* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download glucose
Biochemical cascade wikipedia , lookup
Nicotinamide adenine dinucleotide wikipedia , lookup
Metalloprotein wikipedia , lookup
Cryobiology wikipedia , lookup
Light-dependent reactions wikipedia , lookup
Butyric acid wikipedia , lookup
Biosynthesis wikipedia , lookup
Mitochondrion wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Microbial metabolism wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Lactate dehydrogenase wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Phosphorylation wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Citric acid cycle wikipedia , lookup
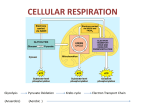
Chapter 3 Carbohydrates 2009 Cengage-Wadsworth • Carbohydrates play a major role in human diets, comprising some 40-75% of energy intake. • Their most important nutritional property is digestibility in the small intestine. • In terms of their physiological or nutritional role, they are often classified as available and unavailable carbohydrates. • Available carbohydrates are those that are hydrolyzed by enzymes of the human gastrointestinal system to monosaccharides that are absorbed in the small intestine and enter the pathways of carbohydrate metabolism. • Unavailable carbohydrates are not hydrolyzed by endogenous human enzymes, although they may be fermented in the large intestine to varying extents. • Carbohydrates are further classified according to their degree of polymerization (DP) as: • sugars (mono- and disaccharides), • oligosaccharides (contain three to nine monosaccharide units), and • polysaccharides (contain ten or more monosaccharide units) Structural Features • Simple carbohydrates – Monosaccharides – Disaccharides • Complex carbohydrates – Oligosaccharides – Polysaccharides 2009 Cengage-Wadsworth Some biologically important monosaccharide 1. Ribose a pentose present in RNA 2. Deoxyribose a pentose present in DNA. 3. Glucose or grape sugar is the main sugar of the blood. 4. Fructose is the sugar of the fruits. 5. Galactose present in milk sugar lactose. 6. Mannose enter in the composition of mucopolysaccharide. Simple Carbohydrates • Disaccharides – Maltose – Lactose – Sucrose 2009 Cengage-Wadsworth Disaccharides • Condensation of 2 monosaccharides forms a disaccharide. • The bond between them is called glycosidic bond. • A disaccharide is reducing when it has free anomeric carbon Disaccharide structure bond Reducing Examples ofsource disaccharides: property Sucrose cane sugar beat sugar table sugar α-D-glucose + β-D-Fructose α-1,2 glycosidic bond. not reducing sugar Lactose milk sugar β-D-galactose + α-Dglucose β-1,4 glycosidic bond Reducing sugar Maltose Malt sugar 2 molecules of α-D-glucose α-1,4 glycosidic bond. Reducing sugar B. The disaccharidases include: 1. Lactase (β-galactosidase) which hydrolyses lactose into two molecules of glucose and galactose: Lactase Lactose Glucose + Galactose 2. Maltase ( α-glucosidase), which hydrolyses maltose into two molecules of glucose: Maltase Maltose Glucose + Glucose 3. Sucrose (α-fructofuranosidase), which hydrolyses sucrose into two molecules of glucose and fructose: Sucrose Sucrose Glucose + Fructose 4. α - dextrinase (oligo-1,6 glucosidase) which hydrolyze (1 ,6) linkage of isomaltose. Dextrinase Isomaltose Glucose + Glucose Complex Carbohydrates • Oligosaccharides – Raffinose – Stachyoses – Verbascose • Polysaccharides – Starch – Glycogen – Cellulose 2009 Cengage-Wadsworth Digestion • Polysaccharides – Salivary -amylase - mouth – Pacreatic -amylase - small intestine – Resistant starches • Digestion of disaccharides – Disaccharidases - active in microvilli of enterocytes 2009 Cengage-Wadsworth Absorption • Absorption is the movement of molecules across the gastrointestinal (GI) tract into the circulatory system. • Most of the end-products of digestion, along with vitamins , minerals, and water, are absorbed in the small intestinal lumen by four mechanisms for absorption: (1) active transport, (2) passive diffusion, (3) endocytosis, and (4) facilitative diffusion. • Active transport requires energy Absorption, Transport, & Distribution • Absorption of glucose & galactose – Into cell: active transport - SGLT1 – Into blood: diffusion, GLUT2 • Absorption of fructose – Into cell: facilitated transport - GLUT5 – Into blood: GLUT2 – Limited in 60% of adults 2009 Cengage-Wadsworth Absorption, Transport, & Distribution • Monosaccharide transport & cellular uptake • Glucose transporters – GLUT isoforms • Integral proteins • Each has specific combining site • Undergoes a conformational change upon binding the molecule • Can reverse this change when unbound 2009 Cengage-Wadsworth Absorption, Transport, & Distribution – Specificity of GLUTs • GLUT1 - basic supply of glucose to cells • GLUT2 - low infinity transporter; glucose from enterocyte to blood • GLUT3 - high-affinity for brain & other glucosedependent tissues • GLUT4 - insulin sensitive, in muscle & adipose tissues • GLUT5 - for fructose 2009 Cengage-Wadsworth Absorption, Transport, & Distribution • Insulin – Role in cellular glucose absorption • Binds to membrane receptor • Stimulates GLUT4 to move to membrane • Maintenance of blood glucose levels 2009 Cengage-Wadsworth Glycemic Response to Carbohydrates • Glycemic index – Increase in blood glucose during 2-hour period after consumption of a certain amount of CHO compared with equal CHO from reference food • Glycemic load – GI x g of CHO in 1 serving of food 2009 Cengage-Wadsworth Introduction to Carbohydrate Metabolism • It is mainly Glucose metabolism which has many anabolic and catabolic pathways: • Major pathway for Glucose oxidation: – Glycolysis – Citric Acid Cycle • Minor Pathways for Glucose oxidation: – HMP (Hexose Monophosphate Pathway) shunt • Glycogenesis • Gluconeogenesis • Conversion to other monosaccharides 2009 Cengage-Wadsworth Dietary Carbohydrate Glucose Fructose Galactose Amino acids Glycerol Lactate Glycogen s si s e si n y e ol og n c e y og Gl c y Gl Gluconeogenesis Gluconeogenesis Other Carbohydrates HMP Pathway Ribose-P Energy Glycolysis Glucose Carbon skeleton of amino acids NADPH Glycerol-P Pyruvate Fatty Acids ATP Acetyl-CoA ADP+Pi Triacylglycerol Electron Transport Chain NADH Kreb's Cycle 2CO2 Major Pathway of Glucose Oxidation • Definition: – Conversion of Glucose to 2pyruvate(or lactate), then to 6CO2 & producing ATPs + reduced nucleotides • Site: – Glycolysis in all cells – Krebs’ Cycle in all cells containing mitochondria Steps: Glucose Anaerobic Phase ( in Cytoplasm ) O2 absent or present t O2 absent 2 Lactic Acid 2 Pyruvic Acid O2 present Aerobic Phase (In mitochondria) O2 present 6 CO2 + H2O I. Glycolysis (Embden Meyerhof Pathway): A. Definition: 1. Glycolysis means oxidation of glucose to give pyruvate (in the presence of oxygen) or lactate (in the absence of oxygen). B. Site: cytoplasm of all tissue cells, but it is of physiological importance in: 1. Tissues with no mitochondria: mature RBCs, cornea and lens. 2. Tissues with few mitochondria: Testis, leucocytes, medulla of the kidney, retina, skin and gastrointestinal tract. 3. Tissues undergo frequent oxygen lack: skeletal muscles especially during exercise. C. Steps: Stages of glycolysis 1. Stage one (the energy requiring stage): a) One molecule of glucose is converted into two molecules of glycerosldhyde-3-phosphate. b) These steps requires 2 molecules of ATP (energy loss) 2. Stage two (the energy producing stage(: a) The 2 molecules of glyceroaldehyde-3-phosphate are converted into pyruvate (aerobic glycolysis) or lactate (anaerobic glycolysis(. b) These steps produce ATP molecules (energy production). D. Energy (ATP) production of glycolysis: ATP production = ATP produced - ATP utilized • In the energy investment phase, ATP provides activation energy by phosphorylating glucose. – This requires 2 ATP per glucose. • In the energy payoff phase, ATP is produced by substrate-level phosphorylation and NAD+ is reduced to NADH. • 2 ATP (net) and 2 NADH are produced per glucose. Fig. 9.8 Energy Investment Phase (steps 1-5) Fig. 9.9a Fig. 9.9b Energy-Payoff Phase (Steps 6-10) Energy production of glycolysis: ATP produced ATP utilized In absence of oxygen (anaerobic glycolysis) 4 ATP (Substrate level phosphorylation) 2ATP from 1,3 DPG. 2ATP from phosphoenol pyruvate 2ATP 2 ATP From glucose to glucose -6-p. From fructose -6-p to fructose 1,6 p. In presence of oxygen (aerobic glycolysis) 4 ATP (substrate level phosphorylation) 2ATP from 1,3 BPG. 2ATP from phosphoenol pyruvate. 2ATP 6 ATP -From glucose to Or glucose -6-p. 8 ATP From fructose -6-p to fructose 1,6 p. + 4ATP or 6ATP (from oxidation of 2 NADH + H in mitochondria). Net energy Differences between aerobic and anaerobic glycolysis: Aerobic Anaerobic 1. End product Pyruvate Lactate 2 .energy 6 or 8 ATP 2 ATP 3. Regeneration of NAD+ Through respiration chain in mitochondria Through Lactate formation 4. Availability to TCA in Available and 2 Pyruvate Not available as lactate mitochondria can oxidize to give 30 is cytoplasmic substrate ATP Biological importance (functions) of glycolysis: 1. Energy production: a) anaerobic glycolysis gives 2 ATP. b) aerobic glycolysis gives 8 ATP. 2. Oxygenation of tissues: Through formation of 2,3 bisphosphoglycerate, which decreases the affinity of Hemoglobin to O2. 3. Provides important intermediates: a) Dihydroxyacetone phosphate: can give glycerol-3phosphate, which is used for synthesis of triacylglycerols and phospholipids (lipogenesis). b) 3 Phosphoglycerate: which can be used for synthesis of amino acid serine. c) Pyruvate: which can be used in synthesis of amino acid alanine. 4. Aerobic glycolysis provides the mitochondria with pyruvate, which gives acetyl CoA Krebs' cycle. Comparison between hexokinase enzymes: glucokinase Glucokinaase and Hexokinase 1. Site Liver only All tissue cells 2. Affinity to glucose Low affinity (high km) i.e. it acts only in the presence of high blood glucose concentration. High affinity (low km) i.e. it acts even in the presence of low blood glucose concentration. 3. Substrate Glucose only Glucose, galactose and fructose 4. Effect of insulin Induces synthesis of glucokinase. No effect 5. Effect of glucose-6-p No effect Allosterically inhibits hexokinase 6. Function Acts in liver after meals. It removes glucose coming in portal circulation, converting it into glucose -6-phosphate. It phosphorylates glucose inside the body cells. This makes glucose concentration more in blood than inside the cells. This leads to continuous supply of glucose for the tissues even in the presence of low blood glucose concentration. Importance of lactate production in anerobic glycolysis: 1. In absence of oxygen, lactate is the end product of glycolysis: Glucose Pyruvate Lactate 2. In absence of oxygen, NADH + H+ is not oxidized by the respiratory chain. 3. The conversion of pyruvate to lactate is the mechanism for regeneration of NAD+. 4. This helps continuity of glycolysis, as the generated NAD+ will be used once more for oxidation of another glucose molecule. • As pyruvate enters the mitochondrion, a multienzyme complex modifies pyruvate to acetyl CoA which enters the Krebs cycle in the matrix. – A carboxyl group is removed as CO2. – A pair of electrons is transferred from the remaining two-carbon fragment to NAD+ to form NADH. – The oxidized fragment, acetate, combines with coenzyme A to form acetyl CoA. Fig. 9.10 Citric acid Cycle (Tricarboxylic Acid Cycle) (Kreb’s Cycle) Definition: Complete oxidation of acetyl-CoA to 2 molecules of CO2 and generating energy either directly as ATP or in the form of reducing equivalents (NADH or FADH2). Location: All cells that contain mitochondria (i.e. not in RBCs) Site: All enzymes are found free in mitochondria matrix except succinate dehydrogenase which is found on the inner border of the inner mitochondrial membrane. The Krebs Cycle • Occurs in the matrix of the mitochondrion • Aerobic phase (requires oxygen) • 2-carbon acetyl CoA joins with a 4-carbon compound to form a 6- carbon compound called Citric acid • Citric acid (6C) is gradually converted back to the 4carbon compound -ready to start the cycle once more • The carbons removed are released as CO2 -enzymes controlling this process called decarboxylases • The hydrogens, which are removed, join with NAD to form NADH2 -enzymes controlling the release of hydrogen are called dehydrogenases Functions of Citric Acid Cycle Amphibolic Function I- Energy production II- Catabolic for glucose, fat &proteins III- Anabolic Function Functions of TCA: I- Energy production Functions of TCA II- Catabolic To carbohydrate, fat & protein: Functions of TCA III- Anabolic Functions Regulation of the citric acid cycle - NADH, ATP, succinyl CoA, citrate Krebs Cycle is a Source of Biosynthetic Precursors Glucose Phosphoenolpyruvate The citric acid cycle provides intermediates for biosyntheses Summary for Complete oxidation of Glucose Complete aerobic oxidation of glucose in glycolysis, citric acid cycle and ETC produces 6 molecules of CO2 + 38 molecules of ATP (38 moles of ATP / one mole of glucose) N.B: Complete oxidation of one glucose molecule in RBC gives 2 ATP + 2 lactate molecules Key Concepts The TCA cycle accounts for more than two thirds of the ATP generated from fuel oxidation. All of the enzymes required for the TCA cycle are in the mitochondria. Acetyl CoA, generated from fuel oxidation, is the substrate for the TCA cycle. Acetyl CoA, when oxidized via the cycle, generates CO2, reduced electron carriers, and GTP. The reduced electron carriers [NADH, FADH2} donate electrons to O2 via the electron-transport chain, which leads to ATP generation from oxidative phosphorylation. The cycle requires a number of cofactors to function properly, some of which are derived from vitamins. These include thiamin pyrophosphate (derived from vitamin B1, thiamin), FAD (derived from vitamin B2, riboflavin), and coenzyme A (derived from pantothenic acid) and NAD (from niacin). Intermediates of the TCA cycle are used for many biosynthetic reactions and are replaced by anaplerotic (refilling) reactions within the cell. The cycle is carefully regulated within the mitochondria by energy and the levels of reduced electron carriers. As energy levels decrease, the rate of the cycle increases. Impaired functioning of the TCA cycle leads to an inability to generate ATP from fuel oxidation and an accumulation of TCA cycle precursors. Minor Pathway for oxidation of glucose • The hexosemonophosphate shunt (pentose phosphate pathway)=pentose shunt=HMP. 2009 Cengage-Wadsworth Pentose Phosphate Pathway Definition: It is a pathway by which pentose phosphate is produced from glucose (with production of two molecules of NADPH), or from other monosaccharides. No ATP is directly consumed or produced in the cycle. Location: Mainly in liver, lactating mammary glands, adipose tissue, adrenal cortex, gonads and RBCs. Site: Cytoplasm Steps: The pentose phosphate pathway occurs in two phases oxidative and nonoxidative I- Oxidative Phase This phase is irreversible; glucose- 6phosphate is converted to ribulose -5phosphate with production of two molecules of NADPH. II- Non-oxidative Phase This phase is reversible. It catalyzes the conversion of pentoses produced in phase one into 2 molecules of Glyceraldehyde-3Phosphate and Fructose-6-Phosphate (By the enzymes transketolase and transaldolase), which continue in the glycolytic pathway. Regulation of HMP The regulated step is glucose-6-P dehydrogenase (G6PD), which is strongly inhibited by NADPH (its product). Importance of Pentose Phosphate Pathway I- It is the ONLY source of ribose-5-phosphate Ribose-5-phosphate forms phosphoribosyl pyrophosphate (PRPP) for synthesis of nucleotides and nucleic acids. In tissues (e.g. muscles) which lack the dehydrogenases of the oxidative phase and in cases of deficiency of G6PD, pentoses are formed by reversal of the non-oxidative phase, starting from fructose-6-P and glyceradehyde-3-P. ll- It is NADPH the main source of required for the reaction of many reductases, hydroxylases and NADPH oxidase. lll – It provides a way for utilizing dietary C4-, C5-, and C7 sugars Regulation of Metabolism • 4 mechanisms: – Negative or positive modulation of allosteric enzymes – Hormonal activation by covalent modification/induction – Directional shifts in reactions – Translocation of enzymes within cells 2009 Cengage-Wadsworth Anabolic Pathway Glycogenesis and glycogenolysis Glycogenesis • Glycogen is a highly branched glucose polymer used for carbohydrate storage in animals • Glycogen stores are used to keep the blood sugar level steady between meals • Glycogenesis is the synthesis of glycogen from glucose-6phosphate - it occurs when high levels of glucose-6-phosphate are formed in the first reaction of glycolysis - it does not operate when glycogen stores are full, which means that additional glucose is converted to body fat Diagram of Glycogenesis • Glucose is converted to glucose-6-phosphate, using one ATP • Glucose-6-phosphate is converted to glucose-1phosphate, which is activated by UTP, forming UTP-glucose • As UTP-glucose attaches to the end of the glycogen chain, UDP is released (and converted to UTP by ATP) Formation of Glucose-6-Phosphate • Glucose is converted to glucose-6-phosphate, using ATP, in the first step of glycolysis P O CH2 O OH OH OH OH Glucose-6-phosphate Formation of Glucose-1-Phosphate • Glucose-6-phosphate is converted to glucose-1-phosphate P O CH2 H O CH2 O O OH OH OH OH OH Glucose-6-phosphate O P OH OH Glucose-1-phosphate Formation of UTP-Glucose • UTP activates glucose-1-phosphate to form UDP-glucose and pyrophosphate (PPi) O CH2OH H O OH O O P O OH OH O- O O P O CH2 O- N N O UDP-glucose OH OH Glycogenolysis • Glycogenolysis is the breakdown of glycogen to glucose • The glucose is phosphorylated as it is cleaved from the glycogen to form glucose-1-phosphate • Glucose-1-phosphate can be converted to glucose-6phosphate, which can enter glycolysis • Phosphorylated glucose can’t be absorbed into cells - in the liver and kidneys, glucose-6-phosphate can be hydrolized to glucose • Glycogenolysis is activated by glucogon in the liver and epinephrine in muscles - these are produced when blood glucose levels are low • Glycogenolysis is inhibited by insulin - insulin is produced when blood glucose levels are high Overview of Glycogen Synthesis and Breakdown Gluconeogenesis (Glucose Synthesis) • Glucose is the primary energy source for the brain, skeletal muscle, and red blood cells • Deficiency can impair the brain function • Gluconeogenesis is the synthesis of glucose from carbon atoms of noncarbohydrates - required when glycogen stores are depleted GLUCONEOGENESIS • Definition: – It is synthesis of glucose from noncarbohydrate sources. Its main function is to supply blood glucose in case of carbohydrate deficiency (fasting more than 10-18 hours). • Location: – It occurs mainly in the liver cells and to lesser extent in kidneys • Site: – Cytoplasm except for the first step (carboxylation of pyruvate) occurs in the mitochondria. Substrates for Gluconeogenesis (Gluconeogenic Precursors) These are molecules that can be used to produce glucose. They give directly or indirectly pyruvate, oxaloacetate or any intermediates of glycolysis or citric acid cycle. 1- Glucogenic Amino Acids 2- Glycerol 3- Lactate Substrates for Gluconeogenesis (Gluconeogenic Precursors) • 1- Glucogenic Amino Acids These are amino acids which are convertible to glucose. They give pyruvate or oxaloacetate directly or indirectly by giving intermediates of citric acid cycle • 2- Glycerol Glycerol released from hydrolysis of TAG in adipose tissue, go to the liver via blood. In the liver the following will occur: NB. Adipose tissue has NO glycerol kinase Substrates for Gluconeogenesis (Gluconeogenic Precursors) • 3- Lactate It is produced by red blood cells and by contracting muscles, then passes to the liver where it is converted to glucose which is released back into the circulation. (Cori’s Cycle) Importance of Gluconeogenesis 1- Maintenance of blood glucose: The main function of gluconeogenesis is the maintenance of blood glucose when carbohydrates are not available in sufficient amounts e.g. fasting, starvation, stress, prolonged exercise and dietary carbohydrate deficiency for more than 10 – 18 hours. 2- Removal of lactic acid produced by red cells and contracting muscles. 3- Removal of glycerol produced by lipolysis in adipose tissues. A common intermediate in the conversion of glycerol and lactate is which of the following? a. Pyruvate b.Oxaloacetate c. Malate d. Glucose 6-phosphate e. Phosphoenolpyruvate Cori and Alanine Cycles Cori cycle prevents loss of lactate as waste product in urine, and prevent its accumulation in blood (acidosis) Both help to maintain blood glucose level specially to tissues that dependant on it as their primary source of energy. Both supply RBCs and contracting muscles with glucose for reutilization and ATP production. Both spare energy in red cells and contracting muscles. Cori Cycle Anaerobic Glucose Glucose 2 NAD+ Glycolysis Gluconeogensis Glucose 6 ATP Urea Urea 2 NADH+H+ 2 ATP ETC 2 Pyruvate 2 Pyruvate 4ATP 4 0r 6 ATP Kidney 2 NH3 transamination transamination deamination 2 Alanine 2 Alanine Liver 2 Alanine Mucsle Cell Alanine Cycle In Alanine Cycle O2 and mitochondria are required in the peripheral tissues REGULATION OF GLUCONEOGENESIS The gluconeogenic regulatory key enzymes are those which reverse the glycolytic key enzymes. • Glycolysis and gluconeogenesis reciprocally controlled. are Factors which increase gluconeogenesis I- Availability of substrates: Availability of gluconeogenic substrates specially glucogenic amino acids provide increased amounts of oxaloacetic acid. Excess ATP (from FA oxidation) produces allosteric inhibition of phosphofructokinase-1 and pyruvate kinase (glycolysis) and activate F1,6-BPase (gluconeogenesis). Excess acetyl-CoA, (from FA oxidation), allosterically stimulates pyruvate carboxylase enzyme and inhibits pyruvate dehydrogenase, thus directs pyruvate to gluconeogenesis. Cori Cycle • When anaerobic conditions occur in active muscle, glycolysis produces lactate • The lactate moves through the blood stream to the liver, where it is oxidized back to pyruvate. • Gluconeogenesis converts pyruvate to glucose, which is carried back to the muscles • The Cori cycle is the flow of lactate and glucose between the muscles and the liver Cori Cycle Anaerobic Cori and Alanine Cycles Cori cycle prevents loss of lactate as waste product in urine, and prevent its accumulation in blood (acidosis) Both help to maintain blood glucose level specially to tissues that dependant on it as their primary source of energy. Both supply RBCs and contracting muscles with glucose for reutilization and ATP production. Both spare energy in red cells and contracting muscles. Pathways for Glucose Regulation of Glycolisis and Gluconeogenesis • High glucose levels and insulin promote glycolysis • Low glucose levels and glucagon promote gluconeogenesis Hypoglycemia • Preprandial vs. postprandial serum glucose levels • Types: – Fasting hypoglycemia • Usually caused by insulin, sulfonylureas – Fed (reactive) hypoglycemia • Impaired glucose tolerance, idiopathic postprandial syndrome 2009 Cengage-Wadsworth