* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 9th seminar Adaptive immunity
Endomembrane system wikipedia , lookup
Tissue engineering wikipedia , lookup
Signal transduction wikipedia , lookup
Extracellular matrix wikipedia , lookup
Programmed cell death wikipedia , lookup
Cell encapsulation wikipedia , lookup
Cell growth wikipedia , lookup
Cytokinesis wikipedia , lookup
Cell culture wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
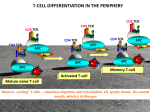
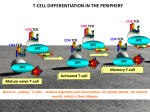
B and T cell functions ADAPTIVE IMMUNITY Humoral immunity/ Antibody-mediated immunity (B cells) 1: processing of a pathogen by an antigen presenting cell and presentation of it on class II MHC molecules to an antigen-specific helper T cell activates the helper T cell to produce cytokines IL-2, IL-4 and IL-5. These cytokines activate a B cell having that same antigen-specific receptor to produce antibodies against that particular antigen. 2. An alternative pathway of B cell activation is the T-independent way, involving no helper T cells and thus no IL-4 and IL-5. It requires receptor aggregation or a strong cross linking of BCR with other PRRs. Cell-mediated immunity (T cells) 1: A bacrteria taken up by a macrophage, degraded and is presented on class II major histocompatibility complex proteins (MHC II) that interacts with the specific antigen-specific receptor on a helper T cell, this activates the T cell to proliferate and produce cytokines (IL-2, IFN-γ). 2: A virus infects cells of the respiratory tract, a viral particle is presented on class I MHC proteins and recognized by an antigen-specific receptor on a cytotoxic T cell it then proliferates with the help of IL-2 from helper T cells, and specifically kill the virus infected cells. Humoral Immunity Cell-Mediated Immunity Microbe Extracellular bacteria Processed by an APC Extracellular microbes phagocytosed in a macrophage Intracellular microbes replicating in infected cells Responding lymphocyte B lymphocytes T lymphocytes T lymphocytes Cell Interactions Cytokine secretion T-dependent: APC MHC IITCR and IL-10 production. Naïve CD4+ T cell Th2 cells secreting IL-2, IL-4 and IL-5 B cell Plasma cell APC MHC II-TCR and IL12 production. Naïve CD4+ T cell Th1 cells secreting IL-2 and IFNγ macrophage activation APC or virus infected cell presents Ag on MHC I to TCR. Naïve CD8+ T cell CTL (cytotoxic T lymphocyte) Activation of macrophages- microbial killing Lytic granules (containing granzymes and perforin) and FasL expressionLysis of infected cells *T-independent: BCR aggregation or cross linking Effector mechanism Secreted antibodieselimination of bacteria T cell migration and activation T cell activation can be induced by antigens in the presence of accessory cellsthe APCs (not by a soluble antigen) or viral antigens on an infected cell Naïve T cells first encounter antigens presented by DCs in the SLO A. Naïve T cells entry from blood to lymph nodes via high endothelial vanules (HEV) is dependent on adhesion molecules and CCR7. Encounter with an Ag presenting DC coming from the afferent lymphatics will increase the chemokine receptor expression on the effector T cells. B. this will guide them to enter the inflamed tissue from the blood. THE IMMUNOLOGICAL SYNAPSE APC T Second signals triggered by co-receptors are required for T-cell activation Th Th Th CD40L CD28 CD40 B7 B7 ACTIVATION Phases of T cell response Effector T cells The three types of effector T cell produce distinct sets of effector molecules Naïve T-cells differentiate into various effector cell types Key step in Th1 differentiation is the production of IL-12 by Macrophages or DCs that will result in the INF-γ production by the T cells and NK cells. A key step in Th2 differentiation is the production of IL-4 by Mast cells and eosinophil granulocytes then later the T cells join to produce IL-4. A key step in Th17 differentiation is the production of IL-1, IL-6 and IL-23 by DCs + TGFβ. Absence of IL-4 and INF-γ. A SEGÍTŐ T LIMFOCITA ALPOPULÁCIÓK KÜLÖNBÖZŐ ANTIGÉN PREZENTÁLÓ SEJTEKKEL MŰKÖDNEK EGYÜTT B7 expression antigen presentation Csíraközpont kialakulása Affinity maturation Th2 B Isotype switch Memória B sejt képződés IL - 4 B7 expression DC MΦ Th1 IFNγ antigen presentation MHC-II expression antigen presentation Érett dendritikus sejt Macrophage activation IL-12 helps Th1 cell differentiation Virus, bacteria, protozoa, fungi NK cell IL-12 IFNγ Th1 IL-2 IFNγ TNF-β GM-CSF IL-3 DC MΦ CD8+ cytotoxic T cell IL-12 IFNγ IL-12 Th0 Th2 IL-4 IL-5 IL-10 IL-13 IL-10 helps Th2 cell differentiation Saját szövet, tumor cell Macrophage DC Th1 IL-2 IFNγ TNF-β TNF-α GM-CSF IL-3 IL-10 Th0 IL-10 Th2 IL-4 IL-5 IL-10 IL-13 TOLERANCE The three types of effector T cell produce distinct sets of effector molecules Cytotoxic T cells alignment and delivery of cytotoxins onto a target cell Naïve CD8+ T cell Microtubules (green) Lytic granules (red) Activated CD8+ cytotoxic T cell, polarization and alignment of lytic granules + cytoplasmic components towards the target cell Release of the clustered granules at the site of cell-cell contact TCR signaling B cell activation Phases of B cell response Lymph node Germinal center (site of intense B cell proliferation) Secondary lymphoid follicle 5. Medullary cords (Macrophage & plasma cell area) Primary Lymphoid follicle B cell zone Paracortex (T cell zone) Afferent lymphatic vessel (Lymph, Ag & cells with captured Ag drained from tissue enters here) Artery Vein 6. Efferent lymphatic vessel Marginal sinus (phagocytes) Afferent lymph Secondary follicle (Ag) Primary follicle (no Ag) B CELLS B CELLS Germinal center (GC) medulla High endothelial venule (HEV) Collagen capsule Efferent lymph mature,naive Mature,naive BB-sejt cell FDC T CELLS vein arthery B CELLS T CELLS Memory B cell Plasma cell STRUCTURE OF LYMPH NODES The germinal center Where somatic Hypermutation takes place LZ FDC DZ LZ: Light zone DZ: Dark zone FDC: Follicular dendritic cell Somatic hypermutation High frequency mutation in the rearranged heavy and light chains V domain genes (at the CDR loops) of immunoglobulin genes in activated B cells. An almost random introduction of single-nucleotide substitutions (point mutations) that results in variant antibodies, some of which have higher affinity for the antigen. 1,000,000 times the ordinary mutation rate of a gene Affinity maturation Increasing the affinity of antigen binding sites of antibodies; 1. Somatic hypermutation and 2. The selection of the B cells with the higher affinity to the antigen to be differentiated into plasma cell. !!! Do not confuse with somatic recombination!!! That is DNA recombination in immunoglobulins and TCRs gene segments during B and T cell development, that encode the variable region polypeptide chain! BCR signaling