a decrease
in blood volume (e.g., as a result of hemorrhage or dehydration) are located in the forebrain as well as the lower brain stem
and include neural, hormonal, and behavioral components. The
signals that activate compensatory responses to a decrease in
blood volume are also complex, including those that are an
immediate consequence of the hypovolemia as well as secondary effects that result from the hypovolemia (15).
For example, hypovolemia caused by dehydration results in
increased blood osmolarity as well as reduced atrial and arterial
pressures (as a consequence of the reduced blood volume and
venous return) (Fig. 13). Apart from the reflex changes in
sympathetic activity resulting from unloading of cardiopulmonary and arterial baroreceptors (11, 13), the reduced arterial
pressure also activates the renin-angiotensin system (Fig. 13).
The increased levels of osmolarity and ANG II in the blood act
on receptors on neurons in the circumventricular organs in the
anterior wall of the third ventricle [especially the organum
vasculosum lamina terminalis (OVLT) and subfornical organ
(SFO)] (21, 32, 33, 50, 52). These neurons in the OVLT and
SFO have direct and indirect (via the median preoptic nucleus)
connections to the hypothalamic supraoptic nucleus (SON) and
paraventricular nucleus (PVN), and thus activation of these
neurons leads to increased sympathetic activity and vasopressin release from the pituitary (Fig. 13) (10, 15, 32, 33, 50, 52).
In addition, these signals also trigger an increase in drinking
(32, 33) (Fig. 13). The combined effect of all these compensatory responses is to minimize fluid loss and increase fluid
intake, thus restoring fluid homeostasis.
Apart from ANG II and Na⫹, other circulating substances
(e.g., relaxin, leptin, and cytokines) can also activate OVLT
and/or SFO neurons, and there is now strong evidence that both
these circumventricular organs, together with the median preoptic nucleus, are critical sites at which these circulating
substances can affect cardiovascular function. For example,
circulating relaxin acts on receptors in the OVLT and SFO to
stimulate vasopressin release (32). Second, infusion of leptin, a
hormone derived from adipose tissue, induces an increase in
renal sympathetic nerve activity, whereas blockade of leptin
receptors in the SFO prevents this effect (60). Third, circulating proinflammatory cytokines act on the brain to increase
blood pressure, heart rate, and sympathetic activity, and these
effects are blocked by lesions of the SFO (55). It should be
noted, however, that these results do not necessarily imply that
circulating leptin or cytokines exert their effects exclusively
via the SFO. For example, blockade of leptin receptors in the
hypothalamic arcuate nucleus also prevents the increase in
renal sympathetic nerve activity evoked by circulating leptin
(22), whereas Yu et al. (61) found that circulating proinflammatory cytokines can also increase sympathetic activity via
increases in prostaglandin production in perivascular macrophages located in hypothalamic regions outside the circumventricular organs.
Taken together, however, the results of many studies over
many years have led to the conclusion that the OVLT, SFO,
and median preoptic nucleus, which collectively is referred to
as the lamina terminalis, have a pivotal role in cardiovascular
regulation (for reviews, see Refs. 32, 33, and 50). This region
also plays an important role in maintaining increased sympathetic activity in at least some forms of experimental
hypertension, as first shown by the pioneering work of
Buggy et al. (7).
Body temperature. Maintenance of body core temperature
within narrow limits is critical for survival in mammals (37).
Ambient temperature is sensed by receptors in the skin,
whereas body core temperature is sensed by receptors in the
hypothalamic preoptic area, spinal cord, and abdomen (33, 37,
39). The afferent signals from all these receptors contribute to
thermoregulation, although it has been proposed that signals
from body core thermoreceptors are important mainly in more
extreme situations where the responses to inputs from periphReceptor
activated
Muscle
vasoconstrictor
Skin
vasoconstrictor
Cardiac
sympathetic
Baroreceptors
Chemoreceptors
Fig. 12. Examples of the different patters of reflex activation of the sympathetic outflow to different vascular beds in response to stimulation of arterial
baroreceptors and chemoreceptors.
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
Skeletal muscle
receptors
Rostral
ventrolateral
medulla (RVLM)
289
Refresher Course
290
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
A
B
Dehydration
SON
Blood osmolarity
Renin release
SFO & OVLT
Angiotensin II
level
MnPO
Vasopressin
release
Higher
integrative
centers
PVN
Sympathetic nerve
activity
SFO
PVN
OVLT
SON
C
c-Fos expression
Control
Hyperosmotic
SON
Drinking
Arterial
pressure
Reabsorption of
water in kidneys
MnPO
PVN
Restoration of
fluid balance
is an increase in the activity of nerves supplying skeletal
muscle, resulting in increased metabolic activity, which, together with increased BAT metabolic activity, also aids heat
production (Fig. 13) (37).
An increase in ambient temperature is detected by warmth
receptors in the skin and leads to autonomic and somatomotor
effects that are opposite to those described above (i.e., cutaneous vasodilation due to inhibition of sympathetic vasoconstrictor activity and excitation of sympathetic vasodilator activity,
together with inhibition of BAT thermogenesis and shivering)
(27, 37, 39, 46). In addition, in humans and other mammals
with sweat glands, sympathetic sudomotor activity is reflexly
increased, causing increased sweat production and consequently increased evaporative heat loss from the skin. In
mammals that lack sweat glands, panting is the most common
means of evaporative cooling (33, 39).
eral thermoreceptors are not adequate to maintain body core
temperature (39).
The central mechanisms that have evolved to maintain body
core temperature are complex and include autonomic (both
cardiovascular and noncardiovascular) and somatomotor components. For example, a decrease in ambient temperature is
detected by skin cold receptors, leading to reflex increases in
the activity of sympathetic nerves innervating skin blood vessels and skin piloerector muscle, causing skin vasoconstriction
and an increase in skin insulation, both of which reduce heat
loss and thus conserve heat (Fig. 14). In addition, it is now
known that, like many other species, both newborn and adult
humans have a significant amount of brown adipose tissue
(BAT), which is innervated by sympathetic nerves (48). An
increase in BAT sympathetic activity increases BAT metabolic
activity and thus heat production (Fig. 14). The somatomotor
component of the reflex response to ambient cold temperature
Cold ambient temperature
AUTONOMIC
Fig. 14. Flow diagram showing the autonomic and somatomotor responses evoked by
cold stress, leading to an increase in heat
conservation as well as heat production.
Sympathetic
activity to skin
blood vessels
SOMATOMOTOR
Skin cold receptor activity
Sympathetic activity
to piloerector
muscle
Sympathetic activity
to brown adipose
tissue (BAT)
Skeletal muscle
motoneuron activity
Shivering
Vasoconstriction
Skin
insulation
Metabolic
activity
Heat conservation
Heat production
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
Fig. 13. A: flow diagram showing the sequence of events following dehydration,
which leads ultimately to compensatory cardiovascular, hormonal, and behavioral responses that restore fluid balance. The subfornical organ (SFO) and organum vasculosum lamina terminalis (OVLT) are key
components of these central mechanisms via
their projections to the paraventricular nucleus (PVN), median preoptic nucleus
(MnPO), and supraoptic nucleus (SON) in the
hypothalamus. B: sagittal section of the rat
brain indicating the locations of the nuclei
referred to in A. C: examples of increased
neural activity, indicated by c-Fos expression, within the SON and PVN induced in a
rat after dehydration compared with a control
rat. [Modified from Ho et al. (21).]
Arterial
pressure
Cardiac
output
Refresher Course
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
291
A
DMH
MnPO
eLPB
PO
RP
sc
Skin
B
BAT, shivering
thermogenesis
MnPO
dLPB
PO
warm skin
RP
sc
Skin vasoconstriction inhibited
Skin shivering thermogenesis inhibited
Figure 15A shows the neural pathways that mediate the
physiological responses to cold stress. Afferent fibers conveying signals from cold receptors terminate in the dorsal column
of the spinal cord, from which an ascending pathway conveys
cold signals to the median preoptic nucleus (MnPO) in the
hypothalamus via a relay in the external subnucleus of the
lateral parabrachial nucleus (eLPB) (33, 37). From the MnPO,
there are direct and indirect descending projections to the raphe
pallidus in the midline medulla, synapsing with sympathetic
premotor neurons that produce skin vasoconstriction and BAT
thermogenesis, as well as premotor neurons that control shivering thermogenesis (33, 37). The indirect descending pathways include synapses in the preoptic area and dorsomedial
hypothalamus (DMH), which are also thus important components of central thermoregulatory mechanisms (33, 37). In
response to a heat stress, the signals arising from warm receptors in the skin are also conveyed to the MnPO, but via a
separate ascending pathway that includes a relay in the dorsolateral subnucleus of the lateral parabrachial nucleus (dlPB)
(Fig. 15B). The neurons in the MnPO that receive these inputs
project to and excite neurons in the preoptic area that inhibit
the sympathetic premotor neurons that produce skin vasoconstriction and BAT thermogenesis, both directly and via the
DMH (Fig. 15B) (33).
The MnPO thus plays a central role in thermoregulation as
well as in the regulation of blood volume, as discussed above.
Furthermore, it has become clear that the MnPO is also a
critical region for other homeostatic functions, including the
regulation of salt balance and sleep (33).
Central Mechanisms Coordinating Cardiovascular
Responses With Different Behaviors: Central Command
The above examples of central cardiovascular mechanisms
all involve reflexes with feedback from peripheral receptors.
As stated in the Introduction, the other general mechanism of
central cardiovascular control is central command, or feedfor-
ward control. Such cardiovascular responses are components
of more complex and highly coordinated responses, which
typically include appropriate respiratory and behavioral components.
Defensive behavior. The ability to respond rapidly and
appropriately to a threat in the external environment is critical
for survival, and so it is not surprising that highly complex
brain systems have evolved that subserve such defensive responses. Such responses may be triggered by a wide variety of
stimuli, which may be either unconditioned salient stimuli
arising from the external environment (e.g., sight, sound, or
odor of a predator or prey) or else conditioned stimuli (e.g.,
stimuli that are normally innocuous but which an animal has
CORTICAL
cortex
Conditioned
stimulus
SUB-CORTICAL
amygdala
hippocampus
thalamus
External
salient
stimulus
midbrain
BRAINSTEM
Sympathetic
activity
hypothalamus
pons/
medulla
Respiratory
activity
Hormone
release
Motor activity
(e.g. freezing)
Fig. 16. Flow diagram showing the major central connections at cortical,
subcortical, and brain stem levels that subserve the autonomic, respiratory, and
somatomotor responses to both conditioned and unconditioned stimuli that
signal a real or potential threat in the external environment.
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
cold skin
DMH
Fig. 15. Diagram showing the brain pathways that mediate cold and warm defense
mechanisms in response to skin cooling (A)
and skin warming (B). Red lines indicate
excitatory neural pathways; blue lines indicate inhibitory neural pathways. As discussed in the text, both an inhibition of skin
vasoconstrictor activity as well as excitation
of skin vasodilator activity contribute to the
skin vasodilation reflexly evoked by warming. The central pathways mediating excitation of skin vasodilator nerves, however,
have not been defined. dLPB, dorsal subnucleus of the lateral parabrachial nucleus;
DMH, dorsomedial hypothalamus; eLPB,
external subnucleus of the lateral parabrachial nucleus; PO, preoptic region; RP, raphe
pallidus nucleus; sc, spinal cord. [Modified
from McKinley et al. (33) with permission.]
Refresher Course
292
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
mPFC
PAG
PVN
NTS
DMH
PeF
Amy
RVLM
Acute
psychological
stressor
via cortex, amygdala & brainstem
DMH/PeF
Baroreflex
resetting
Baroreceptor
inputs
NTS
CVLM
RVLM
Premotor
nucleus
(RVMM?)
Medullary
raphe
Central
respiratory
nuclei
Sympathetic
outflow
Sympathetic
outflow
Phrenic
nucleus
Visceral
vasoconstriction
learned is indicative of a threat or other stimulus that requires
immediate action).
A general scheme illustrating the brain regions that are
involved in generating these coordinated responses is shown in
Heart rate
Skin
vasoconstriction
BAT activity
Fig. 16. Signals relating to the stimulus (e.g., sight, sound, or
touch) reach the cortex, amygdala, and hippocampus via thalamic relay nuclei. The amygdala also receives inputs from the
cortex and hippocampus. The amygdala, which consists of
Flight or freezing
BP and HR
Visceral vasoconstriction
Hindlimb vasodilation&
Fig. 18. Schematic diagram showing the longitudinal columns within the midbrain PAG that mediate
different types of defensive responses. Neurons in
the lateral (l) and dorsolateral (dl) columns generate
active coping responses, characterized by flight or
freezing and increases in blood pressure (BP) and
HR, whereas neurons in the ventrolateral (vl) column generate passive coping responses, characterized by quiescence and decreases in BP and HR.
[Modified from Bandler et al. (2) with permission.]
Respiratory
activity
PAG
Dorsolateral (dl)
Lateral (l)
Ventrolateral (vl)
Active coping strategies evoked
from lPAG and dlPAG
Passive coping strategies
evoked from vlPAG
Quiescence
BP and HR
Sympathetic
activity&
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
Fig. 17. Flow diagram showing the major pathways that
subserve the cardiovascular and respiratory responses to
an acute psychological stressor. Note that the DMH and
perifornical area (PeF) are key components of these
pathways, and they receive inputs from the cortex,
amygdala, and brain stem that signal the real or perceived
threatening stimulus. Note also that the sympathetically
mediated vasoconstriction is dependent on two mechanisms: 1) central command subserved by sympathetic
premotor neurons located outside the RVLM, possibly in
the rostral ventromedial medulla (RVMM), and 2) baroreflex resetting, mediated by descending inputs from the
DMH/PeF. The solid lines indicate direct connections
that have been clearly identified, whereas the dashed lines
may be direct or indirect. Amy, amygdala; mPFC, medial
prefrontal cortex; PAG, periaqueductal gray. For other
abbreviations, see previous figures.
Refresher Course
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
ated with decreases in blood pressure and heart rate as well as
sympathoinhibition (2, 8, 26) (Fig. 18).
The precise pattern of responses generated by the PAG
naturally depends on the pattern of inputs to the PAG. For
example, inputs from visceral nociceptors trigger passive coping responses, whereas inputs from somatic nociceptors (e.g., a
painful stimulus to the skin) trigger active coping responses (2,
26). It is also important to note that active coping responses
triggered by physical stimuli (such as the above example of a
painful stimulus to the skin) are generated by activation of
neurons within the lateral PAG, whereas those triggered by
emotional or psychological stressors (e.g., sight, sound, or
odor of a predator or a perceived emotional stressor) generate a similar pattern of behavioral, cardiovascular, and
respiratory responses but via activation of the dorsolateral
PAG (Fig. 19) (14).
Fig. 19. Schematic diagram showing major inputs to the dlPAG and lPAG
and the proposed output pathways subserving the coordinated changes in
sympathetic vasomotor and respiratory activity regulated by the dlPAG and
lPAG. The lines with arrows indicate connections that are either direct
(monosynaptic) or indirect (polysynaptic). Neurons in the dlPAG are
activated primarily by inputs related to psychological stressors, whereas
those in the lPAG are activated primarily by inputs related to physical
stressors. Note that the dlPAG projects to the DMH via both direct and
indirect [via the superior lateral parabrachial nucleus (PBsl) or cuneiform
nucleus (CnF)]. The cardiovascular and respiratory responses generated
from the dlPAG are dependent on its connections with the DMH, whereas
the responses generated from the lPAG are mediated by direct descending
projections to the medulla. [From Dampney (12).]
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
several interconnected nuclei (43), plays a critical role in
generating cardiovascular and respiratory responses to unconditioned and conditioned alerting stimuli (6, 36). The input to
the amygdala from the hippocampus (Fig. 16) is essential for
the expression of physiological responses to conditioned stimuli but not unconditioned stimuli (43). Inputs arising from
unconditioned salient stimuli that project to the thalamus then
project to the amygdala directly or indirectly via the cortex
(Fig. 16). The direct input from the thalamus is believed to
generate rapid responses to simple external stimuli (e.g., a
sudden loud noise), whereas more complex stimuli require
cortical processing (43).
The output pathways from the amygdala to cardiovascular,
respiratory, and somatomotor nuclei in the lower brain stem
responses include synapses in hypothalamic and midbrain
regions (Fig. 16) (12). One of these regions is the DMH and
adjacent perifornical area (PeF), which, like the amygdala,
have a critical role in generating cardiovascular and respiratory
responses to alerting or stressful stimuli (5, 12, 16, 51). Apart
from the amygdala, there are also inputs to the DMH/PeF from
the cortex and brain stem (Fig. 17) that also may signal alerting
or stressful stimuli. The output pathways from the DMH/PeF
have not been completely identified but include direct descending projections to sympathetic premotor neurons in the medullary raphe pallidus that regulate the sympathetic outflows to
the heart, skin blood vessels, and BAT. These sympathetic
outflows are activated in response to alerting or stressful
stimuli (12) as well as in response to a cold stress, as discussed
above. In addition, there are output pathways from the DMH/
PeF to other sympathetic premotor neurons that regulate the
sympathetic outflow to renal, splanchnic, and other visceral
blood vessels. These premotor neurons are not within the
RVLM, but there is evidence that they are located more
medially, within the rostral ventromedial medulla (RVMM)
(12). Thus, in summary, the sympathetic premotor neurons that
drive the sympathetic outflow during arousal or defensive
behavior appear to be distinct from the sympathetic premotor
neurons within the RVLM that mediate the baroreceptor,
chemoreceptor, and other homeostatic cardiovascular reflexes,
as described above (see Central Mechanisms Subserving Homeostatic Reflexes).
As also discussed above, however, the baroreceptor reflex is
reset during defensive behaviors, such that the sympathetic
outflow continues to be regulated but within a higher operating
range of arterial blood pressure and sympathetic activity. The
DMH/PeF contains neurons that, when activated, reset the
baroreceptor-sympathetic reflex in this way (31), probably via
descending pathways to the NTS (Fig. 17) (12, 34).
It is well established that the PAG in the midbrain is another
brain region that can coordinate a wide variety of behavioral
responses associated with appropriate cardiovascular and respiratory changes (2, 8, 26). The PAG is organized into
longitudinal columns, including dorsolateral, lateral, and ventrolateral columns. The dorsolateral PAG and lateral PAG
columns regulate what has been termed an active coping
strategy (26), consisting of freezing and/or flight, associated
with increases in blood pressure and heart rate, visceral vasoconstriction, skeletal muscle vasodilation, and increased ventilation (Fig. 18) (2, 8, 26). Conversely, the ventrolateral PAG
column regulates what has been termed a passive coping
strategy (2, 26), consisting of behavioral quiescence, associ-
293
Refresher Course
294
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
Conclusions and Key Points
This article has attempted to highlight some of the key
pathways and mechanisms in the brain that are responsible for
regulating the autonomic outflow to the cardiovascular system.
I have emphasized that cardiovascular regulatory mechanisms
do not operate in isolation but are closely coordinated with
respiratory and other regulatory mechanisms to maintain homeostasis. The key points can be summarized as follows:
• The brain regulates the cardiovascular system by two general means: 1) feedforward regulation (central command)
and 2) feedback regulation (reflex control).
• The baroreceptor and chemoreceptor reflexes are the primary homeostatic reflexes.
• The baroreceptor reflex regulates blood pressure not at a
constant fixed level but at a level appropriate for each
particular behavioral state (e.g., rest, exercise, or sleep).
• The chemoreceptor reflex maintains oxygenation of the
arterial blood but in cases of O2 deficiency also conserves
O2, often in concert with other reflexes (e.g., pulmonary
reflexes or the diving reflex).
• Other critical reflexes maintain body temperature and salt
and water balance.
• The brain also can generate patterned changes in autonomic,
respiratory, and neuroendocrine activity during different
behaviors (e.g., exercise, defense, feeding, sexual activity, or
sleep).
• The essential circuitry for baroreceptor and chemoreceptor
reflexes is in the lower brain stem but can be modified by
inputs from higher centers or other peripheral inputs.
• The lamina terminalis in the forebrain (OVLT, SFO, and
median preoptic nucleus) is critical for the regulation of salt
and water balance and in the long-term regulation of sympathetic activity and blood pressure.
• The brain mechanisms regulating cardiovascular and respiratory changes during defensive behavior are complex, but
the prefrontal cortex, amygdala, hypothalamus, midbrain
PAG, and colliculi play key roles.
• During arousal and defensive behavior, orexin (hypocretin)
neurons in the hypothalamus are activated, and this has the
effect of facilitating the cardiovascular and respiratory responses associated with these behaviors.
ACKNOWLEDGMENTS
The author thanks the organizers of the American Physiological Society
2015 Teaching Refresher Course on the Brain and Systems Control, and
particularly Dr. Catharine Young, for the opportunity to participate in the
session on which this article is based.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
R.A.D. prepared figures; R.A.D. drafted manuscript; R.A.D. edited and
revised manuscript; R.A.D. approved final version of manuscript.
REFERENCES
1. Asmussen E, Nielsen M. Alveolo-arterial gas exchange at rest and during
work at different O2 tensions. Acta Physiol Scand 50: 153–166, 1960.
2. Bandler R, Keay KA, Floyd N, Price J. Central circuits mediating
patterned autonomic activity during active vs. passive emotional coping.
Brain Res Bull 53: 95–104, 2000.
3. Barna BF, Takakura AC, Moreira TS. Acute exercise-induced activation of Phox2b-expressing neurons of the retrotrapezoid nucleus in rats
may involve the hypothalamus. Neuroscience 258: 355–363, 2014.
4. Biscoe TJ, Purves MJ, Sampson SR. The frequency of nerve impulses in
single carotid body chemoreceptor afferent fibres recorded in vivo with
intact circulation. J Physiol 208: 121–131, 1970.
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
These differences in inputs to the lateral PAG and dorsolateral PAG are also reflected in differences in outputs (Fig. 19).
Whereas neurons in the lateral PAG descend directly to the
medulla where they synapse with neurons regulating somatomotor, cardiovascular, and respiratory responses, there are no
direct descending projections to the medulla from the dorsolateral PAG (Fig. 19) (14). There are, however, ascending
projections from the dorsolateral PAG to the DMH (Fig. 19),
and this projection is essential for the expression of cardiovascular and respiratory responses generated from the dorsolateral
PAG (12, 14). Thus, the DMH is a site of convergence of
inputs related to psychological stressors that are relayed via the
dorsolateral PAG as well as those from the cortex and
amygdala, as discussed above.
A further component of the brain mechanisms that subserve
the cardiovascular and respiratory responses associated with
defensive behavior is the basal ganglia/colliculi system [for a
more detailed review of this system, see Müller-Ribeiro et al.
(40)]. The basal ganglia/colliculi system is phylogenetically
ancient and independent of the cortex and DMH/PeF and is
capable of responding to threats that require immediate stereotyped responses (17, 40). In contrast, the defense systems
described above that include the DMH/PeF and cortex as
important components appear to be better adapted to integrating responses to more sustained threats that require cognitive
appraisal.
Exercise. The cardiovascular and respiratory changes associated with exercise have been well described, both in animals
and humans (9, 16, 34, 45, 47). It is well established that
central command plays a major role in generating these responses (Fig. 2B) (58), but reflexes also have an important role
(16, 34, 58).
There are many similarities in the pattern of cardiovascular
and respiratory changes associated with exercise and psychological stress (e.g., in both cases, there are increases in blood
pressure, heart rate, and cardiac output, vasoconstriction in the
renal and splanchnic beds, and vasodilation in skeletal muscle
beds) (16). In addition, in both exercise and psychological
stress, the baroreflex is reset in a similar way, as described
above (e.g., Fig. 5). This naturally raises the question as to
whether the cardiovascular and respiratory responses to exercise and those to stress are driven, at least in large part, by the
same central mechanisms. Relatively little is known about the
brain regions responsible for central command during exercise
(58), although studies in animals have indicated that the DMH
and immediately adjacent regions are activated during exercise
(3), as is the case in psychological stress (12). Furthermore,
neurons that contain the peptide orexin (also called hypocretin)
in the DMH/PeF are activated during both exercise and stress,
and it is thought that orexin neurons facilitate cardiorespiratory
responses in both exercise and psychological stress (28).
In summary, the studies to date are consistent with the
hypothesis that the cardiovascular and respiratory responses
associated with exercise and psychological stress are driven by
common central mechanisms, at least in part.
Refresher Course
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
28. Kuwaki T, Zhang W. Orexin neurons as arousal-associated modulators of
central cardiorespiratory regulation. Resp Physiol Neurobiol 174: 43–54,
2010.
29. McAllen RM, May CN, Campos RR. The supply of vasomotor drive to
individual classes of sympathetic neuron. Clin Exp Hypert 19: 607– 618,
1997.
30. McDowall LM, Dampney RA. Calculation of threshold and saturation
points of sigmoidal baroreflex function curves. Am J Physiol Heart Circ
Physiol 291: H2003–H2007, 2006.
31. McDowall LM, Horiuchi J, Killinger S, Dampney RAL. Modulation of
the baroreceptor reflex by the dorsomedial hypothalamic nucleus and
perifornical area. Am J Physiol Regul Integr Comp Physiol 290: R1020 –
R1026, 2006.
32. McKinley MJ, Mathai ML, McAllen RM, McClear RC, Miselis RR,
Pennington GL, Vivas L, Wade JD, Oldfield BJ. Vasopressin secretion:
osmotic and hormonal regulation by the lamina terminalis. J Neuroendocrinol 16: 340 –347, 2004.
33. McKinley MJ, Yao ST, Uschakov A, McAllen RM, Rundgren M,
Martelli D. The median preoptic nucleus: front and centre for regulation
of body fluid, sodium, temperature, sleep and cardiovascular homeostasis.
Acta Physiol 214: 8 –32, 2015.
34. Michelini LC, O’Leary DS, Raven PB, Nobrega AC. Neural control of
circulation and exercise: a translational approach disclosing interactions
between central command, arterial baroreflex, and muscle metaboreflex.
Am J Physiol Heart Circ Physiol 309: H381–H392, 2015.
35. Miki K, Yoshimoto M, Tanimizu M. Acute shifts of baroreflex control
of renal sympathetic nerve activity induced by treadmill exercise in rats. J
Physiol 548: 313–322, 2003.
36. Mohammed M, Kulasekara K, de Menezes RC, Ootsuka Y, Blessing
WW. Inactivation of neuronal function in the amygdaloid region reduces
tail artery blood flow alerting responses in conscious rats. Neuroscience
228: 13–22, 2013.
37. Morrison SF. 2010 Carl Ludwig Distinguished Lectureship of the APS
Neural Control and Autonomic Regulation Section: Central neural pathways for thermo- regulatory cold defense. J Appl Physiol 110: 1137–1149,
2011.
38. Morrison SF, Reis DJ. Reticulospinal vasomotor neurons in the RVL
mediate the somatosympathetic reflex. Am J Physiol Regul Integr Comp
Physiol 256: R1084 –R1097, 1989.
39. Morrison SF, Nakamura K. Central neural pathways for thermoregulation. Front Biosci 16: 74 –104, 2011.
40. Müller-Ribeiro FC, Goodchild AK, McMullan S, Fontes MA, Dampney RA. Coordinated autonomic and respiratory responses evoked by
alerting stimuli: role of the midbrain colliculi. Resp Physiol Neurobiol
226: 87–93, 2016.
41. Ogoh S, Wasmund WL, Keller DM, O-Yurvati A, Gallagher KM,
Mitchell JH, Raven PB. Role of central command in carotid baroreflex resetting in humans during static exercise. J Physiol 543: 349 –364,
2002.
42. Panneton WM, Gan Q, Juric R. The rat: a laboratory model for studies
of the diving response. J Appl Physiol 108: 811– 820, 2010.
43. Phelps EA, LeDoux JE. Contributions of the amygdala to emotion
processing: from animal models to human behavior. Neuron 48: 175–187,
2005.
44. Raven PB, Fadel PJ, Ogoh S. Arterial baroreflex resetting during exercise: a current perspective. Exp Physiol 91: 37– 49, 2006.
45. Rowell LB. Human cardiovascular adjustments to exercise and thermal
stress. Physiol Rev 54: 75–159, 1974.
46. Rowell LB. Cardiovascular aspects of human thermoregulation. Circ Res
52: 367–379, 1983.
47. Rowell LB. Neural control of muscle blood flow: importance during
dynamic exercise. Clin Exp Pharmacol Physiol 24: 117–125, 1997.
48. Saito M, Okamatsu-Ogura Y, Matsushita M, Watanabe K, Yoneshiro
T, Nio-Kobayashi J, Iwanaga T, Miyagawa M, Kameya T, Nakada K,
Kawai Y, Tsujisaki M. High incidence of metabolically active brown
adipose tissue in healthy adult humans: effects of cold exposure and
adiposity. Diabetes 58: 1526 –1531, 2009.
49. Sarelius I, Pohl U. Control of muscle blood flow during exercise: local
factors and integrative mechanisms. Acta Physiol 199: 349 –365, 2010.
50. Smith PM, Ferguson AV. Circulating signals as critical regulators of
autonomic state-central roles for the subfornical organ. Am J Physiol
Regul Integr Comp Physiol 299: R405–R415, 2010.
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
5. Bondarenko E, Beig MI, Hodgson DM, Braga VA, Nalivaiko E.
Blockade of the dorsomedial hypothalamus and the perifornical area
inhibits respiratory responses to arousing and stressful stimuli. Am J
Physiol Regul Integr Comp Physiol 308: R816 –R822, 2015.
6. Bondarenko E, Hodgson DM, Nalivaiko E. Amygdala mediates respiratory responses to sudden arousing stimuli and to restraint stress in rats.
Am J Physiol Regul Integr Comp Physiol 306: R951–R959, 2014.
7. Buggy J, Fink GD, Johnson AK, Brody MJ. Prevention of the development of renal hypertension by anteroventral third ventricular tissue
lesions. Circ Res 40, Suppl 1: I110 –I117, 1977.
8. Carrive P. The periaqueductal gray and defensive behavior: functional
representation and neuronal organization. Behav Brain Res 58: 27– 47,
1993.
9. Castellani JW, Maresh CM, Armstrong LE, Kenefick RW, Riebe D,
Echegaray M, Kavouras S, Castracane VD. Endocrine responses during
exercise-heat stress: effects of prior isotonic and hypotonic intravenous
rehydration. Eur J Appl Physiol 77: 242–249, 1998.
10. Coble JP, Grobe JL, Johnson AK, Sigmund CD. Mechanisms of brain
renin angiotensin system-induced drinking and blood pressure: importance
of the subfornical organ. Am J Physiol Regul Integr Comp Physiol 308:
R238 –R249, 2015.
11. Dampney RA. Cardiovascular and respiratory reflexes: physiology and
pharmacology. In: Clinical Autonomic Disorders, edited by Low P,
Benarroch E. Philadelphia, PA: Lippincott, Williams & Wilkins, 2008, p.
43–56.
12. Dampney RA. Central mechanisms regulating coordinated cardiovascular
and respiratory function during stress and arousal. Am J Physiol Regul
Integr Comp Physiol 309: R429 –R443, 2015.
13. Dampney RA. Functional organization of central pathways regulating the
cardiovascular system. Physiol Rev 74: 323–364, 1994.
14. Dampney RA, Furlong TM, Horiuchi J, Iigaya K. Role of dorsolateral
periaqueductal grey in the coordinated regulation of cardiovascular and
respiratory function. Auton Neurosci 175: 17–25, 2013.
15. Dampney RA, Horiuchi J. Functional organisation of central cardiovascular pathways: studies using c-fos gene expression. Prog Neurobiol 71:
359 –384, 2003.
16. Dampney RA, Horiuchi J, McDowall LM. Hypothalamic mechanisms
coordinating cardiorespiratory function during exercise and defensive
behaviour. Auton Neurosci 142: 3–10, 2008.
17. Dean P, Redgrave P, Westby GW. Event or emergency? Two response
systems in the mammalian superior colliculus. Trends Neurosci 12:
137–147, 1989.
18. Gandevia SC, Killian K, McKenzie DK, Crawford M, Allen GM,
Gorman RB, Hales JP. Respiratory sensations, cardiovascular control,
kinaesthesia and transcranial stimulation during paralysis in humans. J
Physiol 470: 85–107, 1993.
19. Guyenet PG. The sympathetic control of blood pressure. Nat Rev Neurosci 7: 335–346, 2006.
20. Guyenet PG. Regulation of breathing and autonomic outflows by chemoreceptors. Compr Physiol 4: 1511–1562, 2014.
21. Ho JM, Zierath DK, Savos AV, Femiano DJ, Bassett JE, McKinley
MJ, Fitts DA. Differential effects of intravenous hyperosmotic solutes on
drinking latency and c-Fos expression in the circumventricular organs and
hypothalamus of the rat. Am J Physiol Regul Integr Comp Physiol 292:
R1690 –R1698, 2007.
22. Harlan SM, Morgan DA, Agassandian K, Guo DF, Cassell MD,
Sigmund CD, Mark AL, Rahmouni K. Ablation of the leptin receptor in
the hypothalamic arcuate nucleus abrogates leptin-induced sympathetic
activation. Circ Res 108: 808 – 812, 2011.
23. Hooley J. Decoding the oxyhemoglobin dissociation curve. Am Nurse
Today 10: 18 –23, 2015.
24. Jänig W. Pre- and postganglionic vasoconstrictor neurons: differentiation,
types, and discharge properties. Annu Rev Physiol 50: 525–539, 1988.
25. Kanbar R, Oréa V, Barrès C, Julien C. Baroreflex control of renal
sympathetic nerve activity during air-jet stress in rats. Am J Physiol Regul
Integr Comp Physiol 292: R362–R367, 2007.
26. Keay KA, Bandler R. Parallel circuits mediating distinct emotional
coping reactions to different types of stress. Neurosci Biobehav Rev 25:
669 – 678, 2001.
27. Kellogg DL. In vivo mechanisms of cutaneous vasodilation and vasoconstriction in humans during thermoregulatory challenges. J Appl Physiol
100: 1709 –1718, 2006.
295
Refresher Course
296
THE BRAIN AND THE CARDIOVASCULAR SYSTEM
51. Stotz-Potter EH, Willis LR, DiMicco JA. Muscimol acts in dorsomedial
but not paraventricular hypothalamic nucleus to suppress cardiovascular
effects of stress. J Neurosci 16: 1173–1179, 1996.
52. Toney GM, Stocker SD. Hyperosmotic activation of CNS sympathetic drive:
implications for cardiovascular disease. J Physiol 588: 3375–3384, 2010.
53. van der Kooy D, Koda LY, McGinty JF, Gerfen CR, Bloom FE. The
organization of projections from the cortex, amygdala, and hypothalamus
to the nucleus of the solitary tract in rat. J Comp Neurol 224: 1–24, 1984.
54. Veerman DP, Imholz BP, Wieling W, Wesseling KH, van Montfrans GA.
Circadian profile of systemic hemodynamics. Hypertension 26: 55–59, 1995.
55. Wei SG, Zhang ZH, Beltz TG, Yu Y, Johnson AK, Felder RB. Subfornical
organ mediates sympathetic and hemodynamic responses to blood-borne
proinflammatory cytokines. Hypertension 62: 118 –125, 2013.
56. Weil JV, Byrne-Quinn E, Sodal IE, Kline JS, McCullough RE, Filley
GF. Augmentation of chemosensitivity during mild exercise in normal
man. J Appl Physiol 33: 813– 819, 1972.
57. White S, McRitchie RJ, Korner PI. Central nervous system control of
cardiorespiratory nasopharyngeal reflexes in the rabbit. Am J Physiol 228:
404 – 409, 1975.
58. Williamson JW, Fadel PJ, Mitchell JH. New insights into central
cardiovascular control during exercise in humans: a central command
update. Exp Physiol 91: 51–58, 2006.
59. Yates BJ, Bolton PS, Macefield VG. Vestibulo-sympathetic responses.
Compr Physiol 4: 851– 887, 2014.
60. Young CN, Morgan DA, Butler SD, Mark AL, Davisson RL. The
brain subfornical organ mediates leptin-induced increases in renal
sympathetic activity but not its metabolic effects. Hypertension 61:
737–744, 2013.
61. Yu Y, Zhang ZH, Wei SG, Serrats J, Weiss RM, Felder RB. Brain
perivascular macrophages and the sympathetic response to inflammation in rats after myocardial infarction. Hypertension 55: 652– 659,
2010.
Downloaded from http://advan.physiology.org/ by 10.220.33.5 on June 15, 2017
Advances in Physiology Education • doi:10.1152/advan.00027.2016 • http://advan.physiology.org