* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 16: Basal Ganglia
Molecular neuroscience wikipedia , lookup
Caridoid escape reaction wikipedia , lookup
Neuroplasticity wikipedia , lookup
Neurogenomics wikipedia , lookup
Biochemistry of Alzheimer's disease wikipedia , lookup
Externalizing disorders wikipedia , lookup
Embodied language processing wikipedia , lookup
Cognitive neuroscience of music wikipedia , lookup
Optogenetics wikipedia , lookup
Aging brain wikipedia , lookup
Neuroeconomics wikipedia , lookup
Neuroanatomy of memory wikipedia , lookup
Central pattern generator wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Anatomy of the cerebellum wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Neural correlates of consciousness wikipedia , lookup
Eyeblink conditioning wikipedia , lookup
Motor cortex wikipedia , lookup
Synaptic gating wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
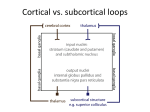
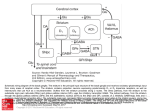
Chapter 16: Basal Ganglia Outline • • • • Anatomy Circuitry Clinical concepts Clinical cases Overview of function • BG Influence descending motor systems by participating in complex networks • Do not directly project to periphery • Lesions lead to two broad phenotypes – Hypokinetic – Hyperkinetic Anatomy • Grey matter nuclei deep within white matter BASAL GANGLIA Striatum Cellular bridges Caudate (head, body, tail) Putamen Globus pallidus Subthalamic nucleus Substantia nigra Pars reticulata, pars compacta Lentiform nucleus Anatomy • Relationships – Head of caudate + lentiform nucleus separated by Anterior limb of internal capsule – Lentiform nucleus and thalamus separated by Posterior limb internal capsule – So: • Caudate and thalamus always medial to IC • Putamen and GP always lateral to IC Brief review vascular supply • Main supply via lenticulostriate branches of MCA • Recurrent artery of Heubner (ACA) – Head of caudate and anterior lentiform nucleus • Anterior choroidal artery (ICA) – Medial GP Input, Output, Connections Inputs • • • • Main input to BG is to striatum Cortex +, Glutamate SNpc + and -, DA Thalamus +, Glutamate – Intralaminar nuclei in internal medullary lamina • Raphe nuclei modulation, serotonin Outputs • SNpr and GPi are main outputs, inhibitory • Thalamus – VL, VA, intralaminar, mediodorsal • Pontomedullary reticular formation – Affects reticulospinal tract • Superior colliculus – Affects tectospinal pathways Intrinsic connections • Excitatory/inhibitory connections within BG • Two main pathways: – Direct pathway – Indirect pathway – Both pathways exert effect via thalamus – Both receive input from SNpc (DAergic nigrostriatal pathway) Direct and Indirect Pathways Parallel BG pathways • Motor channel – Regulation of movement • Oculomotor channel – Regulation of eye movements • Prefrontal channel – Cognitive processes involving frontal lobes • Limbic channel – Limbic regulation of emotions and motivational drives – Role in neurobehavioral and psychiatric disorders Understanding movement disorders based on Pathways • Parkinson’s disease – Degeneration of DA-ergic neurons in SNpc • Hemiballismus – Contralateral STN lesion • Huntington’s disease – Degeneration of striatum, initially indirect pthway Understanding movement disorders Key Clinical Concept 1 – Movement Disorders • “Movement disorders” usually refers to abnormal movement 2ary to BG lesion • Exert effect via projections to cortex • Gradient of hypo- to hyperkinetic Bradykinesia, Hypokinesia, Akinesia • BG lesions that increase inhibition of thalamus – Loss of DA-ergic input from SNpc • Typified by PD – Loss of inhibition of SNr/GPi via direct pthwy – Loss of inhibition of STN • Other lesions – Diffuse lesions of frontal cortex, subcortical white matter, thalami, reticular formation – Depression, schizophrenia Rigidity • Increased resistance to passive limb mvment • Spasticity – Velocity-dependent rigidity in UMN lesions • Clasp-knife spasticity (corticospinal tract lesion) – Increase then decreased in resistive tone as stretch • Lead-pipe rigidity (BG lesion) – Continuous resistive tone throughout stretch • Cogwheel rigidity (PD and related disorders) – Rigidity with superimposed tremor • Paratonia or gegenhalten (frontal lobe dysfctn) – Active resistance to limb movement Dystonia • Abnormal, distorted position of limbs, trunk, face – May be focal, unilateral or generalised • Usually, no focal lesion in BG is found • Examples – Torticollis, blepharospasm, spasmodic dysphonia, writer’s cramp • Etiology – Antipsychotic or anti-emetic medications • Acute or after long-term use (tardive dyskinesia) – BG lesions 2ary infarct, tumor, abscess – Wilson’s, Huntington’s, Parkinson’s disease Athetosis • Writhing, twisting movements of limbs, face, trunk • May merge with chorea choreoathetosis • Etiology – – – – – – Perinatal hypoxia involving BG, Kernicterus Wilson’s disease Ataxia telangiectasia Huntington’s disease Antipsychotic and anti-emetic medications Treatment of PD with levodopa Chorea • Nearly continuous, involuntary movements that have fluid or jerky, varying quality • Involves limbs, trunk, neck, face, resp muscles • Range from mild low-amplitude to severe, large-amplitude movements • Worsen with distraction and ambulation • Etiology – – – – – Huntington’s disease Benign familial chorea Sydenham’s chorea Lupus Antipsychotics, anti-emetics, levodopa in PD, phenytoin Ballismus • Movements of proximal limb muscles with large amplitude, more rotatory or flinging than chorea • Hemiballismus – Unilateral movements 2ary to contralateral BG lesion – Classically, lacunar infarct in STN – Other causes: hemorrhage, tumor, infection Tics • Sudden, brief action – Preceded by urge to perform action – Followed by sense of relief • Motor tics – usu. involve face, neck • Vocal tics – variable, can be elaborate • Etiology – Tourette’s syndrome – Idiopathic tic disorders – 2ary to encephalitis, infarcts, hemorrhage, tumors Myoclonus • Sudden, rapid muscular jerk that is focal, unilateral or bilateral • Localisation: cortex, cerebellum, BG, brainstem, spinal cord • Etiology – Anoxic brain injury, encephalitis, toxic and metabolic encephalopathies – Epileptic cortical activity (e.g. JME) – Paraneoplastic disroders (SCLC, ovarian, breast) – CJD, CBD, late in Alzheimer’s Tremor • Rhythmic or semi-rhythmic oscillating mvmnts • Both agonist and antagonist muscles involved • Classification – Resting • Parkinsonian (3-5Hz), cerebellar (rubral), palatal – Postural • When pt’s limbs actively held in a position • Essential tremor (5-8Hz), toxic/metabolic, physiologic, NM disorder, PD, cerebellar – Intention (ataxic) • Appears when trying to move limb towards target • Cerebellar appendicular ataxia, postural tremor Key Clinical Concept 2 – Idiopathic Parkinson’s Disease • Sporadic, unknown etiology, onset 40-70 y.o. – Rarely, familial • Loss of DA-ergic neurons in SNpc – Lewy bodies in remaining DA-ergic neurons – Loss of pigmented neurons elsewhere in CNS • Diagnosis based on clinical features Idiopathic PD – Clinical Features • Resting tremor • Parkinsonian gait – Slow, shuffling, en bloc • Bradykinesia/hypokinesia – – – – Masked facies Hypophonia Slow saccades Micrographia • Cogwheel rigidity • Postural instability • Retropulsion turn, decreased arm swing • Dementia – 15-40%, late • • • • Bradyphrenia Starts unilaterally Insidious progression Responds to levodopa L-dopa in Idiopathic PD • Most effective drug for treatment • If no response to treatment consider alternative diagnosis • As disease progresses, on-off phenomena – Abnormal regulation of DA levels – May manage with SR, COMT inhibitors, MAOIs • Other treatment options – DA agonists (e.g. pramipexole) – Anticholinergics (e.g. benztropine) – MAOI (e.g. selegiline) Parkinsonism Plus Syndromes • Neurodegenerative conditions w/ atypical parkinsonism – Symmetrical Sx, no resting tremor, early postural instability, little response to DA-ergic agents • Examples – – – – – Multisystem atrophy Progressive supranuclear palsy Lewy body dementia Cortical basal ganglionic degeneration Huntington’s, Wilson’s Huntington’s Disease • Autosomal dominant inheritance pattern – Gene on chromosome 4, CAG trinuc repeats • 4-5/100,000, usu age of onset 30-50 y.o. • Progressive atrophy of striatum – Caudate > putamen > Nacc – All 4 functions of BG affected • Cortical atrophy later in course • Diagnosis – Clinical features, family Hx, genetic testing Clinical Features • Motor control – Clumsiness, subtle chorea, athetosis, tics, dystonic posturing • Eye movement control – Slow saccades, impaired smooth pursuit, difficulty initiating saccades • Cognition – Decreased attn, decreased memory, impaired executive function • Emotion regulation – Depression, anxiety, OCD, manic-like behavior Case 1 • 65M, HIV positive • HPI – Involuntary flinging mvmnts of Rt arm/leg – Worsened over 1 mo – Difficult to walk and use hand • O/E – Continuous wild, uncontrollable flapping and circular movements of Rt arm – Jerky mvments of Rt leg – Unsteady gait, falling to right Case 1 • What would you call this movement disorder? • On the basis of the symptoms and signs, where is the lesion? • What is the most likely diagnosis and what are some possibilities? Case 1 • Decreased inhibition of contralateral thalamus – Subthalamic lesion – Damage to indirect pathway Case 1 Case 2 • 35M, recent-onset jerky mvmnts, marital problems • HPI – Occasional irregular jerking of head, trunk, limbs over past months – Occasional stumbling with fall down stairs – Bitter arguments with wife – Pt denied involuntary mvmnts, gait change, mood disturbance • Family History Case 2 • Mental status: – Normal orientation, speech, memory. – Blunted affect • CN: – Slow saccades • Motor: – Rare, brief, irregular mvments face, neck, trunk – Slightly decreased tone • Reflexes – Normal and symm • Coordination – Normal • Gait – Unsteady tandem Case 2 • On the basis of SSx, which of the four channels through BG are involved? • Which part of BG could lead to this disorder? • What is most likely diagnosis? • What genetic abnormality causes this disorder? • What parts of the brain are predominantly affected? Case 3 • 53M, Rt-handed, 2nd opinion for bradykinesia, tremor, rigidity, unsteady gait • HPI – – – – 10 yrs ago, slowness and difficulty using Rt arm 8 yrs ago shaking of Rt arm and leg Dx PD Sinemet started, beneficial Progressively worse Sx • Tremor of whole body, slower, stiffer, difficulty initiating movements. – Family Hx negative, no antipsychotic meds Case 3 • Mental status – Micrographia • CN – Mask-like facies, hypophonia • Motor – 4Hz tremor U+L/E, Rt > Lt – Cogwheel rigidity – FFM, RAM slow • Reflexes – No extinction of glabellar (+ve Myerson) • Coordinationn – Slow, no ataxia • Gait – Can’t raise from chair w/o assistance – Slow, stiff gait, stooped posture, short steps, decreased arm swing – En bloc turning Case 3 • Idiopathic or atypical parkinsonism? • Degeneration of neurons in which structure 1arily responsible for idiopathic PD? • What is main neurotransmitter? • How does loss of neurons lead to hypokinetic disorder? • If pt has on-off phenomena, what procedures can be recommended? Case 4 • 48 F • HPI – Difficulty type-writing 2ary bilat finger stiffness – Unsteady gait, multiple falls – No benefit with levodopa • Exam 5 yrs after symptom onset – Slow saccades, masked facies, slow dysarthric speech – Prominent bilateral bradykinesia and rigidity of axial and neck muscles – Slow, shuffling gait with retropulsion – No ataxia or autonomic dysfunction Case 4 • Idiopathic vs atypical parkinsonism? • What is most likely diagnosis? • Which neurons degenerate in this condition? Case 4 • Striatonigral degeneration – Loss of DA-ergic neurons in SNpc AND – Degeneration of striatal neurons projecting to GPi and SNpr • Therefore, decreased transmission of DA-ergic stimulation from striatum to GPi/SNpr • the posterior parietal cortex clearly plays a role in voluntary movements, by assessing the context in which they are being made. The parietal cortex receives somatosensory, proprioreceptive, and visual inputs, then uses them to determine such things as the positions of the body and the target in space. It thereby produces internal models of the movement to be made, prior to the involvement of the premotor and motor cortices. Within the posterior parietal cortex, two particular areas are distinguished. Area 5 receives information from somatosensory areas 1, 2, and 3 of the cortex. Area 7 further integrates the already highly integrated signals from the visual areas of the cortex, such as MT and V5. The parietal lobes are themselves closely interconnected with the prefrontal areas, and together these two regions represent the highest level of integration in the motor control hierarchy. It is here that the decisions are made about what action to take. The posterior parietal and prefrontal areas send their axons to Area 6 which, once it has been informed about the kind of action to take, helps to determine the characteristics of the appropriate movement for this purpose. Direct pathway • • • • • From striatum directly to SNpr, GPi Cortex stimulates striatum Striatum inhibits SNpr, GPi Loss of inhibition of thalamus Facilitation of movement via increased thalamic output to motor and premotor cortex Indirect pathway Indirect pathway • Net effect – Increased inhibition of thalamus – Therefore inhibition of movements Some Nomenclature • GPi thalamus output pathway – Ansa lenticularis • Fibers loop ventrally under IC – Lenticular fasciculus • Fibers penetrate straight through IC – Join to form thalamic fasciculus • GPe Subthalamic nucleus and GPi – Subthalamic fasciculus Understanding Movement Disorders • Hemiballismus – Wild flinging movement of extremities – Classically, contralateral subthalamic nucleus lesion – Net result: disinhibition of thalamus • Huntington’s disease – Choreiform movements – Degeneration of striatum • Initially neurons of indirect pathway more affected with resultant inhibition of subthalamic nucleus – Net result: disinhibition of thalamus