* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Blood – Part 2 - Mount Carmel Academy
Cell encapsulation wikipedia , lookup
Endomembrane system wikipedia , lookup
Cell growth wikipedia , lookup
Extracellular matrix wikipedia , lookup
Cellular differentiation wikipedia , lookup
Cytokinesis wikipedia , lookup
Cell culture wikipedia , lookup
Tissue engineering wikipedia , lookup
Cytoplasmic streaming wikipedia , lookup
List of types of proteins wikipedia , lookup
Hematopoietic stem cell transplantation wikipedia , lookup
Cell nucleus wikipedia , lookup
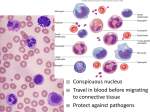
WBCs are classified into two major groups, depending on whether or not they contain visible granules in their cytoplasm. 1. Granulocytes – Granule containing WBCs. 2. Agranulocytes – Lack visible cytoplasmic granules. Granulocytes – Granule containing WBCs. › Have lobed nuclei Typically consist of several rounded nuclear areas connected by thin strands of nuclear material. › The granules in their cytoplasm stain specifically with Wright’s stain. › Granulocytes include the: 1. Neutrophils 2. Eosinophils 3. Basophils Multilobed nucleus. Very fine granules that respond to both acid and basic stains. The cytoplasm as a whole stains pink. Avid phagocytes at sites of acute infection. Blue-red nucleus. › Resembles an old fashioned telephone receiver. Large brick-red cytoplasmic granules. Their number increases rapidly during allergies and infections by parasitic worms (ex: tapeworms and flatworms) Rarest of the WBCs. Contain large histaminecontaining granules that stain dark blue. › Histamine – Inflammatory chemical that makes blood vessels leaky and attracts other WBCs to the inflammatory site. Agranulocytes – lack visible cytoplasmic granules. › Their nuclei is closer to the norm – that is spherical, oval, or kidney shaped. › The agranulocytes include: 1. Lymphocytes 2. Monocytes Have a large, dark purple nucleus that occupies most of the cell volume. Slightly larger than RBCs. Tend to take up residence in lymphatic tissues, where they play an important role in the immune response. Largest of the WBCs. Except for their more abundant cytoplasm and indented nucleus, they resemble large lymphocytes. When they migrate into the tissues, they change into macrophages with huge appetites. Macrophages are very important in fighting chronic infections. Platelets – One of the irregular cell fragments of blood. › Not cells in the strict sense; They are fragments of bizarre multinucleate cells called megakaryocytes. Megakaryocytes rupture releasing thousands of anucleate “pieces” that quickly seal themselves off from the surrounding fluids. Appear as darkly staining, irregularly shaped bodies scattered among the other blood cells. Needed for the clotting process. Hematopoiesis – Blood cell formation. › Occurs in red bone marrow. This tissue is found chiefly in the: 1. 2. 3. 4. Flat bones of the skull and pelvis Ribs Sternum Proximal epiphyses of the humerus and femur › After the cells mature, they are discharged into the blood vessels surrounding the area. All the formed elements arise from a common type of stem cell, the hemocytoblast. › Hemocytoblasts resides in the bone marrow. › Their development differs and once a cell is committed to a specific blood pathway it cannot change. Because they are anucleate, RBCs are unable to synthesize proteins, grow, or divide. As they age, RBCs become more rigid and begin to fragment, or fall apart in 100-120 days. Their remains are eliminated by phagocytes in the liver, spleen, and other body tissues. Lost cells are replaced by the division of hemocytoblasts. The developing RBCs divide many times and then begin synthesizing huge amounts of Hb. › When enough Hb has been accumulated, the nucleus and most organelles are ejected and the cell collapses inward. The entire developmental process from hemocytoblast to mature RBC takes 3-5 days. The rate of erythrocyte production is controlled by a hormone called erythropoietin. › Normally a small amount of erythropoietin circulates in the blood at all times, and RBC are formed at a fairly constant rate. › The kidneys play the major role in producing this hormone. If blood levels of O2 begin to decline, the kidneys step up their release of erythropoietin. An excessive amount of O2 in the bloodstream, depresses erythropoietin release. The formation of leukocytes is stimulated by two hormones: 1. Colony Stimulating Factors (CSFs) 2. Interleukins The production of platelets is accelerated by the hormone thrombopoietin.