* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Assist professor Hayder M. Alkuraishy PROKINETIC and
Survey
Document related concepts
Atypical antipsychotic wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Gastrointestinal tract wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Toxicodynamics wikipedia , lookup
NMDA receptor wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
Transcript
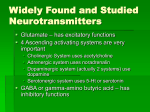
Assist professor Hayder M. Alkuraishy PROKINETIC and ANTIEMETIC AGENTS Gastrokinetic, or prokinetic, is a type of drug which enhances gastrointestinal motility by increasing the frequency of contractions in the small intestine or making them stronger, but without disrupting their rhythm. They are used to relieve gastrointestinal symptoms such as abdominal discomfort, bloating, constipation, heart burn, nausea, and vomiting. They are used to treat a number of gastrointestinal disorders, including irritable bowel syndrome, gastritis, acid reflux disease, gastroparesis, and functional dyspepsia. Activation of a wide range of serotonin receptors by serotonin itself or by certain prokinetic drugs results in enhanced gastrointestinal motility. Other prokinetic drugs may increase acetylcholine concentrations by stimulating the M1 receptor which causes acetylcholine release, or by inhibiting the enzyme acetylcholinesterase which metabolizes acetylcholine. Higher acetylcholine levels increase gastrointestinal peristalsis and further increase pressure on the lower esophageal sphincter, thereby stimulating gastrointestinal motility, accelerating gastric emptying, and improving gastro-duodenal coordination. The 5-HT4 receptor is thought to play a significant role in both the physiology and pathophysiology of GI tract motility. Therefore, 5-HT4 receptors have been identified as potential therapeutic targets for diseases related to GI dysmotility such as chronic constipation. Some of these prokinetic agents, such as mosapride and cisapride, have only moderate affinity for 5HT4 receptors. Prucalopride, is a selective, high affinity serotonin (5-HT4) receptor agonist that stimulates colonic mass movements, which provide the main propulsive force to defecation. SSRIs have been found to have prokinetic actions on the small intestine. Other molecules, including macrolides such as mitemcinal and erythromycin, have affinity for the motilin receptor where they act as agonists resulting in prokinetic properties. PROKINETIC AGENTS Cholinergic Agents CHOLINE DERIVATIVES ACh itself is not used pharmacologically because it affects all classes of cholinergic receptors (nicotinic and muscarinic;) and is degraded rapidly by acetylcholinesterase. Modification of the ACh structure has yielded drugs such as bethanechol that have increased receptor selectivity and that resist enzymatic hydrolysis. In addition to its lack of real prokinetic efficacy, bethanechol has significant side effects resulting from its broad muscarinic effects on contractility and secretion in the GI tract and other organs, including bradycardia, flushing, diarrhea and cramps, salivation, and blurred vision. ACETYLCHOLINESTERASE INHIBITORS These drugs inhibit the degradation of ACh by its esterase thereby allowing ACh to accumulate at sites of release. Unlike muscarinic receptor agonists, these parasympathomimetic drugs do not stimulate muscle directly, but rather accelerate GI transit times by enhancing the contractile effects of ACh released at synaptic and neuromuscular junctions. Among these cholinergic muscle stimulants, neostigmine has been used off-label for some GI disorders, particularly those associated with acute colonic pseudo-obstruction (Ogilvie’s syndrome) and paralytic ileus. Dopamine Receptor Antagonists Dopamine is present in significant amounts in the GI tract and has several inhibitory effects on motility, including reduction of lower esophageal sphincter and intragastric pressures. These effects, which apparently result from suppression of ACh release from myenteric motor neurons, are mediated by D2 receptors. By antagonizing the inhibitory effect of dopamine on myenteric motor neurons, dopamine receptor antagonists are effective as prokinetic agents; they have the additional advantage of relieving 1 nausea and vomiting by antagonism of dopamine receptors in the chemoreceptor trigger zone . Examples of such agents are metoclopramide and domperidone. METOCLOPRAMIDE The mechanisms of action of metoclopramide involve Peripheral 5-HT4 receptor agonist vagal and central 5-HT3 antagonism Sensitization of muscarinic receptors on GIT smooth muscle Dopamine receptor antagonism. Metoclopramide, one of the oldest true prokinetic agents, stimulates coordinated contractions that enhance transit. Its effects are confined largely to the upper digestive tract, where it increases lower esophageal sphincter tone and stimulates antral and small intestinal contractions. Metoclopramide has no clinically significant effects on large-bowel motility. Metoclopramide is indicated for Symptomatic patients with gastroparesis As an adjunctive measure in medical or diagnostic procedures such as intestinal intubation or contrast radiography of the GI tract Postoperative ileus Nausea and vomiting that often accompany GI dysmotility syndromes Metoclopramide is absorbed rapidly after oral ingestion, undergoes sulfation and glucuronide conjugation by the liver, and is excreted principally in the urine, with a t1/2 of 4–6 hours. Peak concentrations occur within 1 hour after a single oral dose; the duration of action is 1–2 hours. Metoclopramide is available for oral and parenteral use. The usual initial oral dose range is 10 mg, 30 minutes before each meal and at bedtime. The onset of action is within 30–60 minutes after an oral dose. In patients with severe nausea, an initial dose of 10 mg can be given intramuscularly (onset of action 10–15 minutes) or intravenously (onset of action 1–3 minutes). The usual pediatric dose for gastroparesis is 0.1–0.2 mg/kg of body weight per dose, given 30 minutes before meals and at bedtime. Adverse Effects The major side effects of metoclopramide include extrapyramidal effects. Dystonias, usually occurring acutely after intravenous administration, and parkinsonian-like symptoms that may occur several weeks after initiation of therapy generally respond to treatment with anticholinergic or antihistaminic drugs and are reversible upon metoclopramide discontinuation. Tardive dyskinesia also can occur with chronic treatment (months to years) and may be irreversible. Metoclopramide can elevate prolactin levels by blocking the inhibitory effect of dopamine on pituitary lactotropes. Methemoglobinemia has been reported in premature and full-term neonates receiving metoclopramide. Domperidone; D2 Receptor Antagonists domperidone predominantly antagonizes the dopamine D2 receptor without major involvement of other receptors and has modest prokinetic activity in doses of 10–20 mg three times a day. Although it does not readily cross the blood–brain barrier to cause extrapyramidal side effects, domperidone exerts effects in the parts of the CNS that lack this barrier, such as those regulating emesis, temperature, and prolactin release. 5-HT Receptor Modulators 5-HT plays an important role in the normal motor and secretory function of the gut . Indeed, >90% of the total 5-HT in the body exists in the GI tract. The enterochromaffin cell, a specialized cell lining the mucosa of the gut, produces most of this 5-HT and rapidly releases 5-HT in response to chemical and mechanical stimulation (e.g., food boluses; noxious agents such as cisplatin; certain microbial toxins; adrenergic, cholinergic, and purinergic receptor agonists). 5-HT triggers the peristaltic reflex by stimulating intrinsic sensory neurons in the myenteric plexus (via variant 5-HT receptors, 5-HT1p, and 2 via 5-HT4 receptors), as well as extrinsic vagal and spinal sensory neurons (via 5-HT3 receptors). Additionally, stimulation of submucosal intrinsic afferent neurons activates secretomotor reflexes resulting in epithelial secretion. 5-HT receptors also are found on other neurons in the ENS, where they can be either stimulatory (5-HT3 and 5-HT4) or inhibitory (5-HT1a). In addition, serotonin also stimulates the release of other neurotransmitters, depending upon the receptor subtype. Thus, 5-HT1 stimulation of the gastric fundus results in release of nitric oxide and reduces smooth muscle tone. 5-HT4 stimulation of excitatory motor neurons enhances ACh release at the neuromuscular junction, and both 5-HT3 and 5-HT4 receptors facilitate interneuronal signaling. Developmentally, 5-HT acts as a neurotrophic factor for enteric neurons via the 5-HT2B and 5-HT3 receptors. Reuptake of serotonin by enteric neurons and epithelium is mediated by the same mechanism as 5-HT reuptake by serotonergic neurons in the CNS. This reuptake therefore also is blocked by selective serotonin reuptake inhibitors which explain the common side effect of diarrhea that accompanies the use of these agents. TEGASEROD Tegaserod is structurally related to serotonin and is a partial 5-HT4 agonist with negligible affinity for other receptor subtypes. It stimulates motility and accelerates transit in the esophagus, stomach, small bowel, and ascending colon. It also stimulates chloride secretion. The clinical efficacy of tegaserod has been shown for male and female patients with constipation-predominant irritable bowel syndrome. In patients with constipation, tegaserod results in mild-to-modest improvement in stool frequency, with less consistent effects on other parameters such as stool form, bloating, and pain. The absolute improvement is modest at best. It is not clear that the drug has any greater efficacy in this regard than other agents used for constipation. MOTILIN AGONISTS: MACROLIDES AND ERYTHROMYCIN Motilin, a peptide hormone found in the GI M cells and some enterochromaffin cells of the upper small bowel, is a potent contractile agent of the upper GI tract. The effects of motilin can be mimicked by erythromycin and by other macrolide antibiotics including oleandomycin, azithromycin, and clarithromycin. THERAPEUTIC USE The best-established use of erythromycin as a prokinetic agent is in patients with diabetic gastroparesis, where erythromycin can improve gastric emptying in the short term. Erythromycin stimulated gastric contractions can be intense and result in “dumping” of relatively undigested food into the small bowel. This potential disadvantage is exploited clinically to clear the stomach of undigestible residue such as plastic tubes or bezoars. Rapid development of tolerance to erythromycin, possibly by down-regulation of the motilin receptor, and undesirable antibiotic effects have limited the use of this drug as a prokinetic agent. A standard dose of erythromycin for gastric stimulation is 3 mg/kg intravenously or 200–250 mg orally every 8 hours. For small-bowel stimulation, a smaller dose (e.g., 40 mg intravenously) may be more useful, as higher doses may actually retard small-bowel motility. Other prokinetics The GI hormone cholecystokinin (CCK) is released from the intestine in response to meals and delays gastric emptying. Dexloxiglumide is a CCK1 (or CCK-A)–receptor antagonist that can improve gastric emptying and is being investigated as a treatment for gastroparesis and constipation-dominant irritable bowel syndrome. Clonidine also may be of benefit in patients with gastroparesis. Octreotide acetate , a somatostatin analog, also is used in some patients with intestinal dysmotility . Vomiting Vomiting can be caused by a wide variety of conditions; it may present as a specific response to ailments like gastritis or poisoning, or as a non-specific sequela of disorders ranging from brain tumors and elevated intracranial pressure to overexposure to ionizing radiation. The feeling that one is about to vomit 3 is called nausea, which often precedes, but does not always lead to, vomiting. Vomiting is different from regurgitation, although the two terms are often used interchangeably. Regurgitation is the return of undigested food back up the esophagus to the mouth, without the force and displeasure associated with vomiting. The causes of vomiting and regurgitation are generally different. Mechanisms of vomiting Two brainstem sites have key roles in the vomiting reflex pathway. The chemoreceptor trigger zone is located in the area postrema (a circumventricular structure at the caudal end of the fourth ventricle). It is outside the blood-brain barrier, thus, it can respond directly to chemical stimuli in the blood or cerebrospinal fluid. The second important site, the vomiting center, which is located in the lateral reticular formation of the medulla, coordinates the motor mechanisms of vomiting. The vomiting center also responds to afferent input from the vestibular system, the periphery (pharynx and gastrointestinal tract), and higher brainstem and cortical structures. The vestibular system functions mainly in motion sickness. Chemotherapeutic agents (or their metabolites) can directly activate the medullary chemoreceptor trigger zone, or vomiting center. Several neuroreceptors, including dopamine receptor Type 2 and serotonin Type 3 (5-HT3), play critical roles. Often, the color or smell of chemotherapeutic drugs (and even stimuli associated with chemotherapy, such as cues in the treatment room or the physician or nurse who administers the therapy) can activate higher brain centers and trigger emesis. Chemotherapeutic drugs can also act peripherally by causing cell damage in the GI tract and releasing serotonin from the enterochromaffin cells of the small intestinal mucosa. The released serotonin activates 5-HT3 receptors on vagal and splanchnic afferent fibers, which then carry sensory signals to the medulla, leading to the emetic response. 4 Antiemetic drugs Phenothiazines: The first group of drugs shown to be effective antiemetic agents, phenothiazines, such as prochlorperazine act by blocking dopamine receptors. Prochlorperazine is effective against low or moderately emetogenic chemotherapeutic agents. Although increasing the dose improves antiemetic activity, side effects, including hypotension and restlessness, are dose limiting. Other adverse reactions include extrapyramidal symptoms and sedation. 5-HT3 receptor blockers: The specific antagonists of the 5-HT3 receptor ondansetron, granisetron, palonosetron, and dolasetron selectively block 5-HT3 receptors in the periphery (visceral vagal afferent fibers) and in the brain (chemoreceptor trigger zone). These drugs can be administered as a single dose prior to chemotherapy (intravenously or orally) and are efficacious against all grades of emetogenic therapy. Headache is a common side effect. Electrocardiographic changes, such as a prolonged QT interval, can occur with dolasetron. Patients who may be at risk should take this medication with caution. Substituted benzamides: metoclopramide is effective at high doses against the emetogenic cisplatin, preventing emesis in 30 to 40 percent of patients and reducing emesis in the majority. Antidopaminergic side effects, including sedation, diarrhea, and extrapyramidal symptoms, limit its high-dose use. It is commonly used as a prokinetic drug. Butyrophenones: Droperidol and haloperidol act by blocking dopamine receptors. Droperidol had been used most often for sedation in endoscopy and surgery, usually in combination with opiates or benzodiazepines. However, it may prolong the QT interval, and current practice reserves it for patients whose response to other agents is inadequate. High-dose haloperidol was found to be nearly as effective as high-dose metoclopramide in preventing cisplatin-induced emesis. Benzodiazepines: The antiemetic potency of lorazepam and alprazolam is low. Their beneficial effects may be due to their sedative, anxiolytic, and amnesic properties. 5 Corticosteroids: Dexamethasone and methylprednisolone used alone, are effective against mildly to moderately emetogenic chemotherapy. Most frequently, however, they are used in combination with other agents. Their antiemetic mechanism is not known, but it may involve blockade of prostaglandins. Substance P/neurokinin-1 receptor blocker: Aprepitant belongs to a new family of antiemetic agents. It targets the neurokinin receptor in the brain and blocks the actions of the natural substance. Aprepitant is usually administered orally with dexamethasone and palonosetron. It undergoes extensive metabolism, primarily by CYP3A4. As would be expected, it may affect the metabolism of other drugs that are metabolized by this enzyme. Aprepitant can also induce CYP3A4 and thereby affect its response to other agents. For example, concomitant use with warfarin can shorten the half-life of the anticoagulant. Constipation and fatigue appear to be the major side effects. Aprepitant is only indicated for highly or moderately emetogenic chemotherapy regimens. Note: Antiemetic drugs are often combined to increase antiemetic activity or decrease toxicity. Corticosteroids, most commonly dexamethasone, increase antiemetic activity when given with high-dose metoclopramide, a 5-HT3 antagonist, phenothiazine, butyrophenone, or a benzodiazepine. Antihistamines, such as diphenhydramine, are often administered in combination with high-dose metoclopramide to reduce extrapyramidal reactions or with corticosteroids to counter metoclopramide induced diarrhea. 6