* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 6
Biological neuron model wikipedia , lookup
Perception of infrasound wikipedia , lookup
Resting potential wikipedia , lookup
NMDA receptor wikipedia , lookup
Neuromuscular junction wikipedia , lookup
Optogenetics wikipedia , lookup
Electrophysiology wikipedia , lookup
End-plate potential wikipedia , lookup
Circumventricular organs wikipedia , lookup
Synaptogenesis wikipedia , lookup
Endocannabinoid system wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Signal transduction wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Channelrhodopsin wikipedia , lookup
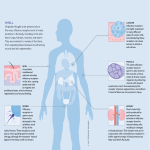
BIO2305 Peripheral Nervous System (PNS) Afferent Division Part 1 PNS – all neural structures outside the brain and spinal cord. Provides links to and from the external environment. Includes: sensory receptors peripheral nerves associated ganglia motor endings Organization of the Nervous System Afferent Pathway- transmit impulses from PNS to CNS Properties of Sensory Systems • Stimulus – Internal--interoceptors – External --exteroceptors – Energy source—heat, light, sound, pressure • Receptors - Afferent pathway ( from PNS to CNS) – Sense organs – Transducer • CNS integration 1 From Sensation to Perception • Survival depends upon sensation and perception • Sensation is the awareness of changes in the internal and external environment • Perception is the conscious interpretation of those stimuli Sensory Receptors: Transducers • Transduction - stimulus energy converted into information processed by CNS • Sensory receptors are structures specialized to respond to stimuli, activation results in – Ion channels or second messengers that initiate membrane potential change is sensory receptors – Depolarizations trigger impulses to the CNS • The realization of these stimuli, sensation and perception, occur in the brain Sensory Receptor Types Classification of receptors can be classified by stimulus • Mechanoreceptors – respond to touch, pressure, vibration, stretch, and itch • Thermoreceptors – sensitive to changes in temperature • Photoreceptors – respond to light energy (e.g., retina) • Chemoreceptors – respond to chemicals (e.g., smell, taste, changes in blood chemistry) • Nociceptors – sensitive to pain-causing stimuli • Osmoreceptors – detect changes in concentration of solutes, osmotic activity 2 Receptors • The receptor must have specificity for the stimulus energy • The receptor’s receptive field must be stimulated • Stimulus energy must be converted into a graded potential • A generator potential in the associated sensory neuron must reach threshold Conversion of Receptor & Generator Potentials into Action Potentials • Generator potentials – Occur in specialized nerve endings – Stimulus opens ion channels in receptor causing local current flow – Local current flow opens ion channels in afferent neuron AP generating region – If threshold reached, AP is generated • Receptor potentials – Occur in separate receptor cells – Stimulus opens ion channels in receptor causing graded membrane potential – Receptor cell releases chemical messenger – Chemical messenger opens ion channels in afferent neuron AP generating region – If threshold reached, AP is generated Receptor Potential Generator Potential Sensory Pathways Stimuli exist in a variety of energy forms or modalities – heat, light, sound, pressure, chemical etc. • Stimulus as physical energy sensory receptor – Receptor acts as a transducer • Intracellular signal usually change in membrane potential • Stimulus > threshold action potential to CNS • Integration in CNS cerebral cortex or acted on subconsciously Transduction The process of converting energy forms into electrical signals via a generator potential which triggers an action potential if it is large enough to reach threshold. A generator potential is a type of graded potential similar to an EPSP 3 Sensory Pathways -- External Stimuli • Vision • Hearing • Taste • Smell • Equilibrium • Somatic Senses Somatic Senses—Internal Stimuli • Touch • Temperature • Pain • Proprioception 4 Somatic Pathways • First-order neurons – soma reside in dorsal root or cranial ganglia, and conduct impulses from the skin to the spinal cord or brain stem • Second-order neurons – soma reside in the dorsal horn of the spinal cord or medullary nuclei and transmit impulses to the thalamus or cerebellum • Third-order neurons – located in the thalamus and conduct impulses to the somatosensory cortex of the cerebrum Sensory Coding • Modality – type of stimulus • Location – Coded by site of the stimulated receptor – Precision of location called acuity, • Receptive field • Lateral inhibition • Intensity – Increased stimulus results in a larger receptor potential leading to a higher frequency of action potential – Stronger stimuli also affect a larger area and recruit a larger number of receptors • Duration - Adaptation – Tonic receptors – Phasic receptors Receptive field = area within which a receptor can detect a stimulus 5 Receptive Fields of Sensory Neurons Receptive Field: Two-point discrimination 6 Lateral inhibition To facilitate localization and sharpen contrast, the most strongly activated pathway at the center inhibits the less excited pathways from the fringe areas Sensory Coding: Stimulus Intensity & Duration • Intensity - coded by number of receptors activated and frequency of action potentials • Duration - coded by duration of action potentials • Some receptors can adapt or cease to respond Amplitude Membrane potential (mV) (a) Stimulus (b) Longer and stronger stimulus Membrane potential (mV) Duration 20 0 -20 -40 -60 -80 20 0 -20 -40 -60 -80 Threshold 0 5 10 0 5 10 Time (sec) 0 5 10 0 5 10 Threshold 0 5 10 0 5 10 7 Adaptation Occurs when sensory receptors are subjected to an unchanging stimulus o Receptor membranes become less responsive o Receptor potentials decline in frequency or stop. Adaptation occurs in the receptor, not the CNS Tonic receptors o Do not adapt at all or very slowly, important when maintaining information about a stimulus is valuable – stretch, pain receptors Phasic receptors o Rapidly adapt, useful in situations where it is important to signal a change in stimulus – tactile (touch) receptors Sensory Adaptation • Tonic receptors (Pain): – Produce constant rate of firing as long as stimulus is applied • Phasic receptors: – Burst of activity but quickly reduce firing rate (adapt) if stimulus maintained. – Sensory adaptation: cease to pay attention to constant stimuli. 8 Adaptation • Receptors responding to pressure, touch, and smell adapt quickly • Receptors responding slowly include Merkel’s discs, Ruffini’s corpuscles • Pain receptors and proprioceptors do not exhibit adaptation Adaptation mechanisms 1. Mechanical – specialized receptor ending consists of concentric layers of connective tissue. Sustained pressure causes layers to slip, dissipating stimulus intensity 2. Chemical – Na+ channels that initial opened are slowly inactivated Tactile Receptors (pressure) • Mechanoreceptors • Free nerve endings – Lamellated (Pacinian) corpuscles - rapidly adapting skin receptor that detects pressure and vibration. – Corpuscle of touch (Meissner‘s) - receptor for discriminative touch – Type I cutaneous (Merkel) receptors for discriminative touch – Type II cutaneous(Ruffini) receptor for continuous touch sensation – Baroreceptors – receptors to detect pressure changes in blood vessels 9 Proprioceptors Located in muscles, tendons, joints and internal ear and provide information about body position and movement. • Muscle spindle – In muscles – Sense stretch • Golgi tendon organ – Near tendon – Sense force • Joint receptors – Sense position & pressure Muscle spindle structure • Consist of collections of specialized muscle fibers known as intrafusal fibers – Lie within spindle-shaped connective tissue capsules parallel to extrafusal fibers – Each spindle has its own private efferent and afferent nerve supply – Play key role in stretch reflex – Muscle spindles monitor changes in length of muscle by responding to the rate and degree of change 10 Tendon Organs (Golgi tendon organs) Consists of sensory fiber penetrating a thin capsule of connective tissue and entwining around a few collagen fibers Found at the junctions of a tendon with a muscle Help protect tendons and associated muscles from damage due to excessive tension or stretching Stretch Reflex Primary purpose is to resist tendency for passive stretch of extensor muscles by gravitational forces when person is standing upright Classic example is patellar tendon, or knee-jerk reflex Pain • • • • Nociceptors- protective mechanism Reflexive path Fast pain Slow pain 11 Pain Receptors Three types of receptors (nociceptors) - mechanical, thermal, polymodal All are naked nerve endings and do not adapt All can be sensitized by prostaglandins (increase pain) • Prostaglandins derived from lipid bilayer of membrane released from damaged tissues Mechanical (crushing, cutting, pinching) and thermal (extreme temperatures) are transmitted over small myelinated A-delta fibers – 30m/sec fast pain pathway Polymodal respond to all kinds of damaging stimuli and is carried by small unmyelinated C-fibers 12m/sec slow pain pathway Nociceptive Transmission Pathway: Fibers • A-Delta – Small, thinly myelinated. – 10 % sensory pain fibers. – Conduct at 5-30 m/sec. – Mechanical and thermal stimuli. – Sensations of sharp, pricking pain. • C Fibers – Small, unmyelinatd fibers. – 90% of afferent sensory fibers. – Conduct at 0.5-2.0 m/sec. – Mechanical, thermal, chemical. – Long lasting, burning pain. Ad and C Nociceptors Mediate Pain C-fiber A fiber First pain Second pain Pain intensity Time 12 Neurotransmitters in Spinal Cord • Key nociceptor transmitter is substance P. – Activates ascending pathways that transmit nociceptor impulses. • Glutamate: – Binds to AMPA receptors, increases permeability, increasing likelihood of AP. – Binds to NMDA receptors increases excitability of dorsal horn neurons. Processing of pain - Afferent pathway • 1st order pain neurons use substance P and glutamate as neurotransmitters • Stimulus > nociceptor – substance P > spinal cord neuron >brainstem > thalamus > somatosensory cortex • Glutamate released from primary afferent pain terminals – major excitatory NT (similar to LTP mechanism) exaggerated sensitivity of an injured area to subsequent stimulus. • Built in analgesic system- periaqueductal gram matter >> RAS >> Endogenous opiate >> Inhibitory opiate receptor>> suppresses release of substance P Spinal Cord: Excitatory Transmitters Spinothalamic Tract DRG Substance P Glutamate 2nd Order Neuron 13 2305 Chapter 6 – Afferent Division Part 2: Special Senses Special Senses – External Stimuli • Vision • Hearing • Taste • Smell • Equilibrium Anatomy Review of the Eye • Outer coat of the eyeball is called the fibrous tunic consisting of the cornea - avascular, transparent coat that covers the iris and sclera, the white coat of dense connective tissue covering the remainder of the eye. • Lens - nonvascular structure made up of proteins called crystallins. It lies behind the iris and is held in position by suspensory ligaments. o The lens divides the interior of the eyeball into an anterior cavity and a vitreous chamber. Anterior cavity is filled with a watery fluid called the aqueous humor and further divided into 1. anterior chamber - lies behind the cornea and in front of the iris 2. posterior chamber - lies behind iris and in front of suspensory ligaments The vitreous chamber is filled with a jelly-like substance called vitreous body • Ciliary body - thick anterior portion consisting of ciliary processes which secrete aqueous humor and ciliary muscles which alters the shape of the lens for accommodation • Iris - colored portion suspended between the cornea and lens and attached to the ciliary body, it consists of circular and radial muscles, the hole in the center of the iris is the pupil, and it functions to regulate the amount of light entering the eye. • Choroid - highly pigmented (black-brown appearance) epithelium, vascularized posterior portion, absorbs scattered light that might distort image. • The third layer or inner coat is the retina (nervous tunic) which lines the posterior three fourths of the eyeball • Slightly off center in the retina is the optic disc (blind spot) where the optic nerve exits the eyeball. 14 Cross Section of the Eye Organization of the Retina The Structure of the Eye • Modifies light before it is detected by the rods & cones. The light level is altered by changing the size of the pupil and light waves are focused by changing the shape of the lens. Electromagnetic Spectrum • Extends from high energy short wavelength gamma rays to low energy long wavelength radio waves. Human visible light lies only within the range ~380-750 nm 15 Vision • Light enters the eye through the pupil, diameter of pupil modulates light • Shape of lens focuses the light on the retina • Retinal rods and cones are photoreceptors • Reflected light translated into mental image Pupils • Bright light they constrict to ~ 1.5 mm • Dark they dilate to ~ 8 mm. • Controlled by the autonomic nervous system, pupillary reflex Image Projection The image projected onto the retina is inverted or upside down. Visual processing in the brain reverses the image 16 • Convex structures of eye produce convergence of diverging light rays that reach eye Refraction of Light • The eye refracts the entering light to focus the image on the retina. • Refraction by the cornea and lens form an image on the retina by bending light rays due to the light passing through media of different densities at an angle. • Constriction of the pupil prevents light from entering the eye through the periphery. • The curved corneal surface contributes most of the refractive ability of the eye 17 Optics Mechanism of Accommodation Accommodation is the process by which the eye adjusts the shape of the lens to keep objects in focus Ability to adjust strength of the lens is known as accommodation which depends on its shape which is regulated by the ciliary muscle Mechanism of Accommodation When the ciliary muscle is relaxed the lens is flattened, when it contracts the lens takes more of a spherical shape. An increase in curvature is needed for near vision 18 Common Visual Defects Myopia - near sighted, far light source is focused in front of retina and appears blurry Hyperopia – far sighted, near objects are focused “behind” the retina appearing blurry Presbyopia - loss of elasticity – the lens can no longer assume the spherical shape required to accommodate for near vision. Normally occurs in middle aged people Retina Specialized photoreceptor cells, rods & cones, found within the retina transduce visible light energy into electrical signals that ultimately pass to the visual cortex. • Photoreceptors - rods and cones detect light stimulus • Bipolar - generate APs • Amacrine & Horizontal cells – local integration of APs • Ganglion cells converge form optic nerve Retinal Layers • Photoreceptor layer - Rod and cone cells specialized to transduce light • Rods - predominate in peripheral areas and cones - are densely concentrated in the fovea - the center of the visual field • Bipolar cell layer - The cells in this layer establish pathways for nerve impulses. Horizontal cells transmit inhibitory signals to bipolar cells. Bipolar cells and Amacrine cells produce graded potentials to ganglion cells which may depolarize and initiate action potentials • Ganglion cell layer - neurons whose axons merge to form the optic nerve which passes through the optic disc and optic tract to thalamus which passes the visual information to the occipital lobe. 19 Retina Photoreceptors Neurons Amacrine cell Optic nerve Ganglion fibers cell Cone Rod Horizontal cell Bipolar cell Pigmented epithelium Photoreceptors • Rods - light-sensitive but don’t distinguish colors; monochromatic, night vision • Cones - Three types; red, green, & blue, distinguish colors but are not as sensitive, high acuity day vision; respond to selectively various wavelengths of light • Color vision depends on the three cone types various ratios of stimulation in response to different wavelengths • Photoreceptors contain photopigments which absorb various wavelengths of light. They are made up of two components: • opsin – a protein that is an integral part of the disc membrane • retinene, derivative of Vitamin A that is bound within the interior of the opsin molecule 20 Rods v. Cones • 30 times more rods than cones (100 million to 3 million) • Cones used for color perception, have low sensitivity to light, being turned on only by bright light but they have visual acuity, there is very little convergence of cones in retinal pathway • Rods used for shades of gray, have low acuity but high sensitivity (high convergence) so they respond to dim light • Dark adaptation - phenomena involving switching between rods and cones Dark & Light Adaptation • Sensitivity to light based on the amount of photopigment present in rods and cones. Breakdown of photopigments during exposure to bright light tremendously decreases photoreceptor sensisitivity • Dark adaptation: In dark, the photopigments broken down during light exposure are gradually regenerated. Sensitivity gradually increases so that you begin to see in the darkened surroundings – only highly sensitive rejuvenated rods are turned on by the dim light • Light adaptation: when transitioning from dark to high levels of light, the increased amount photopigment produced during dark causes extreme sensitivity and images appear “bleached out.” After photopigments broken down, normal contrast reappears Phototransduction • Conversion of light in to electrical signals • Each rod or cone contains visual pigments consisting of a light-absorbing molecule called retinal bonded to a protein called opsin Rod Outer segment Disks Cell body Inside of disk cis isomer Light Enzymes Synaptic terminal Cytosol Retinal Rhodopsin Opsin trans isomer 21 Phototransduction • Rods contain the pigment rhodopsin, which changes shape when absorbing light • Photons "bleach" opsin, retinal changes shape and released, transduction cascade, decreased cGMP, Na+ channel closes, K+ opens , hyperpolarization reduces NT release (a) In darkness, rhodopsin is inactive, cGMP is high, and ion channels are open. (b) Light bleaches rhodopsin. Opsin decreases cGMP, closes Na+ channels, and hyperpolarizes the cell. Activated retinal Pigment epithelium cell Opsin (bleached pigment) (c) In the recovery phase, retinal recombines with opsin. Activates transducin Retinal converted to inactive form Disk Transducin (G protein) Inactive rhodopsin (opsin and retinal) Cascade Decreased cGMP cGMP levels high Na+ Na+ channel closes Na+ K+ Retinal recombines with opsin to form rhodopsin. K+ Membrane hyperpolarizes to -70 mV. Membrane potential in dark = -40mV Light Tonic release of neurotransmitter onto bipolar neurons Neurotransmitter decreases in proportion to amount of light. 22 Phototransduction Light INSIDE OF DISK Active rhodopsin EXTRACELLULAR FLUID PDE Plasma membrane Membrane potential (mV) 0 Dark Light Inactive rhodopsin Transducin Disk membrane cGMP –40 GMP Na+ Hyperpolarization –70 Time CYTOSOL Na+ • • • • In the dark, rods and cones release the neurotransmitter glutamate into synapses with neurons called bipolar cells Bipolar cells are hyperpolarized In the light, rods and cones hyperpolarize, shutting off release of glutamate The bipolar cells are then depolarized Dark Responses Light Responses Rhodopsin inactive Rhodopsin active Na+ channels open Na+ channels closed Rod depolarized Rod hyperpolarized Glutamate released No glutamate released Bipolar cell hyperpolarized Bipolar cell depolarized 23 Summary • In the absence of light the Na+ channels stay open due to the binding of second messenger cGMP causing depolarization, keeping Ca+ channels open at the synaptic terminals which continually produce NT glutamate which inhibits the bipolar cells. • When light hits retinene it changes shape and activates the photopigment which activates a G protein called transducin which activates an enzyme that degrades cGMP which permits the chemically gated Na+ to close which hyperpolarizes the receptor potential lead to closure of the Ca+ gates and reduction of NT. • Photoreceptors hyperpolarize on light absorption! Opposite of normal receptor mechanism • Removal of inhibition has the same effect as direct excitation of the bipolar cell • Greater the illumination, the greater the removal of inhibition of the bipolar cell, the greater excitation of these cells Convergence and Ganglion Cell Function The Retina & Visual Acuity Light adapted eye has greatest visual acuity at the fovea Photopic vision (cones) Dark adapted eye has least visual acuity at the fovea but has greater acuity in the parafoveal region Scotopic vision (rods) Fovea 24 Visual Integration/Pathway Retinal cells 2x binocular vision plus accessory structures Optic disk - blood supply optic nerve Retina Vision Integration / Pathway • Optic nerve • Optic chiasm • Optic tract • Thalamus • Visual cortex Afferent pathway rods or cones >> bipolar cells>> ganglion cell axons >>fibers from each medial retina chiasm>> fibers from both retinas >> optic tracts terminate in midbrain and thalamus >> optic radiation carries information from thalamus to primary visual cortex 25 The Ear/Auditory Physiology External Ear: Structures & Functions • Pinna—Collects sound waves and channels them into the external auditory canal. • External Auditory Canal— directs the sound waves toward the tympanic membrane. • Tympanic membrane— receives the sound waves and transmits the vibration (bows in & out according to frequency) to the ossicles of the middle ear Middle Ear: Structures & Functions • Middle ear houses the malleus, incus, and stapes which transfer the vibratory movements of the TM to the fluid of the middle ear. • The stapes is attached to the oval window, the entrance to the cochlea – the “hearing” portion of the inner ear • As the oval window is pushed in and out, the resultant pressure produces wavelike movements in the inner ear fluid at the same frequency as the original sound waves. 26 Cochlear Anatomy • The cochlea is a coiled tubular system lying deep within the temporal bone. It is divided lengthwise into three fluid filled compartments. 1. Cochlear duct (scala media) the middle compartment filled with endolymph fluid 2. Scala vestibuli, upper compartment filled with perilymph fluid 3. Scala tympani, lower compartment also filled with perilymph • The round window seals the scala tympani from the middle ear. • The vestibular membrane forms the ceiling of the cochlear duct and separates it from the scala vestibule, the basilar membrane forms the floor of the cochlear duct – holds the organ of Corti Sound and Hearing • Sound waves – traveling vibrations of air that consist of regions of high pressure (compression) and low pressure (rarefraction) • Pitch (tone) determined by frequency, intensity (loudness) depends on amplitude • Hearing – neural perception of sound energy – what and where • Sound waves travel toward tympanic membrane, which vibrates • Auditory ossicles conduct the vibration into the inner ear • Movement at the oval window applies pressure to the perilymph of the cochlear duct • Pressure waves move through vestibular membrane through endolymph to distort basilar membrane • Hair cells of the Organ of Corti are pushed against the tectorial membrane The Organ of Corti • The organ of Corti contains sound receptors called hair cells (~16,000). There are three rows of outer hair cells and one row of inner hair cells • Protruding from each hair cell are about 100 hairs called stereocilia which are mechanically embedded in the tectorial membrane which hangs over the organ of Corti. • The inner hair cells transform the mechanical forces of sound into electrical impulses of hearing – transduction 27 Cochlea & Organ of Corti Organ of Corti • Ion channels open, depolarizing the hair cells, releasing glutamate that stimulates a sensory neuron. • Greater displacement of basilar membrane, bending of stereocilia; the greater the amount of NT released. • Increases frequency of APs produced. 28 Summary 1. Sound waves enter the external auditory canal, strike the tympanic membrane vibrating the auditory ossicles. 2. The ossicles mechanically amplify the vibrations and then strike the oval window 3. The oval window acts like a piston by creating fluid pressure waves in the perilymph of the cochlea. 4. The fluid pressure of perilymph in the scala vestibuli is transmitted to the scala tympani and eventually to the round window. 5. The pressure waves push against the vestibular membrane causing the fluid pressure of the endolymph inside the cochlear duct to increase and decrease. 6. The pressure fluctuations of the endolymph vibrates the basilar membrane which moves the hair cells of the spiral organ against the tectorial membrane The bending of the microvilli produces receptor potentials that lead to the generation of nerve impulses to vestibulocochlear nerve which passes to the thalamus and then to the temporal lobes. 7. The mechanical deformation of the hairs alternately opens and closes mechanically gated ion channels in the hair cells resulting in alternating depolarization and hyperpolarization changes in potential. 8. The inner hair cells synapse on afferent neurons of the auditory nerve. 9. Bending of the hair cells in one direction causes depolarization which increases the rate on NT release, which increases the rate of firing of afferent neurons 10. Hyperpolarization causes less NT to be released when the hair cells are displaced in the opposite direction Signal Transduction in Hair Cells • The apical hair cell is modified into stereocilia 29 Pitch Discrimination • Different frequencies of vibrations (compression waves) in cochlea stimulate different areas of Organ of Corti • Displacement of basilar membrane results in pitch discrimination. Cochlea (uncoiled) Basilar Apex membrane (wide and flexible) 500 Hz (low pitch) 1 kHz 2 kHz 4 kHz 8 kHz 16 kHz (high pitch) Base (narrow and stiff) Frequency producing maximum vibration Sensory Coding for Pitch • Waves in basilar membrane reach a peak at different regions depending upon pitch of sound. • Sounds of higher frequency cause maximum vibrations of basilar membrane. Vestibular Apparatus • Detects position and motion of the head • Consists of the semicircular canals and the otolith organs 30 Vestibular Apparatus Vestibular apparatus provides information about movement and position in space Vestibular Apparatus • Cristae are receptors within ampullae that detect rotational acceleration • Maculae are receptors within utricle and saccule that detect linear acceleration and gravity 31 Vestibular Apparatus: Semicircular Canals • Provide information about rotational acceleration. – Project in 3 different planes Semicircular Canals • Endolymph provides inertia so that the sensory processes will bend in direction opposite to the angular acceleration 32 Rotational Forces in the Cristae Semicircular Canals Summary • Semicircular canals detect rotational or angular acceleration- change of movement. It consists of three circular canals arranged in planes that lie at right angles to each other, they are filled with endolymph • The receptive hair cells are located in the ampulla. The hair cell holds 20-50 microvilli (stereocilia) and one cilium – the kinocilium which are embedded in cupula –a caplike gelatinous layer • When the head is set in motion the cupula moves through the fluid which does not initially move due to inertia, causing the cupula to sway or bend. • At constant speed, the fluid eventually catches up with the ampulla and the ampulla returns to resting position. • When motion of the head stops, the ampulla stops, but the fluid lags behind causing the ampulla to be bent in the opposite direction (similar to the motion of seaweed during the tide) • Each hair cell is oriented so that it depolarizes when the stereocilia are bent toward the kinocilium, bending in the opposite direction hyperpolarizes. The hair cells synapse on the vestibular nerve Otolith Organs: Maculae • The otolith organs sense linear acceleration and head position 33 Otolith Organs Stereocilia and Kinocilium • When stereocilia bend toward kinocilium; membrane depolarizes, and releases NT • When bends away from kinocilium hyperpolarization occurs • Frequency of APs carries information about movement 34 Maculae of the Utricle and Saccule • Utricle: – More sensitive to horizontal acceleration. • During forward acceleration, otolithic membrane lags behind hair cells, so hairs pushed backward. • Saccule: – More sensitive to vertical acceleration. • Hairs pushed upward when person descends. Summary of Otolith Organs • Provides information on the position of the head relative to gravity and linear acceleration • The otolith organs, utricle and saccule are situated between the semicircular canals and the cochlea. • The hairs of the receptors in these organs also protrude into an overlying gelatinous sheet whose movement displaces the hairs and results in changes in hair cell potential • Tiny crystals of calcium carbonate (otoliths) are suspended in the layer making it heavier and giving it more inertia than the surrounding fluid • Utricle hairs are oriented vertically and the saccule hairs are lined up horizontally • Utricle hairs - when the head is tilted in any direction other than vertical, the hairs are bent in the direction of the tilt because of the gravitational force pulling on the top heavy gelatinous layer – The utricle hairs are also displaced by any change in linear motion because the top heavy layer labs behind the endolymph and hair cells causing the hairs to bend in the opposite direction of head movement. • The saccule functions similarly except that it responds to the tilting of the head away from a horizontal position (getting out of bed) Taste (Gustation) • • • Taste Receptors - Clustered in taste buds (~10,000) Associated with lingual papillae Taste buds – Contain basal cells which appear to be stem cells – Gustatory cells extend taste hairs through a narrow taste pore 35 • • • • • • • • • Epithelial cell receptors clustered in barrel-shaped taste buds Each taste bud consists of 50-100 specialized epithelial cells (taste receptor cells) • Each taste bud has a taste pore from which fluid in the mouth can contact the receptor cells • The receptor cells are modified epithelium with many surface folds (mircovilli) to increase surface area. Epithelial cells differentiate into supporting cells and then into receptor cells. Taste receptors have a life span of about ten days Taste cells are not neurons, but depolarize upon stimulation and if reach threshold, release NT that stimulate sensory neurons. Each taste bud contains taste cells responsive to each of the different taste categories. A given sensory neuron may be stimulated by more than 1 taste cell in # of different taste buds One sensory fiber may not transmit information specific for only 1 category of taste Brain interprets the pattern of stimulation with the sense of smell; so that we perceive complex tastes The microvilli plasma membranes contain receptor sites that bind selective chemical molecules (tastants). Binding of a tastant with the receptor site produces a depolarizing receptor potential Terminal afferent endings of several cranial nerves synapse with taste buds in various regions of the mouth. The nerves relay to the brain stem and thalamus and on the cortical gustatory area Taste Receptor Distribution • Taste discrimination is base on varying combination of four primary tastes: salt, sour, sweet, bitter and perhaps a fifth umami. Receptor cells use different pathways to bring about depolarization 36 • • • • • • Salty: – direct entry of Na+ is responsible for – Na+ passes through channels, activates specific receptor cells, depolarizing the cells, and releasing NT. Sour: – H+ ion block K+ channels, the decrease in K+ produces depolarization – Presence of H+ passes through the channel, opens Ca+ channels Sweet and bitter: – Mediated by receptors coupled to G-protein (gustducin). Sweet – sugars –glucose and others bind with a taste receptor that activates a G protein which turns on cAMP second messenger pathway which ultimately blocks K+ channels Bitter – alkaloids, poisons also activate a G protein (gastducin) which sets off a second messenger pathway similar to the visual G protein Umami – triggered by amino acids that activate a G protein pathway but is yet unknown 37 Summary of Taste Transduction Smell/Olfaction • • • • Olfactory epithelium with olfactory receptors, supporting cells, basal cells • Basal cells are precursors to new olfactory receptors which are replaced every two months Unlike other special senses, olfactory receptors are specialized endings of afferent neurons • The axons of the olfactory receptor cell collectively form the olfactory nerve Surfaces are coated with secretions from olfactory glands Olfactory reception involves detecting dissolved chemicals as they interact with odorant binding proteins 38 Olfactory Receptors • Bipolar sensory neurons located within olfactory epithelium – Dendrite projects into nasal cavity, terminates in cilia – Axon projects directly up into olfactory bulb of cerebrum – Olfactory bulb projects to olfactory cortex, hippocampus, and amygdaloid nuclei Olfaction • Neuronal glomerulus receives input from 1 type of olfactory receptor • Odorant molecules bind to receptors and act through G-proteins to increase cAMP. – Open membrane channels, and cause generator potential; which stimulates the production of APs. – Up to 50 G-proteins may be associated with a single receptor protein. – G-proteins activate many G- subunits - amplifies response 39 Olfaction Overview • The receptor portion of an olfactory receptor cell consists of an enlarged knob bearing several long cilia that extend like a tassle to the surface of the mucosa. • The cilia contain binding sites for the attachment of odorants – molecules that can be smelled, they must sufficiently volatile (vaporized) and water soluble to dissolve in the mucosa • Human nose contains 5 million receptors of about 1000 different types. Each receptor responds to only one discrete component of an odor- the odor is dissected. A given receptor can respond to particular odor component shared in common by different scents • Binding of an appropriate scent signal to an olfactory receptor activates a G protein triggering cAMP cascade leading to Na + gates to open bringing about a depolarizing receptor potential that can generate and action potential in the afferent fiber. • The afferent fiber synapse in the olfactory bulb, each bulb is lined by neural junction called glomeruli (little balls) • The glomeruli serve as the first relay station in the brain for processing olfactory information and play a key role in organizing scent perception • Within each glomerulus, the terminals of receptors cells carrying information about a specific scent component synapse with the next cells in the olfactory pathway, the mitral cells which refine the smell signals and relay them to the brain – limbic system and the thalamic-cortical route • Although the olfactory system is sensitive and highly discriminative, it is also quickly adaptive 40