* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Evolution of metal ions in biological systems wikipedia , lookup
Metabolic network modelling wikipedia , lookup
Oligonucleotide synthesis wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Ribosomally synthesized and post-translationally modified peptides wikipedia , lookup
Nitrogen cycle wikipedia , lookup
Catalytic triad wikipedia , lookup
Point mutation wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Metalloprotein wikipedia , lookup
Protein structure prediction wikipedia , lookup
Peptide synthesis wikipedia , lookup
Proteolysis wikipedia , lookup
Genetic code wikipedia , lookup
Citric acid cycle wikipedia , lookup
Biochemistry wikipedia , lookup
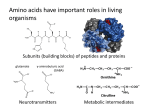
Metabolism of Nitrogenous Compound Mpenda F.N 1 Introduction • This topic describes the amino acids that are important in human nutrition. • It covers the digestion and absorbtion of proteins in the gut. • The amino acid degradation pathways in the tissues, and the urea cycle. • The amino acid synthesis pathways • There are separate topic dealing with nucleotide and 'one carbon' metabolism and with porphyrin on the integration of metabolism. 2 Introduction… • Human proteins have very different lifetimes. • Total body protein is about 11kg, but about 25% of this is collagen, which is metabolically inert. • A typical muscle protein might survive for three weeks, but many liver enzymes turn over in a couple of days. • Some regulatory enzymes have half-lives measured in hours or minutes. • The majority of the amino acids released during protein degradation are promptly re-incorporated 3 into fresh proteins. Introduction… • Net protein synthesis accounts for less than one third of the dietary amino acid intake, even in rapidly growing children consuming a minimal diet. • Most of the ingested protein is ultimately oxidised to provide energy, and the surplus nitrogen is excreted, a little as ammonia but mostly as urea. 4 Protein degradation • Soluble intracellular proteins are tagged for destruction by attaching ubiquitin, a low molecular weight protein marker. • They are then degraded in proteasomes to short peptides. • A very few of these are displayed on the cell surface by the MHC [major histocompatibility] complex as part of the immune system, • But most of them are further metabolised to free amino acids. • Some proteins are degraded by an alternative system within the lysosomes. 5 Protein degradation • Dietary proteins are initially denatured by the stomach acid, in conjunction with limited proteolysis by pepsin. • In young mammals gastric rennin partially hydrolyses and precipitates milk casein and increases gastric residence time. • Gastric acid also kills most ingested bacteria, rendering the upper part of the gut almost sterile. 6 Protein degradation • Protein digestion is largely completed in the small intestine at a slightly alkaline pH. • The pancreatic proteases trypsin, chymotrypsin and elastase divide the proteins into short peptides. • These are attacked from both ends by aminopeptidase and carboxypeptidase, and the fragments are finished off by dipeptidases secreted from the gut wall. 7 Amino acid catabolism • In animals, amino acids undergo oxidative degradation in three different metabolic circumstances: During the normal synthesis and degradation of cellular proteins. When a diet is rich in protein and the ingested amino acids exceed the body’s needs for protein synthesis. During starvation or in uncontrolled diabetes mellitus, when carbohydrates are either unavailable or not properly utilized, cellular proteins are used as fuel. 8 Amino acid catabolism • The liver is the principal site of amino acid metabolism. • Other tissues, such as the kidney, the small intestine, muscles, and adipose tissue, take part. • The first step in the breakdown of amino acids is the separation of the amino group from the carbon skeleton, usually by a transamination reaction. • The carbon skeletons resulting from the deaminated amino acids are used to form either glucose or fats, or they are converted to a metabolic intermediate that can be oxidized by the citric acid cycle. 9 Amino acid catabolism • Under all these metabolic conditions, amino acids lose their amino groups to form α-keto acids, the “carbon skeletons” of amino acids. • The α-keto acids undergo oxidation to CO2 and H2O • More importantly provide three- and four-carbon units that can be converted by gluconeogenesis into glucose, the fuel for brain, skeletal muscle, and other tissues 10 Amino acid catabolism • Therefore, the processes of amino acid degradation converge on the central catabolic pathways. • The carbon skeletons of most amino acids finding their way to the citric acid cycle. • In some cases the reaction pathways of amino acid breakdown closely parallel steps in the catabolism of fatty acids. 11 Amino acid catabolism • The pathways for amino acid degradation include a key step in which the α-amino group is separated from the carbon skeleton and shunted into the pathways of amino group metabolism • We will deal first with amino group metabolism and nitrogen excretion. • We will then deal with the fate of the carbon skeletons derived from the amino acids; along the way we see how the pathways are interconnected. 12 13 Metabolic Fates of Amino Groups • Excess ammonia generated in other (extrahepatic) tissues travels to the liver for conversion to the excretory form. • Glutamate and glutamine play especially critical roles in nitrogen metabolism, acting as a kind of general collection point for amino groups. • In the cytosol of hepatocytes, amino groups from most amino acids are transferred to α-ketoglutarate to form glutamate, which enters mitochondria and gives up its amino group to form NH4. 14 Metabolic Fates of Amino Groups • Excess ammonia generated in most other tissues is converted to the amide nitrogen of glutamine, which passes to the liver, then into liver mitochondria. • Glutamine or glutamate or both are present in higher concentrations than other amino acids in most tissues. • In skeletal muscle, excess amino groups are generally transferred to pyruvate to form alanine, another important molecule in the transport of amino groups to the liver. 15 Central role of glutamate • Glutamate also occupies a special position in amino acid breakdown • Most of the nitrogen from dietary protein is ultimately excreted from the body via the glutamate pool. • Glutamate is special because it is chemically related to 2oxoglutarate (= α-keto glutatarate) which is a key intermediate in the citric acid (Krebs) cycle. • Glutamate can be reversibly converted into 2-oxoglutarate by transaminases or by glutamate dehydrogenase. • In addition, glutamate can be reversibly converted into glutamine, an important nitrogen carrier, and the most common free amino acid in human blood plasma. 16 Central role of glutamate 17 Central role of glutamate 18 Central role of glutamate • Because of the participation of 2-oxoglutarate in numerous transaminations, glutamate is a prominent intermediate in nitrogen elimination as well as in anabolic pathways. • Glutamate, formed in the course of nitrogen elimination, is either oxidatively deaminated by liver glutamate dehydrogenase forming ammonia, or converted to glutamine by glutamine synthetase and transported to kidney tubule cells. • There the glutamine is sequentially deamidated by glutaminase and deaminated by kidney glutamate dehydrogenase. 19 Central role of glutamate 20 Central role of glutamate • The ammonia produced in the latter two reactions is excreted as NH4+ in the urine, where it helps maintain urine pH in the normal range of pH 4 to pH 8. • The extensive production of ammonia by peripheral tissue or hepatic glutamate dehydrogenase is not feasible because of the highly toxic effects of circulating ammonia. • Normal serum ammonium concentrations are in the range of 20–40μM, and an increase in circulating ammonia to about 400μM causes alkalosis and neurotoxicity. 21 Biosynthesis of urea Urea biosynthesis occurs in four stages: Transamination oxidative deamination of glutamate ammonia transport reactions of the urea cycle 22 Transamination reactions • The first step in the catabolism of most L-amino acids, once they have reached the liver, is removal of the α-amino groups, promoted by enzymes called aminotransferases or transaminases. • In these transamination reactions, the -amino group is transferred to the -carbon atom of alphaketoglutarate, leaving behind the corresponding keto acid analog of the amino acid • The effect of transamination reactions is to collect the amino groups from many different amino acids in the form of L-glutamate 23 Transamination reactions • Transamination is an exchange of functional groups between any amino acid (except lysine, proline, and threonine) and an α-keto acid. • The amino group is usually transferred to the keto carbon atom of pyruvate, oxaloacetate, or αketoglutarate, converting the α-keto acid to alanine, aspartate, or glutamate, respectively. • Transamination reactions are catalyzed by specific transaminases (also called aminotransferases), which require pyridoxal phosphate as a coenzyme. 24 Transamination reactions 25 Transamination reactions •Inmanyaminotransferase reactions, α -ketoglutarate is the amino group acceptor. • All aminotransferases have pyridoxal phosphate (PLP) as cofactor. •The reaction is readily reversible. 26 The role of Pyridoxal Phosphate in the Transfer of -Amino Groups to alpha-Ketoglutarate • All aminotransferases have the same prosthetic group and the same reaction mechanism. • The prosthetic group is pyridoxal phosphate (PLP), the coenzyme form of pyridoxine, or vitamin B6. • Also we saw pyridoxal phosphate in as a coenzyme in the glycogen phosphorylase reaction. • Its primary role in cells is in the metabolism of molecules with amino groups. 27 The role of Pyridoxal Phosphate in the Transfer of α-Amino Groups to α-Ketoglutarate • Pyridoxal phosphate functions as an intermediate carrier of amino groups at the active site of aminotransferases. • It undergoes reversible transformations between its aldehyde form, pyridoxal phosphate, which can accept an amino group, and its aminated form, pyridoxamine phosphate, which can donate its amino group to an α-keto acid. 28 L-GLUTAMATE DEHYDROGENASE OCCUPIES A CENTRAL POSITION IN NITROGEN METABOLISM • Transfer of amino nitrogen to α-ketoglutarate forms L-glutamate. • Release of this nitrogen as ammonia is then catalyzed by hepatic L-glutamate dehydrogenase • (GDH), which can use either NAD+ or NADP+ • Conversion of α-amino nitrogen to ammonia by the concerted action of glutamate aminotransferase and GDH is often termed “transdeamination” 29 L-GLUTAMATE DEHYDROGENASE OCCUPIES A CENTRAL POSITION IN NITROGEN METABOLISM • The L-glutamate dehydrogenase reaction. • NAD(P)+ means that either NAD+ or NADP+ can serve as co-substrate. • The reaction is reversible but favors • glutamate formation. 30 L-GLUTAMATE DEHYDROGENASE OCCUPIES A CENTRAL POSITION IN NITROGEN METABOLISM • Glutamate dehydrogenase operates at an important intersection of carbon and nitrogen metabolism. • An allosteric enzyme with six identical subunits, its activity is influenced by a complicated array of allosteric modulators. • The best-studied of these are the positive modulator ADP and the negative modulator GTP • Mutations that alter the allosteric binding site for GTP or otherwise cause permanent activation of glutamate dehydrogenase lead to a human genetic 31 disorder called hyperinsulinism-hyperammonemia L-GLUTAMATE DEHYDROGENASE OCCUPIES A CENTRAL POSITION IN NITROGEN METABOLISM • Serum aminotransferases such as aspartate aminotransferase, AST (also called serum glutamate-oxaloacetate transaminase, SGOT) and alanine transaminase, ALT (also called serum glutamate-pyruvate transaminase (SGPT) have been used as clinical markers of tissue damage, • with increasing serum levels indicating an increased extent of damage. • As indicated earlier, ALT has an important function in the delivery of skeletal muscle carbon and nitrogen (in the form of alanine) to the32 liver in a Glutamine Transports Ammonia in the Bloodstream • Ammonia is quite toxic to animal ,and the levels present in blood are regulated. • In many tissues, including the brain, some processes such as nucleotide degradation generate free ammonia. • In most animals much of the free ammonia is converted to a nontoxic compound before export from the extrahepatic tissues into the blood and transport to the liver or kidneys. • For this transport function, glutamate,33critical to Glutamine Transports Ammonia in the Bloodstream 34 Glutamine Transports Ammonia in the Bloodstream • The glutamine is sequentially deamidated by glutaminase and deaminated by kidney glutamate dehydrogenase. • The ammonia produced in the kidney reactions is excreted as NH4+ in the urine. • This helps maintain urine pH in the normal range of pH 4 to pH 8. • The extensive production of ammonia by peripheral tissue or hepatic glutamate dehydrogenase is not feasible because of the highly toxic effects of 35 circulating ammonia. 35 Glucose-alanine cycle • Alanine also plays a special role in transporting amino groups to the liver in a nontoxic form, via a pathway called the glucose-alanine cycle • In muscle and certain other tissues that degrade amino acids for fuel, amino groups are collected in the form of glutamate by transamination. • Glutamate can transfer its -amino group to pyruvate, a readily available product of muscle glycolysis, by the action of alanine aminotransferase. 36 Glucose-alanine cycle • The alanine so formed passes into the blood and travels to the liver. • In the cytosol of hepatocytes alanine aminotransferase transfers the amino group • from alanine to alpha-ketoglutarate, forming pyruvate and glutamate 37 Glucose-alanine cycle 38 Urea cycle • About 80% of the excreted nitrogen is in the form of urea is produced exclusively in the liver, in a series of reactions that are distributed between the mitochondrial matrix and the cytosol. • The series of reactions that form urea is known as the Urea Cycle or the Krebs-Henseleit Cycle. • In the urea cycle, amino groups of urea are donated by carbamoyl phosphate and aspartate, while the carbon atom of urea is contributed by bicarbonate. 39 Urea cycle • The essential features of the urea cycle reactions and their metabolic regulation are as follows: Arginine from the diet or from protein breakdown is cleaved by the cytosolic enzyme arginase, generating urea and ornithine. In subsequent reactions of the urea cycle a new urea residue is built on the ornithine, regenerating arginine and perpetuating the cycle. 40 Arginine 41 42 Urea cycle • The net reaction for urea synthesis shows consumption of 4 "high energy" phosphoanhydride bonds, contributed by ATP. • Two of these are used by for synthesis of carbamoyl phosphate from bicarbonate and ammonia. • The ammonia is itself ultimately derived from various amino acids by the combined action of transaminase enzymes and glutamate dehydrogenase. • Carbamoyl phosphate synthesis occurs in the mitochondrial matrix, and is catalyzed43by carbamoyl Urea cycle • The carbamoyl phosphate produced is then consumed in the synthesis of citrulline from ornithine. • This reaction is catalyzed by ornithine carbamoyltransferase. • The citrulline is shuttled out of the mitochondrion and into the cytosol, where the rest of the urea cycle takes place. • Another amino acid-derived amino group is incorporated into the intermediate Aspartate is joined via its α-amino group to citrulline in the 44 Urea cycle • The next reaction is the elimination of fumarate from argininosuccinate, yielding arginine. • This step is catalyzed by argininosuccinase. • Finally, urea is produced by arginase, acting on arginine and water as substrates. • Urea is secreted into the bloodstream, from which it is ultimately eliminated by the kidneys for excretion. • The ornithine produced in this last step is shuttled into the mitochondrial matrix, completing the cycle 45 Regulation of the Urea Cycle • The urea cycle operates only to eliminate excess nitrogen. • On high-protein diets the carbon skeletons of the amino acids are oxidized for energy or stored as fat and glycogen, but the amino nitrogen must be excreted. • Enzymes of the urea cycle are controlled at the gene level. • long-term changes in the quantity of dietary protein, changes of 20-fold or greater in the concentration of cycle enzymes are observed. 46 Regulation of the Urea Cycle • • • • • When dietary proteins increase significantly, enzyme concentrations rise. On return to a balanced diet, enzyme levels decline. Under conditions of starvation, enzyme levels rise as proteins are degraded and amino acid carbon skeletons are used to provide energy, thus increasing the quantity of nitrogen that must be excreted. Short-term regulation of the cycle occurs principally at CPS-I, which is inactive in the absence of its obligate activator Nacetylglutamate. The steady-state concentration of N-acetylglutamate is set by the concentration of its components acetyl-CoA and glutamate and by arginine, which is a positive allosteric effector of N-acetylglutamate synthase 47 . Read on molecular basis of ammonia intoxication 48 Krebs bicycle • Because the fumarate produced in the argininosuccinase reaction is also an intermediate of the citric acid cycle. • each cycle can operate independently and communication between them depends on the transport of key intermediates between the mitochondrion and cytosol. • The fumarate generated in cytosolic arginine synthesis can therefore be converted to malate in the cytosol, and these intermediates can be further metabolized in the cytosol or transported into 49 Urea Cycle Disorders (UCDs) • A complete lack of any one of the enzymes of the urea cycle will result in death shortly after birth. • However, deficiencies in each of the enzymes of the urea cycle, including N-acetylglutamate synthase, have been identified. • These disorders are referred to as urea cycle disorders or UCDs. • Take your time read on UCDs 50 Krebs bicycle • Aspartate formed in mitochondria by transamination between oxaloacetate and glutamate can be transported to the cytosol, where it serves as nitrogen donor in the urea cycle reaction catalyzed by argininosuccinate synthetase. 51 52 Catabolism of the Carbon Skeletons of Amino Acids • The 20 catabolic pathways converge to form only six major products, all of which enter the citric acid cycle. • From here the carbon skeletons are diverted to gluconeogenesis or ketogenesis or are completely oxidized to CO2 and H2O. • All or part of the carbon skeletons of seven amino acids are ultimately broken down to acetyl-CoA. 53 Catabolism of the Carbon Skeletons of Amino Acids • Five amino acids are converted to alphaketoglutarate, four to succinyl-CoA, two to fumarate, and two to oxaloacetate. • Parts or all of six amino acids are converted to pyruvate, which can be converted to either acetylCoA or oxaloacetate. • Note that some amino acids appear more than once, reflecting different fates for different parts of their carbon skeletons. 54 55 56 Some Amino Acids Are Converted to Glucose, Others to Ketone Bodies • The seven amino acids that are degraded entirely or in part to acetoacetyl-CoA and/or acetyl-CoA— phenylalanine, tyrosine, isoleucine, leucine, tryptophan, threonine, lysine • Can yield ketone bodies in the liver 57 Some Amino Acids Are Converted to Glucose, Others to Ketone Bodies • Where acetoacetyl-CoA is converted to acetoacetate and then to acetone and hydroxybutyrate . • These are the ketogenic amino acids • Their ability to form ketone bodies is particularly evident in uncontrolled diabetes mellitus, in which the liver produces large amounts of ketone bodies from both fatty acids and the ketogenic amino acids. 58 Some Amino Acids Are Converted to Glucose, Others to Ketone Bodies • The amino acids that are degraded to pyruvate, ketoglutarate, succinyl-CoA, fumarate, and/or oxaloacetate can be converted to glucose and glycogen. • They are the glucogenic amino acids. • However, division between ketogenic and glucogenic amino acids is not clear. • For examplel, five amino acids—tryptophan, phenylalanine, tyrosine, threonine, and isoleucine— are both ketogenic and glucogenic 59 • Leucine is an exclusively ketogenic amino acid that Enzyme Cofactors Playing Important Roles in Amino Acid Catabolism • We have already considered one important class: transamination reactions requiring pyridoxal phosphate. • Another common type of reaction in amino acid catabolism is one-carbon transfers, which usually involve one of three cofactors: biotin, tetrahydrofolate, or S-adenosylmethionine Read on how these cofactors are synthesized 60 Amino Acids Degraded to Pyruvate • The carbon skeletons of six amino acids are converted in whole or in part to pyruvate. • The pyruvate can then be converted to either acetyl-CoA (a ketone body precurs) or oxaloacetate (a precursor for gluconeogenesis). • Thus amino acids catabolized to pyruvate are both ketogenic and glucogenic • Tryptophan, cysteine, serine, glycine, and threonine 61 62 Amino Acids Degraded to Acetyl-CoA • Portions of the carbon skeletons of seven amino acids—Tryptophan, lysine, phenylalanine, tyrosine, leucine,isoleucine, and threonine—yield acetylCoA and/or acetoacetyl-CoA, the latter being converted to acetyl-coA. • Tryptophan breakdown is the most complex of all the pathways of amino acid catabolism in animal tissue 63 Amino Acids Degraded to Acetyl-CoA • Portions of tryptophan (four of its carbons) yield acetyl-CoA via acetoacetyl-CoA. • Some of the intermediates in tryptophan catabolism are precursors for the synthesis of other biomolecules , including nicotinate, precursor of NAD and NADP in animals; serotonin. 64 65 Amino Acids Degraded to Acetyl-CoA • The breakdown of phenylalanine is noteworthy . • Genetic defects in the enzymes of this pathway lead to several inheritable human diseases. • Phenylalanine and its oxidation product tyrosine are degraded into two fragments, both of which can enter the citric acid cycle: Four of the nine carbon atoms yield free acetoacetate, which is converted to acetoacetylCoA. Second four-carbon fragment is recovered as fumarate. 66 67 Amino Acids Degraded to Acetyl-CoA • Phenylalanine, after its hydroxylation to tyrosine, is also the precursor of dopamine, a neurotransmitter, and of norepinephrine and epinephrine, hormones secreted by the adrenal medulla’. • Melanin, the black pigment of skin and hair, is also derived from tyrosine. 68 • • • • Phenylalanine catabolism is genetically defective in some people (Phenylketonuria: PKU) Phenylketonuria (PKU) is an autosomal recessive disorder resulting from defects in the metabolism of phenylalanine. PKU is a hyperphenylalaninemia with multifactorial causes. There are several hyperphenylalaninemias that are not PKU and are called non-PKU hyperphenylalaninemias (HPAs). Hyperphenylalaninemia is defined as a plasma phenylalanine concentration >120μM. 69 • • • • Phenylalanine catabolism is genetically defective in some people (Phenylketonuria: PKU) PKU is caused by mutation in the phenylalanine hydroxylase gene (gene symbol = PAH). The HPAs are disorders of phenylalanine hydroxylation. The reaction catalyzed by PAH involves tetrahydrobiopterin (BH4) as a co-factor, the HPAs can result from defects in any of the several genes required for synthesis and recycling of BH4. Removal of excess phenylalanine normally proceeds via the tyrosine biosynthesis reaction and then via 70 • • • • Phenylalanine catabolism is genetically defective in some people (Phenylketonuria: PKU) However, defects of other factors in phenylalanine hydroxylation system may have similar effect as phenylalanine hydroxylase defect. Also, hyperphenylalaninemia results in abnormalities in the metabolism of many compounds derived from the aromatic amino acids. If left untreated, these metabolic abnormalities cause postnatal brain damage and severe mental retardation. PKU is the most common inborn error in amino acid 71 Phenylalanine catabolism is genetically defective in some people (Phenylketonuria: PKU) • The mental retardation is caused by the accumulation of phenylalanine, which becomes a major donor of amino groups in aminotransferase activity and depletes neural tissue of 2-oxoglutarate (α-ketoglutarate). • This absence of 2-oxoglutarate in the brain shuts down the TCA cycle and the associated production of aerobic energy, which is essential to normal brain development. • The product of phenylalanine transamination, 72 phenylpyruvic acid, is reduced to phenylacetate and 73 74 Amino Acids Converted to αKetoglutarate • The carbon skeletons of proline, glutamate, glutamine, arginine, and histidine enter the citric acid cycle as α-ketoglutarate. • Proline, glutamate, and glutamine have fivecarbon skeletons. • The cyclic structure of proline is opened by oxidation to produce glutamate. 75 76 • Amino Acids Converted to SuccinylCoA The carbon skeletons of methionine, isoleucine, threonine, and valine are degraded by pathways that yield succinyl-CoA, an intermediate of the citric acid cycle. • Methionine donates its methyl group to one of several possible acceptors through Sadenosylmethionine, and three of its four remaining carbon atoms are converted to the propionate of propionyl-CoA, a precursor of succinyl-CoA. • Isoleucine undergoes transamination, followed by oxidative decarboxylation of the resulting α-keto 77 acid. Amino Acids Converted to SuccinylCoA • Valine undergoes transamination and decarboxylation, then a series of oxidation reactions that convert the remaining four carbons to propionyl-CoA. • Some parts of the valine and isoleucine degradative pathways closely parallel steps infatty acid degradation. • In human tissues, threonine is also converted in two steps to propionyl-CoA. This is the primary pathway for threonine degradation in humans. 78 79 Branched-Chain Amino Acids Are Not Degraded in the Liver • Although much of the catabolism of amino acids takes place in the liver, the three amino acids with branched side chains (leucine, isoleucine, and valine) are oxidized as fuels primarily in muscle, adipose, kidney, and brain tissue. • These extrahepatic tissues contain an aminotransferase, absent in liver, that acts on all three branched-chain amino acids to produce the corresponding-keto acids. 80 Non-essential amino acid biosynthesis Non-essential amino acid • Alanine, Asparagine, Aspartate, Cysteine, Glutamate, Glutamine, Glycine, Proline, Serine, Tyrosine. Essential amino acid • Arginine, Histidine, Isoleucine, Leucine, Lysine, Methionine, Phenylalanine, Threonine, Tyrptophan, Valine. 81 Non-essential amino acid biosynthesis • The amino acids arginine, methionine and phenylalanine are considered essential for reasons not directly related to lack of synthesis. • Arginine is synthesized by mammalian cells but at a rate that is insufficient to meet the growth needs of the body and the majority that is synthesized is cleaved to form urea. • Methionine is required in large amounts to produce cysteine if the latter amino acid is not adequately supplied in the diet. • Similarly, phenylalanine is needed in large amounts 82 Glutamate and Aspartate •Glutamate is synthesized from its' widely distributed α-keto acid precursor by a simple one-step transamination reaction catalyzed by glutamate dehydrogenase (GDH). •As it has been discussed, the glutamate dehydrogenase reaction plays a central role in overall nitrogen homeostasis 83 Glutamate and Aspartate Like glutamate, aspartate is synthesized by a simple one-step transamination reaction catalyzed by aspartate aminotransferase, AST (formerly referred to as serum glutamate-oxalate transaminase, SGOT). 84 Glutamate and Aspartate Also, aspartate can be derived from asparagine through the action of asparaginase. The importance of aspartate as a precursor of ornithine for the urea cycle is described in the urea cycle. 85 Alanine and the Glucose-Alanine Cycle • Alanine is second only to glutamine in prominence as a circulating amino acid. • It serves a unique role in the transfer of nitrogen from peripheral tissue to the liver. • Alanine is transferred to the circulation by many tissues, but mainly by muscle, in which alanine is formed from pyruvate at a rate proportional to intracellular pyruvate levels. • Liver accumulates plasma alanine, reverses the transamination that occurs in muscle, and proportionately increases urea production. 86 Alanine and the Glucose-Alanine Cycle There are two main pathways to production of muscle alanine: directly from protein degradation, and via the transamination of pyruvate by alanine transaminase, ALT (also referred to as serum glutamate-pyruvate transaminase, SGPT). 87 • • • • • Cysteine Biosynthesis: Role of Methionine The sulfur for cysteine synthesis comes from the essential amino acid methionine. A condensation of ATP and methionine, catalyzed by methionine adenosyltransferase (MAT), yields Sadenosylmethionine (SAM or AdoMet). In the production of SAM all phosphates of an ATP are lost: one as Pi and two as PPi. It is adenosine which is transferred to methionine. MAT is also called S-adenosylmethionine synthetase. 88 Cysteine Biosynthesis: Role of Methionine • The synthesis of cysteine represents an extremely important and clinically relevant biochemical pathway. • Several vitamins are required for this metabolic pathway to proceed emphasizing the nutritional impact. • Folate, pyridoxal phosphate (PLP, B6), and B12 are all necessary for cysteine synthesis. • The enzyme methionine synthase requires both folate and B12 for activity. • Deficiency in either of these vitamins89contributes 90 Homocysteinemia / Homocystinemia • Homocysteinemias (homocystinemias) represent a family of inherited disorders resulting from defects in several of the genes involved in the conversion of methionine to cysteine. • As the name implies, these disorders result in elevated levels of homocysteine and homocystine in the urine, where the elevated urine output of the metabolite is referred to as homocysteinurina. • Homocystine is a disulfide-bonded homodimer of two homocysteines. • This is similar to the formation of cystine from two 91 cysteines. 92 B Vitamins and Homocysteine • Several studies have shown consistent and strong relationships between low concentrations of blood folate, vitamin B12 and vitamin B6, and high concentrations of homocysteine which, in turn, have been linked with heart disease, stroke and other vascular outcomes. • The breakdown of homocysteine to cysteine requires the vitamin B6 dependent enzyme, cystathionine beta synthase • Re-methylation to methionine requires a vitamin B12 dependent enzyme, with folate as a cofactor. 93 • The most common cause of homocysteine B Vitamins and Homocysteine • Active folate, known as 5-MTHF or 5methyltetrahydrofolate, works in concert with vitamin B12 as a methyl-group donor in the conversion of homocysteine back to methionine. • Normally, about 50% of homocysteine is remethylated; the remaining homocysteine is transsulfurated to cysteine, which requires vitamin B6 as a co-factor. • This pathway yields cysteine, which is then used by the body to make glutathione, a powerful antioxidant that protects cellular components 94 B Vitamins and Homocysteine • Vitamin B2 (riboflavin) and magnesium are also involved in homocysteine metabolism. • Thus a person needs several different B-vitamins to help keep homocysteine levels low and allow for it to be properly transformed into helpful antioxidants like glutathione. • Without B6, B12, B2, folate, and magnesium, dangerous levels of homocysteine may build up in the body. 95 Homocysteine and Heart Disease • Lowering high homocysteine is thought to be important because of its strong and consistent relationship with heart disease. • High homocysteine has been linked with occurrence and mortality from heart disease - as well as with indicators of heart disease risk, including thickening of the carotid arteries and venous thrombosis. • In 1968, a Harvard researcher observed that children with a genetic defect that caused them to have sharply elevated homocysteine levels suffered severe atherosclerotic occlusion and vascular 96 disorders similar to what is seen in middle-aged How Elevated Homocysteine Leads to Vascular Damage • If unhealthy levels of homocysteine accumulate in the blood, the delicate lining of an artery (endothelium) can be damaged. • Homocysteine can both initiate and potentiate atherosclerosis. • For example, homocysteine-induced injury to the arterial wall is one of the factors that can initiate the process of atherosclerosis, leading to endothelial dysfunction and eventually to heart attacks and strokes 97 Tyrosine Biosynthesis • Tyrosine is produced in cells by hydroxylating the essential amino acid phenylalanine. • This relationship is much like that between cysteine and methionine. • Half of the daily requirement for phenylalanine is for the production of tyrosine; • If the diet is rich in tyrosine itself, the requirements for phenylalanine can be reduced by about 50%. 98 Tyrosine Biosynthesis • Phenylalanine hydroxylase (PAH) is a mixedfunction oxygenase: one atom of oxygen is incorporated into water and the other into the hydroxyl of tyrosine. • The reductant is the tetrahydrofolate-related cofactor tetrahydrobiopterin, which is maintained in the reduced state by the NADH-dependent enzyme dihydropteridine reductase (DHPR). 99 100 Tyrosine Biosynthesis • Missing or deficient phenylalanine hydroxylase results in hyperphenylalaninemia. • Hyperphenylalaninemia is defined as a plasma phenylalanine concentration greater than 2mg/dL (120μM). • The most widely recognized hyperphenylalaninemia (and most severe) is the genetic disease known as phenlyketonuria (PKU). • Patients suffering from PKU have plasma phenylalanine levels >1000μM, whereas the nonPKU hyperphenylalaninemias exhibit levels of 101 Ornithine and Proline Biosynthesis • Glutamate serves as the precursor for the synthesis of both ornithine and proline which are derived from the Δ1-pyrroline-5-carboxylate intermediate in the pathway. • Formation of Δ1-pyrroline-5-carboxylate occurs via the action of the bi-functional enzyme, aldehyde dehydrogenase • The transamination of the tautomeric form of Δ1pyrroline-5-carboxylate (glutamate γ-semialdehyde) results in the generation of ornithine. • The reduction of Δ1-pyrroline-5-carboxylate to 102 proline occurs via the action of pyrroline-5- Ornithine and Proline Biosynthesis 103 Serine biosynthesis Serine can be derived from the glycolytic intermediate, 3phosphoglycerate, in a three-step reaciton pathway. The first reaction is catalyzed by phosphoglycerate dehydrogenase (PHGDH). The second reaction is a simple transamination catalyzed by phosphoserine aminotransferase 1 (PSAT1) which utilizes glutamate as the amino donor and releases 2-oxoglutarate (α-ketoglutarate). The last step in the reaction pathway is catalyzed by phosphoserine phosphatase (PSPH). 104 Glycine Biosynthesis • The main pathway to glycine is a one-step reversible reaction catalyzed by serine hydroxymethyltransferase (SHMT). • This enzyme is a member of the family of onecarbon transferases and is also known as glycine hydroxymethyltransferase. • This reaction involves the transfer of the hydroxymethyl group from serine to the cofactor tetrahydrofolate (THF), producing glycine and N5,N10-methylene-THF 105 Glycine Biosynthesis 106 Glycine Biosynthesis Glycine as a Neurotransmitter • Glycine is involved in many anabolic reactions other than protein synthesis including the synthesis of purine nucleotides, heme, glutathione, creatine and serine. • Also, glycine functions in the central nervous system as an inhibitory neurotransmitter where it participates in regulating signals that process motor and sensory information that permit movement, vision and audition. • Glycine is co-released with GABA which is the primary inhibitory neurotransmitter. 107 Aspartate/Asparagine and Glutamate/Glutamine Biosynthesis Glutamate is synthesized by the reductive amination of 2oxoglutarate (α-ketoglutarate) catalyzed by glutamate dehydrogenase it is thus a nitrogen-incorporating reaction. In addition, glutamate arises by aminotransferase reactions, with the amino nitrogen being donated by a number of different amino acids. Thus, glutamate is a general collector of amino nitrogen 108 Aspartate/Asparagine and Glutamate/Glutamine Biosynthesis Aspartate is formed in a transamination reaction catalyzed by aspartate transaminase, AST. This reaction uses the aspartate α-keto acid analog, oxaloacetate, and glutamate as the amino donor. Aspartate can also be formed by deamination of asparagine catalyzed by asparaginase 109 Aspartate/Asparagine and Glutamate/Glutamine Biosynthesis •Asparagine synthetase and glutamine synthetase, catalyze the production of asparagine and glutamine from their respective α-amino acids. •Glutamine is produced from glutamate by the direct incorporation of ammonia; and this can be considered another nitrogen incorporating reaction. • Asparagine, however, is formed by an amidotransferase reaction. 110 Aspartate/Asparagine and Glutamate/Glutamine Biosynthesis 111 Specialized products of amino acids 112 Specialized products of amino acids • Important products derived from amino acids include heme, purines, pyrimidines, hormones, neurotransmitters, and biologically active peptides. • Small peptides or peptide-like molecules not synthesized on ribosomes fulfill specific functions in cells. • Histamine plays a central role in many allergic reactions. • Neurotransmitters derived from amino acids include γ-aminobutyrate, 5-hydroxytryptamine (serotonin), dopamine, norepinephrine, and 113 epinephrine. Tyrosine-Derived Neurotransmitters / Hormones • Much of the tyrosine that does not get incorporated into proteins is catabolized for energy production. • Another significant fate of tyrosine is conversion to the catecholamines. • The catecholamines are dopamine, norepinephrine, and epinephrine. • All three catecholamines exert effects in numerous locations in the body as either a neurotransmitter or as a hormone. • Within the brain the catecholamines exert their 114 effects as neurotransmitters, in the periphery they Tyrosine-Derived Neurotransmitters / Hormones • Tyrosine is transported into catecholaminesecreting neurons and adrenal medullary cells where catecholamine synthesis takes place. • The first step in the process requires tyrosine hydroxylase which, like phenylalanine hydroxylase (of tyrosine synthesis), requires tetrahydrobiopterin (H4B, or written as BH4) as cofactor. • The tyrosine hydroxylase reaction represents the rate-limiting reaction of catecholamine biosynthesis. • The dependence of tyrosine hydroxylase on H4B necessitates the coupling to the action115of Tyrosine-Derived Neurotransmitters / Hormones • The product of the tyrosine hydroxylase reaction is 3,4-dihydrophenylalanine (L-DOPA; more commonly just DOPA). • The enzyme DOPA decarboxylase then converts DOPA to dopamine. • The enzyme dopamine β-hydroxylase then converts dopamine to norepinephrine. • Dopamine β-hydroxylase is a major vitamin C and copper (Cu2+)-dependent enzyme. • The last step of catecholamine biosynthesis is the 116 Tyrosine-Derived Neurotransmitters / Hormones • The enzyme phenylethanolamine Nmethyltransferase catalyzes this methylation reaction utilizing SAM as a methyl donor. • In addition to epinephrine synthesis, the last reaction generates S-adenosylhomocysteine. • Within the substantia nigra locus of the brain, and some other regions of the brain, synthesis proceeds only to dopamine. • Within the locus coeruleus region of the brain the end product of the pathway is norepinephrine. 117 • Within adrenal medulla chromaffin cells, tyrosine is 118 Tyrosine-Derived Neurotransmitters / Hormones • The actions of norepinephrine and epinephrine are exerted via receptor-mediated signal transduction events. • The receptors to which epinephrine and norepinephrine bind are referred to as adrenergic receptors. • The adrenergic receptors are members of the Gprotein coupled receptor (GPCR) family. • There are two distinct classes of adrenergic receptor identified as the α (alpha) and β (beta) receptors. 119 Tyrosine-Derived Neurotransmitters / Hormones • The α1 class contains the α1A, α1B, and α1D receptors. • The α1 receptor class are coupled to Gq-type Gproteins that activate PLCβ resulting in increases in IP3 and DAG release from membrane PIP2. • The α2 class contains the α2A, α2B, and α2C receptors. • The α2 class of adrenergic receptors are coupled to Gi-type G-proteins that inhibit the activation of adenylate cyclase and therefore, receptor activation results in reduced levels of cAMP and consequently reduced levels of active PKA. • The β class of receptors is composed of three 120 Tyrosine-Derived Neurotransmitters / Hormones • Dopamine binds to dopamineric receptors identified as D-type receptors and there are five subclasses identified as D1, D2, D3, D4, and D5. • All five dopamine receptors belong the the Gprotein coupled receptor (GPCR) family. • The D1 and D5 dopamine receptors are coupled to the activation of Gs-type G-proteins and, therefore, receptor activation results in activation of adenylate cyclase. • The D2, D3, and D4 dopamine receptors are coupled to Gi-type G-proteins and, therefore, receptor 121 • Tryptophan-Derived Neurotransmitters Tryptophan serves as the precursor for the synthesis of serotonin (5-hydroxytryptamine, 5-HT) and melatonin (N-acetyl-5-methoxytryptamine) 122 serotonin • Serotonin is synthesized through a two-step process involving a tetrahydrobiopterin-dependent hydroxylation reaction (catalyzed by tryptophan-5monooxygenase, also called tryptophan hydroxylase) and then a decarboxylation catalyzed by aromatic Lamino acid decarboxylase. • Tryptophan hydroxylase represents the rate-limiting step in serotonin and melatonin synthesis. • READ ON THE FUNCTIONS OF SEROTONIN 123 Melatonin • Melatonin is derived from serotonin within the pineal gland and the retina, where the necessary Nacetyltransferase enzyme is found. • The pineal parenchymal cells secrete melatonin into the blood and cerebrospinal fluid. • Synthesis and secretion of melatonin increases during the dark period of the day and is maintained at a low level during daylight hours. • This diurnal variation in melatonin synthesis is brought about by norepinephrine secreted by the postganglionic sympathetic nerves that innervate 124 the pineal gland. Melatonin • The effects of norepinephrine are exerted through interaction with β-adrenergic receptors. • This leads to increased levels of cAMP, which in turn activate the N-acetyltransferase required for melatonin synthesis. • Melatonin functions by inhibiting the synthesis and secretion of other neurotransmitters such as dopamine and GABA. 125 Creatine Biosynthesis • Creatine synthesis begins in the kidneys using the amino acids arginine and glycine. • The formation of guanidinoacetate from these two amino acids is catalyzed by the enzyme glycine amidinotransferase, also called L-arginine:glycine amidinotransferase. • Guanidinoacetate is transported to the blood and picked up by heptocytes where it is methylated forming creatine. • The methyl donor for this reation is Sadenosylmethionine (SAM) and the reaction is 126 catalyzed by the enzyme guanidinoacetate N- Creatine Biosynthesis • Creatine is released to the blood where is is picked up by the brain and skeletal muscle cells through the action of the transporter. • Within these cells creatine is phosphorylated by creatine kinases (CK; also called creatine phosphokinase, CPK) that generate the high-energy storage compound, creatine phosphate. 127 128 Creatine Biosynthesis • Creatine is used as a storage form of high energy phosphate. • The phosphate of ATP is transferred to creatine, generating creatine phosphate, through the action of creatine phosphokinase. • The reaction is reversible such that when energy demand is high (e.g. during muscle exertion) creatine phosphate donates its phosphate to ADP to yield ATP. • Both creatine and creatine phosphate are found in muscle, brain and blood. • Creatinine is formed in muscle from creatine phosphate by a nonenzymatic dehydration and loss of phosphate. • The amount of creatinine produced is related to muscle mass and remains remarkably constant from day to day. • Creatinine is excreted by the kidneys and the level of excretion (creatinine clearance rate) is a measure of renal function. 129 Glutathione • Glutathione (GSH) is a tripeptide composed of glutamate, cysteine and glycine. • Glutathione serves as a potent reductant eliminating hydroxy radicals, peroxynitrites, and hydroperoxides. • It is conjugated to drugs to make them more water soluble. • It is involved in amino acid transport across cell membranes (the γ-glutamyl cycle) • It is a substrate for the peptidoleukotrienes. • it serves as a cofactor for some enzymatic reactions. • It serves as an aid in the rearrangement of protein disulfide bonds. 130 131 Glutathione • GSH is synthesized in the cytosol of all mammalian cells via the two-step reaction. • The rate of GSH synthesis is dependent upon the availability of cysteine and the activity of the ratelimiting enzyme, γ-glutamylcysteine synthetase (also called glutamate-cysteine ligase, GCL). • The second reaction of GSH synthesis involves the enzyme, glutathione synthetase, which condenses γ-glutamylcysteine with glycine. • Both reactions of GSH synthesis require ATP. 132