* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Biochemistry Study Guide NITROGEN METABOLISM
Nicotinamide adenine dinucleotide wikipedia , lookup
Point mutation wikipedia , lookup
Microbial metabolism wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Oligonucleotide synthesis wikipedia , lookup
Catalytic triad wikipedia , lookup
Proteolysis wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Butyric acid wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Genetic code wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Peptide synthesis wikipedia , lookup
Metalloprotein wikipedia , lookup
Citric acid cycle wikipedia , lookup
Biochemistry wikipedia , lookup
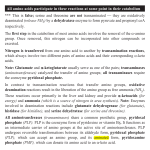
Biochemistry Study Guide NITROGEN METABOLISM PROSTAGLANDINS SYNTHESES OF PROSTAGLANDINS: O2 is required for synthesis. Phospholipase-A2 catalyzes Linolenic (Linoleic) Acid ------> Arachidonic Acid. This is the rate-limiting step in Prostaglandin Synthesis. Prostaglandin H Synthase: Arachidonic Acid ------> Prostaglandin-H2 (PGH2) O2 is required for synthesis at this step, too. End Products from PGH2: Prostacyclin Thromboxane Other Prostaglandins SYNTHESIS OF LEUKOTRIENES: Leukotrienes found only in monocytes, neutrophils, macrophages, and beta-lymphocytes. O2 is required for synthesis. 5-Lipoxygenase: Arachidonic Acid ------> Leukotriene-A4 (LTA4) EICOSANOID STRUCTURE: All contain 20 carbon atoms All contain additional oxygen atoms. Names are based on the type of ring-structure formed. Numerical subscripts refer to the parent fatty acid. PLATELET AGGREGATION: Prostacyclin PGI2 inhibits it. It is made in the vascular endothelium. Thromboxane TXA2 promotes it. It is made in the platelets. If / when the platelets are killed, this promotion of clotting is disposed of, at least temporarily. ASTHMA: Leukotrienes may play a role in asthma, in eliciting an a release of mucous from neutrophils in the lungs. THE INFLAMMATORY RESPONSE: Platelets adhere to damages cellular surfaces and eject their granules into the extracellular space. More platelets flock to the region causing swelling. Platelet Activating Factor promotes further aggregation. Mediators hormonally control and promote the inflammatory response. There are many mediators (histamines, prostaglandins, leukotrienes) specific to a tissue or circumstance. SYMPTOMS of Inflammation: Erythema = prolonged period of vasodilation. Edema = swelling of extracellular tissue, resulting increased permeability of vascular tissues. 1 Hyperalgesia = pain. Fever ASTHMA is a chronic inflammatory disease. Treated with Steroidal Anti-Inflammatory as an inhaler. RHEUMATOID ARTHRITIS is a chronic inflammatory disease. Treated with Aspirin as an anti-inflammatory. STEROIDAL ANTI-INFLAMMATORIES: Cortisol is a very strong anti-inflammatory. It probably acts by disrupting the action of Phospholipase A2. NON-STEROIDAL ANTI-INFLAMMATORIES (NSAID's): They inhibit the enzyme Prostaglandin-H Synthetase in the tissues of the inflamed site. This results in a block of the conversion of arachidonic acid into prostaglandins, thereby shunting them to leukotrienes. Aspirin, Acetylsalicylic Acid: Inhibits the Cyclooxygenase activity of PGH-Synthase (PGHS) by acetylating a unique Serine residue IRREVERSIBLY. The only way to get more PGH-synthesis from these tissues is to make more of the cyclooxygenase enzyme de novo. Thus aspirin is an effector inhibitor. SIDE-EFFECT = aspirin will also block prostaglandin-mediated secretion of mucous membrane in the intestinal wall, which can result in damage to intestinal epithelia. Other NSAID's are REVERSIBLE. ACETAMINOPHEN: A good anti-pyretic and analgesic, but not shown to be a good antiinflammatory per se. ALCOHOLISM METABOLISM OF ETHANOL: The ultimate product of alcohol metabolism is Acetyl-CoA. Alcohol Dehydrogenase: Ethanol + NAD+ ------> Acetaldehyde + NADH This action requires Zn+2 OR, at the same time you can do it with Cytochrome P450, utilizing NADPH. Acetaldehyde Dehydrogenase: Acetaldehyde + NAD+ ------> Acetate + NADH Acetate + ATP + Coenzyme-A ------> Acetyl-CoA PROLIFERATION OF SMOOTH ER: Increased Cytochrome-P450 in microsomes from chronic alcohol consumption is associated with a proliferation of smooth endoplasmic reticulum. ALCOHOL EFFECT ON TISSUES: Elevated EtOH can lead to uncontrolled uptake of fatty acids in cells, as the fatty acids can esterify to the ethanol for uptake. Increased NADH from Alcohol Dehydrogenase ------> Increased NADH/NAD+ ratio ------> Increased levels of Lactate in the blood INTERFERENCE WITH LIVER DETOXIFICATION: Lots of alcohol can interfere with the conjugation of bilirubin in the liver to bilirubin diglucuronide. EtOH ------> Lower levels of Direct Bilirubin, which is conjugated water-soluble bilirubin in the blood. EtOH ------> Higher levels of Indirect Bilirubin, which is unconjugated bilirubin stuck 2 to albumin. This interference with detoxification leads to fibrotic liver with fatty deposits. You will also see marked proliferation of smooth-ER prior to this. ETHANOL AND OTHER DRUGS: ACUTE Consumption: Ethanol may increase the effects of other drugs by interfering with their metabolism in the liver, thereby increasing their effects. Barbiturates have a dangerous effect with alcohol because their half-life is increased in the presence of alcohol. The synergistic effect of both EtOH + Barbiturates together is to induce sleep. CHRONIC alcohol effect may actually decrease the effects of other drugs. Can be seen in acetaminophen toxicity which can lead to hepatic necrosis. PROTEOLYTIC DIGESTION and ABSORPTION OF PROTEINS PEPSIN: Proteolytic digestive enzyme. Pepsinogen is converted to Pepsin by the action of acid (H+). The acid is secreted by parietal cells in the intestinal wall. The parietal cells secrete acid whenever food enters the stomach from the esophagus. Auto-Catalytic: Active pepsin acts on pepsinogen to create more of itself. CLEAVAGE-SPECIFICITY: Pepsin is specific to non-polar amino acids that are adjacent to Phenylalanine, Tyrosine, or Leucine. It cleaves at the carboxyl group adjacent to those residues. Pepsin function at an acidic pH -- it uses an interesting catalytic mechanism of interacting carboxyl groups. The active site is only operational at a pH around 2. THE ENDOPEPTIDASES: Peptidases that cleave peptides within TRYPSIN: It is a Serine-Protease, i.e. it uses Serine as its active site to cleave proteins. Trypsin is activated by ENTEROKINASE, which is secreted in the intestinal mucosa. It converts Trypsinogen ------> Trypsin CLEAVAGE-SPECIFICITY: Trypsin cuts amino acids that are adjacent to Lysine and Arginine. Auto-Catalytic: Activated trypsin acts on trypsinogen to make more of itself. Trypsin also acts on Chymotrypsinogen to make Chymotrypsin! CHYMOTRYPSIN: Chymotrypsinogen is activated by Trypsin. CLEAVAGE-SPECIFICITY: It cleaves aromatic and non-polar side-chains. It is not as specific in its cleavage site as Trypsin. It will cleave any of the following residues: Trp, Phe, Tyr, Met, Leu 3 ELASTASE: Elastase is activated by Trypsin, too. It converts Proelastase ------> Elastase CLEAVAGE-SPECIFICITY: It cleaves residues adjacent to Alanine, Glycine, and Serine residues. THE EXOPEPTIDASES: Cut the very last residue off a protein. Generally work on smaller polypeptides after they have been broken down a bit by the endopeptidases. CARBOXYPEPTIDASE: These are exopeptidases that cleave at the carboxy-end. They are both activated by Trypsin just like above: Procarboxypeptidase ------> Carboxypeptidase They are both metalloproteases which require Zinc for catalysis. This is a different mechanism than the endopeptidases which are serine proteases. These guys are secreted in the pancreas. Carboxypeptidase-A: Cleaves neutral and acidic side-chains (on the carboxy end), such as Alanine, Valine, Isoleucine, Leucine. Carboxypeptidase-B: Cleaves basic residues -- Lysine, Arginine Every time Trypsin cuts a protein, you are left with a protein piece that has either Lys or Arg at the carboxy-end! Carboxypeptidase can then take over to remove that end-piece. This in effect gives us a free amino acid of Lysine or Arginine which can then be absorbed. AMINOPEPTIDASE: Exopeptidases that cut at the amino end of a peptide. This is secreted by the intestinal mucosa further along the small intestine (jejunum). This is a metalloprotease that requires Zinc and Manganese for catalysis. This cuts, usually on smaller peptides, one acid at a time off the amino end. DIPEPTIDASE: An Aminopeptidase, similar to above, which cuts two acids at a time from the amino end of a peptide. At this point, the peptides are small enough (two or three residues max) that they can be absorbed by small intestine and go, through portal circulation, to liver. SECRETAGOGUES: They stimulate the pancreas to release pancreatic enzymes. They have specific receptors on the pancreatic acinar (exocrine) cells. CHOLECYSTOKININ: Stimulates the alpha-Adrenergic Phosphatidylinositol intracellular pathway in Pancreatic acinar cells. Acetylcholine has the same effect on these cells, through the same pathway, via neural stimulation. Has a sulfonated tyrosine side-chain. SECRETIN: Stimulates the beta-Adrenergic Adenylate Cyclase (cAMP) intracellular pathway Between the two above, there is dual stimulation on the pancreatic acinar cells to cause them to secrete pancreatic enzyme. GASTRIN: Has a sulfonated tyrosine side-chain. OVERALL ACTIVATION-SCHEME OF INTESTINAL PEPTIDASES: Food enters stomach, activating parietal cells to secrete HCl 4 HCl (i.e. low pH) causes the following: Pepsinogen ------> Pepsin, which is also auto-catalytic. Gastrin is released Histamine is released When food reaches small intestine, small intestine releases two secretagogues: Cholecystokinin Secretin The Secretagogues cause the following: Pancreatic secretion of Trypsinogen, Chymotrypsinogen, and Proelastase. Intestinal epithelial secretion of Enteropeptidase Enteropeptidase causes Trypsinogen ------> Trypsin, which is also auto-catalytic. Trypsin causes: Chymotrypsinogen ------> Chymotrypsin Proelastase ------> Elastase Procarboxypeptidases ------> Carboxypeptidases SYNTHESIS OF ACTIVE SULFATES: Sulfonation is the process of adding a sulfate to a substance, such as a hormone or drug. In the case of drugs, it makes more soluble so it can be excreted in the urine. First, the sulfate group must be activated. ATP-Sulfurase: SO3-2 + ATP ------> Adenosine-5-Phosphosulfate (AMPS) This reaction releases pyrophosphate, and a pyrophosphatase is used to cleave the high energy and drive the reaction right. AMPS-Phosphokinase: Adenosine-5-Phosphosulfate ------> 3-Phosphoadenosine-5Phosphosulfate (PAPS) Mg+2, ATP required here. PAPS is then the active sulfate, which can be transferred to hydroxyl groups to exert various chemical effects. TOTAL ENERGY REQUIRED: 3 ATP 2 ATP equivalent from release and cleavage of pyrophosphate in step 1 1 ATP required in step two. PROTEIN TURNOVER: Degrading proteins in the cell and then rebuilding them. Cathepsins: A class of acidic LYSOSOMAL degradative enzymes that function optimally at acidic pH. Lysosomes normally act on proteins that are taken up by receptor mediated endocytosis. Calpains: A class of neutral NON-LYSOSOMAL (CYTOSOLIC) degradative enzymes that function optimally at physiological pH. Many of them are metalloproteases, metal-requiring. Ubiquitin: This tagging-ligand is often added to the proteins that are destined (doomed) for degradation by calpains. Proteins must be tagged for degradation, so that the Calpains don't attack just any old protein in the cytosol! Attachment of Ubiquitin requires ATP. Ubiquitin almost invariably attaches to Lysine residues, but it is not clear how it knows which proteins to tag on to or what role the Lys residues might play. 5 Proteosome Complex: The ubiquitin-tagged proteins are broken down in very large proteosome complexes (presumably these are the Calpains). PROTEIN SYMPORT: Facilitated transport of amino acids is one of two ways that amino acids can get into cells. The other way is via glutathione. Amino Acid comes in as a symport with Na+, with Na+ flowing with its concentration gradient. So, this transport itself does not require energy. Na+ gradient is usually created by a Na+/K+ ATPase pump, which does require energy. Every ATP yields 3Na+ pumped and 2K+ pumped in. The above creates a net negative charge inside the cell, causing Na+ to come back in by facilitated diffusion. There are multiple types of these symport-mechanisms. Different ports were discovered by protein-saturation experiments and by their deficiency in disease states. General Port: Transports neutral amino acids and Citrulline Dibasic Port: Transports basic amino acids Dicarboxylic Port: Transports acidic amino acids Glycine / Imino Port: Transports Gly, Pro, Hydroxyproline GLUTATHIONE: gamma-Glutamylcysteinylglycine. It is a tripeptide that aids in protein transport and is essential to RBC-membrane integrity. Structure and Prevalence: Glutathione is a tripeptide of Glu-Cys-Gly Oxidation States: Glutathione comes in reduced and oxidized states. Reduced Form: Abbreviated GSH, to indicate the thiol group on cysteine. Oxidized Form: It dimerizes to GS-SG to indicate disulfide bond. The reduced form is dominant in the cell, about 100-500x more prevalent than oxidized form. Glutathione Reductase: GS-SG ------> GSH. This reaction requires NADPH. Overall prevalence of Glutathione in cell: 5mM. Very prevalent! Cellular Roles of Glutathione: Amino Acid Transport (see below) Peroxide detoxification Methemoglobin Reduction: Glutathione keeps iron in its ferrous (Fe+2) state. The ferrous state is necessary for hemoglobin to bind to oxygen. Oxidizing agents (as in aging) can cause oxidation of iron to ferric oxidation state. Protein Folding: It aids by providing a means for exchanging disulfide bonds during protein folding. Prostaglandin and Leukotriene Synthesis GLUTATHIONE-TRANSPORT OF AMINO ACIDS: OUTSIDE CELL: A free amino acid is "glutamylated" from glutathione, so that it can go through a specific receptor to get through membrane. Free Amino Acid + Glutathione ------> gamma-Glutamyl Amino Acid + Cysteinyl-Glycine TRANSPORT: The gamma-Glutamyl amino acid goes through a glutamine-specific transport 6 protein to get through the membrane. The Cysteinyl-Glycine gets through the membrane INSIDE CELL: The acid is freed, and glutathione is resynthesized. gamma-Glutamyl Amino Acid ------> Free Amino Acid + 5-Oxoproline 5-Oxoproline ------> Glutamic Acid This is the opening of a ring to form free Glutamate ATP is required. Cysteinyl-Glycine ------> Cysteine + Glycine: Cys and Gly are split apart so that can be used in the resynthesis of glutathione. Cysteine + Glycine + Glutamate ------> Glutathione 2 ATP are required, to synthesize the two peptide bonds. OVERALL ENERGETICS: 3 ATP are required per amino acid transported via Glutathione. 1 ATP for opening of the 5-Oxoproline ring 2 ATP for forming the peptide bonds to resynthesize glutathione. TRANSAMINATION AND GLUTAMATE DEHYDROGENASE PYRIDOXAL PHOSPHATE: Pyridoxal phosphate acts as the intermediate in a number of reactions, by forming schiff bases, which involves the condensation (i.e. loss of water) of an aldehyde function with an amino group, to yield a C=NR structure. Transamination Decarboxylation of histidine Aldol Cleavage of Fructose Biphosphate (aldolase) Elimination of beta-carbons in Ser and Thr Dehydratases OXIDATIVE DEAMINATION via GLUTAMATE DEHYDROGENASE CYCLE: A way to take the amino group from an amino acid and transfer it to another carbon skeleton, in order to (1) get rid of the amino group, or (2) create a different amino acid. Amino Acid + alpha-Ketoglutarate ------> Keto Acid + Glutamate This is catalyzed by Aminotransferase. It is simply the "swapping" of an amino group for a keto group, between many different amino acids and alpha-Ketoglutarate: Glutamate serves as a carrier of nitrogen of here. Hence alpha-Ketoglutarate is often used for this aminotransferase reaction. This reaction is reversible Pyridoxyl Phosphate is required as an intermediate. Transamination is achieved via Schiff base. Glutamate ------> alpha-Ketoglutarate + NH3 NAD+ is required. This reaction is an oxidation; NAD+ ------> NADH is concurrent reduction. The NADH can then be used in electron transport. This reaction is catalyzed by Glutamate Dehydrogenase. 7 The free ammonia will then must be taken up by some other reaction, such as urea synthesis. alpha-Ketoglutarate is most commonly used in aminotransferase reactions, because Glutamate Dehydrogenase is available to regenerate the reactant and make it a cycle. However, other keto acids may also be used. OVERALL CYCLE: Two cofactors are required: Pyridoxal Phosphate and NAD+ (but no ATP!) For every turn of the cycle, we have Aminotransferase: alpha-amino acid ------> alpha-keto acid alpha-Ketoglutarate ------> Glutamate Glutamate Dehydrogenase: Glutamate ------> alpha-ketoglutarate NADH produced NH3 produced Clinical Significance: Historically, aminotransferase levels were measured in the blood to diagnose myocardial infarction. REVERSIBLE: Glutamate Dehydrogenase is completely reversible. Because it is reversible, you can transaminate free ammonia to other carbon skeletons to make other amino acids. Although the reverse reaction uses free ammonia, it is not an important source of ammonia disposal. NON-OXIDATIVE DEAMINATION: SERINE AND THREONINE can be deaminated nonoxidatively (i.e. no NAD+ is required). Enzyme = Serine-Threonine Dehydratase. Serine ------> Pyruvate + NH4+ Threonine ------> alpha-Ketobutyrate + NH4+ Cofactor: Pyridoxal Phosphate is required for these reactions, too, and Schiff-Base formation is involved. OTHER OXIDATIVE DEAMINATION PATHWAYS: L-Amino Acid Oxidase catalyzes Amino Acid ------> Keto Acid Concurrent reduction: FMN ------> FMNH2 FMN is regenerated from FMNH2 using O2, which forms a peroxide. The peroxide can then be reduced down to water with catalase (in peroxisomes). D-Amino Acid Oxidase only works on D-acids. So in humans it only works achiral Glycine. It is suspected that these oxidases exist as a defense mechanism against bacteria. AMMONIA TRANSPORT VIA GLUTAMATES: NH3 can be stored in glutamate or glutamine for non-toxic storage and transport. Free ammonia is not tolerated in very high concentrations. A way of carrying NH3 on a glutamine residue: Glutamine Synthetase: Glutamate + NH3 ------> Glutamine 8 Glutaminase: Glutamine ------> Glutamate + NH3 A way of carrying NH3 on a glutamate residue: Aminotransferase: alpha-Ketoglutarate + NH3 ------> Glutamate Glutamate Dehydrogenase: Glutamate ------> alpha-Ketoglutarate + NH3 Between the two above, we can carry a total of two NH3's on a glutamine residue. THE UREA CYCLE SYNTHESIS OF CARBAMOYL PHOSPHATE: This is how we "activate" a free ammonia before we subsequently make urea. Enzyme = Carbamoyl Phosphate Synthetase. This reaction occurs in the mitochondrion. 2 ATP are required. Basically these are used to "charge" or "activate" ammonia with a highenergy phosphate bond, before we subsequently start urea synthesis. N-Acetylglutamate is absolutely required as a cofactor. This compound also serves a regulatory role in urea synthesis. The rate of carbamoyl phosphate synthesis is dependent on the levels of NAcetylglutamate in the mitochondria (I'm not sure whether this is a linear relationship). Usually, the free ammonia is derived directly from Glutamate Dehydrogenase, but it could come from anywhere. THE UREA CYCLE: REQUIRED STARTING MATERIALS: Carbamoyl Phosphate: It donates a free NH3 to urea, per turn of the cycle. Ornithine: It is regenerated each turn of the cycle Aspartic Acid: It donates an NH3 to urea from aminotransferases, per turn of the cycle. Aspartic Acid has the same carbon skeleton as Oxaloacetate: 4 ATP are required per molecule of urea 2ATP required to synthesize Carbamoyl Phosphate 2ATP required to synthesize Arginosuccinate, via 1 ATP and a pyrophosphatase Carbamoyl Phosphate + Ornithine ------> Citrulline This is THE COMMITTED STEP One of the two NH3's of urea comes to us from Carbamoyl Phosphate, essentially the same as starting with a charged free NH3. This step occurs in the mitochondria. Citrulline is then transferred from mitochondria to the cytosol for the rest of the steps. Enzyme: Ornithine Transcarbamoylase 9 Citrulline + Aspartic Acid ------> Arginosuccinate ATP ------> AMP + PPi. Metabolic equivalent of 2ATP required, with pyrophosphatase driving the reaction forward, making the reaction irreversible. Aspartic Acid carries with it the other NH3 of urea. This NH3 has come to us via Aspartic Acid, courtesy of Aspartate Aminotransferase. This step, and all subsequent steps, occurs in the cytosol. Arginosuccinate ------> Arginine + Fumarate Catalyzed by Arginosuccinase Fumarate then goes through the TCA Cycle, in order to regenerate the carbon skeleton of Aspartic Acid: Fumarase: Fumarate ------> L-Malate L-Malate Dehydrogenase: L-Malate ------> Oxaloacetate Aspartate Aminotransferase: Oxaloacetate + NH3 ------> Aspartic Acid Arginine ------> Urea + Ornithine Catalyzed by Arginase. Know this enzyme, because this is the step that regenerates ornithine. END PRODUCTS: Fumarate, which is recycled, via the TCA cycle and transamination, to Aspartate Urea Ornithine, which is recycled to the first step. REGULATION OF THE UREA CYCLE: Short-Term Regulation (metabolic regulation): The primary regulated step is Carbamoyl Phosphate Synthetase. Increased levels of Arginine promotes the formation of N-Acetyl Glutamate, which is required for carbamoyl phosphate synthesis. Glutamate + Acetyl-CoA ------> N-Acetylglutamate So when Arginine levels goes up, carbamoyl phosphate is made and urea synthesis occurs. Long-Term Regulation (diet) In the long-term, a high-protein diet will increase overall levels of urea synthesis. People who are protein derived would be ill-equipped to handle a sudden massive increase in the amount of protein in their diet, because enzyme levels would not be high enough. That's why you change a diet gradually as a rule of thumb, especially for the malnourished. AMMONIA DETOXIFICATION: Ways of getting rid of excess ammonia in the bloodstream. From Benzoic Acid: HIPPURATE Benzoic Acid + Coenzyme-A ------> Benzoyl-CoA 2 ATP are required (coupled with pyrophosphatase), as usual, to make a CoA derivative. Benzoyl-CoA + Glycine ------> Hippurate Amino groups are fed in at this step, in the form of Glycine. Hippurate is innocuous and is readily excreted in the urine. 10 This form of detoxification will only work if we can transaminate an NH3 group onto glyoxalase (the keto-acid form of glycine). If we can't get the NH3 into glycine, then we can't get rid of it by this means! From Phenylacetate: PHENYLACETYLGLUTAMINE Phenylacetate + Glutamine ------> Phenylacetylglutamine Coenzyme-A is required as a cofactor, but there is no free Coenzyme-A intermediate. In other words, it is a concerted reaction. 2 ATP are required (coupled with pyrophosphatase), as usual. Phenylacetylglutamine is readily excreted in the urine. CLINICAL CASE-STUDY: HYPERAMMONEMIA The patient had a deficiency in Ornithine Transcarbamoylase. Blood-levels of NH3 were almost twice normal. The enzyme was not completely absent, however. If you gave the patient protein, it would take him 120 hours to completely metabolize the protein to urea, which is far longer than normal. CLINICAL PRESENTATION: Bizarre behavior: crying, agitation, babbling, loss of sense of reality. Lab results suggest a deficiency in ornithine transcarbamoylase: High levels of Alanine, Glutamine, and Orotic Acid (a metabolite of purine synthesis) NH3 of course was way high The Carbamoyl Phosphate builds up and must be shunted off to another pathway. TREATMENT: A high carbohydrate, low protein diet (but not no protein) Treat with benzoic acid or phenylacetate for ammonia detoxification. SYNTHESIS AND DEGRADATION OF AMINO ACIDS GLUCOGENIC: Amino acids whose degradation results in pyruvate or one of the intermediates of the TCA cycle. That means that those carbons can be used to make glucose via gluconeogenesis, under the right metabolic circumstances. KETOGENIC: Amino acids whose degradation results only in Acetyl-CoA or Acetoacetyl-CoA. These carbon-skeletons can only be funneled into fat-metabolism: aerobic respiration of acetyl-CoA, or fatsynthesis. ESSENTIAL: The amino acid is required in the diet. We can't synthesize it de novo. NON-ESSENTIAL: The amino acid can be synthesized de novo from other amino acids or from metabolic precursors. SAME CARBON SKELETONS: Each of the below have the same carbon skeletons: Glutamate, Glutamine, alpha-Ketoglutarate Aspartate, Asparagine, Oxaloacetate 11 Alanine, Pyruvate PVT TIM HALL: A mnemonic for the essential amino acids. Phe, Val, Thr // Trp, Ile, Met // His*; Arg*; Lue; Lys Amino Acid Synthesis Degradation Leucine ESSENTIAL KETOGENIC: Leucine ------> Acetyl-CoA + Acetoacetate (branched) Lysine ESSENTIAL KETOGENIC Phenylalanine ESSENTIAL -- and it's an essential precursor to Tyrosine GLUCOGENIC + KETOGENIC Tyrosine NON-ESSENTIAL: Phenylalanine ---- GLUCOGENIC + KETOGENIC --> Tyrosine (Phenylalanine Hydroxylase) Tryptophan ESSENTIAL GLUCOGENIC + KETOGENIC Isoleucine ESSENTIAL GLUCOGENIC + KETOGENIC: Isoleucine ------> Acetyl-CoA + Propionyl CoA ------> Succinyl-CoA (branched) Threonine ESSENTIAL GLUCOGENIC + KETOGENIC: Threonine ------> Propionyl-CoA -----> Succinyl-CoA (although it isn't branched) (Propionyl-CoA Carboxylase) Aspartate NON-ESSENTIAL: Oxaloacetate ------ GLUCOGENIC: Aspartate ------> > Aspartate (aminotransferase) Oxaloacetate (aminotransferase) Glutamate NON-ESSENTIAL: alphaKetoglutarate ------> Glutamate (aminotransferase) NON-ESSENTIAL: Glutamate ------> alpha-Ketoglutarate (aminotransferase) Asparagine NON-ESSENTIAL: Aspartate ------> Asparagine (Aminotransferase) GLUCOGENIC: Asparagine ------> Aspartate ------> Oxaloacetate (Asparaginase, Aminotransferase) Glutamine NON-ESSENTIAL: Glutamate ------> Glutamine (Glutamine Synthetase) GLUCOGENIC: Glutamine ------> Glutamate ------> alphaKetoglutarate (Glutaminase, Glutamate Dehydrogenase) Histidine NON-ESSENTIAL -- but it is required in infancy and during recovery from disease; Glutamate ------> 5aminoimidazole-4-carboxamide ------> GLUCOGENIC: Histidine ------> Glutamate ------> alphaKetoglutarate (bacterial, Glutamate Dehydrogenase) 12 Histidine (bacterial) Proline NON-ESSENTIAL: Glutamate ------> Proline (reduce the gamma-carboxyl group of Glutamate) GLUCOGENIC: Proline ------> Glutamate ------> alphaKetoglutarate (open ring, oxidize, Glutamate Dehydrogenase) Arginine NON-ESSENTIAL -- but it is required in infancy and during recovery from disease; Glutamate ------> Ornithine -----> Arginine (second step via Arginase) GLUCOGENIC: Arginine ------> Ornithine ------> Glutamate ------> alpha-Ketoglutarate (Arginase, Glutamate Dehydrogenase) Glycine NON-ESSENTIAL: Serine ------> Glycine (demethylation with tetrahydrofolate as cofactor) GLUCOGENIC: Glycine ------> Pyruvate Alanine NON-ESSENTIAL: Pyruvate ------> Alanine (aminotransferase) GLUCOGENIC: Alanine ------> Pyruvate (aminotransferase) Serine NON-ESSENTIAL: 3Phosphoglycerate ------> Serine GLUCOGENIC: Serine ------> Pyruvate Cysteine NON-ESSENTIAL: Methionine ------> GLUCOGENIC Homocysteine + Serine ------> Cysteine Methionine ESSENTIAL -- and, it's an essential precursor to Cysteine Valine ESSENTIAL GLUCOGENIC: Methionine ------> Propionyl-CoA ------> Succinyl-CoA (although it isn't branched) (Propionyl-CoA Carboxylase) GLUCOGENIC: Valine ------> Propionyl-CoA ------> Succinyl-CoA (branched) (Propionyl-CoA Carboxylase) ASPARAGINASE: The breakdown of asparagine to aspartate. It can be used as a treatment for Leukemia, by giving Asparaginase and thereby starving metastatic cells of their need for Asparagine. PRODUCTS OF AMINO ACID DEGRADATION: All amino acids are ultimately broken down to one of the following, as described above. Know this list: PYRUVATE ACETOACETYL-CoA ACETYL-CoA alpha-KETOGLUTARATE SUCCINYL-CoA FUMARATE OXALOACETATE DEGRADATION OF BRANCHED AMINO ACIDS: Valine, Isoleucine, Leucine. These three acids 13 are degraded by parallel mechanisms. All of the below applies to all three. Branched Amino Acid ------> alpha-Keto Acid + NH3 This is called a transamination and is catalyzed by aminotransferases The NH3 will then form Carbamoyl phosphate and go onto urea synthesis or purine synthesis. alpha-Keto Acid ------> Acyl-CoA This is an Oxidative Decarboxylation very similar to pyruvate dehydrogenase reaction. It uses the same cofactors as PDH-Dehydrogenase and Succinate Dehydrogenase: Thiamine Pyrophosphate (TPP), Lipoic Acid, NAD+, FAD, Coenzyme-A are all required. CO2 is given off; Coenzyme-A is put on; NAD+ ------> NADH is ultimately the concurrent reduction. Acyl-CoA ------> ------> End Products (Propionyl-CoA, Acetyl-CoA, Acetoacetyl-CoA). These are done by dehydrogenation reactions, similar to beta-oxidation. Specific products are as follows: Valine ------> ------> Propionyl-CoA Isoleucine ------> ------> Acetyl-CoA + Propionyl-CoA Leucine ------> ------> Acetyl-CoA + Acetoacetyl-CoA METABOLISM OF PROPIONATE: In the case of Valine and Isoleucine, we need to further convert Propionyl-CoA to Succinyl-CoA by adding a carbon. Propionyl-CoA + HCO3- ------> D-Methylmalonyl-CoA + L-Methylmalonyl-CoA Catalyzed by Propionyl-CoA Carboxylase It requires biotin as a cofactor. 2ATP (coupled with pyrophosphatase) is required, too. The reaction produces the racemic mixture of a chiral compound. The products are driven toward D-product by the action of the next step. D-Methylmalonyl-CoA ------> Succinyl-CoA Catalyzed by Methylmalonyl-CoA Mutase It requires Cobalamin (Vit B12) as a cofactor. This is an isomerization reaction: the carboxyl group is rearranged and put on the end of the molecule. Because of this product, Propionyl-CoA can lead to glucose via gluconeogenesis. So, not all fatty acids are exclusive of glucose. Propionyl-CoA is the exception. INBORN ERRORS OF AMINO ACID METABOLISM: Problems of nitrogen metabolism can be caused by a lot of things. Generally nitrogen-metabolism diseases involve mental retardation and other neurological problems. Tyrosine deficiency (a consequence of PKU) can lead to albinism. THE METHYLATION CYCLE: Cysteine is synthesized from Methionine and Serine, via S-Adenosyl Methionine. The methylation cycle consists of methylating and demethylating methionine repeatedly. REQUIRED STARTING REACTANTS: Methionine, which is recycled, each turn of the cycle 1 ATP, to generate S-Adenosylmethionine, each turn of the cycle. 14 Tetrahydrofolate, which donates a methyl group to homocysteine, each turn of the cycle. Vitamin-B12, which is required to resynthesize methionine. Methionine ------> S-Adenosyl Methionine This is an adenylation reaction. ATP is required -- it is cleaved all the way down to the Adenosine base (ribose + adenine), releasing both Pi and PPi. Thus the reaction is very driven. The adenosine base is put on Methionine, and the phosphates are not. The pyrophosphate is cleaved by a pyrophosphatase to drive the reaction. S-Adenosyl Methionine ------> S-Adenosyl Homocysteine + -CH3 S-Adenosyl Methionine has a formal positive charge. It is a strong methylating agent. Methylation restores the neutral charge on the molecule. The methyl group may be donated to any of a number of acceptor-molecules in this step. S-Adenosyl Homocysteine ------> Homocysteine + Adenosine This is a hydrolysis reaction. The adenosine is recycled through purine metabolism. Homocysteine + -CH3 ------> Methionine Homocysteine here is used to regenerate Methionine, making the methylation routine a cycle. This reaction requires Cobalamin (Vit B12) The single carbon fragment is coming from N5-Methyl Tetrahydrofolate. Thus another essential cofactor is folic acid. SYNTHESIS OF CYSTEINE: Instead of regenerating methionine, homocysteine can also do the following: Homocysteine + Serine ------> Cystathionine Cystathionine is a thioether (C-S-C linkage) Cystathionine ------> Cysteine + alpha-Ketobutyrate Cysteine is formed simply by transferring the sulfur to the carbon skeleton of Serine. So, cysteine is formed from both Serine and Methionine. SYNTHESIS OF TYROSINE: Phenylalanine ------> Tyrosine Enzyme = Phenylalanine Hydroxylase. O2 is required. This enzyme is a Mixed-function Oxidase, utilizing a mini-electron transport chain and redox cofactors. Tetrahydrobiopterin is a required cofactor. PHENYLKETONURIA (PKU): Deficiency of Phenylalanine Hydroxylase Phenylalanine Hydroxylase is required for the normal breakdown of Phenylalanine, as well as for Tyrosine synthesis. The following build up in the absence of functional Phenylalanine Hydroxylase: Phenylalanine Phenylpyruvate, aminotransferase product of Phenylalanine, which isn't normally made. Phenyl lactate, reduced phenylpyruvate, which isn't normally made. 15 Phenylacetate, oxidized phenylpyruvate, which isn't normally made. Clinical Symptoms: Mental Retardation, possible albinism (from tyrosine deficiency). Differential Diagnoses: Excretion of phenyl ketones in the urine High levels of phenylalanine in the blood Treatment: PKU screening is done early in life, because the disorder is quite treatable with diet. Diet very low (but not absent) in phenylalanine. Critical period to prevent retardation is infancy. Tetrahydrobiopterin: Up to 3% may have a defect in this cofactor instead of Phenylalanine Hydroxylase. This leads to a more serious condition, because tetrahydrobiopterin is also an essential cofactor for production of DOPA and the Catecholamines, which are both also phenylalanine derivatives. Supplemental Treatment for Tetrahydrobiopterin-based PKU includes therapeutic doses of DOPA and hydroxytryptophan. L-DOPA is also used to treat people with Parkinson's Disease. GARROD'S HYPOTHESIS: It states that "all inherited diseases result from defects found in a single gene," as opposed to multifactorial etiology of diseases. This somewhat holds true for phenylalanine, in that most cases are due to a single deficiency. Now we know it is not completely accurate for PKU. PKU is a recessive inherited disorder. FOLIC ACID and TETRAHYDROFOLATE: Folic Acid is an essential vitamin in the diet. Structure: para-aminobenzoic acid base, with multiple glutamates connected to the carboxyl via peptide bonds. Thus Folic Acid is a polyglutamic acid conjugate Conjugase in our intestine converts Folic Acid Polyglutamate ------> Folic Acid Monoglutamate, so that we can absorb it. SULFA DRUGS: The old class of antibiotics. They mimic and block paraaminobenzoic acid (PABA), which is required for folic acid synthesis in bacteria, thus killing the bacteria. SYNTHESIS OF TETRAHYDROFOLATE: Folic Acid Monoglutamate ------> Dihydrofolic Acid ------> Tetrahydrofolic Acid Two NADPH ------> NADP+ are required. Hence this is a standard reductive biosynthetic reaction. Enzyme = Dihydrofolate Reductase. CHEMOTHERAPY: Dihydrofolate Reductase is essential to maintain levels of Tetrahydrofolate (THF) Methotrexate is an analog of dihydrofolate and a great inhibitor of dihydrofolate reductase. Because THF is required for purine synthesis, methotrexate stops proliferation of metastatic cells. Sulfanilamide (Sulfa drugs) is another drug that acts in the same way. Obvious side effects are that it will stop THF synthesis in other cells, too, preventing division in intestinal epithelia, skin, and hair, e.g. 16 In high doses, methotrexate kills bone marrow. UTILIZATION OF TETRAHYDROFOLATE: Once in the fully reduced form, THF is utilized in various forms as a methylating agent: Tetrahydrofolate + -CH3 ------> N5-N10-methylene tetrahydrofolate The CH3 in this reaction comes from Serine. Concurrent demethylation therefore is Serine ------> Glycine This (Serine) is the most common source of methyl groups for the tetrahydrofolate cofactor. Methylene-Tetrahydrofolates exist in several different forms having different oxidation states. Thus THF can donate a methyl group, as it does in purine synthesis, in several different oxidation states. N5-Methyl Tetrahydrofolate: This is the form that donates a methyl group to the reaction: Homocysteine + CH3 ------> Methionine Again, Vit-B12 is required for this reaction. METHYL-TRAP HYPOTHESIS explains a Vitamin-B12 deficiency, saying that methyl groups get "trapped" in the form of N5-Methyl Tetrahydrofolate because VitB12 is deficient. Result of this = THF can't get to other essential forms for lack of methyl groups, and purine synthesis is impeded as a result. PURINE (ADENINE, GUANINE) METABOLISM SYNTHESIS OF PURINES: The basic purine is Inosinate (IMP), from which AMP and GMP are made. SYNTHESIS OF THE RIBOSE SUGAR and N-LINKAGE IN PURINES Ribose-5-Phosphate + Glutamine ------> 5-Phosphoribosyl-1-Pyrophosphate (PPRP) + Glutamate Catalyzed by PPRP-Synthetase, or Ribose-5-Phosphate Pyrophosphokinase Ribose-5-Phosphate came from the Pentose Phosphate Pathway, of course. ATP is required, yielding pyrophosphate which is cleaved by pyrophosphatase. Thus the reaction is irreversible. PPRP is also one of the starting points of pyrimidine biosynthesis. PPRP ------> 5-Phosphoribosyl-1-Amine Enzyme = Amidophosphoribosyl Transferase This product has a nitrogen attached to the C-1 Carbon of the ribose. Thus this product already has the ribose nitrogen-linkage intact. This is the same linkage that will remain in the final purine structure. This is the COMMITTED STEP in the Purine Biosynthesis. SYNTHESIS OF THE SMALLER OF THE TWO PURINE RINGS 5-Phosphoribosyl-1-Amine ------> Glycinamide Ribonucleotide Addition of Glycine, which donates 2 carbons and 1 nitrogen to the ring 17 Glycinamide Ribonucleotide ------> Formylglycinamide Ribonucleotide Addition of a single carbon from 10-formyl-tetrahydrofolate. So, this carbon comes on as a highly oxidized formate group (single carboxylic acid), from one of the oxidation states of THF. Formylglycinamide Ribonucleotide ------> Formylglycinimadine Ribonucleotide Add a lone nitrogen (I presume it comes from free ammonia) Formylglycinimadine Ribonucleotide ------> 5-Aminoimidazole Ribonucleotide Cyclization to form the imidazole ring (the smaller of the two purine rings) Condensation reaction occurs between the Formate of Step-b and the lone nitrogen of step-c above. SYNTHESIS OF THE LARGER OF THE TWO PURINE RINGS 5-Aminoimidazole Ribonucleotide ------> 5-Aminoimidazole-4-Carboxylate Ribonucleotide Addition of a carbon from HCO3 5-Aminoimidazole-4-Carboxylate Ribonucleotide ------> 5-Aminoimidazole-4-NSuccinocarboxamide Ribonucleotide Addition of Aspartic Acid 5-Aminoimidazole-4-N-Succinocarboxamide Ribonucleotide ------> 5-Aminoimidazole4-Carboxylate Ribonucleotide Removal of the carbon skeleton of Aspartate (i.e. fumarate), leaving only the alpha-amino Nitrogen Aspartate only donates 1 nitrogen to the purine ring -- not its entire structure. 5-Aminoimidazole-4-Carboxylate Ribonucleotide ------> 5-Formamidoimidazole-4Carboxamide Ribonucleotide Addition of a single carbon, from 10-formyl-tetrahydrofolate. Again the carbon is added in the form of a formyl group. 5-Formamidoimidazole-4-Carboxamide Ribonucleotide ------> Inosinate Monophosphate (IMP) Closure of the second (larger) purine ring Condensation reaction occurs between the Nitrogen from the Aspartate, and the single carbon that just came from THF. SYNTHESIS OF AMP: Replace the carbonyl on the larger purine ring with an amine group. Inosinate (IMP) + Aspartic Acid ------> Adenylosuccinate The entire Asp residue is put onto the carbonyl of the larger of the two purine rings. Adenylosuccinate ------> Adenylate (AMP) + Fumarate Aspartic acid leaves again as fumarate. So, again aspartate only donates a nitrogen to change IMP to AMP. SYNTHESIS OF GMP: Add an amine to the other (non-oxidated) carbon of the larger purine ring. Inosinate (IMP) ------> Xanthylate This is an oxidation of the non-carbonyl carbon on the larger purine ring. Concurrent reduction: NAD+ ------> NADH Xanthylate + Glutamine ------> Guanylate (GMP) + Glutamate 18 This is just addition of an NH3 from glutamine. It gets put on the newly oxidized carbon (keto group) of the purine ring, forming an imine linkage. So, in this case the extra NH3 comes from the side chain of glutamine, and glutamine does not stay on the ring as an intermediate. ATP is required. SUMMARY: WHAT DONATES CARBONS TO THE PURINES? RIBOSE and N-LINKAGE: Carbons from Ribose-5-Phosphate, from Pentose Phosphate Shunt Nitrogen Linkage from Glutamine side-chain nitrogen SMALLER PURINE RING (3 carbons, 2 nitrogens) 2 carbons and 1 nitrogen from Glycine 1 nitrogen from Free NH3 1 carbon from 10-formyl-tetrahydrofolate LARGER PURINE RING (4 carbons, 2 nitrogens) 1 nitrogen from the alpha-amino group of Aspartic Acid 1 carbon from HCO3 1 carbon from 10-formyl-tetrahydrofolate (the 2 carbons that fuse the two rings together both come from Glycine) AMP EXTRA MODIFICATION: An extra nitrogen from the side chain of Aspartate GMP EXTRA MODIFICATION: An extra nitrogen from the side chain of Glutamine REGULATION OF PURINE BIOSYNTHESIS: IMP, AMP, and GMP: They show negative feedback on their own synthesis. They inhibit steps 1 and 2 of purine synthesis. Inhibit formation of PPRP (phosphoribosyl pyrophosphate), which is common to both purine and pyrimidine synthesis. Inhibit formation of Phosphoribosylamine from PPRP -- the committed step. SYNERGISTIC: The inhibitory effects of AMP and GMP on these steps are independent and additive. They bind to separate sites. Remember that these reactions are never turned completely off. They are only slowed down. GMP specifically inhibits the conversion of IMP to Xanthylate. Simple negative feedback. AMP specifically inhibits the conversion of IMP to Adenylosuccinate. Simple negative feedback. THE SALVAGE PATHWAY: Recycling of Hypoxanthine, Guanine, and Adenine, which are all purines. A salvage pathway exists for pyrimidines too, but it isn't clinically important. PPRP + Purine ------> Purine Ribonucleotide All we are doing here is putting another ribose-phosphate moiety on a naked purine base. Enzyme for Hypoxanthine and Guanine= Hypoxanthine-Guanine Phosphoribosyl 19 Transferase (HGPRT) Enzyme for Adenine = Adenine Phosphoribosyl Transferase DEGRADATION OF PURINES: Purines are broken down to URIC ACID for excretion. AMP ------> IMP ------> Hypoxanthine Hypoxanthine ------> Xanthine Xanthine Oxidase catalyzes this step. We need to know this enzyme. GMP ------> Xanthine: GMP is degraded directly to Xanthine at this stage. Xanthine ------> Uric Acid Xanthine Oxidase catalyzes this step, too. Uric Acid is then excreted. GOUT: Buildup and precipitation of uric acid in the joints There are multiple causes of Gout: Often caused by partial deficiency of HGPRT, the main enzyme of the Salvage Pathway. No salvage pathway means there is no place for purines to go but to uric acid ------> buildup of uric acid. Loss of feedback inhibition of PRPP-Synthetase, resulting in overproduction of purines and hence over secretion. Kidney damage resulting in reduced secretion uric acid. Treatment: Allopurinol: A suicide-inhibitor of Xanthine Oxidase. Allopurinol is an analog of Xanthine. Xanthine Oxidase reacts with Allopurinol, forming Alloxanthine. Upon reacting, Xanthine Oxidase renders itself non-functional. Hence allopurinol is a "suicide inhibitor" of xanthine oxidase. Xanthine and Hypoxanthine build up as a side-effect. But they are more soluble than uric acid. LESCH-NYHAN SYNDROME: Complete loss of HGPRT and hence the Salvage Pathway Partial loss of HGPRT results in Gout. Complete loss is far more serious. Symptoms: Mental retardation and autistic self-mutilation. Gout-like symptoms as well, which can be treated with allopurinol. HGPRT is an X-Linked gene. Thus the disease is more common in men. De Novo purine synthesis is still available, thus there is no shortage of purines. It is not clear why the symptoms occur. HGPRT is found to be 10-20x more concentrated in the brain. Maybe the brain depends on that pathway more for some reason. ANTI-OXIDANTS: Uric Acid, along with Bilirubin, Ascorbic Acid and Glutathione, plays a role in defense against anti-oxidants. 20 PYRIMIDINE (CYTOSINE, THYMINE, URACIL) BIOSYNTHESIS CARBAMOYL PHOSPHATE SYNTHETASE II: Forms carbamoyl phosphate to start pyrimidine synthesis, using a different enzyme and different reaction than is used for urea synthesis. Glutamine + HCO3- ------> Carbamoyl Phosphate + Glutamate Glutamine is the nitrogen donor rather than NH3, losing an NH3 to become glutamate. This can occur as a CYCLE -- to make multiple pyrimidines. Just resynthesize glutamine using more free ammonia. SHUNT: If there were a block somewhere in urea synthesis, carbamoyl phosphate could build up and force this pathway. Carbamoyl Phosphate Synthetase II is the primary regulated step of Pyrimidine Biosynthesis. It is standard negative feedback inhibition: UTP inhibits the enzyme. CARBAMOYL PHOSPHATE SYNTHETASE I CARBAMOYL PHOSPHATE SYNTHETASE II Synthesis: First step in Urea metabolism First step in Pyrimidine metabolism Nitrogen Donor: Free NH4+, primarily from the Glutamate Dehydrogenase reaction. Glutamine, which can be regenerated again from glutamate, to form a cycle. Tissue Distribution: Liver primarily All tissues make pyrimidines Cellular Location: Mitochondria Cytosol PYRIMIDINE SYNTHESIS: SYNTHESIS OF UMP. The first pyrimidine synthesized de novo is UMP. The other pyrimidines are made off of that. After we have carbamoyl phosphate... Carbamoyl Phosphate + Aspartate ------> N-Carbamoylaspartate The whole aspartate is added to the carbamoyl phosphate. This step occurs in the cytosol. This is the COMMITTED STEP of pyrimidine biosynthesis. N-Carbamoylaspartate <====> Dihydroorotate This is a cyclization reaction, making a ring by forming an amide linkage between the alpha-amino of aspartate and a carbonyl from carbamoyl phosphate. This step also occurs in the cytosol. Dihydroorotate <====> Orotate This reaction occurs in the mitochondria. Everything from here forward occurs in the mitochondria. It is your basic redox reaction, with dihydroorotate being oxidized to orotate (not sure what the redox cofactor is). Enzyme = Dihydroorotate Dehydrogenase Orotate + PPRP ------> Orotidylate + PPi This is the step where we add the ribose and form the sugar C1-N linkage. Note that in pyrimidine synthesis we add it here, whereas in purine synthesis we started with it in the first place. Enzyme = Orotate Phosphoribosyl Transferase. We are adding a ribosyl-phosphate to the orotate structure. Orotidylate ------> Uridylate (UMP) + CO2 21 Enzyme = Orotidylate Decarboxylase Lose the final CO2 off the ring, and all we are left with is the pyrimidine (6-member) ring structure. ADDING MORE PHOSPHATES: Once the basic nucleotide is formed (such as UMP or IMP), it can always be converted to the diphosphate and triphosphate level by using phosphates transferred from ATP, i.e. use a nucleotide kinase. SYNTHESIS OF CYTIDINE (CTP): Cytidine synthesis occurs at the triphosphate level. It is the addition of a nitrogen group from the side-chain of glutamine. UTP + Glutamine ------> CTP + Glutamate 1 ATP is required! SYNTHESIS OF DEOXYRIBONUCLEOTIDES: RIBONUCLEOTIDE REDUCTASE. The reduction involves changing the 2' OH to just an H. An ENZYME COMPLEX utilizing a MINI-ELECTRON TRANSPORT CHAIN carries out the reaction. For all nucleotides, this reaction occurs at the DIPHOSPHATE LEVEL -- i.e. CDP, UDP, ADP, GDP Thioredoxin is the key COFACTOR that has oxidized and reduced forms. Oxidized form: Disulfide S--S linkage. Reduced form: HS-- --SH thiol groups Order of Reactions in the chain: Reduction Oxidation Ribonucleotide ------> Deoxyribonucleotide Thioredoxin (reduced) ------> Thioredoxin (oxidized) Thioredoxin (oxidized) ------> Thioredoxin (reduced) FADH2 ------> FAD FAD ------> FADH2 NADPH ------> NADP+ This reaction is driven by NADPH -- This is a biosynthetic reductive reaction. SYNTHESIS OF THYMINE: Thymine is made from deoxy-uridine (dUMP). First, some uridine is converted to deoxyuridine. Then that is used to make thymine. dUDP ------> dUMP. First a phosphate must be removed before we make thymine. dUMP ------> dTMP Enzyme = Thymidylate Synthetase. This is methylation reaction. A methyl group is added to uridine to make thymidine. The methylation is done by N5,N10-Methylene Tetrahydrofolate. Dihydrofolate is left over as a byproduct. Thus Dihydrofolate Reductase is required to maintain thymidine synthesis. Every time we make a thymidine, we use up a THF by oxidizing it to the dihydrofolate form. Ultimately we must re-reduce it to make more thymidine. REGULATION OF RIBONUCLEOTIDE REDUCTASE: 22 ATP stimulates the production of Deoxy-Cytidine (dCDP) and Uridine (dUDP) Extra ATP means have lots of ribonucleotide but not enough deoxyribonucleotide. Hence it encourages the production of DNA. dATP inhibits the production of all the deoxyribonucleotides. Three nucleotides inhibit dCDP production: dATP, dTTP, dGTP dGTP stimulates dADP synthesis. If we have too much dGTP around, relatively, then we need more dATP. dTTP stimulates dGDP synthesis. Don't ask me why. Comparison of Purine and Pyrimidine Biosynthesis: PURINES PYRIMIDINES Committed Step Formation of PPRP Formation of NCarbamoylaspartate Cellular Location Cytosol Cytosol and Mitochondria Order of Events We start with PPRP -- the ribose We start by building the moiety, and build the purine pyrimidine ring and then add the rings around it ribose to it. Regulation IMP, AMP, and GMP inhibit enzymes at multiple steps Carbamoyl Phosphate Synthetase II is inhibited by UTP Degradative Product Uric Acid. The purine ringSuccinyl-CoA. The pyrimidine structure is not broken. ring-structure is broken down DEGRADATION OF PYRIMIDINES: Pyrimidines are ultimately broken down to Succinyl-CoA and then recycled. Degradation of Thymine: Thymidine ------> ------> Methylmalonyl-CoA In multiple steps we get Methylmalonyl-CoA The nitrogen is lost as NH3 (to go to urea synthesis or transamination) Methylmalonyl-CoA ------> Succinyl-CoA. I think here a carbon is added, so this is a carboxylation reaction. Take Home Lesson: Pyrimidine rings can be broken down to yield succinate. Degradation of Uracil: We get beta-Alanine as the product, which ultimately then goes to Acetyl-CoA. CHEMOTHERAPY AGENTS: Also see methotrexate above. Azaserine: It is a glutamine analog. It would interfere with nucleotide synthesis wherever glutamine is the nitrogen donor (such as in Carbamoyl Phosphate Synthetase II) 5-Fluorocil -- inhibits thymidylate synthetase 3-Deazauridine -- Uridine analog with a missing nitrogen. It will stop translation at uridine residues. AZT: An analog of thymidine that is missing TWO hydroxy groups on the ribose sugar instead of one. This prevents it from base-pairing in HIV viral replication and transcription. 23 Side-Effects: Other tissues will also use the drug, esp. liver tissue. OTHER AIDS DRUGS: Other drugs have recently hit the market: DDC, DDA, DDI. PORPHYRIN METABOLISM SYNTHESIS OF HEME: Protoporphyrin IX is the precursor of the heme group found in hemoglobin and myoglobin. Succinyl-CoA + Glycine ------> delta-Aminolevulinate Enzyme = delta-Aminolevulinate Synthetase This is the COMMITTED STEP and the REGULATED STEP of heme-biosynthesis. This is a condensation reaction. Coenzyme-A is given off to drive the reaction, and a CO2 is given off of glycine. delta-Aminolevulinate x 2 ------> Porphobilinogen Two of them condense together and cyclize to form porphobilinogen. Porphobilinogen x 4 ------> Protoporphyrin IX This condensation gives the basic tetrapyrrole structure of heme, with no iron in the middle yet. Protoporphyrin IX, as well as heme, are basically planar. Protoporphyrin IX still has side chains hooked to it, of three sorts: Propionate group Methyl group Vinyl group HEME STRUCTURE AND FUNCTION: Coordination Points: The central iron has six coordination points: Four of them are to the four nitrogens of the porphyrin ring. This holds the iron in place. One is to a Histidine residue on the globin molecule. The final one binds reversibly to O2 or H2O depending on whether oxygen is currently bound. Iron: The central iron of the heme group must remain in the Fe+2 state in order to be functional. It is the job of reducing agents like Glutathione to keep Iron in the ferrous (Fe+2) state. Irons ability to bind oxygen in the heme structure is unique: oxygen can bind reversibly to it with oxidizing it. BREAKDOWN OF HEME: Heme degradation ultimately leads to bilirubin. Heme breakdown occurs in the liver. Heme ------> Biliverdin This is a Mixed-Function Oxidase using the enzyme Heme Oxygenase to cleave the heme ring-structure. Despite the fact that this is an oxygenation, NADPH is required as well! 24 Biliverdin ------> Bilirubin Enzyme = Biliverdin Reductase NADPH is required for this step too: NADPH ------> NADP+ (but this time it makes more sense because its a reduction reaction). BILIRUBIN: Derivatives of bilirubin and clinical stuff Bilirubin should not build up. Buildup of bilirubin in the blood is an indication of liver dysfunction. Bilirubin in high levels is non-soluble and toxic. It acts as a neurotoxin. JAUNDICE: High levels of bilirubin coupled with hepatitis (liver inflammation) leads to jaundice. Bilirubin is photosensitive. When it builds up in infants, it can be converted to more soluble, less toxic forms by exposing it to fluorescent light. CONJUGATION OF BILIRUBIN: Bilirubin + UDP-Glucuronic Acid ------> Bilirubin Diglucuronide. This is the soluble, conjugated form of bilirubin. BILIRUBIN EXCRETION: Glucuronide form is excreted in the feces primarily, and some in the urine as well. Urobilinogen is excreted in the urine and is the primary form that gives urine its color. Urobilinogen is reabsorbed from the GI-Tract, after it has been acted on by intestinal bacteria. PORPHYRIAS: Hereditary problems with heme metabolism. Commonly found symptoms = neurological disturbances and skin photosensitivity Acute Intermittent Porphyria: dominant Problem with delta-Aminolevulinate Synthetase, the first step in heme-synthesis. Or it could happen with an error in the second step of heme-synthesis -- production of Porphobilinogen (Uroporphyrinogen I Synthetase) Symptoms: Neurological disturbances Congenital Erythropoietic Porphyria: recessive Skin sensitivity and fragile erythrocytes Hereditary Coproporphyria -- dominant, + same screwed up enzymes as above. Neurological disturbances and skin photosensitivity. Hereditary Protoporphyria -- dominant Ferrochelatase is altered enzyme -- the enzyme that puts the iron in heme. Lead Poisoning: This disorder is also associated with lead poisoning, which alters deltaaminolevulinate metabolism. TREATMENT: Injection of hematin -- preformed heme with the iron already present. REGULATION OF HEME SYNTHESIS: Negative feedback. Heme inhibit delta-aminolevulinate synthetase, which is the committed step in the pathway. ANTI-OXIDANTS: Here are nitrogen metabolic intermediates that serve as anti-oxidants. Reduced glutathione (with SH at the end) Uric Acid -- One theory of evolution says that we live long because we have high (almost to the precipitation point) concentrations of uric acid. Ascorbic Acid (Vit. C) 25 Bilirubin has anti-oxidant properties MISCELLANEOUS STUFF SYNTHESIS OF S-ADENOSYL METHIONINE (SAM): Review. Once again, S-Adenosyl Methionine is formed from Methionine + ATP, where the Adenylyl Group of the ATP goes onto the Methionine, and all three phosphates are given off as Pi + PPi. METHYL-TRANSFERS: Some of the methylation reactions that S-Adenosyl Methionine partakes in. Remember that THF is required to recycle Homocysteine back to SAM, for each time it methylates. METHYLATION AT A NITROGEN: The CH3 group is added to a N. Norepinephrine ------> Epinephrine Guanidoacetate ------> Creatine Phosphatidylethanolamine ------> Phosphatidylcholine Lysine or Guanine ------> N-Methyl Lysine or N-Methyl Guanine METHYLATION AT AN OXYGEN: Synthesis of Melatonin Norepinephrine ------> Normetanephrine (Ephedrine) METHYLATION AT CARBON: Cytosine ------> 5-Methyl Cytosine OTHER TRANSFERS REACTIONS: Aminopropyl group of SAM is transferred in the synthesis of polyamines (see below) Adenosyl group of SAM may be transferred in the conversion of vitamin B12 (Cobalamin) to storage form. CHOLINE: Phosphatidylcholine is a Quaternary Amine with a positive charge -- R-N+(CH3)4. So to completely convert ethanolamine to choline, it takes 3 SAM. Serine ------> Ethanolamine Ethanolamine ------> Choline POLYAMINES: Polyamines are highly positively-charged species that serve to condense negativelycharged DNA in sperm. They are made from Ornithine, from the Urea cycle. Ornithine ------> Putricine Decarboxylation reaction. Putricine ------> Spermidine This reaction involves an Aminopropyl Group Transfer from a derivative of SAM. Spermidine ------> Spermine Same as above -- we use SAM to transfer yet another Aminopropyl group -- to give us a highly aminated (and therefore very positively charged) compound. ROADKILL: Polyamine formation occurs with dead, decaying tissue. It smells bad. TISSUE DISTRIBUTION: Prostate, seminal vesicles, and sperm itself have highest concentration of polyamines. Brain tissue has almost none. 26 CREATINE: Creatine Phosphate is the form in which high-energy bonds are stored in muscle. SYNTHESIS: Creatine is formed by methylating the dipeptide Arg-Gly. Arginine-Glycine ------> Creatine via S-Adenosyl Methionine (SAM) Creatine Kinase: Creatine + ATP ------> Creatine Phosphate + ADP. This is the longer-term storage form of high energy bonds in muscle. ATP can only stick around for so long. EXCRETION: Muscle has a high concentration of creatine phosphate. The amount of creatine we find in our system is therefore proportional to muscle mass and to muscle activity. Creatine <====> CREATININE. Creatinine is a cyclized form of creatine, and the form in which we excrete it. In a healthy individual, the amount of creatinine excreted in the urine is constant over a given period, and is proportional to muscle mass. CARNITINE: Carnitine was the acyl-intermediate in mitochondria, necessary for beta-oxidation. Lysine ------> Epsilon Trimethyl-Lysine. This again is the transfer of 3 methyl groups using 3 SAM. Like choline, all three of the CH3's go onto a nitrogen to make a quaternary amine. Epsilon Trimethyl-Lysine ------> Carnitine CERAMIDE: The basic component of sphingomyelin and of the gangliosides. Palmitoyl-CoA + Serine ------> Sphingosine Sphingosine is the base-structure of ceramide, without any acyl groups added. Sphingosine + Acyl-CoA ------> Ceramide + CoA Acylate the sphingosine, using a charged acyl-group, to make ceramide. Ceramide ------> Sphingomyelin -- Add a choline as the polar head group, to make sphingomyelin. Ceramide ------> ------> Gangliosides -- Add UDP-Galactose (and other sugars) to make gangliosides GAMMA-AMINOBUTYRIC ACID (GABA): GABA, a neurotransmitter implicated in depression, is made from glutamate. Glutamate Decarboxylase: Glutamate ------> GABA + CO2. GABA is simply a decarboxylated form of glutamate. Chinese-Restaurant Syndrome: MSG can be hazardous because of its associated to GABA. People who are sensitive to MSG are though to get too high levels of GABA in the brain for a short time. DEGRADATION of GABA: GABA ------> ------> Succinate. GABA can be degraded down to succinate. CATECHOLAMINES: Dopamine, Epinephrine, Norepinephrine. Tyrosine ------> DOPA (Dihydrophenylalanine) This is a hydroxylation reaction -- simply add another hydroxyl group. DOPA ------> Dopamine This is a Decarboxylation Dopamine ------> Norepinephrine 27 Hydroxylation of the benzylic carbon. Norepinephrine ------> Epinephrine This is a SAM-Methylation. Epinephrine is methyl-norepinephrine. PARKINSON'S DISEASE: Deficiency of dopamine neurotransmitter, from cell death i the substantia nigra. Treatment = huge doses of dopamine along with an inhibitor that prevents rapid breakdown of dopamine, in hopes of getting lots to the brain. The treatment only treats the symptoms. It does not cure the disease. FORMS OF BREAKING DOWN the Catecholamines: They are rapidly inactivated and excreted by two enzymes. So, we need a continuous supply of them. Norepinephrine ------> 3,4-Dihydroxyphenylglycolaldehyde, via Monoamine Oxidase Norepinephrine ------> 3-O-Methylepinephrine, via Catechol-O-Methyltransferase. SEROTONIN: Neurotransmitter comes directly from tryptophan, via a two-step process: decarboxylation and hydroxylation HISTAMINE: Intercellular mediator, comes directly from histidine, via a single decarboxylation. MELANIN: Comes from Tyrosine COENZYME-A: Comes from pantothenic acid, plus cysteine and ATP. NICOTINIC ACID: You can make nicotinic acid, and hence NAD, from Tryptophan via its degradative pathway. INTEGRATED METABOLISM Generalities: ATP is the universal currency of energy. ATP is generated by the oxidation of metabolic fuels Glycolysis Oxidative Phosphorylation NADPH is the major electron donor in REDUCTIVE BIOSYNTHETIC pathways. NAD+ is the major electron acceptor in OXIDATIVE DEGRADATIVE pathways. Biological molecules are constructed from a small set of building blocks. Synthetic and Degradative pathways are almost always distinct from each other. Principles of Metabolic Regulation: Substrate Supply: An enzymatic reaction cannot proceed in the absence of sufficient substrate. Allosteric Interactions. They can be either positive or negative. They are not all-or-none interactions. Covalent Modifications = primarily phosphorylation. This is completely on-or-off per molecule, but still overall you are not affecting every substrate so the change is still at least somewhat gradual one way or the other. Enzyme-Levels 28 Compartmentalization Organ Specialization GLUCOSE: Glucose-6-Phosphate has key metabolic branch points. Glucose-6-P <====> Glucose-1-P <====> Glycogen: Glycogenesis, Glycogenolysis Glucose-6-P ------> 6-Phosphogluconolactone (PPP Shunt) Glucose-6-P <====> Fructose-6-P <====> Pyruvate (Glycolysis) PYRUVATE: Key metabolic branch points Pyruvate <====> Oxaloacetate (Anaplerosis) ------> Glucose-6-P (Gluconeogenesis) Pyruvate <====> Lactate (Lactate Dehydrogenase, regeneration of NAD+) Pyruvate ------> Acetyl-CoA (Pyruvate Dehydrogenase) ACETYL-CoA: Primary branch points Acetyl-CoA ------> HMG-CoA (Sterol Biosynthesis) HMG-CoA ------> Cholesterol ------> Hormones etc. HMG-CoA ------> Ketone Bodies Acetyl-CoA ------> CO2 (Oxidative Phosphorylation) Acetyl-CoA <====> Fatty Acids (Lipogenesis, Lipolysis) FATTY ACID BIOSYNTHESIS: REGULATION Regulated Step = Acetyl-CoA Carboxylase: Acetyl-CoA ------> Malonyl-CoA INHIBITED by Palmitoyl-CoA, i.e. by its own product. STIMULATED by Citrate Citrate generally indicates lots of energy to spare, hence its time to do fat synthesis. GLYCOLYSIS: REGULATION Regulated Step = Phosphofructokinase (PFK): Fructose-6-Phosphate ------> Fructose-1,6Biphosphate STIMULATED BY -- these two indicate a deficiency of energy Fructose-2,6-Biphosphate AMP INHIBITED BY -- once again... Citrate ATP GLUCONEOGENESIS: REGULATION Regulated Step = Fructose-1,6-Biphosphotase: Fructose-1,6-Biphosphate ------> Fructose-1Phosphate INHIBITED BY AMP and Fructose-2,6,-Biphosphate (not enough energy is around for gluconeogenesis) STIMULATED BY Citrate and ATP PENTOSE PHOSPHATE PATHWAY: REGULATION Regulated Step: Glucose-6-Phosphate Dehydrogenase: Glucose-6-Phosphate ------> 6Phosphogluconolactone ------> 6-Phosphogluconate 29 INHIBITED by NADPH STIMULATED by NADP+, which means we need to make more NADPH. THE HORMONES: GLUCAGON = generally catabolic PROMOTE Gluconeogenesis in liver, glycogenolysis, lipolysis INHIBIT Glycogenesis, Lipogenesis EPINEPHRINE = generally catabolic -- the "hormone of starvation" STIMULATES Lipolysis in particular, plus the other catabolic processes STIMULATES the release of glucagon from the pancreas CORTISOL = both catabolic and anabolic -- the "hormone of the defense state" PROMOTE GLycogenesis, Gluconeogenesis, and Proteolysis. INSULIN = generally anabolic PROMOTE Glucose absorption by cells, amino acid transport into cells, Glycogenesis, Lipogenesis It does NOT promote Glucose-Uptake, per se, in the lens of the eye and brain, where glucose is essential at all time anyway. INHIBITS Gluconeogenesis and Glycogenolysis FUTILE CYCLES: Irreversible reactions, catalyzed by different enzymes going in each direction. The purpose to them is that you can go back and forth, accomplishing nothing but generating heat from lost high-energy bonds (usually ATP). PEP <====> Pyruvate Fructose-1-Phosphate <====> Fructose-1,6-Biphosphate Lots and lots of them CORI CYCLE: Hard-working muscles release lactate. MUSCLE = Glycolysis: Glucose-6-Phosphate ------> Pyruvate ------> Lactate LACTATE than travels from skeletal muscle to liver. LIVER = Gluconeogenesis: Lactate ------> Pyruvate ------> Oxaloacetate ------> Glucose-6Phosphate GLUCOSE-ALANINE CYCLE: Alanine is released by muscles that are not necessarily working so hard. Object = Take an AMINO GROUP from muscle and send it to liver for urea synthesis. MUSCLE: Glucose-6-Phosphate ------> Pyruvate ------> Alanine The alanine step is accomplished via transamination of pyruvate. Both of them have the same carbon-skeleton! ALANINE then travels in venous blood to liver. LIVER: Alanine ------> Pyruvate ------> ------> Glucose-6-Phosphate The nitrogen group is removed from Alanine here to contribute to urea synthesis AMINO ACID BALANCE: After eating (i.e. in the post absorptive state): There is more glutamine and alanine being released from the skeletal muscle into the blood. Glutamine is released significantly, because it is a carrier of amino groups out of the tissues. 30 Alanine is released significantly because of the glucose-alanine cycle. That means there is much more of these amino acids in venous blood then in arterial blood. Vir: http://www.kumc.edu/AMA-MSS/Study/nitrogen.htm 31