* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download METABOLISM OF CARBOHYDRATES: GLYCOLYSIS
Metalloprotein wikipedia , lookup
Lipid signaling wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Nicotinamide adenine dinucleotide wikipedia , lookup
Paracrine signalling wikipedia , lookup
Photosynthetic reaction centre wikipedia , lookup
Microbial metabolism wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Biochemical cascade wikipedia , lookup
Biosynthesis wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Lactate dehydrogenase wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Blood sugar level wikipedia , lookup
Citric acid cycle wikipedia , lookup
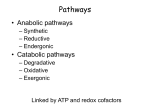
METABOLISM OF CARBOHYDRATES: GLYCOLYSIS For centuries, bakeries and breweries have exploited the conversion of glucose to ethanol and CO2 by glycolysis in yeast DIGESTION OF CARBOHYDRATES Glycogen, starch and disaccharides (sucrose, lactose and maltose) are hydrolyzed to monosaccharide units in the gastrointestinal tract. The process of digestion starts in the mouth by the salivary enzyme –amilase. The time for digestion in mouth is limited. Salivary -amilase is inhibited in stomach due to the action of hydrochloric acid. Another -amilase is produced in pancreas and is available in the intestine. -amilase hydrolyzes the -1-4-glycosidic bonds randomly to produce smaller subunits like maltose, dextrines and unbranched oligosaccharides. -amilase The intestinal juice contains enzymes hydrolyzing disaccharides into monosaccharides (they are produced in the intestinal wall) Sucrase hydrolyses sucrose into glucose and fructose Glucose sucrase Fructose Sucrose Galactose lactase Glucose Lactase hydrolyses lactose into glucose and galactose Lactose Glucose maltase Maltase hydrolyses maltose into two glucose molecules Maltose Glucose ABSORPTION OF CARBOHYDRATES Only monosaccharides are absorbed The rate of absorption: galactose > glucose > fructose Glucose and galactose from the intestine into endothelial cells are absorbed by secondary active transport Na+ Protein Glucose Protein Carrier protein is specific for D-glucose or D-galactose. L-forms are not transported. There are competition between glucose and galactose for the same carrier molecule; thus glucose can inhibit absorption of galactose. Fructose is absorbed from intestine into intestinal cells by facilitated diffusion. Absorption of glucose from intestinal cells into bloodstream is by facilitated diffusion. Transport of glucose from blood into cells of different organs is mainly by facilitated diffusion. The protein facilitating the glucose transport is called glucose transporter (GluT). GluT are of 5 types. GluT2 is located mainly in hepatocytes membranes (it transport glucose into cells when blood sugar is high); GluT1 is seen in erythrocytes and endothelial cells; GluT3 is located in neuronal cells (has higher affinity to glucose); GluT5 – in intestine and kidneys; The fate of glucose molecule in the cell Glucose Glycogenogenesis (synthesis of glycogen) is activated in well fed, resting state Glucose-6phosphate Pentose phosphate pathway supplies the NADPH for lipid synthesis and pentoses for nucleic acid synthesis Ribose, NADPH Glycogen Pyruvate Glycolysis is activated if energy is required Glycolysis is the earliest discovered and most important process of carbohydrates metabolism. Glycolysis – metabolic pathway in which glucose is transformed to pyruvate with production of a small amount of energy in the form of ATP or NADH. Glycolysis is an anaerobic process (it does not require oxygen). Glycolysis pathway is used by anaerobic as well as aerobic organisms. In glycolysis one molecule of glucose is converted into two molecules of pyruvate. In eukaryotic cells, glycolysis takes place in the cytosol. Pyruvate can be further metabolized to: (1) Lactate or ethanol (anaerobic conditions) (2) Acetyl CoA (aerobic conditions) • Acetyl CoA is further oxidized to CO2 and H2O via the citric acid cycle • Much more ATP is generated from the citric acid cycle than from glycolysis Acetyl CoA • Catabolism of glucose in aerobic conditions via glycolysis and the citric acid cycle The glycolytic pathway consist of ten enzymecatalyzed reactions that begin with a glucose and split it into two molecules of pyruvate Glycolysis (10 reactions) can be divided into three stages • In the 1st stage (hexose stage) 2 ATP are consumed per glucose • In the 3rd stage (triose stage) 4 ATP are produced per glucose • Net: 2 ATP produced per glucose Stage 1, which is the conversion of glucose into fructose 1,6-bisphosphate, consists of three steps: a phosphorylation, an isomerization, and a second phosphorylation reaction. The strategy of these initial steps in glycolysis is to trap the glucose in the cell and form a compound that can be readily cleaved into phosphorylated threecarbon units. Stage 2 is the cleavage of the fructose 1,6-bisphosphate into two three-carbon fragments dihydroxyacetone phosphate and glyceraldehyde 3-phosphate. Dihydroxyacetone phosphate and glyceraldehyde 3phosphate are readily interconvertible. In stage 3, ATP is harvested when the threecarbon fragments are oxidized to pyruvate. Glycolysis Has 10 Enzyme-Catalyzed Steps • Each chemical reaction prepares a substrate for the next step in the process 1. Hexokinase • Transfers the -phosphoryl of ATP to glucose C-6 oxygen to generate glucose 6-phosphate (G6P) • Four kinases in glycolysis: steps 1,3,7, and 10 • All four kinases require Mg2+ and have a similar mechanism Properties of hexokinases • Broad substrate specificity - hexokinases can phosphorylate glucose, mannose and fructose • Isozymes - multiple forms of hexokinase occur in mammalian tissues and yeast • Hexokinases I, II, III are active at normal glucose concentrations • Hexokinase IV (Glucokinase) is active at higher glucose levels, allows the liver to respond to large increases in blood glucose • Hexokinases I, II and III are allosterically inhibited by physiological concentrations of their immediate product, glucose-6-phosphate, but glucokinase is not. 2. Glucose 6-Phosphate Isomerase • Converts glucose 6-phosphate (G6P) (an aldose) to fructose 6-phosphate (F6P) (a ketose) • Enzyme preferentially binds the a-anomer of G6P (converts to open chain form in the active site) • Enzyme is highly stereospecific for G6P and F6P • Isomerase reaction is near-equilibrium in cells 3. Phosphofructokinase-1 (PFK-1) • Catalyzes transfer of a phosphoryl group from ATP to the C-1 hydroxyl group of F6P to form fructose 1,6bisphosphate (F1,6BP) • PFK-1 is metabolically irreversible and a critical regulatory point for glycolysis in most cells • A second phosphofructokinase (PFK-2) synthesizes fructose 2,6-bisphosphate (F2,6BP) 4. Aldolase • Aldolase cleaves the hexose F1,6BP into two triose phosphates: glyceraldehyde 3-phosphate (GAP) and dihydroxyacetone phosphate (DHAP) • Reaction is near-equilibrium, not a control point 5. Triose Phosphate Isomerase (TPI) • Conversion of DHAP into GAP • Reaction is very fast, only the D-isomer of GAP is formed • Reaction is reversible. At equilibrium, 96% of the triose phosphate is DHAP. However, the reaction proceeds readily from DHAP to GAP because the subsequent reactions of glycolysis remove this product. Fate of carbon atoms from hexose stage to triose stage 6. Glyceraldehyde 3-Phosphate Dehydrogenase (GAPDH) • Conversion of GAP to 1,3-bisphosphoglycerate (1,3BPG) • Molecule of NAD+ is reduced to NADH • Energy from oxidation of GAP is conserved in acidanhydride linkage of 1,3BPG • Next step of glycolysis uses the high-energy phosphate of 1,3BPG to form ATP from ADP 7. Phosphoglycerate Kinase (PGK) • Transfer of phosphoryl group from the energy-rich mixed anhydride 1,3BPG to ADP yields ATP and 3-phosphoglycerate (3PG) • Substrate-level phosphorylation - Steps 6 and 7 couple oxidation of an aldehyde to a carboxylic acid with the phosphorylation of ADP to ATP 8. Phosphoglycerate Mutase • Catalyzes transfer of a phosphoryl group from one part of a substrate molecule to another • Reaction occurs without input of ATP energy 9. Enolase: 2PG to PEP • 2-Phosphoglycerate (2PG) is dehydrated to phosphoenolpyruvate (PEP) • Elimination of water from C-2 and C-3 yields the enolphosphate PEP • PEP has a very high phosphoryl group transfer potential because it exists in its unstable enol form 10. Pyruvate Kinase (PK) PEP + ADP Pyruvate + ATP • Catalyzes a substrate-level phosphorylation • Metabolically irreversible reaction • Regulation both by allosteric modulators and by covalent modification • Pyruvate kinase gene can be regulated by various hormones and nutrients Net reaction of glycolysis During the convertion of glucose to pyruvate: • Two molecules of ATP are produced • Two molecules of NAD+ are reduced to NADH Glucose + 2 ADP + 2 NAD+ + 2 Pi 2 Pyruvate + 2 ATP + 2 NADH + 2 H+ + 2 H2O Scientific investigations into fermentation of grape sugar were pioneering studies of glycolysis GLYCOLYSIS The Fate of Pyruvate The sequence of reactions from glucose to pyruvate is similar in most organisms and most types of cells. The fate of pyruvate is variable. Three reactions of pyruvate are of prime importance: 1. Aerobic conditions: oxidation to acetyl CoA which enters the citric acid cycle for further oxidation 2. Anaerobic conditions (muscles, red blood cells): conversion to lactate 3. Anaerobic conditions (microorganisms, yeast): conversion to ethanol Diverse Fates of Pyruvate Metabolism of Pyruvate to Ethanol Ethanol is formed from pyruvate in yeast and several other microorganisms in anaerobic conditions. Two reactions required: The first step is the decarboxylation of pyruvate to acetaldehyde. Enzyme - pyruvate decarboxylase. Coenzyme - thiamine pyrophosphate (derivative of the vitamin thiamine B1) The second step is the reduction of acetaldehyde to ethanol. Enzyme - alcohol dehydrogenase (active site contains a zinc). Coenzyme – NADH. The conversion of glucose into ethanol is an example of alcoholic fermentation. The net result of alcoholic fermentation is: Glucose+2Pi + 2ADP + 2H+ 2 ethanol + 2CO2 + 2ATP + 2H2O The ethanol formed in alcoholic fermentation provides a key ingredient for brewing and winemaking. There is no net NADH formation in the conversion of glucose into ethanol. NADH generated by the oxidation of glyceraldehyde 3-phosphate is consumed in the reduction of acetaldehyde to ethanol. Metabolism of Pyruvate to Lactate Lactate is formed from pyruvate in an animal organism and in a variety of microorganisms in anaerobic conditions. The conversion of glucose into lactate is called lactic acid fermentation. Enzyme - lactate dehydrogenase. Coenzyme – NADH. • Muscles of higher organisms and humans lack pyruvate decarboxylase and cannot produce ethanol from pyruvate • Muscle contain lactate dehydrogenase. During intense activity when the amount of oxygen is limiting the lactic acid can be accumulated in muscles (lactic acidosis). • Lactate formed in skeletal muscles during exercise is transported to the liver. • Liver lactate dehydrogenase can reconvert lactate to pyruvate. Overall reaction in the conversion of glucose into lactate: Glucose + 2 Pi + 2 ADP 2 lactate + 2 ATP + 2 H2O As in alcoholic fermentation, there is no net NADH formation. NADH formed in the oxidation of glyceraldehyde 3phosphate is consumed in the reduction of pyruvate. Metabolism of Pyruvate to Acetyl CoA In aerobic conditions pyruvate is converted to acetyl coenzyme A (acetyl CoA). Acetyl CoA enters citric acid cycle where degrades to CO 2 and H2O and the energy released during such oxidation is utilized in NADH and FADH 2. Pyruvate is converted to acetyl CoA in the matrix of mitochondria. The overall reaction: Pyruvate + NAD+ + CoA acetyl CoA + CO2 + NADH Reaction is catalyzed by the pyruvate dehydrogenase complex (three enzymes and five coenzymes). If pyruvate is converted to acetyl CoA, NADH formed in the oxidation of glyceraldehyde 3-phosphate ultimately transfers its electrons to O 2 through the electron-transport chain in mitochondria. Other Sugars Can Enter Glycolysis • Glucose is the main metabolic fuel in most organisms • Other sugars convert to glycolytic intermediates • Fructose and sucrose (contains fructose) are major sweeteners in many foods and beverages • Galactose from milk lactose (a disaccharide) • Mannose from dietary polysaccharides, glycoproteins The Entry of Fructose into Glycolysis Much of the ingested fructose is metabolized by the liver, using the fructose 1-phosphate pathway. The first step is the phosphorylation of fructose to fructose 1phosphate by fructokinase. Fructose 1-phosphate is then split into glyceraldehyde and dihydroxyacetone phosphate, an intermediate in glycolysis, by a specific fructose 1 -phosphate aldolase. Glyceraldehyde is then phosphorylated to glyceraldehyde 3-phosphate, a glycolytic intermediate, by triose kinase. Fructose Is Converted to Glyceraldehyde 3-Phosphate Fructose can be phosphorylated to fructose 6-phosphate by hexokinase. However, the affinity of hexokinase for glucose is 20 times as great as it is for fructose. Little fructose 6-phosphate is formed in the liver because glucose is so much more abundant in this organ. Glucose, as the preferred fuel, is also trapped in the muscle by the hexokinase reaction. Because liver and muscle phosphorylate glucose rather than fructose, adipose tissue is exposed to more fructose than glucose. Hence, the formation of fructose 6-phosphate in the adipose tissue is not competitively inhibited to a biologically significant extent, and most of the fructose in adipose tissue is metabolized through fructose 6-phosphate. The Entry of Galactose into Glycolysis Galactose is converted into glucose 6-phosphate in four steps. The first reaction is the phosphorylation of galactose to galactose 1-phosphate by galactokinase. Galactose 1-phosphate react with uridine diphosphate glucose (UDP-glucose). UDP-galactose and glucose 1-phosphate are formed. Enzyme - galactose 1-phosphate uridyl transferase. The galactose moiety of UDP-galactose is then epimerized to glucose. The configuration of the hydroxyl group at carbon 4 is inverted by UDP-galactose 4-epimerase. Glucose 1-phosphate, formed from galactose, is isomerized to glucose 6-phosphate by phosphoglucomutase. The Entry of Mannose into Glycolysis Mannose is converted to Fructose 6-Phosphate in two steps. Hexokinase catalyzes the convertion of mannose into mannose 6-phosphate. Isomerase converts mannose 6-phosphate into fructose 6-phosphate (metabolite of glycolysis). Intolerance to Milk Many people are unable to metabolize the milk sugar lactose and experience gastrointestinal disturbances if they drink milk. Lactose intolerance, or hypolactasia, is caused by a deficiency of the enzyme lactase, which cleaves lactose into glucose and galactose. Microorganisms in the colon ferment undigested lactose to lactic acid generating methane (CH4) and hydrogen gas (H2). The gas produced creates the uncomfortable feeling of gut distention and the annoying problem of flatulence. The lactic acid is osmotically active and draws water into the intestine, as does any undigested lactose, resulting in diarrhea. The gas and diarrhea hinder the absorption of other nutrients (fats and proteins). Treatment: to avoid the products containing lactose; - Galactosemia The disruption of galactose metabolism is referred to as galactosemia. Classic galactosemia is an inherited deficiency in galactose 1-phosphate uridyl transferase activity. Symptoms: - vomiting, diarrhea after consuming milk, enlargement of the liver, jaundice, sometimes cirrhosis, - cataracts, - lethargy and retarded mental development, - markedly elevated blood-galactose level The absence of the -transferase in red blood cells is a galactose is found indefinitive the urine. diagnostic criterion. The most common treatment is to remove galactose (and lactose) from the diet. Regulation of Glycolysis The rate glycolysis is regulated to meet two major cellular needs: (1) the production of ATP, and (2) the provision of building blocks for synthetic reactions. There are three control sites in glycolysis - the reactions catalyzed by hexokinase, phosphofructokinase 1, and pyruvate kinase These reactions are irreversible. Their activities are regulated by the reversible binding of allosteric effectors by covalent modification by the regulation of transcription (change of the enzymes amounts). The time required for allosteric control, regulation by phosphorylation, and transcriptional control is typically in milliseconds, seconds, and hours, respectively. Phosphofructokinase 1 Is the Key Enzyme in the Control of Glycolysis Phosphofructokinase 1 is the most important control element in the mammalian glycolytic pathway. Phosphofructokinase 1 in the liver is a tetramer of four identical subunits. The positions of the catalytic and allosteric sites are identical. High levels of ATP allosterically inhibit the phosphofructokinase 1 in the liver lowering its affinity for fructose 6-phosphate. AMP reverses the inhibitory action of ATP, and so the activity of the enzyme increases when the ATP/AMP ratio is lowered (glycolysis is stimulated as the energy charge falls). A fall in pH also inhibits phosphofructokinase 1 activity. The inhibition of phosphofructokinase by H + prevents excessive formation of lactic acid and a precipitous drop in blood pH (acidosis). Phosphofructokinase 1 is inhibited by citrate, an early intermediate in the citric acid cycle. A high level of citrate means that biosynthetic precursors are abundant and additional glucose should not be degraded for this purpose. Fructose 2,6-bisphosphate (F-2,6-BP) is a potent activator of phosphofructokinase 1. F-2,6-BP activates phosphofructokinase I by increasing its affinity for fructose 6-phosphate and diminishing the inhibitory effect of ATP. Fructose 2,6-bisphosphate is formed in a reaction catalyzed by phosphofructokinase 2 (PFK2), a different enzyme from phosphofructokinase 1. Fructose 2,6-bisphosphate is hydrolyzed to fructose 6phosphate by a specific phosphatase, fructose bisphosphatase 2 (FBPase2). Both PFK2 and FBPase2 are present in a single polypeptide chain (bifunctional enzyme). Regulation of Glycolysis by Fructose 2,6-bisphosphate When blood glucose level is low the glucagon is synthesized by pancreas Glucagon binds to cell receptors, stimulates the protein kinase A activity Protein kinase A phosphorylates the PFK-2 inhibiting its kinase activity and stimulating its phosphatase activity As result the amount of F-2,6-BP is decreased and glycolysis is slowed. Regulation of Hexokinase Hexokinase is inhibited by its product, glucose 6-phosphate (G-6-P). High concentrations of G-6-P signal that the cell no longer requires glucose for energy, for glycogen, or as a source of biosynthetic precursors. Glucose 6-phosphate levels increase when glycolysis is inhibited at sites further along in the pathway. Glucose 6-phosphate inhibits hexokinase isozymes I, II and III. Glucokinase (isozyme IV) is not inhibited by glucose 6-phosphate. The role of glucokinase is to provide glucose 6-phosphate for the synthesis of glycogen. Regulation of Pyruvate Kinase (PK) Several isozymic forms of pyruvate kinase are present in mammals (the L type predominates in liver, and the M type in muscle and brain). Fructose 1,6-bisphosphate allosterically activates pyruvate kinase. ATP allosterically inhibits pyruvate kinase to slow glycolysis when the energy charge is high. Finally, alanine (synthesized in one step from pyruvate) also allosterically inhibits the pyruvate kinases (signal that building blocks are abundant). The isozymic forms of pyruvate kinase differ in their susceptibility to covalent modification. The catalytic properties of the L (liver) form—but not of the M (brain) form controlled by reversible phosphorylation. When the blood-glucose level is low, the glucagon leads to the phosphorylation of pyruvate kinase, which diminishes its activity. Inhibition 1) PFK-1 is inhibited by ATP and citrate 2) Pyruvate kinase is inhibited by ATP and alanine 3) Hexokinase is inhibited by excess glucose 6-phosphate Regulation of Glycolysis Stimulation 1) AMP and fructose 2,6bisphosphate (F2,6BP) relieve the inhibition of PFK-1 by ATP 2) F1,6BP stimulate the activity of pyruvate kinase Alanine Regulation of Hexose Transporters Several glucose transporters (GluT) mediate the thermodynamically downhill movement of glucose across the plasma membranes of animal cells. GluT is a family of 5 hexose transporters. Each member of this protein family consists of a single polypeptide chain forming 12 transmembrane segments. GLUT1 and GLUT3, present in erythrocytes, endothelial, neuronal and some others mammalian cells, are responsible for basal glucose uptake. Their Km value for glucose is about 1 mM. GLUT1 and GLUT3 continually transport glucose into cells at an essentially constant rate. GLUT2, present in liver and pancreatic -cells has a very high Km value for glucose (15-20 mM). Glucose enters these tissues at a biologically significant rate only when there is much glucose in the blood. GLUT4, which has a Km value of 5 mM, transports glucose into muscle and fat cells. The presence of insulin leads to a rapid increase in the number of GLUT4 transporters in the plasma membrane. Insulin promotes the uptake of glucose by muscle and fat. The amount of this transporter present in muscle membranes increases in response to endurance exercise training. GLUT5, present in the small intestine, functions primarily as a fructose transporter. The Pasteur Effect Under anaerobic conditions the conversion of glucose to pyruvate is much higher than under aerobic conditions (yeast cells produce more ethanol and muscle cells accumulate lactate) The Pasteur Effect is the slowing of glycolysis in the presence of oxygen. • More ATP is produced under aerobic conditions than under anaerobic conditions, therefore less glucose is consumed aerobically. The Pentose Phosphate Pathway The fate of glucose molecule in the cell Synthesis of glycogen Glucose Pentose phosphate pathway Glucose-6phosphate Glycogen Ribose, NADPH Degradation of glycogen Gluconeogenesis Glycolysis Pyruvate The Role of Pentose Phosphate Pathway (phosphogluconate pathway) (1) Synthesis of NADPH (for reductive reactions in biosynthesis of fatty acids and steroids) (2) Synthesis of Ribose 5-phosphate (for the biosynthesis of ribonucleotides (RNA, DNA) and several cofactors) (3) Pentose phosphate pathway also provides a means for the metabolism of “unusual sugars”, 4, 5 and 7 carbons. Pentose phosphate pathway does not function in the production of high energy compounds like ATP. Occurrence of the pentose phosphate pathway • Liver, mammary and adrenal glands, and adipose tissue • Red blood cells (NADPH maintains reduced iron) • NOT present in skeletal muscles. • All enzymes in the cycle occur in the cytosol Two phases: 1) The oxidative phase that generates NADPH 2) The nonoxidative phase (transketolase/ transaldolase system) that interconvert phosphorylated sugars. Oxidative phase of pentose phosphate cycle Nonoxidative phase of pentose phosphate cycle Conversion of glucose-6-phosphate to 6-phosphogluconolactone Conversion of 6-phosphogluconolactone to 6-phosphogluconate Conversion of 6-phosphogluconate to ribuloso 5-phosphate Conversions of ribulose 5-phosphate Ribose 5-phosphate isomerase The pentose phosphate pathway ends with these five reactions in some tissue. In others it continue in nonoxidative mode to make fructose 6-phosphate and glyceraldehyde 3-phosphate. These reactions link pentose phosphate pathway with glycolysis. The net reaction for the pentose phosphate pathway Glucose + ATP + 2NADP+ + H2O ribose 5-phosphate + CO2 + 2NADPH + 2H+ + ADP Interconversions Catalyzed by Transketolase and Transaldolase • Transketolase and transaldolase have broad substrate specificities • They catalyze the exchange of twoand three-carbon fragments between sugar phosphates • For both enzymes, one substrate is an aldose, one substrate is a ketose Reaction catalyzed by transketolase Reaction catalized by transaldolase Reaction catalyzed by transketolase Glucose-6-phosphate dehydrogenase deficiency NADPH is required for the proper action of the tripeptide glutathione (GSH) (maintains it in the reduced state). GSH in erythrocytes maintains hemoglobin in the reduced Fe(II) state necessary for oxygen binding. GSH also functions to eliminate H2O2 and organic peroxides. Peroxides can cause irreversible damage to hemoglobin and destroy cell membranes. Glucose-6-phosphate dehydrogenase deficiency – the most common enzymopathy affecting hundreds of millions of people. About 10 % of individuals of African or Mediterranean descent have such genetic deficiency. Erythrocytes with a lowered level of reduced glutathione are more susceptible to hemolysis and are easily destroyed especially if they are stressed with drugs (for example, antimalarial drugs). In severe cases, the massive destruction of red blood cells causes death. Red blood cells with Heinz bodies. Dark particles (Heinz bodies) are denaturated proteins adhered to cell membranes.