* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Oncogenomics wikipedia , lookup
Ridge (biology) wikipedia , lookup
Gene desert wikipedia , lookup
Epigenetics of diabetes Type 2 wikipedia , lookup
Minimal genome wikipedia , lookup
X-inactivation wikipedia , lookup
Genetic engineering wikipedia , lookup
Gene nomenclature wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Quantitative trait locus wikipedia , lookup
Genome evolution wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Gene therapy wikipedia , lookup
History of genetic engineering wikipedia , lookup
Biology and consumer behaviour wikipedia , lookup
Genomic imprinting wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Gene expression programming wikipedia , lookup
Point mutation wikipedia , lookup
Public health genomics wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Epigenetics of human development wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Dominance (genetics) wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Gene expression profiling wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Designer baby wikipedia , lookup
Gene Characteristics
Relations between genes
Relationships between Genes
I. Between Alleles
Dominance – recessiveness
Co-dominance
Lethal and semi-lethal genes
Poly-allelism
Gene families
II. Between Non-alleles
Epistasis
Genetic heterogeneity
Ask your questions in due time!
Dominance – recessiveness
► Genes
that influence the
PHENOTYPE both in the
homozygous and the
heterozygous state are dominant.
Year introduced: 1968
► Genes
that influence the
PHENOTYPE only in the
homozygous state are recessive.
►
( 1968)
Dominance – recessiveness
►
A dominant trait refers to a genetic feature that hides the
recessive trait in the phenotype of an individual.
►
A dominant trait is a phenotype that is seen in both the
homozygous AA and heterozygous Aa genotypes.
►
For example Huntington Disease is an abnormal dominant
trait in humans.
►
A dominant trait when written in a genotype is always written before
the recessive gene in a heterozygous pair. A heterozygous genotype
is written Aa, not aA
Dominance – recessiveness
►
►
►
►
Many traits are determined by pairs of
complementary genes, each inherited from a
single parent.
Often when these are paired and compared,
one allele (the dominant) will be found to
effectively shut out the instructions from the
other, recessive allele.
For example, if a person has one allele IA and
one i, that person will always have blood type
A.
For a person to have blood type 0, both alleles
must be i (recessive).
Dominance – recessiveness
► When
an individual has two dominant
alleles, the condition is referred to as
homozygous dominant (e.g. IA IA);
► An individual with two recessive alleles is
called homozygous recessive (e.g. ii).
► An individual carrying one dominant and
one recessive allele is referred to as
heterozygous (e.g. Iai).
Words don’t come easy?
► Repeat,
exercise
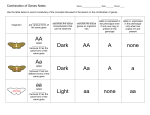
Parents
Offspring Genotype
Offspring
Phenotype
1) AA x AA
100% AA (homozygotes)
100% A
2) AA x Aa
50% AA ; 50% Aa (homo-;heterozygotes)
100% A
3) AA x aa
100% Aa (heterozygotes)
100% A
4) Aa x aa
50% Aa; 50% aa (homo-; heterozygotes)
50% A; 50% a
5) Aa x Aa
25% AA; 50% Aa; 25% aa
(homo-; heterozygotes)
75% Aa; 25% aa
6) aa x aa
100% aa (homozygotes)
100% a
Dominant Inheritance
►
If one of two parents (4. in the previous table) is affected by a
genetic condition with a dominant inheritance pattern, every child has
a one-in-two risk of being affected.
►
So on average half their children will be affected and half their
children will not be affected and so will not pass on the condition.
►
However, as chance/probability determines inheritance, it is also
possible that all or none of their children will be affected.
►
Examples of genetic conditions that show a dominant pattern of
inheritance are Huntington’s disease, achondroplasia and
neurofibromatosis.
Achondroplasia
People with this condition have an average body size,
but shorter limbs.
This is because the bones in their arms and legs grow
more slowly, both in the womb and throughout
childhood.
Achondroplasia is one of the most common causes of
short stature.
Most people with achondroplasia do not consider
themselves disabled, just different.
Young children with achondroplasia may have
hearing, speech or breathing problems but all of these
can be treated.
Father and son, both with
achondroplasia.
How is achondroplasia inherited?
People with achondroplasia may pass on the condition to their children.
If one parent is affected, each child has a one-in-two risk of having
achondroplasia, and a one-in-two probability of being of average height
(normal).
How is achondroplasia inherited?
If both parents have achondroplasia (An),
children have a one in four chance of
inheriting the gene from both parents, being
thus homozygotes (AA) for the mutant gene.
Newborns who inherit both genes are
considered to have a severe form of
achondroplasia, where survival is usually
less than 12 months after birth.
How is achondroplasia inherited?
If both parents have achondroplasia (An),
children have a one in four chance of
inheriting the gene from both parents, being
thus homozygotes (AA) for the mutant gene.
Newborns who inherit both genes are
considered to have a severe form of
achondroplasia, where survival is usually
less than 12 months after birth.
Average adult height of 131 cm (4 feet, 3.8 inches) for males
and 123 cm (4 feet, 0.6 inches) for females
The FGFR3 gene is responsible for
causing achondroplasia.
FGFR3 is the acronym for fibroblast growth
factor receptor 3
Cytogenetic location of FGFR3 Gene : 4p16.3
Molecular location on chromosome 4: from base
pair 1,762,853 to base pair 1,777,828
The protein plays a role in the development and
maintenance of bone and brain tissue.
Researchers believe that this receptor regulates
bone growth by limiting the formation of bone
from cartilage, particularly in the long bones.
FGFR3 Function
► This
protein is part of the family of
fibroblast growth factor receptors.
These proteins are very similar and play
a role in several important cellular
functions, which include:
► Regulation of cell growth and
► Determination of cell type
► Formation of blood vessels
► Wound healing
► Embryo development.
division
Achondroplasia
Is a bone growth disorder
Cartilage has difficulty converting to bone,
which results in dwarfism.
Although the word literally means "without
cartilage formation," the problem is not the
formation of cartilage. The problem occurs when
the cartilage has difficulty converting to bone,
especially in the long bones of the arms and legs.
►
http://bones.emedtv.com/achondroplasia/achondroplasia.html
From cartilage to bone
Achondroplasia and FGFR3 Gene Function
►
►
►
The protein made by the FGFR3 gene is a receptor that
regulates bone growth by limiting the formation of bone
from cartilage (a process called ossification), particularly in
the long bones.
Researchers believe that mutations in the FGFR3 gene
cause the receptor to be overly active, which interferes
with ossification and leads to the disturbances in bone
growth seen with this disorder.
This theory is supported by the knockout mouse model in
which the receptor is absent, and so the negative regulation
of bone formation is lost. The result is a mouse with
excessively long bones and elongated vertebrae, resulting
in a long tail.
Achondroplasia
► Achondroplasia
can be either inherited, or
the result of a new mutation in the FGFR3
gene ;
► In most cases (80 percent), the condition
is due to a random, new, sporadic
mutation of FGFR3.
► Scientists know this because people with
this type of achondroplasia have parents
of average size (normal), but scientists do
not know (yet) why this mutation occurs.
Achondroplasia
►
►
►
Achondroplasia can be detected before birth
by the use of prenatal ultrasound.
The diagnosis can be made by fetal ultrasound
by progressive discordance between the
femur length and biparietal diameter by age.
The trident hand configuration can be seen if
the fingers are fully extended.
Additionally a DNA test can be performed
before birth to detect homozygosity, where
two copies of the mutant gene are inherited, a
condition which is lethal and leads to
stillbirths.
The left image is a radiograph of the hand of a young patient with achondroplasia. The characteristic
"trident" deformity is present, consisting of separation of the first and second as well as the third and fourth
digits. Notice the shortened tubular bones of the hand, particularly the proximal phalanges.
The right image is of an
adult. To identify are the
short tubular bones with
a gracile distal ulna,
characteristic of
achondroplasia.
Achondroplasia
►
No cure for achondroplasia currently exists. Therefore,
achondroplasia treatment involves preventing or treating
the signs, symptoms, or health conditions that occur as a
result of the disorder.
►
Health problems commonly associated with achondroplasia
that may require treatment include:
►
Reduced muscle strength
Recurring ear infections
Breathing disorders (apnea)
Obesity
Crowded teeth.
Social and family support, along with regular follow-up
visits with healthcare providers, are also an important part
of achondroplasia treatment.
Achondroplasia
► Characteristic
symptoms include:
o An average-size trunk.
o Short arms and legs, with particularly short
upper arms and thighs.
o An enlarged head with a prominent forehead.
o Fingers that are typically short. The ring finger
and middle finger may diverge, giving the hand
a trident appearance.
Achondroplasia is one of the most common causes of dwarfism.
Characteristics of a person with the disease include:
A short stature with proportionately short arms and legs
A large head (macrocephaly),
A prominent forehead (frontal bossing)
A flattened bridge of the nose.
Dominance – recessiveness
►
An example of an autosomal dominant human
disorder is Huntington's disease (HD), which is a
neurological disorder resulting in impaired motor
function.
►
The mutant allele results in an abnormal protein,
containing large repeats of the amino acid glutamine.
This defective protein is toxic to neural tissue,
resulting in the characteristic symptoms of the
disease.
►
Hence, one copy of the deffective gene is sufficient to
confer the disorder to the person carrying it.
1983
Scientists discover a gene marker
linked to HD on the short arm of
chromosome 4, which indicates that
the Huntington gene is also located
on chromosome 4. Predictive linkage
testing is introduced to assess the
likelihood of contracting HD.
Huntington disease (HD)
►
Huntington disease (HD) is a disorder affecting
nerve cells in the brain.
1993
The location of the Huntington
gene is discovered at the 4p16.3
gene site on chromosome 4. The
gene is found to contain codon
C-A-G in varying numbers.
An abnormal number of CAG repeats turns out to be a highly
reliable way to tell whether someone has the allele for HD.
Do not loose your enthusiasm, there is still more to find out
Huntington disease (HD)
► Huntington's
disease is one of several
trinucleotide repeat disorders, caused by
the length of a repeated section of a
gene exceeding the normal range. The
huntingtin gene (HTT) normally provides
the information to produce Huntingtin
protein, but when affected, produces
mutant Huntingtin (mHTT) instead.
Huntington disease (HD)
►It
is an inherited progressive
neurodegenerative disorder
characterized by:
choreiform movements (uncoordinated,
jerky body movements),
psychiatric problems, and
dementia ( decline in some mental abilities)
Huntington disease (HD)
►
This genetic neurological disorder itself isn't fatal, but as
symptoms progress, complications reducing life expectancy
increase.
►
Abnormal movements are initially exhibited as general lack of
coordination, an unsteady gait and slurring of speech, but, as
the disease progresses, any function that requires muscle
control is affected, causing physical instability, abnormal facial
expression, but the most characteristic physical symptoms are
jerky, random, and uncontrollable movements called chorea.
Huntington disease
►
►
Mild symptoms, which include forgetfulness, clumsiness and
personality changes first appear in middle age.
Over the next 10-20 years, a person with HD gradually loses all control
of their mental and physical abilities.
►There is no
cure for HD at
the moment,
although some
of the
symptoms can
be treated
with drugs.
Huntington disease
(Huntington chorea)
► The
advances in molecular genetics
make it possible to detect Huntington
disease in a preclinical stage at or
even before birth.
► The
molecular approach does not
replace prior approaches to
Huntington disease but is synergistic
and provides a model of the new
genetics.
Huntington disease (HD)
►
►
►
The Huntingtin gene (HTT), also called HD
(Huntington disease) gene, or the IT15
("interesting transcript 15") gene is located
on the short arm of chromosome 4 (4p16.3).
HTT contains a sequence of three DNA bases—
cytosine-adenine-guanine (CAG)—repeated
multiple times (i.e. ...CAGCAGCAG...) on its 5'
end, known as a trinucleotide repeat/codon.
CAG is coding for the amino acid glutamine, so a
series of them results in the production of a
chain of glutamine known as polyglutamine or
polyQ tract, and the repeated part of the gene,
the PolyQ region
Where is the HTT gene located?
Cytogenetic Location: 4p16.3
Molecular Location on chromosome 4:
base pairs 3,046,205 to 3,215,484
Huntington disease (HD)
►
Huntington disease is caused by a
abnormal trinucleotide (CAG)
expansion in the HD gene
►
Normal persons have a CAG repeat
count of between 7 and 35 repeats
►
HTT gene encodes the protein
huntingtin, and if abnormal resulting
in an expanded polyglutamine tract.
►
Huntingtin is present in a large
number of tissues throughout the
body, with the highest levels of
expression seen in the brain.
Huntingtin
► The
exact function of this protein
is yet not known, but it plays an
important role in nerve cells.
► Within cells, huntingtin may be
involved in
o signaling,
o transporting materials,
o binding proteins and other structures, and
o protecting against programmed cell death (apoptosis).
►
Huntingtin protein is required for normal
development before birth.
Huntington disease (HD)
►
The pathophysiology of HD is not fully
understood, although it is thought to be
related to toxicity of the mutant
huntingtin protein.
►
However, pathology appears to be limited
to the central nervous system, with
atrophy of the caudate and putamen (the
neostriatum) being most prominent.
►
At the cellular level, protein aggregates
are seen both in the cytoplasm and
nucleus.
Huntington disease (HD)
►
Although most cases start clinically in
midadulthood, usually between 35 and
42 years of age, there is great
variability in age of onset.
►
About 3% of cases are diagnosed as
juvenile Huntington disease before the
age of 15 years. Late onset is well
known after 50 years of age.
Huntington disease (HD)
► Generally,
the number of CAG repeats
is related to how much the person is
affected, and correlates with age at
onset and the rate of progression of
symptoms.
► For
example, 36–39 repeats result in
much later onset and slower
progression of symptoms than the
mean of ill persons, such that some
individuals may die of other causes
before they even manifest symptoms of
Huntington disease, this is termed
"reduced/incomplete penetrance”
Repeat count Classification
<27
Normal
Disease
status
Unaffected
27–35
Intermediate
Unaffected
36–39
Reduced
Penetrance
Full Penetrance
+/- Affected
>39
Affected
There is a variation in age of onset for any given CAG repeat
length, particularly within the intermediate range (40–50
CAGs). For example, a repeat length of 40 CAGs leads to an
onset ranging from 40 to 70 years of age in one study. This
variation means that, although algorithms have been
proposed for predicting the age of onset, in practice, it can
not be predicted confidently
Understanding HD
The symptoms of Huntington
disease (HD) appear when an
abnormal protein builds up in nerve
cells in certain areas of the brain,
causing the cells to die.
► One of the brain areas affected is
the area that controls movement.
► Cells in the outer layer of the brain
also die, affecting mental abilities.
►
►
Brain scan from a patient with
Huntington disease (right)
showing a larger cavity where
brain cells have died, compared
with a normal brain (left).
(arrows)
Testing for HD
As the symptoms of Huntington disease (HD) do not usually appear until
middle age, some people only discover they are at risk when one of
their parents or grandparents is diagnosed.
A genetic test is available to HD families that can tell people whether or
not they have inherited the altered gene, but not the age at which
they will start to develop symptoms.
Although there is no cure available at the moment, genetic tests can help
people at risk of HD make decisions about their future. However most
decide not to take the test.
DNA analysis of
Huntington’s disease.
Each lane shows a
different person's DNA:
two bands in the normal
(N) range show someone
is unaffected.
One band in the H range
predicts the person will
get Huntington disease.
How is HD inherited?
►
Huntington disease (HD) is caused by a single altered gene,
which is passed on from one generation to the next in affected
families
►
With one affected parent, each child has a one-in-two chance of
inheriting HD.
►
Children who do not
carry the altered gene
are free from the
condition and cannot not
pass it on to their own
children
Testing for HD
Genetic testing may infer information about relatives who
do not want it.
► Testing a descendant of an undiagnosed parent has
implications to other family members, since a positive
result automatically reveals the parent as carrying the
affected gene, and siblings (and especially identical twins)
as being 'at risk' of also inheriting it.
► This emphasizes the importance of disclosure, as
individuals have to decide when and how to reveal the
information to their children and other family members.
► For those at risk, or known to carry a mutant allele, there
can be the consideration of prenatal genetic testing in
order to ensure that the disorder is not passed on.
►
Testing for HD
►
Embryonic screening is another possibility for
affected or at-risk individuals to know if their
children will or will not inherit the disease.
►
It is possible for women who would consider
abortion of an affected fetus to test an embryo in
the womb (prenatal diagnosis).
►
Other techniques, such as preimplantation genetic
diagnosis in the setting of in vitro fertilisation, can
be used to ensure that the newborn is unaffected
Co-dominance
► In
genetics, co-dominant is denoting an
equal degree of dominance of two genes,
both being expressed in the phenotype of
the individual;
► e.g.,
genes IA and IB of the ABO blood
group are co-dominant;
► individuals
with both genes (genotype IA
IB) are type AB (phenotype).
Co-dominance
► Co-dominant
inheritance means
that the two alleles are individually
expressed in the presence of each
other, being thus equipotent;
{there may be other alleles
available at the locus that may or
may not exhibit co-dominance}.
(Latin Dominari = to govern)
Co-dominance
►
So, the heterozygous individual expresses
both phenotypes.
►
A common example is the ABO blood group
system.
►
The gene for blood types has three alleles:
IA, IB, and i on 9q34.1 - q34.2 .
►
i causes 0 blood type and is recessive to
both IA and IB
Co-dominance
►
The A and B alleles are codominant with each
other.
►
When a person has both an IA and a IB allele,
the person has AB blood type.
►
When two persons with AB blood type have
children, the children can be type A, type B, or
type AB.
►
There is a 1A:2AB:1B phenotype ratio instead
of the 3:1 phenotype ratio found when one
allele is dominant and the other is recessive.
Co-dominance
► In
the ABO blood group both types of
antigens are expressed on the surface of
the red blood cells, meaning that both
alleles result in an effective product.
The AB phenotype is less frequent
► If
the Rhesus blood groups are added, the
less frequent type is AB negative (0.5%)
Co- dominance
► Another
normal trait which shows this type of
inheritance is represented by the MN blood
group, where both alleles are fully expressed in
the phenotype
► This
trait is inherited linked to another
erythrocytic antigen S/s (dominant/ recessive)
► The
proteins coded are :glycophorin A in case of
M and N and glycophorin B responsible for S
and s
Co- dominance
► The
MNS locus (= GYP) consists of three
closely linked genes on 4 q28-q31:
5’-GYPA–GYPB-GYPE–3’
► GYPA controls M and N antigens
► GYPB controls S and s
► GYPE is not responsible for antigens on
erythrocytes
► The three genes (each of about 30 kb)
show a high degree of sequence
homology: almost 95 %
Co- dominance
►
The two different versions (alleles) of a gene are
expressed, and each version makes a slightly different
protein; as in the above illustration: GPA as type M or N
►
Both alleles influence the genetic trait or determine the
characteristics of the genetic condition
►
Most molecular markers are considered to be
codominant
Lethal and semi-lethal genes
► Genes
which result in the premature death
of the organism = LETHAL GENES
► Dominant
lethal genes kill
heterozygotes and homozygotes,
whereas recessive lethal genes kill only
homozygotes.
Lethal and semi-lethal genes
►
Lethal genes cause the death of the organisms
that carry them. Sometimes, death is not
immediate; it may even take years, depending on
the gene.
►
In any case, if a mutation results in lethality, then
this is indicative that the affected gene has a
fundamental function in the growth, development,
and survival of an organism
Lethal and semi-lethal genes
►
Another definition: A gene that in some (as
homozygous) conditions may prevent
development or cause the death of an
organism or its germ cells -- called also lethal
factor, lethal mutant, lethal mutation
►
Lethal genes can be recessive, dominant,
conditional, semi-lethal, or synthetic,
depending on the gene or genes involved
Lethal Genes
►
At the beginning of the 20th century Cuénot and Baur
discovered the first recessive lethal genes because
these altered Mendelian inheritance ratios in their
animal models.
►
Examples of human diseases caused by recessive
lethal alleles include cystic fibrosis, Tay-Sachs
disease, sickle-cell anemia.
►
Achondroplasia is an autosomal dominant bone
disorder that causes dwarfism. While the inheritance
of one achondroplasia allele can cause the disease,
the inheritance of two alleles is fatal.
Dominant Lethal Genes
►
Dominant lethal genes are expressed in both homozygotes and
heterozygotes.
►
But how can alleles like this be passed from one generation to
the next if they cause death?
►
Dominant lethal genes are rarely detected due to their rapid elimination
from populations.
►
One example of a disease caused by a dominant lethal allele is
Huntington's disease, which reduces life expectancy. Because the onset
of Huntington's disease is slow, individuals carrying the allele can pass it
on to their offspring.
►
This allows the allele to be maintained in the population.
►
Dominant traits can also be maintained in the population through
recurrent mutations beside the low of the gene (less than 100%), like in
Huntington’s chorea.
Conditional Lethal Genes
► Favism is a sex-linked, inherited condition that
►
►
►
results from deficiency in an enzyme called glucose6-phosphate dehydrogenase.
It is most common among people of Mediterranean,
African, Southeast Asian, and Sephardic Jewish
descent (Allison, 1960).
The disease was named because when affected
individuals eat fava beans, they develop hemolytic
anemia, a condition in which red blood cells break
apart and block blood vessels. Blockage can cause
kidney failure and result in death (Bowman &
Walker, 1961).
Affected individuals may also develop anemia when
administered therapeutic doses of anti-malaria
medications and other drugs.
Conditional Lethal Genes
►
Note, however, that the defective glucose-6-phosphate
dehydrogenase allele only causes death under certain
conditions, which makes it a conditional lethal gene.
►
But why would this allele be so common? The interesting thing
about individuals with the favism allele is that they are resistant
to malaria, because it is more difficult for malaria parasites to
multiply in cells with deficient amounts of glucose-6-phosphate
dehydrogenase. Therefore, carrying the allele for favism
confers an intrinsic genetic or adaptive advantage by protecting
individuals from contracting malaria.
Conditional Lethal Genes
►
Conditional lethal genes can also be expressed due to
specific circumstances, such as temperature.
►
For example, a mutant protein may be genetically
engineered to be fully functional at 30°C and
completely inactive at 37°C. Meanwhile, the wild-type
protein is fully functional at both temperatures.
►
The condition in which the mutant phenotype is
expressed is termed non-permissive, while the
condition in which the wild-type phenotype is
expressed is called permissive.
►
In order to study a conditional lethal mutant, the organism must be maintained under
permissive conditions and then switched to the non-permissive condition during the course of
a specific experiment. By developing a conditional lethal version of a dominant lethal gene,
scientists can study and maintain organisms carrying dominant lethal alleles
Synthetic Lethal
►
Two genes are synthetic lethal if mutation of either alone is
compatible with viability but mutation of both leads to
death.
►
So, targeting a gene that is synthetic lethal to a cancerrelevant mutation should kill only cancer cells and spare
normal cells.
Synthetic lethality therefore provides a conceptual
framework for the development of cancer-specific cytotoxic
agents.
This paradigm has not been exploited in the past because
there were no robust methods for systematically identifying
synthetic lethal genes.
This is changing as a result of the increased availability of
chemical and genetic tools for perturbing gene function in
somatic cells
►
►
►
Semi-lethal or Sub-lethal Genes
► Hemophilia is a hereditary disease caused
by deficiencies in clotting factors, which results
in impaired blood clotting and coagulation.
►
Because the allele responsible for hemophilia is
carried on the X chromosome, affected
individuals are predominantly males, and they
inherit the allele from their mothers.
Hemophilia
►
Normally, clotting factors help form a temporary scab
after a blood vessel is injured to prevent bleeding, but
hemophiliacs cannot heal properly after injuries because
of their low levels of blood clotting factors.
►
Therefore, affected individuals bleed for a longer period
of time until clotting occurs.
►
This means that normally minor wounds can be fatal in
a person with hemophilia.
Semi-lethal or Sub-lethal
Genes
► The
alleles responsible for
hemophilia are thus called semilethal or sub-lethal genes, because
they cause the death of only some
of the individuals or organisms
with the affected genotype.
LETHAL ALLELES
►
They differ in the developmental stage at
which they express their effects.
►
Human lethals illustrate this very well: we are
all estimated to be heterozygous for a small
number of recessive lethals in our genomes.
►
The lethal effect is expressed in the
homozygous progeny of a mating between
two people who by chance carry the same
recessive lethal in the heterozygous condition.
LETHAL ALLELES
►
►
►
►
Some lethals are expressed as deaths in utero,
where they either go unnoticed or are noticed as
spontaneous abortions.
Other lethals, such as those responsible for
Duchenne/Becker muscular dystrophy, cystic
fibrosis, or Tay-Sachs disease, exert their effects in
childhood.
The time of death can even be in adulthood, as in
Huntington disease.
The total of all the deleterious and lethal genes that
are present in individual members of a population is
called genetic load, a kind of genetic burden that
the population has to carry
Exactly what goes wrong in lethal mutations?
►
In many cases, it is possible to trace the cascade of
events that leads to death.
►
A common situation is that the allele causes a deficiency
in some essential chemical reaction. The human diseases
PKU (phenylketonuria) and cystic fibrosis are good
examples of this kind of deficiency.
►
In other cases, there is a structural defect. For example,
a lethal allele is expressed phenotypically in several
different organs, resulting in lethal symptoms. Sickle-cell
anemia, is an example.
►OVERALL...
much is still being learned about
genetics -- it is not as simple as we once thought - but the principles above are generally true.
Lethal…semi-lethal…..sublethal….conditional……is there a
difference?
Electrophoresis of hemoglobin from a person with sickle-cell anemia, a
heterozygote (called sickle-cell trait), and a normal person. The smudges
show the positions to which the hemoglobins migrate on the starch gel
Despite the 3
phenotypes,
which can be
proven in the lab,
usually the sickle
cell trait is
considered
recessive in
pathology!
Thus explaining
the inheritance of
the disease!
Still biologists use
the term
“intermediate
inheritance”, that
describes the
presence of 3
distinct
phenotypes in
the laboratory
findings.
► Often,
evolution is not totally
straightforward in practice....
► One
example in humans: Malaria and
sickle-cell anemia.
► This is actually a balanced polymorphism,
where natural selection is working in two
opposite directions at once, which holds
the different allele frequencies in
balance... instead of gradually eliminating
one!
Normal red blood cells and a sickle cell.
(diagnosis: sickle cell anemia)
Under special
conditions (low
oxygen pressure)
the normal cells
might prove the
carrier state!
HbA/HbS
Plasmodium
falciparum
does not
‘enjoy’ either
cells: of the
homozygous,
ill person (SS)
or the (AS)
heterozygous/
carrier one.
►
Hemoglobin molecules in the red blood cells carry oxygen to the
body's tissues.
►
Alleles for hemoglobin:
►
A for normal Hb --> normal cells
►
S for hemoglobin that doesn't carry as much oxygen, and which
crystallizes inside the red blood cell, causing it to become sickleshaped.
►
These sickled cells are fragile, can't carry much oxygen, and
can't get down the tiny capillary blood vessels to the body's
tissues.... resulting in pain, anemia, general disability, and if
left untreated, early death.
►
If a person has one copy of Hb (S), they can be quite fine, being
a carrier, showing occasional sickle-like cells, but not suffering
from sickle crisis and most of them have only very mild signs
and symptoms.
►
If they have two copies of Hb(S), they are usually very ill.
Die
Selected
Die
So why hasn't the gene for sickle cell simply
vanished over time due to natural selection working
against it?
►
Because in one circumstance, it's actually an ADVANTAGE to have one copy of
Hb(S): in areas with a high prevalence of malaria.
►
The malaria parasite (a protozooan, genus Plasmodium) is transmitted by
mosquitoes, and lives in the red blood cells, where it obtains the oxygen that it
needs to live.
►
Malaria can be fatal, and often hits children (i.e. before reproductive age).
►
The Plasmodium can't live in sickle cells! So... if you have some sickled cells...
your malaria infection isn't as bad as if you have all normal red blood cells!
►
So the effects of sickle cell anemia push the population's Hb alleles in one
direction, while the effects of malaria push the population's Hb alleles in the
other direction.
Whether an allele is lethal or not often
depends on the environment in which the
organism develops
►
Whereas certain alleles are lethal in virtually any
environment, others are viable in one
environment but lethal in another.
►
For example, the human hereditary diseases
cystic fibrosis and PKU are diseases that would
be lethal without treatment.
►
Furthermore, many of the alleles favored and selected by
animal and plant breeders would almost certainly be
eliminated in nature as a result of competition with the
members of the natural population. Modern grain varieties
provide good examples; only careful nurturing by farmers
has maintained such alleles for our benefit.
Lethal and semi-lethal genes
►
Geneticists commonly encounter situations in which expected
phenotypic ratios are consistently skewed in one direction by
reduced viability caused by one allele.
►
For example, in the cross A/a × a/a, we predict a progeny ratio
of:
50% A/a and
50 % a/a,
►
but we might consistently observe a ratio such as
55 %: 45 % or
60 %: 40%.
►
In such a case, the recessive phenotype is said to be sub-vital,
►
Thus, lethality may range from 0 to 100 percent,
depending on the gene itself, the rest of the genome,
and the environment.
or semi-lethal, because the lethality is expressed in only some
individuals.
Cystic fibrosis
► Is
► It
an autosomal recessive disorder
is due to mutations in the CFTR gene
(= cystic fibrosis transmembrane regulatory
gene)
The gene is large (over 250kb) consisting of
27 exons encoding a 6.5 kb transcript with
several alternatively spliced forms of
mRNA.
Cystic fibrosis – clinical aspects
►
The disease primarly affects:
► the
bronchial system
► the gastrointestinal tract
►
It is severe, progressive with formation of viscous
mucus, leading to frequent, recurrent bronchopulmonic
infections
►
Average life expectancy in typical CF is about 30 years
►
The high frequency of heterozygotes (1:25) is thought to
result from a selective advantage: they have reduced
liability to epidemic diarrhea as for example in cholera
Cystic fibrosis
Multiple allelism
►
A gene can have several different states or forms—
called multiple alleles.
►
The alleles are said to constitute an allelic series, and the
members of a series can show various degrees of dominance
to one another.
►
As examples (the normal genetic systems studied) the two
erythrocytic enzymes: acid phosphatase and glucose-6phosphate dehydrogenase.
►
Official Symbols:
ACP1 for acid phosphatase 1, the gene
being located on 2p25
G6PD glucose-6-phosphate
dehydrogenase; Gene map locus: Xq28
ACID PHOSPHATASE 1
►
Hopkinson et al. described in 1963 a new human polymorphism
involving erythrocyte acid phosphatase as demonstrated in
starch-gel electrophoresis.
►
Three alleles: P(a), P(b) and P(c), are thought to be involved,
their frequency being estimated to be 0.35, 0.60 and 0.05,
respectively. Another rare allele, P(r), was described by Giblett
and Scott (1965).
►
Dissing and Johnsen (1992) provided evidence for the molecular
basis of the 3 common alleles in Caucasians:
ACP1*A,
ACP1*B, and
ACP1*C,
which give rise to 6 possible genotypes and these
to 6 phenotypes (A, B, C, AB, AC, and BC). ( so the 3 alleles are
codominant)
GLUCOSE-6-PHOSPHATE DEHYDROGENASE
►
G6PD DEFICIENCY causes chronic ANEMIA
►
Since identification of deficiency of G6PD (Carson et al., 1956)
and of its X-chromosomal determination (Childs et al., 1958) in
the 1950s and demonstration of electrophoretic variants of this
enzyme in the early 1960s (Boyer et al., 1962), the genetic,
clinical and biochemical significance of this polymorphism has
been found to be great.
►
G6PD is in the hexose monophosphate pathway, the only NADPH-generation process in
mature red cells, which lack the citric acid cycle. For this reason G6PD deficiency has adverse
physiologic effects.
GLUCOSE-6-PHOSPHATE DEHYDROGENASE
►
Deficiency of the red cell enzyme, in various forms, is
the basis of favism,
primaquine sensitivity and some other drug-
sensitive hemolytic anemias, anemia and jaundice in the newborn, and
chronic nonspherocytic hemolytic anemia
►
Different variants of the enzyme are found in high
frequency in African, Mediterranean and Asiatic
populations and heterozygote advantage vis-a-vis
malaria has been invoked to account for the high
frequency of the particular alleles in these populations.
GLUCOSE-6-PHOSPHATE DEHYDROGENASE
►
The variety of forms of the enzyme is great, as
illustrated by the published tables (Yoshida and Beutler)
►
The demonstrated polymorphism at this X-linked locus
rivals that of the autosomal loci for the polypeptide
chains of hemoglobin.
►
Single amino acid substitution has been demonstrated as
the basis of the change in the G6PD molecule resulting
from mutation (Yoshida et al., 1967).
Designation of variant
G6PD-A(+)
Gene’s
short name
Gd-A(+)
Mutation type
Subtype
Polymorphism
nucleotide
A→G
Structure change
Asparagine→
Function change
No enzyme defect (variant)
Aspartic acid
G6PD-A(-)
Gd-A(-)
Substitution
nucleotide
G→A
Valine→Methionine
Asparagine→Aspartic acid
Lower function
G6PD-Mediterran
Gd-Med
Substitution
nucleotide
C→T
Serine→Phenylalanine
Favism
G6PD-Canton
Gd-Canton
Substitution
nucleotide
G→T
Arginine→Leucine
G6PD-Chatham
Gd-Chatham Substitution
nucleotide
G→A
Alanine→Threonine
G6PD-Cosenza
Gd-Cosenza Substitution
nucleotide
G→A
Arginine→Proline
G6PD-Mahidol
Gd-Mahidol
Substitution
nucleotide
G→A
Glycine→Serine
G6PD-Orissa
Gd-Orissa
Substitution
nucleotide
G6PD-Asahi
Gd-Asahi
Substitution
Alanine→Glycine
A→G
Asparagine→Aspartic acid
Multiple allelism
► Is
the state of having more than two alternative
contrasting characters controlled by multiple
alleles at a single genetic locus.
► E.g. All mutations that cause G6PD deficiency are
found on the long arm of the X chromosome, on
band Xq26.
► The normal G6PD gene spans some 18.5 kilobases
being symbolized GdB. The 9 variants and
mutations in the table above are well-known and
described.
What are gene families?
►
A gene family is a group of genes that share
important characteristics.
► 1.
In many cases, genes in a family share a similar
sequence of DNA building blocks (nucleotides).
► These
genes provide instructions for making products
(such as proteins) that have a similar structure or
function.
► 2.
In other cases, dissimilar genes are grouped together
in a family because proteins produced from these genes
work together as a unit or participate in the same
process.
GENE FAMILIES
►Classifying
individual genes into families helps
researchers describe how genes are related to
each other.
►
Researchers can use gene families to predict
the function of newly identified genes based
on their similarity to known genes.
►Similarities
among genes in a family can also
be used to predict where and when a specific
gene is active (expressed).
►Additionally,
gene families may provide clues
for identifying genes that are involved in
particular diseases.
►Sometimes
not enough is known about a gene
to assign it to an established family.
►In
other cases, genes may fit into more than
one family.
►No
formal guidelines define the criteria for
grouping
genes
together.
Classification
systems for genes continue to evolve as
scientists learn more about the structure and
function
of
genes
between them.
and
the
relationships
For more information about gene families
►
►
►
►
►
►
Genetics Home Reference provides information about gene families
including a brief description of each gene family and a list of the
genes included in the family.
The HUGO Gene Nomenclature Committee (HGNC) has classified
many human genes into families. Each grouping is given a name and
symbol, and contains a table of the genes in that family.
The textbook Human Molecular Genetics (second edition, 1999)
provides background information on human gene families .
The Gene Ontology database lists the protein products of genes by
their location within the cell (cellular component), biological process,
and molecular function.
The Reactome database classifies the protein products of genes
based on their participation in specific biological pathways. For
example, this resource provides tables of genes involved in controlled
cell death (apoptosis), cell division, and DNA repair.
http://ghr.nlm.nih.gov/geneFamily
Blood group gene family
►
►
►
►
Blood is classified into different groups according to the
presence or absence of molecules called antigens on the
surface of every red blood cell in a person's body.
The genes that provide instructions for making the
antigens are known as blood group determining genes.
Antigens determine blood type and can either be proteins
or complexes of sugar molecules (polysaccharides).
Blood group proteins, which carry antigens, serve a variety
of functions within the cell membrane of red blood cells.
These protein functions include:
transporting other proteins and molecules into and out of the cell,
maintaining cell structure,
attaching to other cells and molecules and
participating in chemical reactions.
Blood group gene family
►
Blood group antigens play a role in recognizing foreign cells in
the bloodstream.
►
For example, if a person with blood type A receives a blood
transfusion with blood type B, the recipient's immune system
will recognize the type B cells as foreign and mount an
immune response. Antibodies against type B blood cells (anti-B
antibodies) are made, which attack and destroy the type B
blood cells.
►
This sort of blood type mismatch can lead to illness.
►
Some blood types are associated with more severe immune
reactions than others (Rh)
►
The blood type of donated cells, or tissues in the case of organ
donation, is checked before being given to a recipient in order
to prevent this immune response.
Blood group gene family
►
There are
29 recognized blood groups, most involving only one
gene (pair), like Xg.
►
Variations (polymorphisms) within the genes that determine blood group
give rise to the different antigens for a particular blood group protein. For
example, changes in a few DNA building blocks (nucleotides) in genes
give rise to the A, B, and 0 blood types.
►
The changes that occur in the genes that determine blood groups
typically affect only the blood type and are not associated with adverse
health conditions, although exceptions do occur (Rh- mothers having a
second Rh+ conception product).
►
Erythrocytic non-enzymatic genetic systems which belong here are beside
ABO, Rh and Xg, the glycophorins A and B.
►
Another gene family is that of the globins.
C.
Relations between Genes
I. Between Alleles
Dominance – recessiveness
Co-dominance
Lethal and semi-lethal genes
Poly-allelism
Gene families
II. Between Non-alleles
Epistasis
Genetic heterogeneity
D. Correlation Genotype–Phenotype-Environment
Influences
Pleiotropy
Polygenic – Multifactorial Inheritance
Genomic imprinting
Epistasis
► Epistasis
occurs when the alleles of one
gene (e.g. H) cover up or alter the
expression of alleles of another gene (I).
► Some genes mask the expression of other
genes (e.g. h/h) just as a fully dominant
allele masks the expression of its recessive
counterpart.
► A gene that masks the phenotypic effect of
another gene is called an epistatic gene; the
gene it subordinates is the hypostatic gene.
► In the following example H/h are epistatic,
while IA/IB/i are hypostatic.
Fucosyltransferase 1 also known as FUT1
couples L-fucose to the precursor in the erythrocytic
membrane, when there is at least one allele H on
chromosome 19q, the H antigen being thus
formed.
H/H
or
H/h
This is the H antigen on
the membrane of the red
blood cells of H/H and H/h
h is the FUT1 gene with a point mutation (T725);
H is dominant and h is recessive;
in case of the h/h, recessive homozygote the transferase is
not synthesized, so that L-fucose is not going to be coupled
to the precursor and thus no H antigen is built up!
If on 9q there is at least one
gene IB, D – galactosetransferase is synthesized
and in the presence of at
least one H, D – Galactose
couples to the H antigen
building up the B antigen of
the B blood group.
Gene on chromosome
19q
9q
Precursor on the membrane
The FUT1 (H) gene is expressed predominantly in erythroid tissues whereas
the FUT2 (Se) gene is expressed predominantly in secretory tissues. When
alleles of both genes are recessive (h and se, respectively), individuals bearing
them, in homozygous state, lack the substrates for the A or B transferases
and do not express the A and B antigens.
If h/h or se/se on
19q, even if on
the chromosome
9q there is an IA
/IB the blood
group is still O,
the so called
“apparent” O or
Bombay
phenotype
If on 9q there is at least
one IA then N- acetylgalactosaminetransferase is synthesized
i=I
o
N- acetylgalactosamine
transforms the H
antigen into A
‘true”O
blood
group
No A or B antigen can be built
up!
The alleles on 19q control the activity of the alleles on 9q: h/h
individuals do not express on their erythrocytes the A or B antigen,
maybe because they lack the L-
fucose (no antigen H)
If a person is H/H or H/h and has an i/i combination on chromosome 9, the
blood group is O, also called “true” O, having on the erythrocytes the H antigen.
Notes
►
Chromosomal location: 19 q13.3 for FUT1 and FUT2, which are 35kb apart, in the same
orientation, namely, Cent-FUT2-FUT1-Ter;
►
Primary gene products of functional alleles are closely homologous alpha 1,2
fucosyltransferases that use nearly identical substrates but are expressed in different
tissues. Their products serve as substrates for the glycosyltransferases that result in
epitopes for the A and B blood group antigens; in addition, the product of FUT2 is a
precursor of epitopes resulting in antigens of the Lewis blood group system. Although
their precise function is still not known,the fucosylated glycans that are the products of
FUT1 and FUT2 may serve as ligands in cell adhesion or as receptors for certain
microorganisms.
►
FUT1 product is expressed predominantly in erythoid tissues, vascular endothelium and
primary sensory neurons of peripheral nervous system; the product of FUT2 is expressed
in saliva and other exocrine secretions, and in epithelia.
►
Expression of the antigens is known to undergo changes during development,
differentiation and maturation.
►
Aberrant expression is often observed in human pre-malignant and malignant cells.
Reminder
► Human
blood type is determined by three different
alleles, known as IA, IB, and i. The IA and IB alleles
are codominant, and the i allele is recessive.
► The possible human phenotypes for blood group
are type A, type B, type AB, and type O. Type A
and B individuals can be either homozygous (IAIA
or IB IB, respectively), or heterozygous (IAi or IBi,
respectively).
► A woman with type A blood and a man with type B
blood could potentially have offspring with which
of the following blood types? A, B, AB and/or O.
QUIZ
Which are the possibilities of alleles on chromosome 19 in each case?
Epistasis: absence of expected phenotype as a result of
masking expression of one gene pair by the expression of
another gene pair.
The homozygous recessive condition masks the effect of a
dominant allele at another locus.
Genetic heterogeneity
►
The phenomenon that a single disorder may be
caused by different allelic or non-allelic mutations.
►
For example, there are mutant genes that in the
homozygous state produce profound deafness in humans.
One would expect that the children of two persons with
such hereditary deafness would be deaf. This is frequently
not the case, because the parents’ deafness is often
caused by different genes. Since the mutant genes are not
alleles, the child becomes heterozygous for the two nonallelic genes and hears normally. In other words, the two
mutant genes complement each other in the child.
So, this is another form of interaction between nonallelic
genes.
►
Genetic Heterogeneity
- definition from Online Medical Dictionary
►
The presence of apparently similar characters for
which the genetic evidence indicates that different
genes or different genetic mechanisms are involved
in different pedigrees/ the same family tree (next).
►
In clinical settings genetic heterogeneity refers to
the presence of a variety of genetic defects which
cause the same disease, often due to mutations at
different loci on the same gene, a finding common
to many human diseases including Alzheimer's
Disease, Cystic Fibrosis, and Polycystic Kidney
Disease.
The affected persons are deaf and mute
aa/ BB
Children in generation IV are normal, being in the genotype double heterozygotes: Aa/Bb
AA/ bb
Correlation
Genotype–Phenotype-Environment
Influences
Pleiotropy
►
a single gene exerts an effect on many aspects of an
individual's phenotype.
►
The phenomenon whereby a single mutation
affects several apparently unrelated aspects of
the phenotype
►
The control by a single gene of several distinct and
seemingly unrelated phenotypic effects.
Pleiotropism
►
For example in MARFAN’s SYNDROME, a mutant
gene is unable to code for production of a normal
protein, fibrillin.
►
This results in the inability to produce normal
connective tissue.
►
Individuals with Marfan syndrome tend to be tall
and thin with long legs, arms, and fingers; are
nearsighted; and the wall of their aorta is weak.
►
From this view Abraham Lincoln may have had
Marfan syndrome
What is Marfan syndrome?
Marfan syndrome is a disorder of the connective tissue.
►
Connective tissue provides strength and flexibility to structures
throughout the body such as bones, ligaments, muscles, the walls
of blood vessels, and heart valves.
►
Marfan syndrome affects most organs and tissues, especially the
skeleton, lungs, eyes, heart, and the large blood vessel that
distributes blood from the heart to the rest of the body (the
aorta).
►
The signs and symptoms of Marfan syndrome vary widely in
severity, timing of onset, and rate of progression.
►
Affected individuals often are tall and slender, have elongated
fingers and toes (arachnodactyly), and have an arm span that
exceeds their body height.
Arachnodactyly
Marfan syndrome
►
►
►
Most people with Marfan syndrome have abnormalities
of the heart and the aorta.
Leaks in valves that control blood flow through the
heart can cause shortness of breath, fatigue, and an
irregular heartbeat felt as skipped or extra beats
(palpitations).
If leakage occurs, it usually affects the mitral valve,
which connects two chambers of the heart, or the aortic
valve, which regulates blood flow from the heart into
the aorta.
►
The aorta can weaken and stretch, which may lead to a
bulge in the blood vessel wall (an aneurysm).
►
Stretching of the aorta may cause the aortic valve to
leak, which can lead to a sudden tearing of the layers in
the aorta wall (aortic dissection).
Aortic aneurysm and dissection can be life threatening.
►
What gene is related to Marfan syndrome?
►
Mutations in the FBN1 gene cause Marfan syndrome.
►
The FBN1 gene provides instructions for making a protein
called fibrillin-1.
Fibrillin-1 binds to itself and other proteins and molecules to form
threadlike filaments called microfibrils.
► Microfibrils become part of the fibers that provide strength and
flexibility to connective tissue.
► Additionally, microfibrils hold molecules called growth factors and
release them at the appropriate time to control the growth and
repair of tissues and organs throughout the body.
►
►
A mutation in the FBN1 gene can reduce the amount and/or
quality of fibrillin-1 that is available to form microfibrils.
►
As a result, growth factors are released inappropriately, causing
the characteristic features of Marfan syndrome.
Because FBN 1 is active in many cells of the
body, the syndrome associates abnormalities
in different organs.
Bone
anomalies
Heart valve anomaly
dislocated lens
Aortic dissection death
Marfan syndrome
► This
condition is inherited in an
autosomal dominant pattern, which
means one copy of the altered gene in
each cell is sufficient to cause the
disorder.
► At least 25 percent of classic Marfan
syndrome cases result from a new
mutation in the FBN1 gene. These
cases occur in people with no history
of the disorder in their family.
► Beside pleiotropy the syndrome also
shows variable expressivity in families.
What ever you want to do……stop it!
Learn or at least remember that