* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The neuronal ceroid lipofuscinoses: the same, but different?
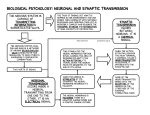
Neuroinformatics wikipedia , lookup
National Institute of Neurological Disorders and Stroke wikipedia , lookup
Single-unit recording wikipedia , lookup
Neural modeling fields wikipedia , lookup
Nonsynaptic plasticity wikipedia , lookup
Synaptic gating wikipedia , lookup
Alzheimer's disease wikipedia , lookup
Channelrhodopsin wikipedia , lookup
Optogenetics wikipedia , lookup
Aging brain wikipedia , lookup
Neuroanatomy wikipedia , lookup
Activity-dependent plasticity wikipedia , lookup
Holonomic brain theory wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Haemodynamic response wikipedia , lookup
Biological neuron model wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Nervous system network models wikipedia , lookup
Biochemistry of Alzheimer's disease wikipedia , lookup
1448 Biochemical Society Transactions (2010) Volume 38, part 6 The neuronal ceroid lipofuscinoses: the same, but different? Jonathan D. Cooper1 Pediatric Storage Disorders Laboratory, Department of Neuroscience and Centre for the Cellular Basis of Behaviour, James Black Centre, Institute of Psychiatry, King’s College London, 125 Coldharbour Lane, London SE5 9NU, U.K. Biochemical Society Transactions www.biochemsoctrans.org Abstract The NCLs (neuronal ceroid lipofuscinoses) (also known as Batten disease) are a group of at least ten fatal inherited storage disorders. Despite the identification of many of the disease-causing genes, very little is known about the underlying disease mechanisms. However, now that we have mouse or large-animal models for most forms of NCL, we can investigate pathogenesis and compare what happens in the brain in different types of the disease. Broadly similar neuropathological themes have emerged, including the highly selective nature of neuron loss, early effects upon the presynaptic compartment, together with an early and localized glial activation. These events are especially pronounced within the thalamocortical system, but it is clear that where and when they occur varies markedly between different forms of NCL. It is now becoming apparent that, despite having pathological endpoints that resemble one another, these are reached by a sequence of events that is specific to each subtype of NCL. Introduction LSDs (lysosomal storage disorders) broadly share several common features. Each is caused by a single gene defect that results in lysosomal dysfunction, resulting in the intralysosomal accumulation of material that would normally be degraded [1,2]. The end result is a devastating impact upon the affected individual, their families and those that care for them. However, this superficially similar picture masks a great deal of heterogeneity, both in terms of the underlying gene defect and material stored, and also in the clinical presentation of affected individuals [1,2]. This heterogeneity represents a considerable challenge in terms of understanding the pathogenesis of these disorders and trying to devise effective therapies, and highlights the importance of carefully investigating each disorder individually. It also raises a more general concern about how to classify disorders that are broadly similar, but display marked differences between individual subtypes. What’s in a name? There are several different ways to classify LSDs, according to the type of material stored, age of onset and whether the disease-causing gene codes for a soluble lysosomal enzyme or a transmembrane protein [1]. Uncomfortably straddling all of these classification schemes sit the NCLs (neuronal ceroid lipofuscinoses), a group of at least ten storage disorders that are more commonly known as Batten disease [3,4]. Although Key words: Batten disease, lysosomal dysfunction, lysosomal storage disorder (LSD) neuroimmune response, neuronal ceroid lipofuscinosis (NCL), selective neuron vulnerability. Abbreviations used: LSD, lysosomal storage disorder; NCL, neuronal ceroid lipofuscinosis. 1 email [email protected] C The C 2010 Biochemical Society Authors Journal compilation individually rare, these disorders are collectively the single largest cause of childhood neurological impairment in the U.K. [5,6]. Once considered a form of ‘amaurotic familial idiocy’, the term NCL was coined in the 1960s [7], initially to distinguish these profoundly neurodegenerative disorders from Tay–Sachs disease. This was largely on the basis that all forms of NCL display the distinctive intralysosomal accumulation of autofluorescent lipopigments [3,8], not only in the brain, but also throughout the body. Characteristically, the NCLs also share a number of other features, including visual failure leading to blindness, seizures of increasing severity and a relentless decline in cognitive and motor ability, invariably ending in a premature death [3,8]. However, this may present at widely different ages ranging from shortly after birth to early middle age. It’s all in the genes Originally, it was thought that there were just four different types of NCL, each caused by a mutation in a single gene, with infantile-, late-infantile- and juvenile-onset forms and a rarer adult-onset subtype proposed. However, the advent of molecular genetics has revealed that at least ten genetically distinct forms of NCL exist, with several new disease-causing ‘CLN’ genes identified in recent years [9,10]. (This ‘CLN’ nomenclature is another potential source of confusion, rather than the more logical choice ‘NCL’, but this was already assigned to another group of completely unrelated genes.) Many of these mutations result in additional variant forms of late-infantile NCL, but a congenital form has also recently been found [11]. There is a certain degree of phenotype– genotype correlation in some forms of NCL, but this does Biochem. Soc. Trans. (2010) 38, 1448–1452; doi:10.1042/BST0381448 Lysosomes in Health and Disease not hold true for all of these disorders, with many different mutations in an individual gene producing apparently similar clinical presentations [8,9]. Identifying the genetic basis of eight of the postulated forms of NCL has revealed multiple levels of complexity. Not only do these genes code for distinctly different types of protein [3,10,12], soluble (CLN1, CLN2, CLN10 and probably CLN5) compared with transmembrane protein (CLN3, CLN6, CLN7 and CLN8), but also not all of them are expressed within the lysosome, with the remainder expressed elsewhere within the endosomal–lysosomal system (e.g. CLN6 and CLN8 in the endoplasmic reticulum). Even this issue of intracellular location has been difficult to resolve, with a lack of sufficiently specific antisera available against highly hydrophobic transmembrane proteins such as CLN3. Similarly, very little is known about how mutations in these different genes lead to such devastating effects upon the brain [13,14], with apparently relatively few consequences in the rest of the body. Nor is it clear how genes that code for proteins of such radically different nature and that are expressed at different intracellular sites might produce neurological disorders that resemble one another. The model answer Examining post-mortem material from individuals with different forms of NCL provides the first hints that these disorders do not resemble one another as closely as might be thought [14,15]. Even at the disease end stage, it is apparent that not all brain regions or cell types are affected equally in any given type of NCL and, perhaps unsurprisingly, that these phenotypes vary between different forms of the disease. For example, there are pronounced differences between the extent of neuron loss between different hippocampal subfields [15] and cortical regions [16], with accompanying differences in the extent of glial activation. Although informative, the main drawback of these post-mortem studies is that they provide a static snapshot of the disease endpoint and cannot reveal anything of the events leading to this conclusion. Fortunately, revealing the genes defective in most forms of NCL has also made it possible to generate a series of genetically modified mouse models and to identify spontaneously occurring mutants which bear mutations in these genes [17]. In addition to mice, these models include a diverse series of large-animal species [18], with dog and sheep models the best characterized and most widely used. The larger and more complex brain of these species has particular advantages for modelling human disease and for addressing the translation of experimental therapies into a clinical setting. Nevertheless, as for many other diseases, the mainstay of our research remains mouse models of NCL [17], with at least one available for each genetically identified form of NCL, the exception being the most recently identified CLN7 [19]. These include both knockout mice, in which the function of the diseasecausing gene has been disrupted, and knockin mice, in which a particular disease-causing mutation has been introduced into this gene [17]. What do we know about NCL pathogenesis so far? Over the last decade, we have been characterizing each of the available mouse models of NCL, documenting the onset and progression of pathological changes [20–34] and testing the efficacy of a range of therapeutic interventions [35–38]. Our studies have revealed a number of new and surprising pathological features that are broadly shared by the different forms of NCL, but with subtype-specific differences in the staging of these events and some more pronounced differences between certain forms of NCL. Selective neuron loss in the NCLs At the outset of our studies, it was assumed that neuron loss occurred to very similar extents throughout the NCL brain. Although the loss of neurons is indeed widespread at the end stages of disease, there is remarkable selectivity in its earlier stages with populations of GABAergic interneurons, thalamocortical projection neurons and cerebellar Purkinje neurons proving especially vulnerable [4,17]. The vulnerability of interneuron populations might be predicted, given that seizures are a prominent feature of these disorders, but it remains to be seen whether these events are related to one another. More unexpected, given the profound degeneration of the cortical mantle, was the discovery that neuron loss within the thalamocortical system consistently starts in the thalamus in the vast majority of NCL mouse models [25– 27,30]. Even more surprising has been the observation that this sequence of neuron loss is completely reversed in at least one form of NCL [33], starting instead within the cortex. Clearly, even within one defined set of pathways, the impact of mutations in these disease-causing genes may have radically different consequences. A key consideration is whether these phenotypes observed in mice are also present in a more complex CNS (central nervous system), most importantly in the human disease. In this respect, large animal models of NCL are particularly informative [18], as we can examine the onset and progression of the same neuropathological features we have seen in mice. Making such comparisons between mice and sheep that model the same form of NCL [17,39,40] reveals that, although similar phenotypes are evident, they are much more severe in sheep and in the corresponding human disease. This may just reflect the inherent complexity of these larger brains compared with mice. However, another plausible explanation for such species-specific effects is that gene defects in the endosomal–lysosomal system impair intracellular trafficking and/or anterograde transport within neurons. This has already been reported in murine NCL [29] and would be expected to have greater effects in a larger and more complex brain, in which the distances for transport are much greater, and the precise requirements for accurate trafficking are more demanding. The challenge lies in determining why such specific effects upon neuron survival should exist, and certainly this is at odds with the ubiquitous accumulation of storage material C The C 2010 Biochemical Society Authors Journal compilation 1449 1450 Biochemical Society Transactions (2010) Volume 38, part 6 within the NCL brain. As new data become available for the regional and cellular expression of genes within these pathways [34], a clearer picture of the underlying mechanisms will undoubtedly emerge. Until this happens, another fruitful approach has been to determine the other pathological events that precede neuron loss. Trouble in store? The ubiquitous and characteristic build up of storage material that occurs in the NCLs has traditionally been thought to be central to its pathogenesis and may even be toxic to neurons. Easily detected via UV illumination and with a subtype-specific ultrastructural appearance, it is not difficult to see why much attention has been focused upon this phenotype. However, more recent evidence suggests that there is no direct relationship between neuron loss and storage material accumulation [4,17]. Certainly, there is no correlation between the regional and temporal patterns of these events in any form of NCL. It is also possible to pharmacologically induce this type of storage material accumulation with no effects on neuron survival [41] and to significantly decrease the storage burden with no appreciable effect on neuron survival or lifespan [36]. If the accumulation of storage material is not the decisive event that leads to neuron loss, then what might be? Without a clear understanding of the normal function of any of the ‘CLN’ gene products, it has been difficult to determine the underlying disease mechanisms. As with other disorders, a whole variety of different possibilities have been suggested across the different forms of NCL, including, among others, an autoimmune response, oxidative stress or mitochondrial dysfunction [3,4,17]. Many of these are likely to be secondary events and determining which are central to pathogenesis is a significant challenge. Pathways to neuron loss? We have started investigating these issues and identified glial activation and synaptic pathology as two key events that happen early in the pathogenesis of all forms of NCL and accurately predict the distribution of subsequent neuron loss. The same regions and pathways that exhibit neuron vulnerability display anterograde transport defects [29], an early rearrangement of the presynaptic compartment, altered SNAP (soluble N-ethylmaleimide-sensitive fusion proteinattachment protein)/SNARE (soluble N-ethylmaleimidesensitive fusion protein-attachment protein receptor) formation and synapse elimination before the onset of neuron loss [30,34,42]. As in other LSDs, several lines of evidence point to important roles for both astrocytes and microglia in the early stages of disease progression, although the precise nature and timing of these events vary markedly between different forms of NCL [4,17]. Neuron loss in all forms of NCL is invariably preceded by localized glial activation of one type or another [24,25,27,30,31,33,39], and this process starts much earlier C The C 2010 Biochemical Society Authors Journal compilation than previously suspected, already being evident prenatally in sheep models of NCL [43]. There is also evidence for a direct relationship between the extent of astrocytosis, microglial activation and neuron loss in human NCL post-mortem material [15,32,37]. We have begun exploring this relationship in more detail and have obtained preliminary evidence that the biology of astrocytes and microglia may be compromised in certain forms of NCL. The activation of astrocytes and microglia appear to be attenuated in human [15] and murine [24,25] juvenile NCL, phenotypes that we are exploring in primary microglial or astrocyte cultures. Concluding comments Until recently, it was assumed that neurons were the main pathological target in the NCLs, with widespread and global neurodegeneration at the later stages of disease. However, evidence that glial cells may themselves be affected in these disorders raises the likelihood of non-cell-autonomous effects in these disorders. Indeed, astrocytes and microglia have the potential to be key players in the pathogenesis of multiple forms of NCL, with the synapse as the prime site where these cell types all converge and interact with one another. The immediate challenge is now to identify the precise contribution of these different cell types to disease progression and how their interactions ultimately lead to neuron loss. Whatever the underlying mechanisms, it is becoming apparent that there are significant differences between the pathological profiles of different forms of NCL. This is not especially surprising given the different types of proteins that are deficient in these disorders and raises the distinct possibility that these subtypes of NCL are far less similar than was once assumed. Perhaps more remarkable is that defects in such widely differing gene products converge to produce pathological endpoints so similar that they have been considered a closely related group of disorders. Funding The studies from the Pediatric Storage Disorders Laboratory cited in this review are the result of a wide series of collaborations and were funded by grants to J.D.C. and collaborators from the U.S. National Institutes of Health [grant numbers NS40297, NS41930, NS043105 and NS044310]; The Wellcome Trust [grant numbers GR079491MA and WT084151AIA and Biomedical Research Collaboration Grant 023360); European Commission 6th Framework Programme [grant number LSHM-CT-2003-503051]; Royal College of Paediatrics and Child Health (WellChild) Fellowship; The Batten Disease Support and Research Association; The Batten Disease Family Association; NCL Stiftung; The Natalie Fund and Ph.D. studentships from the U.K. Medical Research Council. References 1 Platt, F.M. and Walkley, S.U. (2004) Lysosomal defects and storage. In Lysosomal Disorders of the Brain (Platt, F.M. and Walkley, S.U., eds), pp.32–49, Oxford University Press, Oxford Lysosomes in Health and Disease 2 Vellodi, A. (2005) Lysosomal storage disorders. Br. J. Haematol. 128, 413–431 3 Jalanko, A. and Braulke, T. (2009) Neuronal ceroid lipofuscinoses. Biochim. Biophys. Acta 1793, 697–709 4 Cooper, J.D. (2010) Neuronal ceroid lipofuscinosis. In Encyclopedia of Movement Disorders, vol. 2 (Kompoliti, K. and Verhagen Metman, L., eds), pp. 291–295, Academic Press, Oxford 5 Devereux, G., Stellitano, L., Verity, C.M., Nicoll, A., Will, R.G. and Rogers, P. (2004) Variations in neurodegenerative disease across the UK: findings from the national study of Progressive Intellectual and Neurological Deterioration (PIND). Arch. Dis. Child. 89, 8–12 6 Verity, C., Winstone, A.M., Stellitano, L., Will, R. and Nicoll, A. (2009) The epidemiology of progressive intellectual and neurological deterioration in childhood. Arch. Dis. Child. 95, 361–364 7 Zeman, W. and Dyken, P. (1969) Neuronal ceroid-lipofuscinosis (Batten’s disease): relationship to amaurotic family idiocy? Pediatrics 44, 570–583 8 Mole, S.E., Williams, R.E. and Goebel, H.H. (2005) Correlations between genotype, ultrastructural morphology and clinical phenotype in the neuronal ceroid lipofuscinoses. Neurogenetics 6, 107–126 9 Siintola, E., Lehesjoki, A.E. and Mole, S.E. (2006) Molecular genetics of the NCLs: status and perspectives. Biochim. Biophys. Acta 1762, 857–864 10 Getty, A.L. and Pearce, D.A. (2010) Interactions of the proteins of neuronal ceroid lipofuscinosis: clues to function. Cell. Mol. Life Sci., doi:10.1007/s00018-010-0468-6 11 Siintola, E., Partanen, S., Strömme, P., Haapanen, A., Haltia, M., Maehlen, J., Lehesjoki, A.E. and Tyynelä, J. (2006) Cathepsin D deficiency underlies congenital human neuronal ceroid-lipofuscinosis. Brain 129, 1438–1445 12 Kyttälä, A., Lahtinen, U., Braulke, T. and Hofmann, S.L. (2006) Functional biology of the neuronal ceroid lipofuscinoses (NCL) proteins. Biochim. Biophys. Acta 1762, 920–933 13 Cooper, J.D. (2003) Progress towards understanding the neurobiology of Batten disease or neuronal ceroid lipofuscinosis. Curr. Opin. Neurol. 16, 121–128 14 Haltia, M. (2003) The neuronal ceroid-lipofuscinoses. J. Neuropathol. Exp. Neurol. 62, 1–13 15 Tyynelä, J., Cooper, J.D., Khan, M.N., Shemilt, S.J.A. and Haltia, M. (2004) Specific patterns of storage deposition, neurodegeneration, and glial activation in the hippocampus of patients with neuronal ceroid-lipofuscinoses. Brain Pathol. 14, 349–357 16 Hachiya, Y., Hayashi, M., Kumada, S., Uchiyama, A., Tsuchiya, K. and Kurata, K. (2006) Mechanisms of neurodegeneration in neuronal ceroid-lipofuscinoses. Acta Neuropathol. 111, 168–177 17 Cooper, J.D., Russell, C.R. and Mitchison, H.M. (2006) Progress towards understanding disease mechanisms in small vertebrate models of neuronal ceroid lipofuscinosis. Biochim. Biophys. Acta 1762, 873–889 18 Tammen, I., Houweling, P.J., Frugier, T., Mitchell, N.L., Kay, G.W., Cavanagh, J.A., Cook, R.W., Raadsma, H.W. and Palmer, D.N. (2006) A missense mutation (c.184C>T) in ovine CLN6 causes neuronal ceroid lipofuscinosis in Merino sheep whereas affected South Hampshire sheep have reduced levels of CLN6 mRNA. Biochim. Biophys. Acta 1762, 898–905 19 Siintola, E., Topcu, M., Aula, N., Lohi, H., Minassian, B.A., Paterson, A.D., Liu, X.Q., Wilson, C., Lahtinen, U., Anttonen, A.K. and Lehesjoki, A.E. (2006) The novel neuronal ceroid lipofuscinosis gene MFSD8 encodes a putative lysosomal transporter. Am. J. Hum. Genet. 81, 136–146 20 Cooper, J.D., Messer, A., Feng, A.K., Chua-Couzens, J. and Mobley, W.C. (1999) Apparent loss and hypertrophy of interneurons in a mouse model of neuronal ceroid lipofuscinosis: evidence for partial response to insulin-like growth factor-1 treatment. J. Neurosci. 19, 2556–2567 21 Mitchison, H.M., Bernard, D.J., Greene, N.D.E., Cooper, J.D., Junaid, M.A., Pullarkat, R.K., Vos, N., Breuning, M.H, Owens, J.W., Mobley, W.C. et al. (1999) Targeted disruption of the Cln3 gene provides a mouse model for Batten disease. Neurobiol. Dis. 6, 321–334 22 Chattopadhyay, S., Ito, M., Cooper, J.D., Brooks, A.I., Curran, T.M., Powers, J.M. and Pearce, D.A. (2002) An autoantibody inhibitory to glutamic acid decarboxylase in the neurodegenerative disorder Batten disease. Hum. Mol. Genet. 11, 1421–1431 23 Bible, E., Gupta, P., Hofmann, S.L. and Cooper, J.D. (2004) Regional and cellular neuropathology in the palmitoyl protein thioesterase-1 (PPT1) null mutant mouse model of infantile neuronal ceroid lipofuscinosis. Neurobiol. Dis. 16, 346–359 24 Pontikis, C.C., Cella, C.V., Parihar, N., Lim, M.J., Chakrabarti, S., Mitchison, H.M., Mobley, W.C., Rezaie, P., Pearce, D.A. and Cooper, J.D. (2004) Late onset neurodegeneration in the Cln3 − / − mouse model of juvenile neuronal ceroid lipofuscinosis is preceded by low level glial activation. Brain Res. 1023, 231–242 25 Pontikis, C.C., Cotman, S.L., MacDonald, M.E. and Cooper, J.D. (2005) Thalamocortical neuron loss and localized astrocytosis in the Cln3ex7/8 knock-in mouse model of Batten disease. Neurobiol. Dis. 20, 823–836 26 Weimer, J.M., Custer, A.W., Benedict, J.W., Alexander, N.A., Kingsley, E., Federoff, H.J., Cooper, J.D. and Pearce, D.A. (2006) Visual deficits in a mouse model of Batten disease are the result of optic nerve degeneration and loss of dorsal lateral geniculate thalamic neurons. Neurobiol. Dis. 22, 284–293 27 Kielar, C., Maddox, L., Bible, E., Pontikis, C.C., Macauley, S.L., Griffey, M.A., Wong, M., Sands, M.S. and Cooper, J.D. (2007) Successive neuron loss in the thalamus and cortex in a mouse model of infantile neuronal ceroid lipofuscinosis. Neurobiol. Dis. 25, 150–162 28 Lim, M.J., Alexander, N., Benedict, J.W., Chattopadhyay, S., Shemilt, S.J.A., Guérin, C.J., Cooper, J.D. and Pearce, D.A. (2007) IgG entry and deposition are components of the neuroimmune response in Batten disease. Neurobiol. Dis. 25, 239–251 29 Weimer, J.M., Elshatory, Y.M., Short, D.W., Ramirez-Montealegre, D., Benedict, J.W., Ryan, D.A., Alexander, N.A., Federoff, H.J., Cooper, J.D. and Pearce, D.A. (2007) Alterations in striatal dopamine catabolism precede loss of substantia nigra neurons in a mouse model of juvenile neuronal ceroid lipofuscinosis. Brain Res. 1162, 98–112 30 Partanen, S., Haapanen, A., Kielar, C., Pontikis, C.C, Alexander, N.A., Inkinen, T., Saftig, P., Gillingwater, T.H., Cooper, J.D. and Tyynelä, J. (2008) Synaptic changes in the thalamocortical system of cathepsin D deficient mice, a model of human congenital neuronal ceroid-lipofuscinosis. J. Neuropathol. Exp. Neurol. 67, 16–29 31 Macauley, S.L., Wozniak, D.F., Kielar, C., Tan, Y., Cooper, J.D. and Sands, M.S. (2009) Cerebellar pathology and motor deficits in the palmitoyl protein thioesterase 1-deficient mouse. Exp. Neurol. 217, 124–135 32 Weimer, J.M., Benedict, J.W., Getty, A.L., Pontikis, C.C., Lim, M.J., Cooper, J.D. and Pearce, D.A. (2009) Cerebellar defects in a mouse model of juvenile neuronal ceroid lipofuscinosis. Brain Res. 1266, 93–107 33 von Schantz, C., Kielar, C., Hansen, S.N., Pontikis, C.C., Alexander, N.A., Kopra, O., Jalanko, A. and Cooper, J.D. (2009) Progressive thalamocortical neuron loss in Cln5 deficient mice: distinct effects in Finnish variant late infantile NCL. Neurobiol. Dis. 34, 308–319 34 Kielar, C., Wishart, T.M., Palmer, A., Dihanich, S., Wong, A.M., Macauley, S.L., Chan, C.H., Sands, M.S., Pearce, D.A., Cooper, J.D. and Gillingwater, T.H. (2009) Molecular correlates of axonal and synaptic pathology in mouse models of Batten disease. Hum. Mol. Genet. 18, 4066–4080 35 Griffey, M., Bible, E., Vogler, C., Levy, B., Gupta, P., Cooper, J.D. and Sands, M.S. (2004) Adeno-associated virus 2-mediated gene therapy decreases autofluorescent storage material and increases brain mass in a murine model of infantile neuronal ceroid lipofuscinosis (INCL). Neurobiol. Dis. 16, 360–369 36 Griffey, M.A., Wozniak, D., Wong, M., Bible, E., Johnson, K., Rothman, M.R., Wentz, A.E., Cooper, J.D. and Sands, M.S. (2006) CNS-directed AAV2-mediated gene therapy ameliorates functional deficits in a murine model of infantile neuronal ceroid lipofuscinosis. Mol. Ther. 15, 538–547 37 Chang, M., Cooper, J.D., Sleat, D.E., Cheng, S.H., Dodge, J.C., Passini, M.A., Lobel, P. and Davidson, B.L. (2008) Intraventricular enzyme replacement improves disease phenotypes in a mouse model of late infantile neuronal ceroid lipofuscinosis. Mol. Ther. 16, 649–656 38 Tamaki, S.J., Jacobs, Y., Dohse, M., Capela, A., Cooper, J.D., Reitsma, M., He, D., Tushinski, R., Belichenko, P.V., Salehi, A. et al. (2009) Neuroprotection of host cells by human central nervous system stem cells in a mouse model of infantile neuronal ceroid lipofuscinosis. Cell Stem Cell 5, 310–319 39 Oswald, M.J., Palmer, D.N., Kay, G.W., Shemilt, S.J.A., Rezaie, P. and Cooper, J.D. (2005) Glial activation spreads from specific cerebral foci and precedes neurodegeneration in presymptomatic ovine neuronal ceroid lipofuscinosis (CLN6). Neurobiol. Dis. 20, 49–63 40 Oswald, M.J., Palmer, D.N., Kay, G.W., Barwell, K.J. and Cooper, J.D. (2008) Location and connectivity determine GABAergic interneuron survival in the brains of South Hampshire sheep with CLN6 neuronal ceroid lipofuscinosis. Neurobiol. Dis. 32, 50–65 C The C 2010 Biochemical Society Authors Journal compilation 1451 1452 Biochemical Society Transactions (2010) Volume 38, part 6 41 Ivy, G.O., Schottler, F., Wenzel, J., Baudry, M. and Lynch, G. (1984) Inhibitors of lysosomal enzymes: accumulation of lipofuscin-like dense bodies in the brain. Science 226, 985–987 42 Kim, S.J., Zhang, Z., Sarkar, C., Tsai, P.C., Lee, Y.C., Dye, L. and Mukherjee, A.B. (2008) Palmitoyl protein thioesterase-1 deficiency impairs synaptic vesicle recycling at nerve terminals, contributing to neuropathology in humans and mice. J. Clin. Invest. 118, 3075–3086 C The C 2010 Biochemical Society Authors Journal compilation 43 Kay, G.W., Palmer, D.N., Rezaie, P. and Cooper, J.D. (2006) Prenatal activation of non-neuronal cells within the developing CNS of sheep with neuronal ceroid lipofuscinosis (CLN6). Brain Pathol. 16, 110–116 Received 30 August 2010 doi:10.1042/BST0381448