* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Autonomní nervový systém
Effect size wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Toxicodynamics wikipedia , lookup
NMDA receptor wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
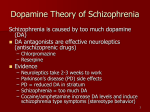
Autonomic nervous system Main functions: • contraction and relaxation of smooth muscles • function of all exocrine and some endocrine glands • heart beat • some metabolic pathways parasympaticus sympaticus Biosynthesis of catecholamines Dopamine Receptor-effector system 1 receptor stimulation • vasoconstriction skin, mucous and splanchnic vessels, very low in coronary and brain areas, increasing of periphery vessels resistance, blood pressure, bradycardia • mydriasis (contraction of m. dilatator pupilae), decreasing of intraocular pressure (reabsorption increasing and decreasing of its production (vasoconstriction of ciliary body vessels) • contraction of pregnant uterus • ejaculation • contraction of urinary bladder sphincter 2 receptor stimulation • (presynaptic) decreasing NA release (especially CNS) • trombocytes aggregation • vasoconstriction after local administration, but after systemic administration decreasing of symphaetic transmission (BP) • hypotensive effect 1 receptor stimulation heart: • heart rate (+ chronotropic) SA nodus • automaticity (+ bathmotropic) AV nodus, ventriculs • contractions (inotropic) • conduction speed (dromotropic) • oxygen consumption kidneys: • renin secretion (breaks down angiotensinogene to angiotensine I) 2 receptor stimulation • vasodilatation, skeletal muscles (”attack of defence"), BP diastolic • bronchodilatation • uterus relaxation (abortion prevention) • relaxation of bowel (+ 2), deceleration of motility • relaxation of urinary bladder • glycogenolysis - hyperglycemia, increased insulin secretion • tremor of skeletal muscles 3 receptor stimulation • lipolysis Receptor activation receptor 1 2 2 3 D1 D2 tissue smooth muscles of blood vessels m. dilatator pupilae uterus penis, vesiculae seminales GIT - sfincters presynaptic trombocytes heart juxtaglomerular cells pancreatic B cells bronchial, vessels, bowel, uterus smooth muscles liver skeletal muscles lipocytes smooth muscles axons effect contraction ( resistance of blood vessels) contraction (mydriasis) contraction ejaculation contraction inhibition of mediator release stimulation of aggregation positively chrono-, dromo- and inotropic renin release insulin release relaxation glykogenolysis stimulation tremor ( uptake K+) lipolysis relaxation of splanchnic vessels modification of transmitter release Receptor selectivity of adrenergic receptors There is no absolute selectivity for adrenergic receptors Sympathomimetics Sympathomimetics direct -agonists indirect -agonists (1+2) non-selective 1+2) ( selective 1 1 2 2 transmitter release reuptake inhibitors MAO inhibitors Epinephrine (adrenaline) • stimulution of , 1 a 2 • affinity mainly to receptors, in lower concentration stimulates only -receptors • Effects heart, vessels blood pressure bronchodilatation glykogenolysis - hyperglycemia, increased insulin secretion lipolysis • break down by MAO a COMT, the end products are 3-metoxy,4hydroxyphenylglycol and vanillylmandelic acid Epinephrine - side effects CNS restlessness, anxiety, headache intracranial hemorrhagia (phenylpropanolamine) cardiac arrhythmia hyperthyreosis - increases amount of adrenergic receptors blockers of catecholamines uptake (kokain, tricycl. antidepressants) and MAO inhibitors increase effect Epinephrine - indications • cardiopulmonal resuscitation. 1-2 mg in 5 ml f.sol. i.v. or intratracheally, intracardial administration is no more used (harm risk) • anaphylactic shock • bronchodilatory • mucosal decongestion • inotropic effect • vasoconstrictive effect • inhibition of mast cells degranulation • glaucoma • local anaesthetic drugs, vasoconstriction elongates anaesthesia • mucosal decongestion • antiastmathic drug: today almost 2-selective drugs Norepinephrine a 1 stimulation • increases systolic and diastolic blood pressure, n. vagus stimulation can cause bradycardia • Indications periphery analeptic drug, therapy of hypotensive states (spinal anaesthesia, sympatectomia, hypotensive drug overdosage) shock therapy is provided by dopamine Dopamine stimulation, stimulation after high doses admin., Dopamine receptors in kidneys and bowel. Effect is dose related. dose 1-2 ug/kg/min: stim. D receptors - increasing of renal perfusion dose 2-8 ug/kg/min: stim. beta receptors - pos. inotropic and chronotropic effect dose over 8 ug/kg/min: stim. alfa1 receptors vasoconstriction • Indication Shock therapy: – 1 simulation = inotropic and chronotropic effect – Stim D rec.= increased blood flow in kidneys and splanchnic area Heart failure Dobutamine • synthetic, 1 stimulation - great inotropic, and low chronotropic effect, oxygen consumption is not so affected, I: heart failure, T1/2 =2.5 min, continuous administration Isoprenaline • inj., synt., 1 a 2 stimulation - increases heart output, but 2 vasodilatation in skeletal muscles decreases diastolic blood pressure. • Indication – A-V blocs and heart arrest, when cardiostimulation is not available – bradycardia (atropine resistant) – (former antishock therapy and bronchodilatatory agent) Influence of different agonists on BP adrenaline isoprenaline noradrenaline Phenylefrine • 1 stimulation – mydriatic & dekongestant eff. • EVERCIL and NEOSYNEPHRINE gtt; VIBROCIL gtt Midodrine • 1 stimulation – postural hypotension (GUTRON) Naphasoline, xylometazoline, oxymetazoline etc. 1 mucous decongestion during 1st phase is a reactive hyperaemia after chronic use - sanorinismus - (use up to one week) 2 agonists Clonidine, - methyldopa • I: hypertension (stimulation of 2 central receptors causes decreasing of periphery adrenergic activity) • hypotensive agents, treatment of morphine withdrawal symptoms agonists • non-selective - dopamine • 1 agonists - dobutamine • 2 agonists - fenoterol, salbutamol, terbutaline, formoterol – bronchodilatatory and tocolytic effect with minimum cardiovascular effects – (inhibition of leukotriens, histamine release and phospholipasis A2 ) Sympathomimetics Sympathomimetics direct -agonists indirect -agonists (1+2) non-selective 1+2) ( selective 1 1 2 2 transmitter release reuptake inhibitors MAO inhibitors Indirect sympatomimetics • Inhibitors MAO (antidepressant) • Amphetamine, metamphetamine, phenmetrazine, methylphenidate • increase of transmitter release from presynaptic vesicles • cross HEB, CNS stim. effect – increased psychomot. activity (doping) – anorectic effect , (hypothalamus stimulation) • abuse risk • I: attention deficit hyperactivity disorder (ADHD) Ephedrine – nasal decongestion (reactive hyperaemia with increased secretion) – bronchodilatans – metamphetamine synthesis (”pervitin") Tyramine • metabolite of tyrosine, eliminated by MAO. But when MAO are administrated, then food with high tyramine concentration (cheese, yoghurt, bananas, sausages) can cause hypertensive reaction Cocain • inhibition of neuromediators re-uptake (esp. dopamine) Side effects Catecholamines - they do not cross HEB, but periphery stimulation of or 1 receptors can cause: vasoconstriction cardiac arrhythmia heart attack haemorrhagia or pulmonal oedema Sympatholytics indirect direct non-selective selective Indirect sympatolytics Reserpine • alcaloid Rauwolfia serpentina. • Inhibits transmitter storage in presynaptic vesicles CNS effects • antipsychotic effect (D receptor) • dysphoric effect - reserpine causes depressions that can induce suicide • cognitive functions inhibition Reserpine Central and peripheral ADRs gastric HCl hypersecretion, diarrhoea, nasal congestion, hypotension Indication • non responding hypertensive states (combination with diuretics and ergot alkaloids). Guanethidine • peripheral acting sympatolytics (causes hypotensive states, especially in the morning) • Blocks exocytosis – release of NE • Local miotic agent Sympatholytics indirect direct non-selective selective Direct sympatolytics Reversible -lytics most of sympatolytics, reversible binds to receptors and acts as agonists or dualists (with intristic sympatomimetic activity - ISA) Irreversible a-lytics binds to receptor by covalent binding phenoxybenzamine (14-48 h). Prazosin, doxazosin Reversible 1B-receptor (espec.) blocker. It does not influence 2-receptors - very low tachycardia. Relaxation of smooth muscle cells either vascular (I: hypertension – prazosin, doxazosin) or in prostate (I: BHP – doxazosin) Indications of -lytics (synthetic) Feochromocytome: adrenal medula tumor that produces catecholamines phentolamine and phenoxybenzamin Mild hypertension: In most cases 1-lytics. Cave postural hypotension after first dose administration – prazosin Peripheral vasospastic diseases: (Raynaud´s disease) phenoxybenzamine, phentolamine, tolazoline. (calcium channel blockers) Urinary obstruction: tamsulosine, alfuzosine (espec. via 1A-receptors) Impotency: phentolamine, yohimbine Natural reversible -lytics (alkaloids and their derivates) • Produced by ergot (Secale cornutum), product of Claviceps purpurea, corn fungus. • -lytics properties, but they are also NA dualists, dopamine agonists ( prolactine production) and serotonin antagonists. • Secale cornutum (ergot) was ground with meal and its toxic effect was very well known. Gangrenes of acral parts of limbs (ergotismus gangrenosus) and cramp (ergotismus convulsivus). Saint Anthony the Great (251 - 356) Ergonovine, ergometrine - -parcial agonists. Uterotonic effects (pregnant uterus – more 1 receptors), especially their methyl- derivatives (methylergometrine). Per os administration (gtt, tbl) is possible Ergotoxine, mixture of alkaloids - ergocristine, ergocriptine and ergocornine - -lytic effect. Bromocriptine - dopaminergic effect; -lytic effect increase its dihydroderivatives (DH). Indications hypertension - DH-ergocristine: CRYSTEPIN drg. (clopamide + reserpine + DH-ergocristine) NEOCRYSTEPIN drg. (chlorthalidone + reserpine ergocristine) vasodilatans - DHergotoxini mesilas migraine uterotonic effect - (surgery - prevention of bleeding) + DH- -sympatolytics • competitive antagonists (no intrinsic activity), partial agonists (ISA, intrinsic sympathomimetic activity) • Selectivity: non-selective beta-lytics - block 1 and 2 receptors; cardioselective block 1 receptors. • Lipid solubility - HE barrier penetration Beta-lytics and their characteristic Drug selectivity ISA atenolol metoprolol esmolol labetalol propranolol metipranol pindolol bopindolol timolol nadolol 1 1 1 a 0 0 0 + 0 0 + + 0 0 t1/2 hour 6-9 3-4 l0 min 5 3.5-6 3-6 3-4 3-4 4-5 14-24 bioaviability (%) lipid solubility 40 50 30 30 40 90-100 90-100 30 33 low medium low medium high medium medium medium medium low CLASSIFICATION OF BETA-BLOCKERS (BB) Non-selective: on 1 and 2 metipranol, sotalol, propranolol, timolol, Cardioselective: mostly on 1 bisoprolol, metoprolol, atenolol, betaxolol Non-selective with ISA: partial -agonistic activity pindolol, bopindolol, oxprenolol,levobunolol Cardioselective with ISA: acebutol (ACECOR), celiprolol BB with vasodilatory eff.: blockage 1 + 2+ 1 carvedilol, labetalol blockage 1 + 1+ 2 + ISA celiprolol - TENOLOC blockage 1 + 2 + ISA bopindolol - SANDONORM HYDROPHILICITY x LIPOPHILICITY a) lipophilic molecules - cross to CNS (insomnia, depression) - metabolized in liver ( bioavailability) - variable level (CYP polymorphism) - metoprolol,... b) hydrophilic molecules - less ADRs (those of CNS origin) - eliminated via kidneys (longer eff., bioavailability) - atenolol, bisoprolol... NO DIFFERENCE IN CLINICAL EFF. WAS DEMONSTRATED Effects cardiovascular: decrease of BP and CO negative chronotropic, inotropic, dromotropic effect. Decrease of rennin production, but due to inhibition of beta-vasodilatation peripheral vascular resistance can increase - increase of PVR (peripheral -receptors are not opposed) bronchopulmonal: block bronchoconstriction, asthma. of especially 2-receptors patients with causes bronchial Effects II eye: intraocular pressure decrease local and systemic administration due to reduction of intraocular liquid production metabotropic effects: glycogenolysis reduction hypoglycaemia Lipolysis inhibition - HDL decrease and VLDL increase CNS effects: sleep disturbances, depression, nightmare => severe Indications Hypertension - monotherapy or combination with other antihypertensive drugs Ischemic heart disease - -lytics decrease chest pain frequency, myocardial output, oxygen consumption, systolic pressure and better myocardial blood distribution (especially to ischemic parts). -lytics decreases risk of death (20-30 %) after heart attack at least 3 years after it. Indications II. Arrhythmia - supraventricular and ventricular tachycardia Glaucoma - reduction of intraocular liquid production by corpus cilliare. (timoptol) Hyperthyreosis prevents catecholamines effect Mild anxiolytic effect heart beat, sweating, anxiety Portal hypertension Side effects I. Bronchial asthma Heart failure: cave! severe heart insufficiency. Bradycardia, A-V blocks Hypoglycaemia - diabetes mellitus. (when hypoglycaemia is present, adrenaline due to its 2-effect increase glucose blood level. -blockers inhibit this contra-regulation. Local ischemia - beta receptor inhibition decrease vasodilatation, alpha receptor stimulation increase vasoconstriction Side effects II. rush, fever CNS: sedation, sleep disturbances, depression rebound phenomena after breaking the therapy - worsening of illness => phased lowering therapy is needed