* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download addiction
Synaptic gating wikipedia , lookup
Activity-dependent plasticity wikipedia , lookup
Nervous system network models wikipedia , lookup
Selfish brain theory wikipedia , lookup
Time perception wikipedia , lookup
Neurophilosophy wikipedia , lookup
Neurolinguistics wikipedia , lookup
Functional magnetic resonance imaging wikipedia , lookup
Neurotransmitter wikipedia , lookup
Brain morphometry wikipedia , lookup
Cognitive neuroscience wikipedia , lookup
Neuroplasticity wikipedia , lookup
Holonomic brain theory wikipedia , lookup
Neuroeconomics wikipedia , lookup
Haemodynamic response wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Neuropsychology wikipedia , lookup
Brain Rules wikipedia , lookup
Neuroanatomy wikipedia , lookup
History of neuroimaging wikipedia , lookup
Aging brain wikipedia , lookup
Metastability in the brain wikipedia , lookup
Substance dependence wikipedia , lookup
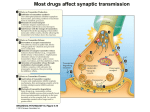
NEWSWEEK FEBRUARY 12, 200I ADDICTION SCIENCE: New research on how cocaine, heroin, alcohol and amphetamines target neuronal circuits is revealing the biological basis of addiction, tolerance, withdrawal and relapse. By Sharon Begley One by one, each crack addict took his turn in the fMRI tube, its magnets pounding away with a throbbing bass. A mirror inside was angled just so, allowing the addict to see a screen just outside the tube. Then the 10-minute video rolled. For two minutes, images of monarch butterflies flitted by; the fMRI, which detects active regions in the brain, saw nothing untoward. Then the scene shifted. Men ritualistically cooked crack ... an addict handed cash to a pusher ... users smoked. It was as if a Neurological switch had been thrown: seeing the drug scenes not only unleashed in the addicts a surge of craving for crack, but also triggered visible changes in their brains as their anterior cingulate and part of the prefrontal cortex-regions involved in mood and learning-lit up like Times Square. Nonaddicts show no such response. The fMRI had pinpointed physical changes in the brain that apparently underlie cue-induced craving, showing why walking past a bar, passing a corner crack house or even partying with the people you used to shoot up with can send a recovering addict racing for a hit. "The brain regions that became active are where memories are stored," says Dr. Scott Lukas of McLean Hospital in Massachusetts, who led the 1998 study. "These cues turn on crack-related memories, and addicts respond like Pavlov's dogs." "This is your brain on drugs": it's not just an advertising line. Through FMRI as well as PET scans, neuroscientists are pinpointing what happens in the brain during highs and lows, why withdrawal can be unbearable and-in one of the most sobering findings-how changes caused by addictive drugs persist long after you stop using. "Imaging and other techniques are driving home what we learned from decades of animal experiments;' says Dr. Alan Leshner, director of the National Institute on Drug Abuse. "Drugs of abuse change the brain, hijack its motivational systems and even change how its genes function." An addicted brain is different-physically different, chemically different-from a normal brain. A cascade of neurobiological changes accompanies the transition from voluntary to compulsive drug use, but one of the most important is this: cocaine, heroin, nicotine, amphetamines and other addictive drugs alter the brains pleasure circuits. Activating this circuit, also called the reward circuit, produces a feel-good sensation. Eating cheesecake or tacos or any other food you love activates it. So does sex, winning a competition, acing a test, receiving praise and other pleasurable experiences. The pleasure circuit communicates in the chemical language of dopamine: this neurotransmitter zips from neuron to neuron in the circuit like a molecular happy face, affecting the firing of other neurons and producing feelings from mild happiness to euphoria. What happens to the circuit if you inject, inhale or swallow an addictive drug? To find out, Dr. Hans Breiter of Massachusetts General Hospital and colleagues recruited cocaine addicts who had been using for an average of seven to eight years and had used on 16 of the past 30 days. After making sure none had a heart problem or any other condition that would put them at risk, Breiter and colleagues gave each a "party" dose of cocaine, up to about 40 milligrams for a 150-pound man. An fMRI took snapshots of their brains every eight seconds for 18 minutes. At first, during the "rush” phase, the addicts described feeling "out of control," as if they were "in a dragster" or "being dangled 10 feet off the ground by a giant hand." They also felt a high, a surge of energy and euphoria. The fMRI showed why cocaine made a beeline for the pleasure circuit, turning on brain areas called the sublenticular extended amygdala and nucleus aqccumbens and keeping them on. How? "Drugs of abuse increase the concentration of dopamine in the brain’s reward circuits," says Nora Volkow of Brookhaven National Lab. The drugs do that more intensely than any mere behavior, be it eating a four-star meal or winning the lottery. But each drug turns up this feel-good neurochemical in a different way: Cocaine blocks the molecule that ordinarily mops up dopamine sloshing around neurons. When all the seats on this so-called transporter molecule are occupied by cocaine, there is no room for dopamine, which therefore hangs around and keeps the pleasure circuit firing. The intensity of a cocaine high, Volkow found in 1997, is directly related to how much cocaine ties up the seats on the transporter bus. Amphetamines block the transporter, too. They also push dopamine out of the little sacs, called NEWSWEEK FEBRUARY 12, 200I vesicles, where neurons store it. More dopamine means more firing of neurons in the pleasure circuit. Heroin stimulates dopamine-containing neurons to fire, releasing the neurochemical into the nucleus accum-bens, a key re 'on in the pleasure circuit. Nicotine does the same. Heroin also excites the same neurons that our brain's natural opioids do, but much more powerfully. Alcohol opens the neurotransmitter floodgates. It releases dopamine, serotonin (which governs our sense of well-being) and the brain's own opioids. It also disturbs levels of glutamate, which incites neurons to fire and helps account for the initial alcoholic high, as well as GABA, which dampens neuronal firing and eventually makes (most) drinkers sleepy. After igniting these acute effects, an ad-dictive drug isn’t nearly through with the brain. Chronic use produces enduring changes. The most important: it reduces the number of dopamine receptors. Receptors are simply little molecular baseball gloves that sit on neurons, grab passing neuro-transmitters like fly balls and reel them in. Animal evidence suggests that the more you take an addictive drug, the more dopamine receptors you wipe out, as the brain attempts to quiet down an overly noisy pleasure circuit. Having fewer dopamine receptors means fewer of those passing dopamines get caught, and the pleasure circuit calms down. But now the law of unintended consequences kicks in. With fewer dopamine receptors, a hit that used to produce pleasure doesn’t. This is the molecular basis for tolerance. Drugs don't have the effect they originally did. To get the original high, the addict has to up his dose. But there's worse. The dearth of dopamine receptors means that experiences that used to bring pleasure become impotent. A good meal, a good chat, a good massage-none ignite that frisson of happiness they once did. The only escape from chronic dysphoria, irritability, anxiety and even depression, the user believes, is to take more drug. Initial use, in other words, may be about feeling good. But addiction is about avoiding abject, unremitting distress and despair. The agony of withdrawal is also a direct result of drugs' resetting the brain’s dopamine system. Withdrawal and abstinence deprive the brain of the only source of dopamine that produces any sense of joy. Without it, life seems not worth living. When a junkie stops supplying his brain with heroin, for instance, he becomes hypersensitive to pain, chronically nauseated and subject to uncontrollable tremors. "This is why addiction is a brain disease' says NIDA’s Leshner. "It may start with the voluntary act of taking drugs, but once you’ve got it, you can’t just tell the addict 'Stop' 'any more than you can tell the smoker 'Don't have emphysema.' Starting may be volitional. Stopping isn’t.” Although the biological basis of tolerance, addiction and withdrawal is yielding some of its secrets, relapse is harder to explain. Why does an addict who has abstained for weeks, months or longer suddenly reach for the needle or the bottle? According to lab-animal studies, abstinence allows dopamine receptors to eventually return to normal, so after some period of withdrawal agony the brain should stop craving the drug. Yet addiction is practically the dictionary definition of a relapsing disease. One clue might lie in Scott Lukas's fMRI findings about cue-induced craving. The memories of drug abuse are so enduring and so powerful that even seeing a bare arm beneath a rolled-up sleeve reawakens them. And just as Pavlov's dog learned to salivate when he heard a bell that meant "chow time," so an addict begins to crave his drug when he sees, hears or smells a reminder of past use. Relapse might also reflect enduring genetic changes. Drugs can act as DNA switches, turning genes on or off. In lab animals, for instance, bingeing on cocaine turns down the activity of a gene that makes a dopamine receptor, finds Dr. Mary Jeanne Kreek of Rockefeller University. If that gene remains chronically inactive, it could lay the basis for relapse as an addict tries to compensate for a crippled pleasure circuit. Genes may also explain, at least in part, why some people are at greater risk of drug addiction than others. It turns out that the same dqpamine system that drugs activate can also be turned on by novel experiences, finds Dr. Michael Bardo of the University of Kentucky. That suggests that people driven to experience the Next New Thing may be trying to appease the same primal pleasure as drug abusers - and that if they don’t by, say, bungee jumping, they may try to do so with drugs. In fact, people who compulsively seek novelty also tend to abuse drugs more than people who are content with the same-old same-old. And novelty-seeking seems to have a genetic basis. That suggests that "there is a heritable component to addiction;' says Kreek. But genes can also reduce the risk of addiction. Many Asians carry variants of genes that control the metabolism of alcohol. As a result, they suffer intense reactions-flushing, nausea, palpitations - from liquor. That could serve as a built-in defense against alcoholism, since people tend to avoid things that make them throw up. If only avoiding addiction were as easy for everyone else. 2