* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download p53 Sequencing for Li-Fraumeni Syndrome
Epigenomics wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Cre-Lox recombination wikipedia , lookup
Genetic engineering wikipedia , lookup
Molecular cloning wikipedia , lookup
Deoxyribozyme wikipedia , lookup
Non-coding DNA wikipedia , lookup
Bisulfite sequencing wikipedia , lookup
DNA paternity testing wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Genealogical DNA test wikipedia , lookup
Metagenomics wikipedia , lookup
History of genetic engineering wikipedia , lookup
Genome (book) wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Cancer epigenetics wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Microevolution wikipedia , lookup
Helitron (biology) wikipedia , lookup
Designer baby wikipedia , lookup
Cell-free fetal DNA wikipedia , lookup
Frameshift mutation wikipedia , lookup
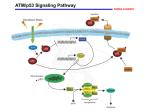
p53 Sequencing for Li-Fraumeni Syndrome Li-Fraumeni Syndrome (LFS) is a rare, autosomal dominant familial cancer syndrome with a gene frequency of approximately 1/50,000. The disease was first described in 1969 by Li and Fraumeni, who, during a study of childhood rhabdomyosarcomas, identified five pedigrees with an unusually large number of family members affected by diverse cancer types. Cancers in these families included soft tissue sarcomas, early-onset breast cancer, acute leukemias, brain tumors, carcinoma of the lung, pancreas and skin, and adrenocortical carcinoma. In 1988, Li and colleagues defined “classic” LFS kindreds as families who met the following criteria: (1) a proband with bone or soft tissue sarcoma diagnosed before the age of 45, (2) one first degree relative of the proband with cancer before the age of 45 and (3) one first or second degree relative (same lineage) of the proband with cancer before the age of 45 or sarcoma at any age. More recently it has been recognized that some families are affected with tumors not previously included in the definition of LFS such as germ cell tumors, melanoma, prostate, and pancreatic cancer. These families have been referred to as extended LFS. In addition to extended LFS, a group of investigators has also defined Li-Fraumeni-syndrome-like (LFSL), in which families demonstrate clustering of tumors typical of LFS families, but do not meet the criteria for classical LFS. Studies which should help to clarify distinctions between LFS, extended LFS, and LFS-L are currently underway. In 1990, Malkin et al. demonstrated germline p53 mutations in families with LFS (Science 250:1233, 1990). The p53 protein is a transcription factor which regulates growth factor expression; the p53 protein exerts antiproliferative effects via control at G1/S and G2/M checkpoints and also plays a role in apoptosis and cellular responses to DNA damage. The p53 gene was investigated as a candidate for LFS because somatic p53 mutations had been previously identified in many sporadic malignancies including rhabdomyosarcomas, osteosarcomas, soft-tissue sarcomas, brain tumors, and carcinoma of the lung and breast. Recent studies have demonstrated that 50-70% of classic LFS families have germline p53 mutations; explanations for the lack of identifiable p53 mutations in 30-50% of classic LFS families have yet to be elucidated. It is also important to note that germline p53 mutations have also been identified in LFS-L families and in a small percentage of patients with cancers not typically associated with LFS. Physicians should be aware: 1. Approximately 30-50% of LFS families do not have an identifiable germline mutation within the p53 gene. For those LFS families in which a p53 mutation is present, the vast majority of these mutations will be located within exons 410. However, for certain cases, sequencing of additional p53 exons may be indicated. These cases should be discussed with the director of the Molecular Diagnostics Lab. 2. For predictive and prenatal testing, it is important to first document the presence of a mutation in an affected family member. 3. Test results should be interpreted in the context of clinical findings, family history, and other laboratory results. 4. Genetic counseling is recommended for all cases. Testing offered: Molecular genetic testing for LFS involves sequence-based analysis for the detection of p53 mutations. DNA is extracted from the patient specimen and four PCR reactions are used to amplify exons 4-10 of the p53 gene. PCR amplified DNA fragments, including intron/exon boundaries, are then sequenced completely in both the forward and reverse directions. Patient sequences are compared to wild type p53 sequences. Turnaround Time: Results are routinely available within 12 weeks. Indications for Testing: Individuals with clinical features of LFS. Individuals with a family consistent with LFS. Sample requirements: Samples should be accompanied by a completed University of Minnesota Outreach Laboratories Molecular requisition. Blood: 5-10 cc blood collected in a yellow top (ACD solution A) or purple top (EDTA) tube sent overnight at room temperature. Isolated DNA: At least 5 µg of purified genomic DNA will be accepted for analysis Cultured cells: 1-2 T-25 flasks of cultured cells may be sent overnight at room temperature in a flask filled completely with media. Some of the sample should be cultured separately in your lab as a backup. Prices effective 1/1/2013-6/30/2014: $1,156.68 for one gene by Next Generation Sequencing; $2,332.45 for 2 genes $270.87 for known mutation In addition, $436.72 for Maternal Cell Contamination (MCC) for prenatal testing Billing: The University of Minnesota Physicians will only bill the sending facility Pre-payment by the patient is also acceptable We DO NOT bill insurance Payment: Make checks payable to the University of Minnesota Physicians Outreach Labs We do not accept credit cards CPT Codes: Full sequencing: 81479 Level II testing for known mutations: 81479 MCC: 81265 Send specimen to: U of MN Physicians Outreach Lab Attn: Specimen Management Mayo Building, Room D293 420 Delaware St S.E. (MMC 198) Minneapolis, MN 55455 Sample requirements: Samples should be accompanied by a completed University of Minnesota Physicians Outreach Laboratory Molecular requisition. Blood: 5-10 cc blood collected into a yellow top (ACD Solution A) or purple top (EDTA) tube sent overnight at room temperature. Isolated DNA: At least 5g of purified genomic DNA will be accepted for analysis. Cultured cells: 1-2 T-25 flasks of cultured cells may be sent overnight at room temperature in a flask filled completely with media. Some of the sample should be cultured separately in your lab as a backup. For more information contact: Molecular Diagnostics Laboratory Lab phone: (612)273-8445 Coordinator phone: (612)624-8948 Lab FAX: (612)273-8959