* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Retrovirus-mediated gene transfer corrects DNA repair
Epigenetics of human development wikipedia , lookup
Genome (book) wikipedia , lookup
DNA supercoil wikipedia , lookup
Cell-free fetal DNA wikipedia , lookup
Epigenomics wikipedia , lookup
Gene therapy wikipedia , lookup
Non-coding DNA wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Zinc finger nuclease wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
Genetic engineering wikipedia , lookup
Deoxyribozyme wikipedia , lookup
Molecular cloning wikipedia , lookup
Cre-Lox recombination wikipedia , lookup
Extrachromosomal DNA wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Primary transcript wikipedia , lookup
DNA damage theory of aging wikipedia , lookup
Mir-92 microRNA precursor family wikipedia , lookup
DNA vaccination wikipedia , lookup
Oncogenomics wikipedia , lookup
Helitron (biology) wikipedia , lookup
Designer baby wikipedia , lookup
Genome editing wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Cancer epigenetics wikipedia , lookup
Microevolution wikipedia , lookup
Point mutation wikipedia , lookup
History of genetic engineering wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
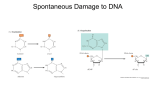
Gene Therapy (1997) 4, 1077–1084 1997 Stockton Press All rights reserved 0969-7128/97 $12.00 Retrovirus-mediated gene transfer corrects DNA repair defect of xeroderma pigmentosum cells of complementation groups A, B and C L Zeng, X Quilliet, O Chevallier-Lagente, E Eveno, A Sarasin and M Mezzina Laboratoire de Génétique Moléculaire, UPR 42 CNRS, 94801 Villejuif, France With the aim to devise a long-term gene therapy protocol for skin cancers in individuals affected by the inherited autosomal recessive xeroderma pigmentosum, we transferred the human DNA repair XPA, XPB/ERCC3 and XPC cDNAs, by using the recombinant retroviral vector LXSN, into primary and immortalized fibroblasts obtained from two XP-A, one XP-B (associated with Cockayne’s syndrome) and two XP-C patients. After transduction, the complete correction of DNA repair deficiency and functional expression of the transgenes were monitored by UV survival, unscheduled DNA synthesis and recovery of RNA synthesis, and Western blots. The results show that the recombinant retroviruses are highly efficient vectors to transfer and stably express the human DNA repair genes in XP cells and correct the defect of DNA repair of group A, B and C. With our previous results with XPD/ERCC2, the present work extends further promising issues for the gene therapy strategy for most patients suffering from this cancer-prone syndrome. Keywords: retroviral vectors; DNA repair genes; skin cancer therapy; xeroderma pigmentosum Introduction Xeroderma pigmentosum (XP) is a rare human autosomal recessive disease characterized clinically by hypersensitivity to ultraviolet (UV) rays, high predisposition for developing skin cancers (basal and squamous cell carcinomas and melanomas) on sunlight exposed areas,1 and in some cases, neurological disorders.2–4 XP has a worldwide distribution, with the incidence varying from about 1:250 000 in Europe and the USA to as high as 1:40 000 in Japan, North Africa and in Egypt.5–7 The cellular phenotype of XP has increased sensitivity to killing following exposure to a wide variety of DNA damaging agents, including UV radiation and UV mimetic chemicals. The observation that skin fibroblasts in culture from an XP patient are unable to carry out nucleotide excision repair (NER) following exposure to UV established the relationship between DNA repair defect and skin photocarcinogenesis in man.1,8,9 The systematic complementation of DNA repair defects by cell fusion assay has led to the identification of seven genetic groups in this disease, designated XP-A to -G,7 and a variant group, designated XP-V, exhibiting normal NER.10 So far, most of the relevant human genes, such as XPA, XPB, XPC, XPD, XPF and XPG, have been cloned and mapped to different specific chromosomal locations. A further source of NER defective mutants is a set of 11 complementation groups of UV-sensitive rodent cells. The human genes that correct the rodent cell phenotype are designated ERCC (excision repair cross- Correspondence: M Mezzina Received 24 March 1997; accepted 23 May 1997 complementing) genes.11,12 Among them, ERCC2, ERCC3, ERCC4, ERCC5 and ERCC6 were found to be identical to the genes involved in xeroderma pigmentosum groups D, B, F and G and Cockayne’s syndrome group B.13–17 A multiprotein complex of approximately 30 gene products is involved in the NER pathway, whereby DNA damage is eliminated and replaced by excision-resynthesis, as has been demonstrated by using the in vitro repair assay with purified factors.18 Mutations in one of these genes result in UV-sensitive disorders: skin cancer-prone XP and other clinically different syndromes, such as skin cancerfree trichothiodystrophy (TTD) and Cockayne syndrome (CS), and association of XP with CS. The NER process is evolutionarily conserved in eukaryotes, and homologue genes of human repair genes have been identified in many organisms, namely in Saccharomyces cerevisiae.19 In humans, the proteins encoded by some of these genes are components of the multiprotein TFIIH complex involved with RNA polymerase II in basal transcription. Consistently, the yeast homologues of some of these proteins, the Rad25 and Rad3 (homologue to ERCC3/XPB and ERCC2/XPD, respectively), have also been identified as components of TFIIH. Therefore, these proteins play a dual role in both NER and transcription.20–22 The mean age of XP patients at the time of diagnosis is 3 years while the mean age of onset of first skin cancer is 8 years. There is an approximate 30–40 year reduction in survival. Many patients have died of neoplasms. 2 So far, there is no effective long-term treatment available for XP patients. Some protective measures can be taken to keep patients from exposure to sunlight,23 and skin grafts from the same patient were performed to resurface the area with cancer in some patients. However, the latter Correction of inborn DNA repair defect by gene transfer L Zeng et al 1078 therapeutical protocol is efficient only in the short term, since skin grafts are still genetically DNA repair defective and thus cancer prone.24 The genetic correction of XP cells by retrovirus-mediated transduction with appropriate DNA repair genes may allow possible alternative long-term therapies. Studies in vitro have shown that DNA repair defects can be corrected by introducing relevant DNA repair genes into cells derived from XP patients.25,26 Several retroviral constructions are efficient tools for gene delivery and stable expression in many human cells and tissues. 27 We recently devised the first retrovirus harboring a DNA repair gene (XPD/ERCC2), which efficiently transduces several DNA repair-deficient human primary skin fibroblasts belonging to the complementation XP-D group and fully corrects their DNA repair defect.28,29 In order to validate this investigation with other genes involved in XP disease and to dispose of basic tools for gene therapy for a larger population of patients, we decided to develop additional constructions harboring other available DNA repair cDNAs. In this paper, we describe the construction of retrovirus harboring the genes XPA, XPB and XPC and show that their expression fully corrects the DNA repair-deficient phenotype of fibroblasts from two XP-A, one XP-B and two XP-C patients. Results Establishment of recombinant retrovirus The LXPASN, LXPBSN and LXPCSN vectors were derived from the Moloney murine leukemia virus (MoMLV)-based retroviral vector LXSN and were produced after insertion into the polylinker of XPA, XPB and XPC cDNAs as described in Materials and methods and depicted in Figure 1. The expression of the introduced sequence was under the control of the LTR promoter and the polyadenylation signal. After transfection of CCRE packaging cells, subsequent infection of CCRIP cells and selection with G418,30–32 among all clones tested, the best virus titers obtained were 3 × 105 c.f.u./ml for LXPASN, 3 × 106 c.f.u./ml for LXPBSN and 2 × 106 c.f.u./ml for LXPCSN. The difference of virus titers might be due to either different expression levels of neo marker or the cytotoxic effect of the transgene, or both. complementation groups, transduced and untransduced cells were analyzed for: (1) UV survival: The colony-forming ability was determined in primary and SV40 immortalized cells. Figure 2 shows survival curves of wild-type SV40 immortalized MRC5V1 and diploid 198VI fibroblast compared with those of UV-sensitive untransduced XP12ROSV and XP24VI (XP-A group, Figure 2a and b, respectively), XPCS2BASV (XP-B group, Figure 2c) and XP16VI and XP30VI (XP-C group, Figure 2d). After transduction with the retrovirus harboring the appropriate cDNA, all cell lines recovered wild-type UV resistance, since their survival curves were indistinguishable from those of 198VI and MRC5V1 lines (Figure 2a–d). When XP cells were cross-transduced with retrovirus containing other cDNA than that involved in the genetic group, no correction of UV survival was observed (Figure 2a, c and d, dotted lines). This indicates that the retroviral transduction is gene specific, consistent with our previous observations with LXPDSN.28,29 (2) Unscheduled DNA synthesis (UDS): To correlate the recovery of UV survival with the ability to perform repair synthesis, the incorporation of 3H-thymidine was measured after UV irradiation (Figure 3). Both XP12ROSV and XP24VI exhibited reduced UDS levels, (5.4 ± 2 and 2.9 ± 1.1 grains per nucleus) at 15 J/m2, corresponding to 26 and 14.6% of normal levels, respectively. After transduction of the same cells with LXPASN, the UDS levels were restored to almost normal levels (18 ± 4 and 17 ± 5 grains per nucleus, respectively, corresponding to 85% of the normal levels, Figure 3a and b). XPCS2BASV cells showed virtually a complete defect of DNA repair with all three Gene-specific correction of DNA repair defect To examine whether the transferred XPA, XPB and XPC correct the DNA repair defect of cells of the three XP Figure 1 Scheme of retroviral vector LXSN based on Moloney murine leukemia virus. LTR: long terminal repeat; C+: packaging signal; polylinker for insertion of DNA repair cDNAs: XPA, XPB and XPC; SV40: simian virus 40 early promoter; NEO: neomycin phosphotransferase gene. Arrows show transcription initiation orientation. Figure 2 UV survival curves in untransduced and transduced XP groups A, B and C cells. (–l–) MRC5V1 (a and c) and 198VI (b and d) wildtype cells; (–p–) XP12ROSV (a), XP24VI (b), XPCS2BASV (c) and XP16VI (d) untransduced and (–P–) transduced cells with LXPASN, LXPBSN and LXPCSN, respectively; (–g–) untransduced and (–G–) transduced XP30VI cells with LXPCSN (d); (--K--) cells transduced with LXPCSN (a and c) and LXPBSN (d, for XP30VI cells only). Correction of inborn DNA repair defect by gene transfer L Zeng et al 1079 Figure 3 Unscheduled DNA synthesis of transduced and untransduced XP-A (a and b), XP-B/CS (c) and XP-C (d) cells. UV doses (,2 grains per nucleus). However, an 87% of repair synthesis (46.7 ± 8 grains per nucleus) compared with normal cells (54 grains per nucleus) at 15 J/m2 was observed in cells transduced with LXPBSN (Figure 3c). The DNA repair synthesis in XP-C cells was recovered at least by 80% of normal cells 198VI (37 ± 6 grains per nucleus) for XP16VI + LXPCSN (30 ± 11 grains per nucleus) and by 92% for XP30VI + LXPCSN (34 ± 7 grains per nucleus), whereas untransduced XP-C cells displayed few grains (0.6 to approximately 4) per nucleus (Figure 3d). (3) Recovery of RNA synthesis (RRS): Because of the association of XP with CS in the XPCS2BA patient, we decided to measure RRS level, which is dramatically impaired in cells from CS and XP/CS.33,34 Therefore, the incorporation of 3H-uridine, measured as described in Materials and methods, was performed in XPCS2BASV before and after LXPBSN transduction. Figure 4b shows that a low RRS level was found (5 ± 2 grains per nucleus) at 24 h after irradiation in untransduced XPCS2BASV cells, compared with that of wild-type cells (.250 grains per nucleus, Figure 4a), while transduced cells showed a wild-type RRS level (Figure 4c). Expression of XPA, XPB and XPC proteins To correlate the correction of UV survival and change of DNA repair properties in transduced cells with the expression of the proteins encoded by introduced cDNA, Western blot analysis was carried out on different cell lines by using cell extracts obtained from untransduced and transduced cells. The proteins of these extracts were resolved by electrophoresis in SDS-polyacrylamide gels, and analyzed by Western blot, as described in Materials and methods by using specific antibodies. Figure 5a and c shows that the XPA and XPC proteins, while clearly detectable in wild-type, were undetectable in XP-A and Figure 4 Recovery of RNA synthesis in MRC5V1 (a), untransduced (b) and transduced (c) XPCS2BASV cells (original magnification × 200). XP-C cells. After retroviral transduction, the level of the signal of these proteins became similar to that of wildtype cells. Similar results could be obtained in untransduced/transduced XPCS2BASV over MRC5V1 cells, with the exception that XPB protein is detectable in XP-B cell extracts, although the signal is lower than in wild-type or transduced cells (Figure 5b). Confirmation of the genetic correction of XP-B cells at RNA level Because the monoclonal antibody 1B3 could not differentiate the mutated XPB from the wild-type protein by Western blot (Figure 5b), in order to confirm that the phenotypic correction is correlated with the expression of transgene, we amplified by RT-PCR a 205 bp fragment of XPB/ERCC3 exon 3 from position 22 to 225 as decribed in Materials and methods. This fragment, when amplified from XPCS2BASV DNA, contains an additional Correction of inborn DNA repair defect by gene transfer L Zeng et al 1080 transduced XPCS2BASV cells (Figure 6b, lanes 2 and 6). The 37 and 19 bp fragments are too short to be visible in the gel conditions used. Discussion Figure 5 Detection of the XPA, XPB and XPC proteins by Western blot. Indicated cell extracts were processed as described in Materials and methods and membranes were probed with anti-XPA (a), anti-XPB (b) and anti-XPC (c) antibodies. HinfI restriction site generated by a T→C transition at position 62 (Figure 6a), yielding F99S substitution in XPB protein, which is present in only one allele.35 HinfI cleavage produces two smaller fragments of the expected size of 185 and 148 bp (Figure 6a) only in untransduced XPCS2BASV cells (Figure 6b, lane 4). An identical pattern of 185 bp fragments was observed in MRC5V1 and in Figure 6 Restriction analysis of RT-PCR amplified fragment of XPB/ERCC3 exon 3. (a) Diagrams showing HinfI sites in wild-type and XPCS2BASV cells and the expected size (bp) of the fragments generated. Between the two diagrams the nucleotide sequence flanking the T→C transition (arrow) is indicated; underlined sequences designate the HinfI site. Numbers in italic indicate the sequence positions. (b) Restriction pattern of RT-PCR amplified 205 bp fragment from wild-type, untransduced and transduced XPCS2BASV cells, before (lanes 1, 3 and 5) and after (lanes 2, 4 and 6) HinfI digestion. The 200 bp marker position is indicated on the left side of the picture. In previous reports we described the first retrovirus carrying a DNA repair gene (LXPDSN) which efficiently transduces diploid fibroblasts from DNA repair-deficient patients belonging to the XP-D group.28,29 This first result allowed us to envisage a novel gene therapy for skin cancers in XP patients. However, unlike other monogenic human disorders, several genes are involved in XP. They encode for the multi-protein complex which, in normal individuals, removes DNA damage and prevents deleterious consequences of UV radiation (skin cancers and other pathologies, including neurological degenerations). This heterogeneity of symptoms in XP patients reflects the genetic heterogeneity of the disease. In fact, severe neurological degenerations are often accompanied by skin tumors in patients belonging to XP-A and XP-D groups, and other metabolic dysfunctions typical of CS (growth and mental retardation, gonadal development impairment, dwarfism and deafness) could be found associated with some XP-B, XP-D and XP-G patients.36 This implies that some DNA repair gene products play a role not only in the mere NER, but also in other pathways involved in cell differentiation and in development. Therefore, we developed retroviral vectors carrying additional DNA repair genes with the aims: (1) to validate the novel transduction technology for other genes involved in XP; and (2) among them, to transduce cells from individuals belonging to the XP-A and XP-C groups, which are the most representative in the XP patient population (27 and 26%, respectively).36 Furthermore, unlike most XP-A, XP-B and XP-D patients, XP-C individuals suffer only from skin tumors (without the above mentioned complex clinical features) and, thus, they are the most probable candidates for gene therapy protocol. The precise role of each DNA repair protein has not yet been established. However, biochemical data of purified proteins and/or amino acid (aa) sequence data allowed us to suggest a specific role in the NER pathway for each protein. XPA XPA protein is a zinc metalloprotein consisting of 273 amino acids which, in connection with XPE protein, binds preferentially to UV- or chemical carcinogeninduced damaged DNA, and, synergically with other proteins (belonging to the TFIIH factor), drives other proteins of the complex toward the lesions and allows excision of damaged DNA strands. This suggests that it is involved in the recognition step of several types of DNA damage.37–39 According to previous results, showing a reduced amount of XPA mRNAs and protein,40–42 XP12ROSV cells exhibited no detectable XPA protein, when revealed by Western blot with anti-XPA antiserum. The chain termination mutation at codon 207 generally predicts synthesis of a truncated protein containing the first 206 of the 273 amino acids of the intact XPA protein. However, such truncated XPA polypeptide has never been shown so far. We also observed a similar result for XP24VI cells, where a similar chain elongation mutation Correction of inborn DNA repair defect by gene transfer L Zeng et al is also present in exon 4 (K Tanaka, personal communication). This suggests that this portion of the gene is essential for the stability of XPA gene products, either at mRNA or protein level, or both. However, following transduction with the recombinant LXPASN retrovirus, XPA protein could be easily detected by Western blot in XP12ROSV cell extract (Figure 5a). Therefore, the restoration of XPA protein expression is sufficient to correct UV sensitivity and DNA repair to normal levels in both cells. XPB XPB protein is an 89 kDa species belonging to the TFIIH complex and it possesses a 3′–5′ ATP-dependent helicase activity. In connection with the 5′–3′ helicase activity of XPD protein, it releases DNA damaged strand after excision.43 It is required for the transcriptional activity of TFIIH complex. Therefore, it plays a dual role in both NER and transcription. Only three families belong to the XP-B group: two presenting a combination of XP and CS (XP11BE and XPCSBA) and one presenting mild symptoms of TTD. Although the precise role of causative mutations in patients has not yet been established, different mutations, such as phenylalanine-to-serine (F99S) and threonine-to-proline (T119S) substitutions, lead to different cellular phenotypes (in terms of DNA repair) and clinical symptoms in patients, ie XP/CS combination and TTD, respectively.35,44 Our results showed a high sensitivity of XPCS2BASV cells to the cytotoxic effect of UV in colony-forming assays, and a poor level of residual UDS (,1% of normal), indicating that the F99S mutation causes virtually complete inactivation of the DNA repair function of the XPB protein. Furthermore, Western blots showed a reduced amount of 89 kDa polypeptide (Figure 5b), according to the hypothesis that in XPCS2BA only the paternal allele is expressed.35 Nevertheless, the reduced level of ERCC3 transcript could also be explained by alteration of the expression of ERCC3/XPB by the mutation. Transduction with LXPBSN confers, however, wild-type expression level of the protein and only wild-type mRNA species are expressed (Figure 5b), suggesting that dominant expression of the transgene over the endogenous mutant one occurs. XPC The XPC protein is a 125 kDa polypeptide45 and its activity is supposed to drive repair proteins to damage DNA in nontranscribed strands, since XP-C cells display defective repair of lesions localized only in nontranscribed strands. Furthermore, mutations in the p53 gene in skin tumors from these patients were detected only in nontranscribed strands.46 All mutations in the XPC gene (single aa substitutions, insertion or chain terminating) identified in several XP-C individuals, were accompanied by a many-fold reduction of XPC mRNA levels.47 In XP30VI and XP16VI cells used here, the low UV survival rate and reduced UDS levels (Figures 2d and 3d) are also accompanied by undetectable XPC protein by Western blots (Figure 5c). Although mutations in our cell lines are not yet identified, we can deduce that alterations in the XPC gene may yield unstable transcripts and altered forms of the protein might not be detectable with conventional Western blotting procedure. Our results have proved that the wild-type XPC protein corrects the repair defect and restores the UV survival rate and the expression of XPC protein to normal levels in our XP-C cell lines. Therefore, this biochemical feature is consistent with the clinical features of XP-C patients, since XP patients with neurological abnormalities are generally found in groups A, B and D, but not in group C. Materials and methods Clinical and genetical data of patients XP donors are listed in Table 1. The XP12RO and the XP24VI patients have skin and neurological abnormalities and both cell lines exhibited UV hypersensitivity. Patient XP12RO carries a C→T transition at nucleotide 619 of exon 5 in the XPA gene. This mutation alters the Arg-207 codon (CGA) to a nonsense codon (TGA) in both alleles.48 XP24VI was assigned to the XP-A group by somatic fusion and microinjection experiments. The XP24VI patient came from a consanguinous marriage and presented photosensitivity from 5 months after birth, and was diagnosed as XP at the age of 5 years with an apparent facial dysmorphosis and difficulty in walking. However, no cutaneous tumor was found at the time of diagnosis. XPCS2BASV cell line came from one of two brothers with relatively mild clinical symptoms of combined XP and CS and with a virtually complete deficiency of NER. This line was assigned to the XP-B group by microinjection experiments. The sequence analysis on PCR-amplified mRNA revealed a single base substitution (T→C transition), resulting in a phenylalanine-to-serine substitution at position 99 (F99S), and this mutation was found in only one allele. 35 The XP30VI patient was diagnosed as classical XP at the age of 2 years without tumor and the XP16VI patient was diagnosed at the age of 7 years with multiple facial carcinoma. Both were confirmed as XP complementation group C by cell fusion experiments. Cell culture conditions Cells were grown at 37°C in 5% CO2 humidified atmosphere in Eagle’s minimal essential medium (GIBCO, Inchinnan, UK) supplemented with 15% fetal calf serum (Dominique Dutscher, Strasbourg, France) and antibiotics at 1 mg/ml each of penicillin and streptomycin and 2.5 mg/ml of fungizone (GIBCO), while 10% FCS was used for transformed cells. NIH3T3 and retrovirus packaging CCRE and CCRIP cells were grown at 37°C in 10% CO2 in DMEM medium supplemented with fetal bovine serum and antibiotics. Construction of vectors and production of recombinant retrovirus The retroviral LXSN vector is based on MoMLV. 31,32 Figure 1 depicts LXSN containing a selectable neomycin (G418) marker which is under the control of the SV40 early promoter. XPA and XPB genes are the fragments of 0.91 kb and 2.85 kb full-length cDNA, respectively.49,50 XPC gene is a fragment of 3.55 kb full-length cDNA.45 These genes were inserted into appropriate restriction sites in LXSN polylinker. The recombinant vectors were named according to the order of genetic elements in the vectors: LXPASN for XPA, LXPBSN for XPB and LXPCSN for XPC. To reduce the potential for helper virus production, we chose two retrovirus-packaging cell lines, CCRE and CCRIP, to produce recombinant retrovirus.30 CCRE cell 1081 Correction of inborn DNA repair defect by gene transfer L Zeng et al 1082 Table 1 Donors and cell lines Donors Phenotype Cells derived 198VI MRC5V1 wild type diploid fibroblasts SV40-transformed XP24VI XP12RO XP diploid fibroblast SV40-transformed XPCS2BA XP/CS SV40-transformed XP-B JHJ Hoeijmakers (Rotterdam, The Netherlands) XP16VI XP30VI XP diploid fibroblasts XP-C Villejuif, France line was cultured in a 6-cm Petri dish at 5 × 105 for 12 h and then the cells were transfected with 5 mg of DNA of each of the three recombinant plasmids using the standard calcium phosphate method. When the cells reached confluency, the culture supernatant was harvested, filtered and used to transduce the CCRIP cell line in the presence of polybrene (Sigma-Aldrich Chimie, St Quentin Fallavier, France) at 8 mg/ml. CCRIP cell line was cultured in the presence of neomycin (GIBCO) at 1 mg/ml for selection and neo-resistant clones obtained were tested for retrovirus titer by transducing NIH3T3 fibroblasts under neomycin selection (1 mg/ml). For every recombinant retrovirus at least 15 G418-resistant colonies were expanded and their titers were determined. These titers may vary from 103 to 106 c.f.u./ml according to the different genes cloned and, for the same construction, to different individual clones. Clones producing the retrovirus with higher titers were expanded. Primary fibroblasts and transformed cells were transduced with the recombinant retrovirus according to the genetic complementation groups and were selected with 1 mg/ml of neomycin and grown in the presence of neomycin for at least 8 weeks. UDS and RRS Analysis of repair synthesis was carried out in untransduced and transduced primary and transformed fibroblasts as previously described.51 Briefly, cells were grown on glass coverslips for 2 days. After 2 more days in serum-deprived medium (0.5%) they were UV irradiated with doses from 0 to 15 J/m2 and then incubated with 3 H-thymidine at 10 mCi/ml (specific activity of 50 Ci/mmol; DuPont de Nemors, Les Ulis, France) for 3 h, followed by a chase of 1 h with cold thymidine. Coverslips with the cells were mounted on to glass slides, dipped in Kodak NTB-2 emulsion (Kodak, New York, NY, USA), and exposed for 1 week at 4°C. The mean number of grains per nucleus was obtained by counting at least 30 non-S-phase nuclei. RRS was measured as follows: cells were grown as for UDS experiments and UV irradiated with 15 J/m2. Cells were then incubated for 23 h and then labeled for 1 h in a medium containing 3Huridine at 10 mCi/ml (specific activity of 50 Ci/mmol). Autoradiography was performed as described above for measurement of UDS except that the exposure time was 24 h. UV survival The colony-forming ability was determined in primary and transformed fibroblast cells by seeding increasing Genetic group Source Villejuif, France C Arlett (Brighton, UK) XP-A Villejuif, France D Bootsma (Rotterdam, The Netherlands) cell numbers in function of UV doses (approximately 1 × 103 to 8 × 103 and 2 × 104 to 2 × 106 for primary and transformed cells, respectively). Irradiation was performed as in UDS experiments and cells were maintained in medium supplemented with 20% and 10% FCS for primary and transformed fibroblasts, respectively, for 14 days. The relative survival was calculated as the number of colonies obtained in UV irradiated over unirradiated cells. Detection of gene expression (Western blot) The proteins encoded by the introduced genes were analyzed by 6 or 8% (according to the molecular mass of proteins to be analyzed) acrylamide-SDS gel electrophoresis of cellular extracts obtained from different cell lines. Protein samples were transferred into Hybond+ membranes (Amersham, Les Ulis, France) and probed with specific antibodies, according to the manufacturer’s procedure: anti-XPA antiserum (kindly provided by Dr K Tanaka, IMCB, Osaka University, Japan); the monoclonal anti-XPB antibody (1B3) raised against the N-terminal of human XPB protein (AA 80–480) was a gift from Dr JM Egly (Strasbourg, France); and the polyclonal antibody raised against human XPC protein was kindly provided by Dr F Hanaoka (IMCB, Osaka University, Japan). Reverse transcription PCR amplification Total RNA was isolated from approximately 1 × 108 cells from MRC5V1 (normal), XPCS2BASV (XP-B/CS) and XPCS2BASV transduced by recombinant retrovirus LXPBSN, using the RNA Isolation Kit (Bioprobe Systems, Montreuil-sous-Bois, France). RNA (5 mg) was used for reverse transcription reaction. Briefly, RNA was dissolved in 10 ml of reverse transcriptase buffer (250 mm Tris-HCl (pH 8.3), 375 mm KCl, 15 mm MgCl2), in the presence of RNase inhibitor (Boehringer Mannheim, Meylan, France), 5 ml of 0.1 m DTT, 5 ml of 10 mm dNTP, 1 mg of poly-dT and 400 units of MoMLV reverse transcriptase (GIBCO) were added, and then incubated at 37°C for 30 min. PCR was performed to amplify the fragment from position 22 to 225 in exon 3 of XPB/ERCC3 containing the T→C transition (Figure 6a) using primers: 5′-TTGGAAGCCTTCTCTCCAG TTTACAAATATGC-3′ and 5′-GCATAATTCCATCAGGGACTCCAGTCTTG-3′ (GENSET, Paris, France). To 1 mg of cDNA, PCR reaction contained 10 ml of Taq reaction buffer (100 mm Tris-HCl, pH 8.8, 15 mm MgCl2, 500 mm KCl, 1% Triton X-100), 1 ml (1 pmole/ml) of each primer, 10 ml of dNTPs (2 mm), and 1.5 U of Taq polymerase (Bioprobe Systems). Amplification was performed by 30 cycles in 100 ml total vol- Correction of inborn DNA repair defect by gene transfer L Zeng et al ume, 1 min denaturing at 95°C, 1 min annealing at 55°C, and 1 min extension at 72°C. Finally, the amplified DNA fragments were digested by HinfI (New England BioLabs, Distributor: Ozyme, Montigny-le-Bretonneux, France) and then analyzed by agarose gel electrophoresis. Acknowledgements This work was supported by grants from the Association Française contre les Myopathies (AFM, Evry, France), the Association pour la Recherche sur le Cancer (ARC, Villejuif, France), the Fédération Nationale des Groupements des Entreprises Françaises dans la Lutte Contre le Cancer (FEGEFLUC, Marseille, France) and the Ligue Nationale Contre le Cancer (LNCC, Versailles, France). L Zeng and X Quilliet are fellows from AFM and the Institut de Formation Supérieure Biomédicale (IFSBM, Villejuif, France), respectively. We are endebted to: Drs K Tanaka, F Hanaoka (Osaka University, Japan), G Weeda (Erasmus University, Rotterdam, The Netherlands) and J-M Egly (CNRS/INSERM, Strasbourg, France) for providing antibodies and cDNA-containing plasmids; Drs C Arlett (MRC, Brighton, UK), D Bootsma and JHJ Hoeijmakers (Erasmus University, Rotterdam, The Netherlands) for providing cell lines and Drs O Danos (AFM-GENETHON, Evry, France) and J-M Heard (Institut Pasteur, Paris, France) for providing packaging cells and helpful discussion. References 1 Cleaver JE. Defective repair replication of DNA in xeroderma pigmentosum. Nature 1968; 218: 652–656. 2 Kraemer KJ, Lee MM, Scotto J. Xeroderma pigmentosum. Cutaneous ocular and neurological abnormalities in 830 published cases. Arch Dermatol 1987; 123: 241–250. 3 Robbins JH. Defective DNA repair causes skin cancer and neurodegeneration. JAMA 1988; 260: 384–388. 4 Sarasin A. The paradox of DNA repair deficient diseases. Cancer J 1991; 4: 233–237. 5 Robbins JH et al. Xeroderma pigmentosum. An inherited disease with sun sensitivity, multiple cutaneous neoplasms and abnormal DNA repair. Ann Intern Med 1974; 80: 221–248. 6 Takebe H et al. DNA repair characteristics and skin cancers of xeroderma pigmentosum patients in Japan. Cancer Res 1977; 367: 490–495. 7 Cleaver JE, Kraemer KH. Xeroderma pigmentosum. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds). The Metabolic Basis of Inherited Diseases, vol. 2. McGraw Hill: New York, 1989, pp 2949–2971. 8 Cleaver JE. Xeroderma pigmentosum: a human disease in which an initial stage of DNA repair is defective. Proc Natl Acad Sci USA 1969; 63: 428–435. 9 Setlow RB, Regan JD, German J, Carrier WL. Evidence that xeroderma pigmentosum cells do not perform the first step in the repair of ultraviolet damage to their DNA. Proc Natl Acad Sci USA 1969; 64: 1035–1041. 10 Lehmann AR et al. Xeroderma pigmentosum cells with normal levels of excision repair have a defect in DNA synthesis after UV irradiation. Proc Natl Acad Sci USA 1975; 72: 219–223. 11 Busch D et al. Summary of complementation groups of UVsensitive CHO cell mutants isolated by large-scale screening. Mutagenesis 1989; 4: 349–354. 12 Riboni R et al. Identification of the eleventh complementation group of UV-sensitive excision repair-defective rodent mutants. Cancer Res 1992; 52: 6690–6691. 13 Weeda G et al. A presumed DNA helicase encoded by ERCC-3 is involved in the human repair disorders xeroderma pigmentosum and Cockayne’s syndrome. Cell 1990; 62: 777–791. 14 Flejter WL et al. Correction of xeroderma pigmentosum complementation group D mutant cell phenotypes by chromosome and gene transfer: involvement of the human ERCC2 DNA repair gene. Proc Natl Acad Sci USA 1992; 89: 261–265. 15 Sijbers AM et al. Xeroderma pigmentosum group F caused by a defect in a structure-specific DNA repair endonuclease. Cell 1996; 86: 811–822. 16 O’Donovan A, Wood RD. Identical defects in DNA repair in xeroderma pigmentosum group G and rodent ERCC group 5. Nature 1993; 363: 185–188. 17 Troelstra C et al. ERCC6, a member of a subfamily of putative helicases, is involved in Cockayne’s syndrome and preferential repair of active genes. Cell 1992; 71: 939–953. 18 Aboussekhra A et al. Mammalian DNA nucleotide excision repair reconstituted with purified protein components. Cell 1995; 80: 859–868. 19 Weeda G, Hoejimakers JHJ. Genetic analysis of nucleotide excision repair in mammalian cells. Semin Cancer Biol 1993; 4: 105–107. 20 Schaeffer L et al. DNA repair helicase: a component of BTF2 (TFIIH) basic transcription factor. Science 1993; 260: 58–63. 21 Drapkin R et al. Dual role of TFIIH in DNA excision repair and in transcription by RNA polymerase II. Nature 1994; 368: 769– 772. 22 van Vuuren A et al. Correction of xeroderma pigmentosum repair defect by basal transcription factor BTF2 (TFIIH). EMBO J 1994; 13: 1645–1653. 23 Davis BE et al. Sunlight avoidance and cancer prevention in xeroderma pigmentosum. Arch Dermatol 1994; 130: 806–808. 24 Atabay K et al. Facial resurfacing in xeroderma pigmentosum with monoblock full-thickness skin graft. Plast Reconstr Surg 1991; 87: 1121–1125. 25 Mezzina M et al. Correction by the ERCC2 gene of UV sensitivity and repair deficiency phenotype in a subset of trichothiodystrophy cells. Carcinogenesis 1994; 15: 1493–1498. 26 Gözükara EM et al. The human DNA repair gene, ERCC2 (XPD), corrects ultraviolet hypersensitivity and ultraviolet hypermutability of a shuttle vector replicated in xeroderma pigmentosum group D cells. Cancer Res 1994; 54: 3837–3844. 27 Clinical Protocols. Cancer Gene Therapy 1994; 1: 73–78. 28 Carreau M et al. Functional retroviral vector for gene therapy of xeroderma pigmentosum group D patients. Human Gene Ther 1995; 6: 1307–1315. 29 Quilliet X et al. Long-term complementation of DNA repair deficient human primary fibroblasts by retroviral transduction of the XPD gene. Mutation Res 1996; 364: 161–169. 30 Danos O, Mulligan RC. Safe and efficient generation of recombinant retroviruses with amphotropic and ecotropic host ranges. Proc Natl Acad Sci USA 1988; 85: 6460–6464. 31 Miller AD, Miller DG, Garcia JV, Lynch CM. Use of retroviral vectors for gene transfer and expression. Meth Enzymol 1993; 217: 581–599. 32 Miller AD, Rosman GJ. Improved retroviral vectors for gene transfer and expression. Biotechniques 1989; 7: 980–989. 33 Mayne LV, Lehmann AR. Failure of RNA synthesis to recover after UV irradiation: an early defect in cells from individuals with Cockayne’s syndrome and xeroderma pigmentosum. Cancer Res 1982; 42: 1473–1478. 34 Venema J et al. The genetic defect in Cockayne’s syndrome is associated with a defect in repair of UV-induced DNA damage in transcriptionally active DNA. Proc Natl Acad Sci USA 1990; 87: 4707–4711. 35 Vermeulen W et al. Clinical heterogeneity within xeroderma pigmentosum associated with mutations in the DNA repair and transcription gene ERCC3. Am J Hum Genet 1994; 54: 191–200. 36 Cleaver J, Kraemer KH. Xeroderma pigmentosum and Cockayne syndrome. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds). The Metabolic and Molecular Basis of Inherited Disease, 7th edn. McGraw Hill: New York, 1995, pp 4393–4419. 37 Robins P et al. Complementation of DNA repair in xeroderma pigmentosum group A cell extracts by a protein with affinity for damaged DNA. EMBO J 1991; 10: 3913–3921. 1083 Correction of inborn DNA repair defect by gene transfer L Zeng et al 1084 38 Asahina H et al. The XPA protein is a zinc metalloprotein with an ability to recognize various kinds of DNA damage. Mutat Res 1994; 315: 229–237. 39 Kuraoka I et al. Identification of a damaged-DNA binding domain of the XPA protein. Mutat Res 1996; 362: 87–95. 40 Satokata I et al. Three nonsense mutations responsible for group A xeroderma pigmentosum. Mutat Res 1992; 273: 193–202. 41 McDowell ML, Nguyen T, Cleaver JE. A single-site mutation in the XPAC gene alters photoproduct. Mutagenesis 1993; 8: 155– 161. 42 Jones CJ, Cleaver JE, Wood RD. Repair of damaged DNA by extracts from a xeroderma pigmentosum complementation group A revertant and expression of a protein absent in its parental cell line. Nucleic Acids Res 1992; 20: 991–995. 43 Roy R et al. The DNA-dependent ATPase activity associated with the class II basic transcription factor BTF2/TFIIH. J Biol Chem 1994; 269: 9826–9831. 44 Weeda G et al. A mutation in the XPB/ERCC3 DNA repair transcription gene, associated with trichothiodystrophy. Am J Hum Genet 1997; 60: 320–329. 45 Masutani C et al. Purification and cloning of a nucleotide excision repair complex involving the xeroderma pigmentosum 46 47 48 49 50 51 group C protein and a human homologue of yeast RAD23. EMBO J 1994; 13: 1831–1843. Dumaz N, Drougard C, Sarasin A, Daya-Grosjean L. Specific UV-induced mutation spectrum in the p53 gene of skin tumors from DNA repair deficient xeroderma pigmentosum patients. Proc Natl Acad Sci USA 1993; 90: 10529–10533. Li L, Bales ES, Peterson CA, Legerski RJ. Characterization of molecular defects in xeroderma pigmentosum group C. Nat Genet 1993; 5: 413–417. Satokata I, Tanaka K, Yuba S, Okada Y. Identification of splicing mutations of the last nucleotides of exons, a nonsense mutation, and a missense mutation of the XPAC gene as causes of group A xeroderma pigmentosum. Mutat Res 1992; 273: 203–212. Tanaka K et al. Analysis of a human DNA excision repair gene involved in group A xeroderma pigmentosum and a zinc-finger domain. Nature 1990; 348: 73–76. Weeda G et al. Molecular cloning and biological characterization of the human excision repair gene ERCC3. Mol Cell Biol 1990; 10: 2570–2581. Sarasin A et al. Prenatal diagnosis in a subset of trichothiodystrophy patients defective in DNA repair. Br J Dermatol 1992; 127: 485–491.