* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Non-Cardiac Chest Pain - Old
Discovery and development of TRPV1 antagonists wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Drug design wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Drug discovery wikipedia , lookup
Epinephrine autoinjector wikipedia , lookup
Drug interaction wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
NMDA receptor wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Theralizumab wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Toxicodynamics wikipedia , lookup
Norepinephrine wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Psychopharmacology wikipedia , lookup
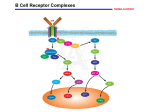
Neurotransmitters Pharm Pearl: The peripheral nervous system (PNS) employs 3 neurotransmitters • Acetylcholine • Norepinephrine • Epinephrine Any given junction in the PNS uses only ONE of these substances 2 Transmitter Recap Acetycholine – employed at most junctions of the PNS • All preganglion neurons of PNS • All preganglion neurons of the SNS • All postganglionic neurons of PNS • All motor neurons to skeletal muscles • Most postganglionic neurons of the SNS that go to sweat glands 3 Transmitter Recap Norepinephrine – released by practically all postganglionic neurons of the SNS (exception – sweat glands) Epinephrine – major neurotransmitter released by the adrenal medulla. The adrenal medulla also releases some norepinephrine. 4 Adrenergic Agonists * Produce their effects by activating adrenergic receptors * Sympathomimetic * Broad spectrum of applications • CHF • Asthma • Preterm labor Mechanisms of Adrenergic Receptor Activation * Direct receptor binding * Promotion of norepinephrine (NE) release * Inhibition of NE reuptake * Inhibition of NE inactivation Overview of Adrenergic Agonists * Therapeutic applications and adverse effects of adrenergic receptor activation * Properties of representative adrenergic agonists * Discussion of adrenergic agonists in other chapters Overview of the Adrenergic Agonists Catecholamines Noncatecholamines • Cannot be used orally • Brief duration of action • Cannot cross the BBB (polar molecules) • Can be given orally • Metabolized slowly by MAO – longer half-life • More able to cross the BBB Mort & Merv: the story of selectivity Receptor specificity • Most drugs in chapter • Peripherally acting sympathomimetic • Direct receptor activation • Amphetamine, cocaine • Indirect acting sympathomimetic • Ephedrine • Direct receptor activation and promotion of NE release Receptor Specificity Terbutaline (Bricanyl) Isoproterenol (Isuprel) Epinephrine • Beta2 only •Beta1 and beta2 •Alpha1 and alpha2 •Beta1 and beta2 Therapeutic Applications Adrenergic Agonists Clinical applications of alpha1 Two responses for therapeutic use • Vasoconstriction (most common use) • • • • Blood vessels Skin Viscera Mucous membranes Mydriasis Therapeutic Applications and Adverse Effects of Adrenergic Receptor Activation * Drugs capable of activating alpha1 receptors • • • • • Epinephrine Norepinephrine (Levophed) Phenylephrine (Neosynephrine) Ephedrine Dopamine Therapeutic Applications and Adverse Effects of Adrenergic Receptor Activation Therapeutic applications of alpha1 activation * Hemostasis • Arrest bleeding via vasoconstriction * Nasal decongestion • Mucosal vasoconstriction * Adjunct to local anesthesia • Delays absorption of local anesthetic * Elevation of blood pressure • Vasoconstriction Mydriasis • Radial muscle of the iris Therapeutic Applications and Adverse Effects of Adrenergic Receptor Activation Adverse effects of alpha1 activation * Hypertension • Widespread vasoconstriction * Necrosis • Treatment with alpha1 blocking agent Bradycardia • Response to vasoconstriction and elevated BP Clinical Consequences of Alpha2 Activation * Alpha2 receptors in periphery • Located presynaptically • Regulate transmitter release • Activation inhibits NE release * Alpha2 in CNS • Reduction of sympathetic outflow to heart and blood vessels • Relief of severe pain Clinical Consequences of Beta1 Activation Therapeutic applications of beta1 activation * Cardiac arrest • Not preferred drug of choice * Heart failure • Positive inotropic effect * Shock • Positive inotropic effect; increases heart rate Atrioventricular heart block • Enhances impulse conduction through AV Clinical Consequences of Beta1 Activation * Adverse effects of beta1 activation • Altered heart rate or rhythm - Tachycardias or dysrhythmias • Angina pectoris - Increased cardiac oxygen demand Clinical Consequences of Beta2 Activation * Therapeutic applications of beta2 activation • Asthma • Delay of preterm labor * Adverse effects of beta2 activation • Hyperglycemia • Tremor Clinical Consequences of Dopamine Receptor Activation * Activation of peripheral dopamine receptors causes dilation of the vasculature of the kidneys Multiple Receptor Activation: Treatment of Anaphylactic Shock * Pathophysiology of anaphylaxis • Severe allergic response • Hypotension, bronchoconstriction, edema of the glottis * Treatment • Epinephrine, injected IM, is the treatment of choice for anaphylactic shock Adrenergic Agonists * * * * * * * * Epinephrine Norepinephrine Isoproterenol Dopamine Dobutamine Phenylephrine (Neo-synephrine) Terbutaline Ephedrine Epinephrine * Therapeutic uses • • • • • • • • Delay absorption of local anesthetic Control superficial bleeding Elevate blood pressure Mydriasis during ophthalmologic procedures Overcome AV block Restore cardiac function in arrest Bronchial dilation in asthma Treatment of choice for anaphylactic shock Epinephrine * Pharmacokinetics • Absorption • Inactivation * Adverse effects • • • • • Hypertensive crisis Dysrhythmias Angina pectoris Necrosis following extravasation Hyperglycemia Epinephrine * Drug interactions • • • • • MAO inhibitors Tricyclic antidepressants General anesthetics Alpha-adrenergic blocking agents Beta-adrenergic blocking agents Epinephrine * Preparations, dosage, & administration EpiPen (1:1000 or 1:2000) IV (monitor closely) (1:10,000) IM SubQ Intracardiac Intraspinal Inhalation Topical Norepinephrine * Receptor specificity • Alpha1 • Alpha2 • Beta1 * Chemical classification • Catecholamine * Therapeutic uses • Hypotensive states • Cardiac arrest Norepinephrine * Differs from epinephrine – does not activate beta2 receptors • Does not promote hyperglycemia * Cannot be given orally (MAO and COMT) * Necrosis with extravasation * Drug interactions • MAOI, TCA, general anesthetics, adrenergic blocking agents Isoproterenol * Receptor specificity: beta1 and beta2 * Chemical classification: catecholamine * Therapeutic uses • Cardiovascular - AV heart block, arrest • Asthma - Bronchodilation – not used anymore • Bronchospasm - During anesthesia Isoproterenol * Adverse effects • Fewer than those of NE or epinephrine (doesn’t activate alpha-adrenergic receptors) • Tachydysrhythmias and angina pectoris • Hyperglycemia in diabetes patients * Drug interactions • MAOI, TCA, beta-adrenergic blockers * Preparations and administration • IV, IM, and intracardiac injections Dopamine * Receptor specificity • Low therapeutic dose – dopamine • Moderate therapeutic dose – dopamine and beta1 • Very high dose – apha1, beta1, and dopamine Dopamine Therapeutic uses * Shock • • Increases cardiac output Increases renal perfusion * Heart failure • Increases myocardial contractility * Acute renal failure • • Was used to preserve renal function with ARF Early ARF – failed to protect renal function, shorten stays, or reduce need for renal transplant Dopamine * Adverse effects • Tachycardia, dysrhythmias, anginal pain • Necrosis with extravasation * Drug interactions • MAOI, TCA, certain general anesthetics, diuretics * Preparations, dosage, and administration • Preparations: dispensed in aqueous solutions • Dosage: must be diluted • Administration: administered by IV Dobutamine Receptor specificity: beta * 1 * Chemical classification: catecholamine * Actions and uses • CHF * Adverse effects • Tachycardia * Drug interactions • MAOI, TCA, certain general anesthetics * Preparations, dosage, and administration • Continuous IV infusion Phenylephrine * Receptor specificity • Alpha1 * Chemical classification Noncatecholamine * Therapeutic uses • • • • Reduce nasal congestion (locally) Elevate blood pressure (parenterally) Dilate pupils (eye drops) Local anesthetic (delay absorption) Terbutaline * Receptor specificity: beta2 * Chemical classification: noncatecholamine * Therapeutic uses • Asthma (selective for beta2) - Replaced isoproterenol in treatment • Delay of preterm labor - Relaxes uterine smooth muscle - Another drug (ritodrine) now preferred * Adverse effects - Minimal at therapeutic doses - Tremor most common; also tachycardia What’s he got to do with Pharm? Anybody ever taken ephedrine? Are you sure? Ephedrine * Receptor specificity: alpha1, alpha2, beta2 * Chemical classification: noncatecholamine * Therapeutic uses • Nasal congestion • Other uses * Adverse effects • HTN, dysrhythmias, angina, hyperglycemia, insomnia (crosses BBB) Good thing gone bad… Questions