* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 07 Adrenoceptor-antagonist
Drug discovery wikipedia , lookup
Orphan drug wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of TRPV1 antagonists wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
NMDA receptor wikipedia , lookup
CCR5 receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Norepinephrine wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
Drug interaction wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
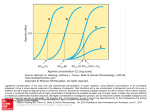
Adrenoceptor blockers Overview • The adrenergic blockers (also called sympathlytic agents) bind to adrenoceptors but do not trigger the usual receptor-mediated intracellular effect • These drugs act by either reversibly or irreversibly blocking the receptor, thus preventing its activation by endogenous catecholamines • The adrenergic antagonists are classified according to the their relative affinities for α or β receptors α-adrenoceptor blocking drugs α-adrenoceptor antagonist drugs Introduction • The main groups of α-adrenoceptor antagonists are: 1) Non-selective α-receptor antagonists: phentolamine 2) α1-selective antagonists: prazosin, doxazosin, terazosin 3) α2-selective antagonists: yohimbine, idazoxan α-adrenoceptor antagonist drugs Pharmacologic effects A. Cardiovascular effects I. α1 Receptor Antagonists: • Blockade of α1 receptors inhibits vasoconstriction induced by endogenous catecholamines • Vasodilation may occur in both arteriolar resistance vessels and veins. The result is a fall in blood pressure due to decreased peripheral resistance (epinephrine reversal) • The fall in blood pressure is opposed by baroreceptor reflexes that cause increases in heart rate and cardiac output, as well as fluid retention α-adrenoceptor antagonist drugs Pharmacologic effects A. Cardiovascular effects I. α1 Receptor Antagonists: • These reflexes are exaggerated if the antagonist also blocks α2 receptors on peripheral sympathetic nerve endings, leading to enhanced release of norepinephrine and increased stimulation of postsynaptic β1 receptors in the heart and kidney α-adrenoceptor antagonist drugs Pharmacologic effects A. Cardiovascular effects II. α2 Receptor Antagonists: • Blockade of α2 receptors in the CNS and on sympathetic nerve endings can increase sympathetic outflow and potentiate the release of norepinephrine from nerve endings, leading to activation of α1 and β1 receptors in the heart and peripheral vasculature with a consequent rise in blood pressure α-adrenoceptor antagonist drugs Pharmacologic effects B. Other effects • The eye: blockade of α1 -receptors in the eye elicits miosis • The nasal cavity: blockade of α1 -receptors elicits nasal stuffiness • The genitourinary tract: blockade of α1 -receptors in the base of the bladder and the prostate decreases resistance to the flow of urine α-adrenoceptor antagonist drugs Specific agents 1. Phenoxybenzamine • Irreversible α-receptor antagonist with long duration of action (14–48 hours or longer) • Phenoxybenzamine is somewhat selective for α1 receptors but less than prazosin • It may inhibit the reuptake of released norepinephrine by presynaptic adrenergic nerve terminals • It also antagonizes the actions of histamin (H1), acetylcholine, and 5-HT α-adrenoceptor antagonist drugs Specific agents 2. Phentolamine • It is a potent competitive α receptor antagonist that has similar affinities for α1 and α2 receptors. Its action is short-lasting (4-hours) • It has minor inhibitory effects at serotonin receptors and agonist effects at muscarinic and H1 and H2 histamine receptors α-adrenoceptor antagonist drugs Specific agents 3. Prazosin, terazosin, and doxazosin • Are selective competitive α1 receptor antagonists • It decrease peripheral vascular resistance and lower arterial blood pressure by causing the relaxation of both arterial and venous smooth muscle., as well as smooth muscles in the prostate • Associated with less tachycardia than occurs with non-selective α-receptor antagonists α-adrenoceptor antagonist drugs Specific agents 4. Tamsulosin • Is a selective α1 antagonist with high affinity for α1A (smooth muscles of the prostate) and α1D than α1B subtype • This selectivity accounts for its relatively minimal effect on blood pressure and its use in BPH α-adrenoceptor antagonist drugs Clinical uses A. Pheochromocytoma: Phenoxybenzamin B. Chronic Hypertension: α1-selective antagonists e.g. prazosin, doxazosin, and terazosin C. Peripheral vascular disease (e.g. Raynaud's phenomenon): prazosin or phenoxybenzamine D. Urinary obstruction in patients with benign prostatic hyperplasia (BPH): selective α1 receptor antagonists (Prazosin, doxazosin, and terazosin, tamsulosin) Raynaud's phenomenon α-adrenoceptor antagonist drugs Adverse effect 1) Orthostatic hypotension: especially first dose of selective α1 antagonist prazosin and non-selective agents 2) Marked reflux tachycardia (non selective agents): contraindicated in patients with decreased coronary perfusion 3) Nasal stuffiness 4) Inhibition of ejaculation (non-selective agents) 5) CNS: fatigue, sedation, & nausea (phenoxybenzamine) β-adrenoceptor blocking drugs Introduction • They differ in their relative affinities for β1 and β2 receptors, intrinsic sympathimimetic activity, in CNS effect, and in pharmacokinetics • None of the clinically available β-receptor antagonists are absolutely specific for β1 receptors: their selectivity is dose-dependent; it tends to diminish at higher drug concentrations • There are no clinically useful β2 antagonists • The names of all β-blockers end in “-olol” except for labetalol and carvedilol Pharmacokinetic Properties of the BetaReceptor Antagonists • Absorption: well absorbed after oral administration & peak concentrations occur 1–3 hours after ingestion • Bioavailability: on average, only about 25% of propranolol, the prototype of β–blockers, reaches the systemic circulation b/c it undergoes extensive hepatic first-pass metabolism Pharmacokinetic Properties of the BetaReceptor Antagonists • Distribution: the β–adrenergic antagonists are rapidly distributed and have large volumes of distribution. Propranolol and penbutolol are quite lipophilic and readily BBB • Clearance: most β–adrenergic antagonists have elemination half-lives in the range of 3–10 hours • Esmolol has a half-life of about 10 minutes. The drug contains an ester linkage, and it is hydrolyzed rapidly by esterases in erythrocytes β-adrenoceptor antagonist drugs Pharmacologic effects A. Cardiovascular effects • Blocked of β1-receptor will produce both negative inotropic and chronotropic effects on the heart: cardiac output, work, and oxygen consumption are decreased • Blockade of vasodilation • Blocked of receptors in the kidney will inhibit the release of renin caused by the sympathetic nervous system • This decreased blood pressure/hypotensive effect triggers a reflex peripheral vasoconstriction that is reflected in reduced blood flow to the periphery β receptors prevents β2-mediated β-adrenoceptor antagonist drugs Pharmacologic effects b. Respiratory system: blockade of the β2 receptors in bronchial smooth muscle may lead to an increase in airway resistance, particularly in patients with asthma & COPD c. Local anesthetic action, also known as "membrane-stabilizing" action, is a prominent effect of several β-blockers (e.g. acebutolol, labetalol, metoprolol, & penbutolol) β-adrenoceptor antagonist drugs Pharmacologic effects d. Metabolic and endocrine effect • β-Receptor antagonists modify the metabolism of carbohydrates and lipids • β–blockade lead to decreased glycogenolysis in the human liver and decreased glucose release (β2receptor blockade) • Therefore, β-blockers should be used with caution in type I diabetic patients β-adrenoceptor antagonist drugs Pharmacologic effects d. Metabolic and endocrine effect • The chronic use of selective β1- and non selective βadrenoceptor antagonists has been associated with increased plasma VLDL and decreased of HDL cholesterol • Such effect is less likely to occur with blockers possessing intrinsic sympathomimetic activity (partial agonists) β-adrenoceptor antagonist drugs Specific agents I. Nonselective β-adrenergic antagonists • Agents: propranolol (prototype), timolol, nadolol, levobunolol , & Carteolol • They lack selectivity and block both β1 and β2 receptors with equal affinity β-adrenoceptor antagonist drugs Specific agents II. β1-adrenergic antagonists (cardioselective) • Agents: metoprolol, acebutolol, atenolol, esmolol, bisoprolol, & nebivolol • Drugs that preferentially block the β1 receptors : eliminate the unwanted bronchoconstrictor effect (β2 effect) of propranolol seen among asthmatic patients • β1-selective antagonists may be preferable in patients with diabetes or peripheral vascular disease when therapy with a blocker is required β-adrenoceptor antagonist drugs Specific agents II. β1-adrenergic antagonists (cardioselective) • Nebivolol is the most highly selective β1-adrenergic receptor blocker, and it has the additional quality of eliciting vasodilation • This may be due to an action of the drug on endothelial nitric oxide pathway β-adrenoceptor antagonist drugs Specific agents III. Partial β-adrenergic agonists • Agents: Pindolol, acebutolol, carteolol, bopindolol, oxprenolol, celiprolol, & penbutolol • They have the ability to weakly stimulate both β1 and β2 receptors and are said to have intrinsic sympathomimetic activity (ISA) β-adrenoceptor antagonist drugs Specific agents III. Partial β-adrenergic agonists • The result of these opposing actions is a much diminished effect on cardiac rate and cardiac output compared to that of β-blockers without ISA. Therefore, these partial agonists may be less likely to cause bradycardia • They minimize the disturbances of lipid and carbohydrate metabolism that are seen with other βblockers β-adrenoceptor antagonist drugs Specific agents III. Antagonists of both α- and β-adrenoceptors • Agents: Labetalol, carvedilol, medroxalol, & bucindolol • These are reversible β-blockers with concurrent α1blocking actions that produce peripheral vasodilation, thereby reducing blood pressure • They contrast with the other β-blockers that produce peripheral vasoconstriction, and they are therefore useful in treating hypertensive patients for whom increased peripheral vascular resistance is undesirable Therapeutic uses of Beta-Receptor–Blocking Drugs I. Cardiovascular applications a) Hypertension b) Ischemic heart disease (IHD) c) Heart failure d) Cardiac arrhythmias Therapeutic uses of Beta-Receptor–Blocking Drugs II. Non-cardiovascular applications A. Glaucoma: topical administration of beta-blockers (e.g. timolol, betaxolol, carteolol, levobunolol, and metipranolol) reduces intraocular pressure by decreasing the production of aqueous humor by the ciliary body, which is physiologically activated by cAMP B. Hyperthyroidsim: propranolol Therapeutic uses of Beta-Receptor–Blocking Drugs II. Non-cardiovascular applications C. Migrane prophylaxis: Propranolol, metoprolol and probably also atenolol, timolol, and nadolol. The mechanism may depend on the blockade of catecholamine-induced vasodilation in the brain vasculature D. Performance anxiety (stage fright) : propranolol E. Tremor: propranolol due to reduced β2-alteration of neuromuscular transmission Choice of a β-adrenoceptor antagonist drug • The various β-receptor antagonists that are used for the treatment of HTN and angina appear to have similar efficacies (i.e. interchangable). • Selection of the most appropriate drug for an individual patient should be based on PK and PD differences among the drugs, cost, and whether there are concurrent medical problems Choice of a β-adrenoceptor antagonist drug • For some diseases (e.g., myocardial infarction, migraine, cirrhosis with varices, and congestive heart failure), it should not be assumed that all members of this class of drugs are interchangeable; the appropriate drug should be selected from those that have documented efficacy for the disease • For example in heart failure clinical trials have demonstrated that at least three antagonists— metoprolol, bisoprolol, and carvedilol—are effective in reducing mortality associated with chronic heart failure Adverse effects of β-adrenoceptor antagonist drug 1) Bradycardia (most common): normal response to βadrenoceptor blockade 2) Bronchoconstriction: β2 receptor blockade associated with the use of non-selective β-blockers (e.g. propranolol) 3) Hypoglycemia in type I diabetic patients who are subject to frequent hypoglycemic episodes 4) Coolness of hands & feet in winter 5) CNS effects: include fatigue, sleep disturbances (including insomnia and nightmares), and depression • Hydrophilic drugs nadolol or atenolol are associated with a lower incidence of central nervous system adverse effects Adverse effects of β-adrenoceptor antagonist drug 6) Cardiac arrhythmias: • Treatment with β-blockers must never be stopped quickly because of the risk of precipitating cardiac arrhythmias, which may be severe especially drugs with short half-lives, such as propranolol and metoprolol • The β-blockers must be tapered off gradually for 1 week. Long-term treatment with a β antagonist leads to up-regulation of the β-receptor. On suspension of therapy, the increased receptors can worsen angina or hypertension