* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pharmacology Block 3 Notes Autonomic Pharmacology I
Survey
Document related concepts
Drug interaction wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
NMDA receptor wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Norepinephrine wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Psychopharmacology wikipedia , lookup
Transcript
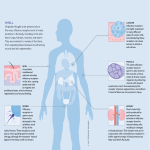
Pharmacology Block 3 Notes Autonomic Pharmacology I-III Autonomic nervous system o A division of the PNS that is further subdivided into sympathetic and parasympathetic components o Is purely MOTOR! o Involuntary (you don’t think about it), is regulated by areas of the brain stem o Tissues it affects: smooth muscle, cardiac muscle, glands Neuron pathways o Three neuron types of concern: Sympathetic motor neuron: Preganglionic axon = short; Postganglionic axon = long At the synapse between the two, you have release of ACh which binds to nicotinic receptors o Nicotinic receptors: ion channel-linked receptors At the synapse between the postganglionic neuron and the target tissue, you have release of norepinephrine (primarily) or ACh which binds to adrenergic or muscarinic receptors o Adrenergic receptors: can be alpha or beta o Binds to muscarinic receptors if target is a sweat gland Alternative pathway: preganglionic neuron synapses with chromaffin cells in the adrenal medulla, releasing ACh which in turn causes the adrenal medulla to secrete epinephrine Parasympathetic motor neuron: Preganglionic axon = long; Postganglionic axon = short ACh still released at first synapse and binds to nicotinic receptors ACh released at synapse between postganglionic neuron and target tissue, where it binds to muscarinic receptors Somatic motor neuron: One neuron system; neuron goes directly to target tissue (probably skeletal muscle) Releases ACh at synapse where it binds to nicotinic receptors on the muscle fiber Enteric nervous system o A division of the PNS that innervates the GI tract o Controls GI motility and secretion; operates independently but is still regulated by the ANS and CNS Autonomic nervous system o Sympathetic division: fight or flight, thoracolumbar outflow (from T1-L2) Mydriasis: DILATION of pupils Stimulates SWEAT glands COMPLETELY innervate peripheral blood vessels o Parasympathetic division: rest and digest, cranio-sacral outflow Cranial nerves: 3, 7, 9, 10; Spinal nerves S2-S4 Miosis: CONSTRICTION of pupils Promotes secretions (except in sweat glands) Acetylcholine o Neurotransmitter released by CHOLINERGIC neurons o Released at the following sites: Between pre and postganglionic neurons in sympathetic, parasympathetic Between parasympathetic postganglionic neuron and target tissue Between somatic motor neuron and skeletal muscle (@ neuromuscular junction) Between sympathetic postganglionic neuron and sweat glands Norepinephrine o Neurotransmitter released by ADRENERGIC neurons o Released between sympathetic postganglionic neuron and target tissue o Note: epinephrine is released by the adrenal medulla in response to sympathetic stimulation Drugs and Neurotransmitters o Each type of neurotransmitter and drug has its own receptor it can bind to Affinity: the extent to which a drug/neurotransmitter binds to a receptor If it binds often, it has a high affinity o Agonist and antagonist: refers to the activity a drug/neurotransmitter has on the RECEPTOR (not the final physiologic effect) Agonist: something binds to the receptor and INCREASES the activity of the receptor (promotes the normal effect of that receptor) Antagonist: something binds to the receptor and DECREASES/INHIBITS the activity of the receptor (prevents the normal effect of the receptor) o A drug or neurotransmitter can serve as both an agonist and an inhibitor of function Example: a neurotransmitter binds to a receptor and increases that receptor’s activity (thus serving as an agonist); however when this receptor is activated, the activity of the neuron is decreased (generating an inhibitory effect) The receptor is thus an INHIBITORY RECEPTOR This is how molecules like GABA operate The goal of neurons (and neurotransmitters) is to generate an action potential o This is the way in which cells (primarily neurons) communicate with one another o It involves changes in resting membrane potential Inside of the neuron is negative and high in K+ and anions Outside of the neuron is positive and high in Na+ and Ca++ o Depolarization: resting membrane potential becomes more positive, you get closer to threshold and more likely to fire an action potential o Hyperpolarization: resting membrane potential becomes more negative, you are farther from threshold and less likely to fire an action potential Neurotransmission o Neurotransmitters are synthesized in the cell body (soma) of the presynaptic neuron, packaged into vesicles, and transported down the axon where they are stored in the axon terminal(s) o Depolarization of the axon terminal via an action potential causes opening of voltage-gated Ca++ channels, leading to an influx of Ca++ into the presynaptic axon terminal o The increase in intracellular Ca++ triggers release of neurotransmitter molecules into the synaptic cleft via exocytosis o Neurotransmitters cross the synaptic cleft and bind to receptors on the postsynaptic cell Ionotropic receptors: associated with an ion channel Metabotropic receptors: associated with a G protein Note: either of these receptors can be excitatory or inhibitory o Any neurotransmitter lingering in the synaptic cleft is removed via: Enzymatic degradation, with the metabolites being reabsorbed by the presynaptic neuron Diffusion away from the synapse Reuptake of the neurotransmitter by the presynaptic neuron o The signal generated in the postsynaptic cells is terminated through various mechanisms Acetylcholine o Synthesized in the presynaptic neuron by reacting acetyl-CoA with choline Note: the acetyl-CoA comes from mitochondria ACh contains a biological amine (very active subgroup) o ACh is broken down in the synaptic cleft by the enzyme acetylcholinesterase into acetate and choline Choline is then taken back up by the presynaptic neuron and recycled Norepinephrine (NE) o Synthesis: tyrosine to DOPA to dopamine Dopamine taken up into presynaptic vesicle where it is converted to norepinephrine o NE is NOT broken down in the synapse, instead is taken back up by the presynaptic neuron or nearby glial cells If taken back up by the neuron, is broken down by monoamine oxidase (MAO) If MAO is inhibited, you don’t get breakdown of NE in the neuron, meaning more of it will be released into the synapse next time If taken up by cells other than neurons, will be broken down by catecholO-methyltransferase (COMT) Receptors o ACh receptors: Muscarinic: found between parasympathetic postganglionic neuron and effector Nicotinic: found at all pre and postganglionic junction (sympathetic, parasympathetic) and neuromuscular junctions o Adrenoreceptors: Alpha-1 receptors: cause smooth muscle contraction Alpha-2 receptors: mediates sympathetic output Beta-1 receptors: cause cardiac stimulation Beta-2 receptors: promote smooth muscle relaxation Sympathetic nervous system effects are performed by stimulating ADRENERGIC receptors (alpha and beta) Parasympathetic nervous system effects are performed by stimulating CHOLINERGIC receptors (muscarinic; M2, M3, etc.) Heart: o Sympathetics: increase heart rate, electrical conduction, force of contraction o Parasympathetics: decrease heart rate, electrical conduction Will SLIGHTLY decrease the force of contraction (but not much) If you block M2 receptors (those receptors that promote parasympathetic activity in the heart) then you will have increased heart rate and electrical conduction, but force of contraction will not be changed much Remember the parasympathetics (b/c the sympathetics will be the opposite) o DUMBBELLS Diarrhea, urination, miosis (pupil constriction), bradycardia, bronchoconstriction/bronchospasm, erection, lacrimation, lethargy, salivation/sweating Baroreceptor reflex o The way in which the body responds to elevated blood pressure (as a result of sympathetic stimulation) o Baroreceptors in your arteries detect the increased arterial pressure and send info by way of afferent fibers to the vasomotor cortex in the medulla o The medulla receives and interprets this information, ultimately sending info out by way of efferent fibers: Decreases sympathetic output, resulting in vasodilation (b/c only sympathetics go to blood vessels) Increases parasympathetic activity of the heart to decrease heart rate and cardiac output End result = decreased blood pressure Drugs that work on acetylcholine neurotransmission o Hemicholinium and vesamicol Hemicholinium: prevents reabsorption of choline by the presynaptic neuron (preventing it from being recycled to make more ACh) Vesamicol: prevents ACh from being taken up into presynaptic vesicles Note: neither of these have clinical use b/c they are NON-SELECTIVE cholinergic antagonists If you were to use either of these, you would inhibit ALL ACh systems in the body, preventing normal ACh activity, resulting in mass paralysis (due to lack of muscle contraction) o Tetrodotoxin (TTX) Blocks voltage-gated Na+ channels needed for depolarization to produce the action potential No depolarization, no action potential, no neurotransmitter release o Alpha-Latrotoxin (derived from black widow spider) Creates pores in the axon’s plasma membrane, resulting in Ca++ flowing in w/o stimulation from an action potential The initial increase in Ca++ causes a massive release of ACh from the presynaptic neuron When an action potential is eventually produced, the ACh reservoir of the presynaptic neuron will be depleted and you will lose normal ACh activity at the postsynaptic cell (b/c you no longer have any ACh to release) o Botulinum toxin Degrades SNAP-25 protein (needed for presynaptic vesicle to fuse w/presynaptic membrane so ACh can be released into the synaptic cleft) Results in no ACh being released o Atropine Is a muscarinic receptor antagonist Binds to muscarinic receptor for ACh on postsynaptic cell, preventing ACh from binding Ultimately prevents ACh’s effect at the postsynaptic cell o Physostigmine Acetylcholinesterase inhibitor Ultimately allows for increased concentrations of ACh in the synaptic cleft, improving the likelihood that ACh will bind to a postsynaptic receptor and exert its effects o Dantrolene Binds to a receptor on the endoplasmic reticulum in the postsynaptic cell, blocking the effects of Ca++ influx Example: in a muscle cell, by blocking Ca++ influx, you prevent release of Ca++ from the sarcoplasmic reticulum of the muscle cell, preventing muscle contraction o Leading to muscle relaxation Cholinergic agonists (molecules that bind to ACh receptors and promote the normal activity of the receptor) o Nicotinic receptor agonists: molecules that bind to the nicotinic ACh receptor and stimulate its activity Nicotinic receptors are EVERYWHERE (these drugs therefore have widespread effects) Classic example: Nicotine Sympathetic effects: increased heart rate, blood pressure Parasympathetic effects: diarrhea, urination CROSSES THE BLOOD-BRAIN BARRIER: resulting in alertness, vomiting, tremors, convulsions, coma Varenicline Used for smoking cessation; reduces cravings and withdrawal effects Cons: suicidal ideation, depression Is a PARTIAL AGONIST: o Varenicline binds to the nicotinic receptor, promoting SOME of its effect, but not to the same degree as would a full agonist In this sense, it is also acting as an ANTAGONIST b/c it is preventing nicotine from binding o Muscarinic receptor agonists (molecule that binds to the muscarinic ACh receptor and promotes the activity of the receptor) Five types of muscarinic receptors M1,3,5 are coupled to Gq which activates phospholipase C o Phospholipase C in turn activates an EPSP M2,4 are coupled to Gi, which inhibits adenylate cyclase o Shuts down the cell’s ability to mobilize Ca++ Primarily promote parasympathetic nerve activity Bethanecol: Used for postoperative ileus, urinary retention Stimulates bladder/GI w/o affecting heart rate or blood pressure Pilocarpine Uses: glaucoma, xerostomia o Lowers intraocular pressure by increasing aqueous humor outflow o Stimulates secretions of salivary glands Cevimeline Uses: xerostomia, Sjogren’s syndrome o Stimulates salivary gland secretion Side effects: In high doses can cause acute circulatory failure and cardiac arrest Contraindications: asthma, COPD, UPD o b/c parsympathetics cause bronchoconstriction o Acetylcholinesterase inhibitors Are reversible and short-acting By inhibiting acetylcholinesterase, you are preventing the breakdown of ACh in the synaptic cleft, therefore more of it will be available to bind to cholinergic receptors (thus acetylcholinesterase inhibitors can be thought of as cholinergic receptor AGONISTS) Edrophonium: used in the diagnosis of myasthenia gravis Neo- and pyridostigmine: used to treat myasthenia gravis, neuromuscular blockade, and postoperative urinary retention Physostigmine: used for glaucoma Donepezil, galantamine, rivastigmine: used in Alzheimer’s Disease Potentiates ACh effects in the hippocampus and other areas responsible for memory Myasthenia gravis o An autoimmune condition where the body produces antibodies against the nicotinic ACh receptors at the neuromuscular junction o Therefore there are significantly fewer ACh receptors available on the muscle cells, meaning the effects of ACh will be greatly hindered o Results in skeletal muscle weakness (altered speech, dysphagia, problems chewing, loss of facial expressions, ptosis, double vision, etc.) o Diagnosis: Administer IV edrophonium (an acetylcholinesterase inhibitor) If patient has MG, they will show rapid but brief improvement in muscle strength If patient does NOT have MG, they will experience fasciculations (twitching beneath the skin) o Treatment: Pyridostigmine: an acetylcholinesterase inhibitor Take PO QD Also given immunosuppressants at the same time (corticosteroids) AE: abdominal cramps, diarrhea Reasoning: you are increasing ACh levels system-wide, therefore ACh will stimulate both nicotinic and MUSCARINIC receptors o Muscarinic receptors = parasympathetic activity = GI tract = increased peristalsis, bowel movements Irreversible cholinesterase inhibitors o Work by phosphorylation of acetylcholinesterase (forming a permanent covalent bond) o With acetylcholinesterase inhibited, acetylcholine accumulates in the synaptic cleft, therefore its effects are potentiated Through triggering BOTH nicotinic and muscarinic receptors o Examples: Organophosphates-pesticides, nerve gases Highly lipid soluble (absorbed via skin, mucous membranes, gut) o Organophosphate toxicity With this, you have knocked out your acetylcholinesterase, therefore you have excess ACh in the synaptic cleft, and its effects are potentiated Symptoms: Miosis, salivation, sweating, bronchoconstriction, vomiting, diarrhea o All are parasympathetic effects triggered through ACh stimulation of MUSCARINIC receptors CNS: cognitive disturbance, seizures, coma Neuromuscular blockade Treatment: Supportive care (especially for maintaining an open airway), decontamination, atropine (large doses), benzodiazepines, 2-PAM o Atropine: muscarinic receptor antagonist Prevents ACh from binding to muscarinic receptor, decreasing muscarinic (parasympathetic) effects o Benzodiazepines: for seizures o 2-PAM: to regenerate acetylcholinesterase Nicotinic receptor antagonists o Molecules that bind to the nicotinic receptor, blocking the normal activity of that receptor o Nicotinic receptors found at the synapse between the pre and postganglionic neurons in both sympathetic and parasympathetic pathways Also found at synapse between somatic motor neuron and skeletal muscle o Depending on whether the blocking effect is greater at the sympathetic or parasympathetic ganglion will determine the effects observed If blocking is greater at the sympathetic ganglion: You won’t get sympathetic activity Symptoms will be parasympathetic in nature o Ex.) hypotension If blocking is greater at the parasympathetic ganglion: You won’t get parasympathetic activity Symptoms will be sympathetic in nature: o Dry mouth, blurred vision, urinary retention o These drugs are NOT used clinically (b/c of widespread systemic effects) Excitatory postsynaptic potentials (EPSP) o If the accumulation of EPSPs is of sufficient magnitude, then an action potential is generated o ACh released from the preganglionic neuron binds to nicotinic ACh receptors in the postganglionic cell membrane o This subsequently causes opening of Na+ channels, leading to an influx of Na+ in the postganglionic neuron, resulting in generation of an EPSP (thus you are more likely to generate an action potential in the postganglionic neuron, allowing for continued signal transmission) Muscarinic receptor antagonists o Molecules that bind to muscarinic receptors (ACh receptors found at the junction between the parasympathetic postganglionic neuron and the effector tissue) and block the activity at said receptor o b/c muscarinic receptors facilitate PARASYMPATHETIC effects, and you are blocking the muscarinic receptors, you are essentially blocking parasympathetic activity o Therefore the effects will be sympathetic in nature o Two big classes of drugs: Belladonna alkaloids: atropine, hyoscyamine, scopolamine Semisynthetic/synthetic agents: dicyclomine, glycopyrrolate, ipratropium, oxybutynin Anticholinergic toxicity o Anticholinergic: inhibiting cholinergic activity, i.e. ACh activity at muscarinic receptors (parasympathetic) Symptoms will be mainly sympathetic in nature (b/c you have inhibited parasympathetic activity) o Example: Jimson weed Contains belladonna alkaloids (muscarinic receptor antagonists) Commonly ingested or inhaled Treatment: decontamination, supportive care, acetylcholinesterase inhibitor Acetylcholinesterase inhibitor would prevent the breakdown of ACh, meaning more of it would be in the synaptic cleft With more ACh in the synaptic cleft, it now has a greater chance of binding muscarinic receptors, increasing parasympathetic activity (thus counteracting the sympathetic related symptoms of toxicity) Note: quaternary amines do NOT cross the blood brain barrier; tertiary amines DO cross the barrier o Belladonna alkaloids (example-atropine) are drugs that act as muscarinic receptor antagonists, blocking the effects of ACh at the muscarinic receptor, thus blocking parasympathetic activity and causing sympathetic related symptoms These compounds contain tertiary amines, so they WILL GET INTO THE BRAIN!! Belladonna alkaloids o Atropine, scopolamine, hyoscyamine o Are well-absorbed and cross the blood brain barrier (thus enter the CNS) o Excreted renally, has a longer half-life in the eye than systemically o Is a muscarinic receptor antagonist Dry as a bone: inhibits secretions Blind as a bat-causes pupillary dilation (mydriasis) Red as a beet- blood pressure increases along with heart rate Mad as a hatter- delirium Semisynthetic/synthetic anticholinergic drugs o Man-made drugs that bind and inhibit the activity of ACh muscarinic receptors (thus you are intentionally trying to inhibit parasympathetic activity, and thus indirectly promoting sympathetic activity) o Ipratropium/tiotropium-inhaled, used for COPD Promotes bronchodilation (by inhibiting bronchoconstriction) o Dicyclomine-used for symptoms of irritable bowel and intestinal cramping Decreasing peristalsis/digestion o Oxybutynin-used for overactive bladder Inhibiting urine production and secretion (promoting urinary retention) o Glycopyrrolate- used preoperatively and in terminally ill patients to inhibit secretions of salivary and respiratory tract Secretions are a parasympathetic response o Tropicamide-used in eye exams to cause pupil dilation (mydriasis) You are inhibiting miosis (pupil constriction, a parasympathetic activity) Contraindications for muscarinic receptor antagonists o i.e. when do you NOT want to inhibit parasympathetic activity o bowel blockage-you do NOT want to inhibit peristalsis during this time o urinary retention/prostatic hypertrophy-you do NOT want to inhibit urine production and secretion (they’re already having trouble urinating) Miosis and Mydriasis in relation to drugs o Miosis = constriction of the pupils (parasympathetic response) o When you give a muscarinic receptor agonist…… Ciliary muscles of the eye contract, suspensory ligaments that hold the lens in place relax, the lens becomes thicker, allowing for accommodation of the eye o Mydriasis = dilation of the pupils (sympathetic response) o When you give a muscarinic receptor antagonist Suspensory ligaments of the eye tighten, the lens becomes thinner and you are now able to focus on distant objects Autonomic Pharmacology IV-V Noradrenergic transmission o The process by which the neurotransmitter norepinephrine is synthesized, stored, released and acts within a synaptic pathway o Norepinephrine is released by postganglionic sympathetic motor neurons and acts on adrenoceptors, which have both alpha and beta forms and subtypes o Again since norepinephrine is released by SYMPATHETIC motor neurons, its targets are: smooth muscle, cardiac muscle and glands Alpha adrenoceptors o Alpha -1: mediates contraction of Vascular smooth muscle (causing vasoconstriction) Iris dilator muscle (causing mydriasis, i.e. pupil dilation) Urinary tract smooth muscle (causing urinary retention) o Alpha-1 receptors are also found in exocrine glands and the CNS o Alpha -2 receptors: INDIRECTLY mediates smooth muscle relaxation Reasoning: In the environment you have high levels of norepinephrine This then acts via a negative feedback loop through stimulating alpha-2 receptors, which tells the noradrenergic neurons to stop producing norepinephrine Eventually norepinephrine levels decrease, and thus their sympathetic effects (in this case smooth muscle contraction) decrease o Causing smooth muscle relaxation o Alpha-2 receptors are also found in platelets and the pancreas Beta adrenoceptors o Beta-1: responsible for cardiac stimulation Will increase heart rate, force of contraction and electrical conduction velocity o Beta-1 receptors are also found in the kidney When stimulated will cause release of renin Begins the renin-angiotensin-aldosterone system which ultimately increases blood pressure o Beta-2: mediate relaxation of Bronchial smooth muscle (causing bronchodilation) Uterine smooth muscle Vascular smooth muscle (causing vasodilation) o Beta-2 receptors are also found in: Skeletal muscle where they mediate K+ uptake Liver where they mediate glycogenolysis Glycogenolysis is the breakdown of glycogen to glucose o The glucose is then released into circulation, where it is available to be utilized by cells during sympathetic responses REMINDER: blood vessels are ONLY under SYMPATHETIC control o Sympathetics act on vascular smooth muscle to cause vasoconstriction, thus increasing blood pressure o If you want to decrease blood pressure through vasodilation, you have to have sympathetic stimulation of beta-2 receptors Other misc. receptors o D-1: mediate smooth muscle relaxation in blood vessels (causing vasodilation) o D-2: modulate neurotransmitter release o Imidazoline receptors: promote natriuresis (removal of Na+ via urine) and decrease sympathetic outflow from CNS Adrenoreceptor agonists: molecules that stimulate activity at the adrenoreceptors (alpha and beta norepinephrine receptors) ; thus stimulate sympathetic activity o Direct-acting agonists: molecules that they themselves actually bind to the receptors and stimulate its activity Example: catecholamines and noncatecholamines o Indirect-acting agonists: increase the concentrations of norepinephrine in the synapse More epinephrine at the synapse means more of it will bind to adrenoreceptors and thus stimulate the receptor’s activity o Mixed-acting agonists: molecules that have both direct and indirect effects Direct acting adrenoreceptor agonists: molecules/drugs that bind to adrenoreceptors and stimulate their activity o Catecholamines: Natural: norepinephrine, epinephrine, dopamine Synthetic: isoproterenol, dobutamine Are rapidly inactivated by monoamine oxidase (in postganglionic neurons) and COMT (in nearby glial cells) in gut, liver, other tissues These drugs have a low bioavailability and short half life Therefore you give parenterally to maximize on the concentration of the drug, thereby improving its effects Norepinephrine: Acting on alpha-1 receptors: vasoconstriction, leading to increased systolic and diastolic blood pressure (which in turn generates a reflex arc leading to bradycardia i.e. slow heart rate) Epinephrine: Low dose: activates beta-2 receptors: vasodilation, leading to decreased diastolic blood pressure and also bronchodilation High dose: activates alpha-1 receptors: vasoconstriction which increases systolic and diastolic blood pressure Dopamine: Low dose: activates D-1 receptors: vasodilation of renal blood vessels Mid dose: activates beta-1 receptors: increased force of contraction/cardiac output/tissue perfusion High dose: activates alpha-1 receptors: vasoconstriction Isoproterenol: activates beta-1,2 receptors: cardiac stimulation (beta-1) and vasodilation (beta-2), decreases diastolic blood pressure but increases systolic blood pressure (via increasing heart rate, contractility) May result in tachycardia and tachyarrhythmias; bronchodilation Dobutamine: activates beta-1 receptors leading to increased force of contraction and cardiac output; activates beta-2 receptors leading to vasodilation and decreased blood pressure Mean arterial pressure o Perfusion pressure seen by organs (organs require a certain blood pressure in order to be supplied vascularly) o MAP greater than 60 mm Hg is enough to sustain the organs of an average person o If MAP significantly decreases, the organs will not receive enough blood flow, leading to ischemia and serious injury o MAP = 1/3 (SBP – DBP) + DBP SBP = systolic blood pressure (top number) DBP = diastolic blood pressure (bottom number) Catecholamines o Are direct-acting adrenoreceptor agonists (meaning they will bind to adrenoreceptors and stimulate the natural activity of that receptor, often times promoting sympathetic actions) o Indications for usage: Shock (cardiogenic, neurogenic/septic, anaphylactic), cardiac arrest, bradycardia/atrioventricular block, prolongation of local anesthetic action, acute heart failure o Catecholamines that result in an INCREASED blood pressure = vasopressors Shock o Profoundly decreased blood flow to vital organs (can lead to ischemia = bad) o Different types of shock: Hypovolemic: decreased blood volume Cardiogenic: inadequate heart function Neurogenic/septic: inadequate vasomotor tone (the blood vessels are not constricted to the degree needed to perfuse organs) Septic: pathogens release toxins that cause massive vasodilation Anaphylactic: severe immediate hypersensitivity reaction leading to hypotension (low blood pressure) and difficulty breathing o Treatment: Hypovolemic shock: fluid resuscitation (but gradually so as not to cause cerebral edema) Cardiogenic shock: dobutamine first (to stimulate beta-1 receptors) and then possibly in addition/in place use dopamine (again to stimulate beta1 receptors) Neurogenic/septic shock: norepinephrine (to activate alpha-1 receptors); often used with dopamine to preserve renal blood flow (through activating D-1 receptors) Get their MAP over 60 mm Hg Anaphylactic shock: epinephrine (activates alpha-1 receptors to cause vasoconstriction and increase blood pressure; also activates beta-2 to cause bronchodilation) Adverse effects of catecholamine treatment o Excessive vasoconstriction (through overstimulating alpha-1 receptors) Tissue ischemia, leading to necrosis Reduced blood perfusion of organs o Excessive cardiac stimulation (overstimulating beta-1 receptors) Arrhythmias o Glycogenolysis (overstimulating beta-2 receptors in the liver) Hyperglycemia (bad if you have diabetes mellitus) Noncatecholamines o Are also direct acting adrenoreceptor agonists o They do NOT have a catechol moiety, therefore they are not substrates for COMT and may be resistant to monoamine oxidase o Therefore they have a higher bioavailability than catecholamines (and thus can be given orally) and also have a longer duration of action (longer half-life) o Phenylephrine Well absorbed orally/topically; also given IV Partially metabolized in liver and intestines by monoamine oxidase Activates alpha-1 receptors: causing smooth muscle contraction Indications: As nasal decongestant or as an ocular decongestant In ophthalmologic exams to induce mydriasis (pupil dilation) Hypotension/shock due to: o Excessive vasodilators, drugs, septic/neurogenic shock, maintenance of blood pressure during surgery o Midodrine Taken orally, rapidly absorbed, and converted to an active metabolite (desglymidodrine) in the liver and tissues Activates alpha-1 receptors, thus causing smooth muscle contraction Results in vasoconstriction and increased blood pressure (both systolic and diastolic) whether patient is standing, sitting or supine Used to treat orthostatic hypotension Adverse effects include hypertension Beta-2 agonists: molecules that bind to the beta-2 adrenoreceptor and stimulate its effects, namely smooth muscle relaxation o Bioavailabilty of 30-50% b/c of incomplete absorption and 1st pass metabolism In other words, not all of the drug that is taken makes it into the bloodstream o Metabolized to inactive compounds and excreted renally o Can be administered orally, IV or inhaled o Beta-2 agonists cause relaxation of bronchial, uterine and vascular smooth muscle o Indications: Asthma, COPD : you want to induce bronchodilation to improve their airflow Premature labor: with this, the problem is contractions of uterine smooth muscle, therefore you want to correct this by RELAXING uterine smooth muscle o Adverse effects: tachycardia, skeletal muscle tremor, nervousness o Examples: albuterol, terbutaline, metaproterenol, etc. Imidazolines o Can activate: Alpha-1 receptors: causing smooth muscle contraction Ex. oxymetazoline-nasal and ocular decongestant Alpha-2 receptors: indirectly causing smooth muscle relaxation via feedback inhibition of norepinephrine Ex. brimonidine- decreases intraocular pressure w/ocular surgery o Alpha-2 and imidazoline leads to receptor activation in the CNS o Clonidine- used to treat HTN Alpha-2 receptor agonist in the CNS By stimulating alpha-2 receptors in the medulla, clonidine promotes feedback inhibition of norepinephrine, leading to decreased effects of norepinephrine o Specifically a decrease in vasoconstriction (thus promoting vasodilation) a decrease in heart rate and cardiac output Leading to decrease in blood pressure Adverse effects: dry mouth, sedation, dizziness DO NOT STOP COLD TURKEY Can result in rebound HTN w/o clonidine, you no longer have the same alpha-2 stimulation, therefore feedback inhibition of norepinephrine is decreased, meaning you will have overarching effects of norepinephrine (HTN via alpha-1 stimulation, tachycardia via beta-1 stimulation and sweating via sympathetic stimulation of sweat glands) Indirect-acting adrenoreceptor agonists o Molecules that increase the concentrations of norepinephrine in the synaptic cleft, thus potentiating the effects of norepinephrine at adrenoreceptors (still promoting sympathetic activities) o Amphetamine: increases the amount of norepinephrine released into the synapse Highly lipid soluble, increases levels of norepinephrine in CNS and peripherally Potentiates the effects of norepinephrine: Vasoconstriction via alpha-1 stimulation Cardiac stimulation via beta-1 stimulation Increased blood pressure via alpha-1 and beta-1 effects CNS stimulation o Cocaine Blocks the reuptake of norepinephrine by postganglionic neurons, therefore increasing its concentration and potentiating its effects at the synapse Results in: Vasoconstriction, pupillary dilation via alpha-1 Cardiac stimulation via beta-1 Increased blood pressure via alpha-1 and beta-1 CNS stimulation Adverse effect: cardiac damage, heart failure due to excessive stimulation Mixed-acting adrenoreceptor agonists o Molecules that promote activity at adrenoreceptors by exerting both direct and indirect effects (i.e. can bind to the receptor or increase the amount of norepinephrine in the synapse) o Ephedrine and pseudoephedrine Activate the following: Alpha-1: causing smooth muscle contraction, leading to vasoconstriction, increased blood pressure and urinary retention Beta-1: cardiac stimulation, leading to tachycardia Beta-2: causing smooth muscle relaxation, leading to bronchodilation CNS stimulation leading to insomnia Adrenoreceptor antagonists o Molecules that inhibit the activity of adrenoreceptors Since adrenoreceptors are involved in sympathetic activities, adrenoreceptor antagonists result in a decrease in sympathetic activities (thus promoting parasympathetic activities) o Benefits of adrenoreceptor antagonists: Blocking alpha-1 receptors: prevents smooth muscle contraction Perhaps used to treat HTN Blocking beta-1 receptors: decrease cardiac stimulation Think beta-blockers o Adverse effects of adrenoreceptor antagonists: By blocking alpha-2 receptors, you get dizziness, headache, nasal congestion By blocking beta-2 receptors, you decrease smooth muscle relaxation In the lungs this results in bronchoconstriction In the liver this results in inhibition of glycogenolysis o Alpha-1 antagonists: Decrease smooth muscle contraction Leads to vasodilation (and decreased blood pressure), relaxation of smooth muscle in urinary tract Indications: HTN, urinary symptoms due to benign prostatic hypertrophy Adverse effects: hypotension, dizziness, sedation Non-selective alpha-adrenergic antagonists Molecules that inhibit the activity of alpha-1 and/or alpha-2 receptors Phenoxybenzamine o Non-competitive antagonist of epinephrine and other adrenoreceptor agonists o Gradual onset/duration o Decreases blood pressure o Used to treat HTN in patients w/pheochromocytoma until sx Phentolamine o Competitive antagonist (competing w/the substrate or an agonist for the alpha adrenoreceptor) o Immediate onset, short duration o Decreases blood pressure o Used to treat: HTN caused by alpha-1 agonists, dermal necrosis/ischemia due to extravasation of epinephrine, perioperatively for patients w/pheochromocytoma o Alpha-2 receptor antagonists Blocks the activity of alpha-2 receptors Meaning they prevent the feedback inhibition of production of norepinephrine by adrenergic neurons You are inhibiting the inhibition, thus you get INCREASED norepinephrine production Example: Yohimbine (Yocon) Competitive antagonist Enters CNS where it: o Increases blood pressure and heart rate (via alpha-1 and beta-1 stimulation) and motor activity o Beta-1 receptor antagonists (aka cardioselective beta-blockers) Molecules that inhibit the activity at beta-1 adrenoreceptors (responsible for cardiac simulation) Beta-1 receptors primarily found in cardiac tissue As you increase the dose of administration of a beta-1 antagonist, it will also have inhibitory effects at beta-2 receptors (responsible for smooth muscle relaxation) Results in decreased heart rate, force of contraction and electrical conduction velocity Ultimately decreasing cardiac output and blood pressure Also decreases secretion of aqueous humor in the eye, thereby decreasing intraocular pressure o Nonselective beta adrenoreceptor antagonists Block beta-1 receptors in the heart: leading to decreased cardiac output/stimulation Block beta-2 receptors: leading to decreased smooth muscle relaxation (thus promoting smooth muscle contraction); also results in inhibition of glycogenolysis (b/c you are blocking beta-2 receptors in the liver) o Partial agonist A molecule that binds to a receptor and promotes the normal activity of the receptor, but not to the same degree (or strength) as the normal substrate/agonist would Also concurrently functions as an antagonist b/c it prevents the normal substrate/full agonist from binding and exerting its complete effect(s) Neuromuscular Blocking Agents Neuromuscular junction o Synapse formed between the presynaptic somatic motor neuron and the postsynaptic muscle fibers o ACh is released into the synaptic cleft, where it binds to receptors (either nicotinic or muscarinic) on the muscle fibers, ultimately leading to muscle contraction Nicotinic: ion-channel coupled receptor Muscarinic: G-protein coupled receptor o Acetylcholinesterase is the enzyme within the synaptic cleft responsible for the breakdown of ACh that lingers in the synapse Nicotinic ACh receptors o Can be Nm or Nn Nm: the nicotinic receptor found on the muscle fibers Nn: the nicotinic receptor found at the synapse between pre and postganglionic neurons in either the sympathetic or parasympathetic neuronal pathways o Ligand-gated ion channels; requires 2 ACh molecules to bind before it opens o Each nicotinic receptor is composed of five subunits (pentamer structure) There are 5 different types of subunits that can come together to form the pentamer Alpha, beta, gamma, delta, epsilon o 10 different alpha types and 4 different beta types Neuromuscular blocking agents o Work by binding to the nicotinic ACh receptors at the muscle fibers of the neuromuscular junction Since the blocking agent is binding to the nicotinic receptor, that means ACh cannot bind and exert its effects on muscle (i.e. contraction of skeletal muscle) Therefore the patient will experience muscle weakness and paralysis o These drugs do NOT cross the blood-brain barrier, therefore CNS effects probably won’t occur, meaning the patient will be paralyzed but still cognitively intact o These drugs are classified as depolarizing or nondepolarizing Depolarizing neuromuscular blocking agent: These drugs act as AGONISTS of the nicotinic ACh receptor It stimulates the activity of the receptor over a PROLONGED period of time, essentially “burning out” the activity of the receptor, which leads to the eventual muscle weakness and paralysis Think of it as “over-stimulation” Nondepolarizing neuromuscular blocking agent: These drugs act as COMPETITIVE ANTAGONISTS of the nicotinic ACh receptor o Meaning they bind to the receptor, thereby preventing ACh from binding and exerting its effects Leading to muscle weakness and paralysis Many of the neuromuscular blocking agents are of this type Neuromuscular blocking agents can have other pharmacologic effects o They can stimulate the release of histamine Histamine release results in bronchospasm (airways close down) and hypotension (decrease in blood pressure) Example: tubocurarine, mivacurium, atracurium o Block the activities of nicotinic ACh receptors at the synapse between pre and postganglionic neurons (in the sympathetic and parasympathetic pathways) Can lead to hypotension and tachycardia (elevated heart rate) o Block cardiac muscarinic receptors (remember muscarinic receptors facilitate parasympathetic activity) Leads to tachycardia Pharmacokinetics of neuromuscular blocking agents o Pharmacokinetics: what the body does to the drug o These drugs are poorly absorbed from the GI tract; therefore they are given IV (to get improved bioavailability) o They do NOT cross the blood-brain barrier or enter cells Distribution and blood volume are similar Meaning that the amount of drug that enters the circulation essentially stays in circulation o Eliminated via urine (by way of kidneys) and bile (by way of liver) essentially unchanged o Two specific drugs: atracurium and cisatracurium Undergo spontaneous nonenzymatic degradation to lighten the burden on the kidneys and liver as far as elimination Used in patients w/poor liver and kidney function Succinylcholine o A DEPOLARIZING neuromuscular blocking agent o Drug binds to the nicotinic ACh receptor at the motor end plate, causing prolonged depolarization (since it can’t be degraded by acetylcholinesterase); ultimately leads to over-stimulation of the receptor, causing it to be desensitized o Effects of the drug occur in two phases Phase I block: initial muscle fasciculation (twitching beneath the skin) over the chest and abdomen; this is followed by flaccid paralysis in the order of: eye/face, arms/legs/neck, intercostal muscles/diaphragm Phase II block: the plasma membrane of the muscle fiber repolarizes but has become desensitized due to prolonged stimulation o The patient’s recovery occurs in the reverse order of presentation Diaphragm, limb and trunk muscles, small muscles of eye and face o Adverse effects: Genetic variations in butyrylcholinesterase Succinylcholine can cause decreased levels of butyrylcholinesterase or can create abnormal forms of the enzyme that result in prolonged activity and apnea Increased intraocular and intragastric pressure Hyperkalemia (increased K+ levels) Patient who experience: burns, neuromuscular disease, nerve damage, closed head injury, trauma, etc. release excess K+ into the blood o Could potentially result in cardiac arrest When to use neuromuscular blockers o Endotracheal intubation o Those patients on mechanical ventilators Done to decrease O2 consumption o Prevent bone fractures during electroconvulsive therapy o To decrease the depth (amount) of anesthesia required for surgery Drug interactions with neuromuscular blocking agents o INHALED ANAESTHETICS POTENTIATE THE EFFECTS OF NEUROMUSCLAR BLOCKERS! o Therefore when you use both of these together, the dosage must be reduced o Malignant hyperthermia can result when succinylcholine is used alongside an inhaled anesthetic (rare) Anesthetic potentiates (increases) the effect of succinylcholine You get abnormal release of calcium from skeletal muscle Increases the initial muscle contraction and rigidity, leading to increased heat production which causes the hyperthermia (increased body temp) o These drug interactions can also cause metabolic acidosis and tachycardia o ANTIBIOTICS POTENTIATE THE EFFECTS OF NEUROMUSCULAR BLOCKERS Aminoglycosides: decrease the release of ACh at the neuromuscular junction; with decreased levels of ACh in the synapse, the nicotinic ACh receptors on the muscle becomes less sensitive Tetracyclines: chelate Ca++, decreasing the release of ACh at the synaptic cleft Clindamycin: blocks nicotinic ACh receptors, preventing the effects of ACh at the neuromuscular junction When administering antibiotics alongside neuromuscular blocking agents, the dosage must be reduced o Local anesthetics and neuromuscular blockers Local anesthetics, like inhaled anesthetics, potentiates the effects of neuromuscular blockers Either blocks neuromuscular transmission (blocking the release of ACh) or prolongs the activity of the blocker Drug-disease considerations o Avoid prolonged duration of neuromuscular blocking agents with the elderly and those with kidney or liver disease Since they are older, their kidneys and liver are probably not the greatest, therefore they may have decreased clearance of these drugs; with decreased clearance, the drugs will therefore have a longer duration of activity Remember NM blocking agents are cleared via urine and bile o Hyperkalemia: potentiates the effects of depolarizing agents but counteracts the effects of non-depolarizing agents o Hypokalemia: potentiates the effects of non-depolarizing agents and counteracts the effects of depolarizing agents Drug selection: How do you choose which NM blocker to administer to your patient? o Onset of action: how long does it take for the drug to kick in o Duration of action: how long does the drug work for o Adverse effects o The patient’s renal and hepatic function o Potential for reversal Non-depolarizing neuromuscular blocking agents (those that act as competitive antagonists) can have their effects reversed by cholinesterase inhibitors Reasoning: if you inhibit acetylcholinesterase, you increase the levels of ACh in the synapse, meaning it can outcompete with the blocker for the nicotinic ACh binding site on the muscle Skeletal Muscle Relaxants Skeletal muscle relaxants = spasmolytics Two broad classes o Antispasticity drugs: Decrease muscle cramping/tightness due to neurological disorders (MS, CP, spinal cord injury, etc.) o Antispasmodic agents: What people typically think of as muscle relaxants Designed to prevent use-related minor muscle spasms; used to treat lower back pain (patient comes to you saying they threw their back out) Antispasticity Drugs o Note: these are the kinds used to treat muscle cramping/tightness due to NEUROLOGICAL disorders o Spasticity: Hyperexcitability of alpha motor neurons in the spinal cord Can be due to: Loss of normal inhibition Imbalance of excitatory and inhibitory neurotransmitters Antispasticity drugs work by altering neurotransmitter activity both in the CNS and at neuromuscular junctions o Antispasticity drugs are designed for SYMPTOMATIC treatment Meaning they are meant to improve the patient’s quality of life and allow them to perform basic activities and functions They are NOT designed to treat the underlying disease/condition o How to manage spasticity (order of progression): Remove or treat the noxious stimuli Physical/occupational therapies including proper positioning and regular stretching Oral drug therapy Injection of botulinum toxin type A Intrathecal baclofen Surgical intervention o Spasticity is associated with the muscle stretch reflex arc A muscle fiber in the periphery undergoes stretching, which activates stretch receptors in the muscle fiber These stretch receptors send sensory information via afferent fibers to the spinal cord (specifically the dorsal horn of the gray matter) Within the gray matter of the spinal cord are numerous interneurons These interneurons receive the sensory information from the stretch receptors, integrate and process the information, deciding the appropriate response The interneurons can then release glutamate (an excitatory neurotransmitter) that in turn acts on the motor (efferent) neuron in the ventral horn, placing it in an excited state The motor neuron, being excited, causes muscle contraction at the effector muscle, resulting in the spasticity characteristic of the patient o Baclofen: MOA: binds to GABA-B receptors on the presynaptic terminal of interneurons in the spinal cord; GABA-B is a metabotropic receptor (coupled to a G-protein) causes hyperpolarization of the membrane, meaning it is now more difficult to reach threshold and fire an action potential no action potential means no Ca++ influx, which means no neurotransmitter release; therefore the motor neuron is not excited Widely distributed, crosses the blood-brain barrier 1ST LINE MEDICATION USED TO TREAT SPASTICITY! Adverse Effects: Drowsiness DO NOT ABRUPTLY WITHDRAW (as it can cause hallucinations, seizures) Use with caution in patients with seizures or renal impairment, as it lowers the threshold for seizures (making it easier to have one) Can be given orally or through an intrathecal pump Intrathecal administration: pump is placed between muscle/skin of abdomen w/catheter running into subarachnoid space Allows direct drug access to CNS o Diazepam MOA: Binds to GABA-A receptors (Cl- channels) at both the pre and postsynaptic neurons in the spinal cord and brain o Specifically binds at the benzodiazepine site, keeping the Cl- channel open longer Cl- influx into the neurons, causing hyperpolarization, leading to decreased chance of generating an action potential and decreased neurotransmitter releases Has quick onset of action (15-30min) Is metabolized by CYP450 in the liver Three of its metabolites are active! Has numerous drug interactions Has long elimination half-life (48hrs) Adverse effects: Sedation, impaired mental/psychomotor function Anterograde amnesia: you have trouble forming new memories Physical dependence and withdrawal (high abuse potential) Crosses the placenta (don’t give to pregnant women) o Tizanidine MOA: Binds to alpha-2 adrenergic receptors on the presynaptic neuron (interneuron) to inhibit spinal motor neurons Has a LOW bioavailability due to extensive hepatic first pass metabolism Metabolized in the liver by CYP1A2 Avoid taking w/ciprofloxacin as this is an inhibitor of CYP1A2, meaning tizanidine will hang around in the patient’s system longer Use with caution in patients with renal insufficiency as clearance of the drug will be reduced by 50% i.e. the drug will remain in their system longer Adverse effects: Dose-related hypotension, sedation, dry mouth Avoid abrupt withdrawal as it can cause rebound hypertension o Dantrolene MOA: Acts WITHIN the skeletal muscle Binds to receptors on the sarcoplasmic reticulum, preventing release of Ca++ from the SR in response to increased intracellular Ca++ concentrations w/o release of Ca++ from the SR, no muscle contraction takes place Well absorbed, metabolized in liver via CYP450 DRUG OF CHOICE FOR TREATING MALIGNANT HYPERTHERMIA Characterized by: high fever, tachycardia, hypertension, rigidity Adverse effects: Hepatotoxicity w/chronic use o Dalfampridine MOA: Broad-spectrum K+ channel blocker that increases action potential conduction through a demyelinated axon Excreted via urine essentially unchanged Adverse effects: Contraindicated in patients with renal dysfunction (creatinine clearance of less than 50ml/min) and in patients with history of seizures o Lowers seizure threshold o Botulinum toxin type A MOA: Works at the neuromuscular junction, blocking the release of ACh from the presynaptic neuron into the synaptic cleft o Specifically functions by degrading the protein SNAP-25, needed for the presynaptic vesicle containing the ACh to fuse with the presynaptic membrane No ACh release means no muscle contraction Given intramuscularly for spasticity, such as that seen with cerebral palsy Takes about 1 week for effect to start (b/c you have to degrade the SNAP-25 proteins) but lasts for about 3 months Antispasmodic agents o Used to prevent minor muscle spasms related to use/activity; also used to treat lower back pain o Typically what most patients think of when they hear the term “muscle relaxant” o Big indications for usage: low back pain, tension headaches However, they are NOT 1ST LINE THERAPY CHOICES Instead, BEGIN WITH ACETAMINOPHEN AND NSAIDS!!! o Pharmacology is UNKNOWN (is why they shouldn’t be used right off the bat) They do NOT act on motor neurons or the muscle However, they are known to be CNS depressants and therefore cause sedation o Chlorzoxazone Undergoes extensive phase II metabolism in the liver Serves as a substrate for numerous CYP450 enzymes and is also an inhibitor of certain CYP450 enzymes As such it has NUMEROUS DRUG INTERACTIONS Adverse effects: RED OR ORANGE URINE Contraindicated in patients w/hepatic dysfunction o Reasoning: since chlorzoxazone undergoes extensive hepatic metabolism, if the patient’s liver function is impaired, the drug won’t be adequately metabolized, therefore it will have a prolonged effect o Cyclobenzaprine Undergoes complete oral absorption A majority binds to proteins Serves as a substrate for certain CYP450 enzymes Be on the lookout for drug interactions Eliminated via urine and bile Reveals the most evidence for efficacy Adverse effects: Tachycardia, hypotension, drowsiness Dry mouth, urinary retention (anticholinergic effects) Avoid w/serotonergic agents Incidences of QT prolongation and possible torsade de pointes have been seen alongside fluoxetine (a CYP450 2D6, 3A4 inhibitor) o Cyclobenzaprine is a substrate for CYP450 2D6 and 3A4 o Therefore if you take cyclobenzaprine alongside fluoxetine, the fluoxetine inhibits the enzymes responsible for metabolism of cyclobenzaprine, leading to longer duration of activity of cyclobenzaprine o Metaxalone Undergoes hepatic metabolism Is a CYP450 substrate for certain forms and an inhibitor of others o Look for drug interactions! Eliminated via kidney Adverse effects: Leukopenia (decreased WBC); hemolytic anemia (rare; decreased RBC) Contraindicated in those with impaired renal/hepatic function o Methocarbamol Widely distributed throughout the body Undergoes first pass metabolism in the liver Eliminated renally 3 days after the first dose Adverse effects: Black/brown/green urine Avoid in pregnancy as fetal abnormalities have been found o Orphenadrine Readily absorbed via GI tract Widely distributed throughout the body Hepatic metabolism; renal elimination Elimination half-life of 14-16 hours (long) Adverse effects: Drowsiness Dry mouth, urinary retention, increased intraocular pressure o Anticholinergic effects Contraindicated in glaucoma, myasthenia gravis o Carisoprodol Aka Soma Is metabolized to meprobamate, a controlled substance w/physical and psychological dependence No better than any other skeletal muscle relaxants DO NOT USE!!!!! o Be aware with all antispasmodic agents of SEDATION Advice your patients to use caution when driving or operating heavy machinery o Evidence of effectiveness of antispasmodic agents They are effective in acute low-back pain and roughly equivalent to NSAIDS (which is why you should administer NSAIDS first) We are not sure whether the pain relief effects are due to muscle relaxation or simply the sedation caused by the drug Using a skeletal muscle relaxant ALONGSIDE an NSAID is better than using either one alone