* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Identifying genetic susceptibility factors for
Genetic drift wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Behavioural genetics wikipedia , lookup
Biology and consumer behaviour wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Genomic imprinting wikipedia , lookup
Epigenetics of diabetes Type 2 wikipedia , lookup
Epigenetics of human development wikipedia , lookup
Gene desert wikipedia , lookup
Polymorphism (biology) wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Quantitative trait locus wikipedia , lookup
Gene nomenclature wikipedia , lookup
Medical genetics wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Gene therapy wikipedia , lookup
Gene expression profiling wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Gene expression programming wikipedia , lookup
Heritability of IQ wikipedia , lookup
Population genetics wikipedia , lookup
Genome-wide association study wikipedia , lookup
Genome evolution wikipedia , lookup
History of genetic engineering wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Genetic engineering wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Human genetic variation wikipedia , lookup
Designer baby wikipedia , lookup
Genome (book) wikipedia , lookup
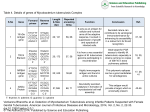
Clinical Science (2000) 98, 245–250 (Printed in Great Britain) G L A X O / M R S P A P E R Identifying genetic susceptibility factors for tuberculosis in Africans: a combined approach using a candidate gene study and a genome-wide screen* Richard BELLAMY Department of Infectious Diseases, University Hospital of Wales, Cardiff CF14 4XW, Wales, U.K. A B S T R A C T There is convincing evidence that host genes affect the outcome of infection in human tuberculosis. Two complementary strategies were used to identify the genes involved. A linkagebased genome-wide screen was carried out to locate the positions of genes exerting a major population-wide effect on tuberculosis susceptibility. A candidate-gene-based case–control study was used to examine the effects of genes that may exert a more moderate effect on risk of clinical tuberculosis. The genome screen was conducted in two stages. In the first stage 299 microsatellite markers, spanning all 23 chromosomes, were typed in 92 independent sib-pairs, and seven regions showed some evidence of co-segregation with the disease. These seven regions were examined in a second set of 81 sib-pairs, and markers on chromosomes 15q and Xq showed evidence of linkage to tuberculosis. An X chromosome susceptibility gene may contribute to the excess of males with tuberculosis observed in many populations. The candidate gene approach compared the frequency of polymorphisms in several genes in over 400 subjects with smearpositive pulmonary tuberculosis and 400 ethnically matched healthy controls. Polymorphisms in genes encoding natural-resistance-associated macrophage protein, vitamin D receptor and mannose-binding lectin were associated with tuberculosis. These results suggest that many genes may be involved in determining host susceptibility to tuberculosis, and highlight the importance of using several different study methods to locate them. INTRODUCTION It is estimated that one-third of the World’s population is infected with Mycobacterium tuberculosis, but that only one in ten of those infected ever develop clinical disease [1,2]. There are many well known risk factors for tuberculosis, including HIV infection, advanced age, malnutrition, alcohol abuse, diabetes and corticosteroids. However, many patients do not have any obvious underlying risk factor, and there is now convincing evidence that individual variability in tuberculosis susceptibility is partly determined by host genes [3]. Racial differences in resistance to tuberculosis may be determined by history of exposure among previous generations [4,5], and concordance for tuberculosis is higher among identical than non-identical twins [6,7]. * This paper was presented at the Glaxo/MRS Young Investigator session at the MRS Meeting, Royal College of Physicians, London, on 19 May 1999. Key words : genetic susceptibility, genome screen, mannose-binding lectin, Nramp, tuberculosis, vitamin D receptor. Abbreviations : MBL, mannose-binding lectin ; NRAMP\Nramp, natural-resistance-associated macrophage protein ; VDR, vitamin D receptor. Correspondence : e-mail bellamyrj!cardiff.ac.uk # 2000 The Biochemical Society and the Medical Research Society 245 246 R. Bellamy M. tuberculosis is a facultative intracellular pathogen which utilizes the macrophage as its host cell. Resistance to M. tuberculosis involves a complex interaction between the bacteria and the host immune system. Several mechanisms have been proposed to explain how the macrophage combats mycobacterial resistance. These include the generation of reactive oxygen and reactive nitrogen intermediates, acidification of phagosomes, phagosome–lysosome fusion and the limitation of intraphagosomal iron [8]. It is uncertain how M. tuberculosis evades these mechanisms. Hypotheses include invading macrophages via C3b receptors to evade the production of reactive oxygen intermediates [9], production of ammonia to resist phagosome acidification [10], and inhibition of phagosome–lysosome fusion [11]. Cytokines are believed to play a key role in mycobacterial resistance. Macrophages are activated by interferon γ, tumour necrosis factor α, vitamin D and interleukin 6 [11]. These cytokines may play an important role in resistance to tuberculosis, although they may also be responsible for much of the tissue destruction that occurs in this disease [12]. Two approaches were used to investigate the role of host genes in susceptibility to tuberculosis in Africans. A linkage study was used to screen the whole human genome for regions containing potential major tuberculosis-susceptibility loci. This approach is systematic and comprehensive, but has a relatively low power of detection and would fail to identify any genes exerting only a moderate effect on disease susceptibility. It has been calculated that if a susceptibility allele with a population frequency of 0.5 exerts a 2-fold increased risk of disease, 2498 sib-pairs would be required to provide 80 % power to detect the effect by linkage analysis [13]. An association (case–control) study would only require 340 cases to provide the same power [13], and can therefore detect smaller population-wide genetic effects. Association studies cannot currently be used to perform genome-wide screens, as at least 3000 markers would need to be typed. Our case–control study was therefore restricted to candidate genes. The study described in this review was approved by the joint ethics committee of the Gambian Government and the Medical Research Council. Verbal consent was obtained from all study subjects. RESULTS OF THE GENOME-WIDE SCREEN The genome screen was carried out using sib-pair families. These are families with two or more full siblings affected by the same disease (tuberculosis in this case). A family containing two affected siblings provides one sibpair, one containing three affected siblings provides two fully independent sib-pairs, and if there are four affected siblings this is equivalent to three independent sib-pairs, # 2000 The Biochemical Society and the Medical Research Society etc. If a genetic marker locus is linked to a major diseasesusceptibility gene, then the siblings will share the parental alleles that they have inherited at that locus more often than would be expected by chance. This nonparametric system of analysis is not dependent on the mode of inheritance, and a major disease-susceptibility locus should be identifiable regardless of whether it is Xlinked or autosomal, dominant or recessive. The genome screen was carried out in two stages, with approximately half of the sib-pairs in each stage. This is more efficient than carrying out the whole genome-wide screen on all of the families. In the first stage, 299 microsatellite markers covering all 23 chromosomes were typed in 67 Gambian families including 73 fully independent sib-pairs, and in 16 KwaZulu–Natal families including 19 independent sib-pairs. A total of seven regions, on chromosomes 3, 5, 6, 8, 9, 15 and X, showed nominal evidence for linkage to tuberculosis (R. Bellamy, N. Beyers, C. Ruwende, H. C. Whittle, E. Hoal van Helden, T. Corrah, R. Wilkinson, K. P. W. J. McAdam, W. Amos, P. van Helden and A. V. S. Hill, unpublished work). These results could have been due to genuine linkage or simply to chance, because of the large number of loci typed, and therefore needed replication in a second series of families. No region showed evidence of strong linkage, indicating that in these populations genetic susceptibility to tuberculosis is not determined by a single-gene effect. In the second round of the screen, 22 markers from the seven regions identified in the first stage of the screen were typed in 12 Gambian sib-pair families and in 41 families including 69 independent sib-pairs from the Western Cape, South Africa. Two regions, on chromosome Xq26 and the pericentromeric region of chromosome 15q, showed evidence of linkage to a putative tuberculosis-susceptibility gene (R. Bellamy, N. Beyers, C. Ruwende, H. C. Whittle, E. Hoal van Helden, T. Corrah, R. Wilkinson, K. P. W. J. McAdam, W. Amos, P. van Helden and A. V. S. Hill, unpublished work). Several candidate genes lie in the region of interest on Xq26, and the CD40 ligand in particular is worthy of further investigation. It is of note that there are approximately twice as many male as female patients with tuberculosis in The Gambia and South Africa (R. Bellamy, unpublished work ; [14]). This significant male excess has been observed in many different ethnic groups [15–17], and our results suggest that it may be due to an X-linked tuberculosis-susceptibility gene. CANDIDATE GENE STUDY Subjects for the case–control study were all recruited from The Gambia. The relative ethnic homogeneity of the population [18] make this an ideal population for case–control studies. All patients were HIV-negative Genetic susceptibility to tuberculosis adults (over 16 years old) with smear-positive pulmonary tuberculosis. The control group consisted of HIVnegative, healthy, unrelated blood donors retrospectively matched to the patients by ethnic group as far as numbers allowed. To have 90 % power to detect a statistically significant difference (P 0.05) between the number of tuberculosis cases and controls with a genotype which has a population frequency of 10 % and which exerts an odds ratio of 2.0 on a 2i2 contingency table would require 402 cases. Thus a greater number than this of cases and of ethnically matched controls were recruited for the candidate gene study to provide this power. Several candidate gene polymorphisms have been typed in this case–control study [19], and associations have been detected for natural-resistance-associated macrophage protein (NRAMP1), vitamin D receptor (VDR) and mannose-binding lectin (MBL) gene variants [20–22]. NRAMP Among inbred strains of mice, natural resistance to infection with several antigenically unrelated intracellular pathogens is controlled by a single dominant gene on mouse chromosome 1, designated Bcg (also known as Lsh\Ity) [23,24]. Two distinct non-overlapping phenotypes are recognized, Bcgs and Bcgr, which are respectively susceptible and resistant to the early stage of infection with Mycobacterium bovis (BCG), M. intracellulare, M. lepraemurium, Leishmania donovani and Salmonella typhimurium [23–28]. A candidate gene for Bcg has been isolated by positional cloning and designated Nramp1 (murine natural-resistance-associated macrophage protein) [29]. Nramp1 and Bcg\Lsh\Ity were proven to be identical by the production of a genedisrupted Nramp1 knockout mouse [30], and an Nramp1 transgenic mouse which restored the wild-type resistant phenotype [31]. It has been shown that Nramp1 is not the sole major gene determining resistance to infection with virulent M. tuberculosis [32] in mice, but it may have a more complex role in murine M. tuberculosis immunity in conjunction with other host genes. The human homologue of the Nramp1 gene, designated NRAMP1, has been cloned and mapped to chromosome 2q35 [33,34]. Several polymorphisms have been described in NRAMP1, and it has been suggested that they could influence NRAMP1 function [34,35]. Weak evidence of linkage has been found between NRAMP1 markers and susceptibility to leprosy in 20 families from Vietnam (P 0.02), although this was not confirmed in seven families from French Polynesia [36,37]. Weak evidence of linkage to the NRAMP1 locus was also found in our own study of tuberculosis in families (P l 0.06) (R. Bellamy, unpublished work) and in a study of 98 Brazilian families (P l 0.025) [38]. The absence of strong evidence of linkage in these studies Combined analysis of NRAMP1 genetic variants The genetic variants are a single-base substitution (G C) in intron 4 (INT4) and a deletion (del) in the 3h untranslated region (3h UTR). Odds ratios (with 95 % confidence intervals in parentheses) and P values (Yates’ ; 1 degree of freedom) shown are for Chi-square comparisons with the GG/jj genotype. An overall 4i2 Chi-square test on combined genotypes shows strong association with tuberculosis (P l 0.000008). Table 1 No. of subjects INT4/3h UTR genotype Tuberculosis cases Controls Odds ratio P value GG/jj GC/jj GG/jdel GC/jdel 191 45 118 31 251 33 84 10 1.0 1.79 (1.07–3.00) 1.85 (1.30–2.62) 4.07 (1.86–9.12) – 0.02 0.0005 0.0001 indicates that NRAMP1 is not the sole determinant of host genetic susceptibility to mycobacterial infections in humans. Case–control studies have much greater power than linkage studies for investigating the complex role of candidate genes in multifactorial diseases. Six NRAMP1 polymorphisms were typed in our large Gambian case– control study. Four polymorphisms were strongly associated with tuberculosis in this population (overall P l 0.000008 ; one gene variant was not associated and the other was too rare to evaluate) [20]. Individuals who possessed two variant alleles were 4-fold overrepresented among the tuberculosis cases compared with the healthy controls (Table 1 ; [20]). This result demonstrates that, although NRAMP1 is not the sole determinant of host tuberculosis susceptibility, it is an important mycobacteria-susceptibility gene in humans as well as in mice. The functions of Nramp1\NRAMP1 remain unknown, although it is believed that they may restrict the availability of iron to intraphagosomal mycobacteria [39]. VDR Genetic variation in bone mineral density has been shown to be associated with polymorphisms in the VDR gene in many, although not all, populations studied [40]. Epidemiological evidence suggests a link between vitamin D deficiency and susceptibility to tuberculosis [41,42], and vitamin D has been shown to have beneficial effects in cutaneous tuberculosis [43]. Vitamin D is an important immunoregulatory hormone [44]. The active metabolite of vitamin D, 1,25-dihydroxyvitamin D (1,25$ dihydroxycholecalciferol), activates monocytes, stimulates cell-mediated immunity and suppresses lymphocyte proliferation, immunoglobulin production and cytokine synthesis [44]. In vitro studies suggest that vitamin D metabolites can enhance the ability of human monocytes # 2000 The Biochemical Society and the Medical Research Society 247 248 R. Bellamy Tuberculosis and VDR genotype The frequency of each genotype is given as an actual value and (in parentheses) as a percentage. The overall distribution of VDR genotypes is significantly different between cases and controls (3i2 Chi-square l 6.98 ; 2 degrees of freedom, P l 0.03). The tt genotype was less common in tuberculosis cases compared with controls (Yates’ Chi-square l 6.06 ; 1 degree of freedom, P l 0.01). Table 2 Frequency (no.) (%) Genotype Tuberculosis cases Controls TT Tt tt Total 204 (50) 177 (43) 27 (6.6) 408 188 (45) 177 (43) 49 (12) 414 to restrict the growth of intracellular M. tuberculosis [45]. Alveolar macrophages in the lungs of tuberculosis patients have been shown to produce 1,25-dihydroxyvitamin D [46], which could therefore be involved in the $ host immune response to M. tuberculosis in vivo. A polymorphism in codon 352 of the VDR gene was typed in our Gambian tuberculosis case–control study. The genotype associated with low bone mineral density, which has been designated tt, was significantly underrepresented in the tuberculosis cases compared with the controls (P l 0.01) (Table 2 ; [21]). The odds ratio for subjects of genotype tt having tuberculosis compared with those of genotypes TT\Tt combined was 0.53 (95 % confidence interval 0.31–0.88), suggesting that tt homozygotes may be resistant to clinical tuberculosis. Subjects with this genotype have also been found to be less likely to develop persistence of hepatitis B virus infection [21] and the lepromatous form of leprosy [47]. Further studies will be required to investigate how VDR polymorphism may influence susceptibility to infectious diseases. throughout Africa and we might therefore expect strong selection against MBL variants. It has been suggested that heterozygote advantage may maintain MBL variant alleles at high frequency by conferring resistance to mycobacterial diseases [50]. In our case–control study in The Gambia it was found that the frequency of the common African variant MBL allele (codon 57) was lower among tuberculosis cases than controls (P l 0.037) [22]. This result will require confirmation in other populations due to its borderline statistical significance. However, it would be fascinating if MBL deficiency, described as the world’s commonest immune deficiency, has been selected for by conferring resistance to tuberculosis. CONCLUSIONS Recent work on subjects with extreme susceptibility to atypical mycobacteria and other intracellular pathogens has identified rare immune deficiencies due to abnormalities of the genes encoding the interferon γ receptor, interleukin 12 and the interleukin 12 receptor [51–54]. These studies provide important candidate genes for investigation in large population-based studies of common, related infections. It is likely that a large number of host genes are involved in susceptibility to mycobacteria and other infectious diseases. A variety of study designs, including family-based linkage studies, large-scale population case–control studies, investigation of unexplained immune deficiencies and comparisons with animal models of disease, will be required to identify further host genes and investigate their interactions. Identifying the critical determinants of host genetic susceptibility to specific pathogens will further our understanding of the pathogenesis of these diseases, and hopefully suggest new treatment strategies. MBL MBL is a calcium-dependent serum lectin. It interacts with the immune system by acting as an opsonin to promote phagocytosis and by activating the complement cascade. Three co-dominant single-base substitutions in codons 52, 54 and 57 of the MBL gene result in reduced serum MBL concentrations. Individuals with two variant alleles have extremely low or undetectable levels of serum MBL, and are predisposed to recurrent childhood infections and possibly to infections in adult life [48]. However, MBL variant alleles are extremely common and have a combined frequency of 22.5 % among a healthy British population, with around 4.6 % of the population possessing two mutant alleles [49]. Among Gambians, MBL variant alleles have a combined frequency of 31 %, and around 10 % of the population carry two mutant alleles [22]. This is surprisingly high, because infections are a frequent cause of premature death # 2000 The Biochemical Society and the Medical Research Society ACKNOWLEDGMENTS I am grateful to Professor A. V. S. Hill for helpful discussions, and to the Wellcome Trust for funding. REFERENCES 1 Dolin, P. J., Raviglione, M. C. and Kochi, A. (1994) Global tuberculosis incidence and mortality during 1990–2000. Bull. WHO 72, 213–220 2 Murray, C. J. L., Styblo, K. and Rouillon, A. (1990) Tuberculosis in developing countries : burden, intervention and cost. Bull. Int. Union Tuberc. Lung Dis. 65, 6–24 3 Bellamy, R. (1998) Genetic susceptibility to tuberculosis in human populations. Thorax 53, 588–593 4 O’Brien, S. J. (1991) Ghetto legacy. Curr. Biol. 1, 209–211 5 Stead, W. W. (1992) Genetics and resistance to tuberculosis : could resistance be enhanced by genetic engineering ? Ann. Int. Med. 116, 937–941 Genetic susceptibility to tuberculosis 6 Kallmann, F. J. and Reisner, D. (1942) Twin studies on the significance of genetic factors in tuberculosis. Am. Rev. Tuberc. 47, 549–574 7 Comstock, G. W. (1978) Tuberculosis in twins : a reanalysis of the Prophit study. Am. Rev. Respir. Dis. 117, 621–624 8 Flesch, I. E. A. and Kaufmann, S. H. E. (1990) Role of cytokines in tuberculosis. Immunobiology 189, 316–339 9 Schlesinger, L. S., Bellinger-Kawahara, C. G., Payne, N. R. and Horwitz, M. A. (1990) Phagocytosis of Mycobacterium tuberculosis is mediated by human monocyte complement receptors and complement component C3. J. Immunol. 150, 2920–2930 10 Gordon, A. H., D’Arcy Hart, P. and Young, M. R. (1980) Ammonia inhibits phagosome–lysosome fusion in macrophages. Nature (London) 286, 79–82 11 Armstrong, J. A. and Hart, P. D. (1971) Response of cultured macrophages to Mycobacterium tuberculosis, with observations on the fusion of lysosomes with phagosomes. J. Exp. Med. 134, 713–740 12 Rook, G. A. W. (1988) Role of activated macrophages in the immunopathology of tuberculosis. Br. Med. Bull. 44, 611–623 13 Risch, N. and Merikangas, K. (1996) The future of genetic studies of complex human diseases. Science 273, 1516–1517 14 Kustner, H. G. V. (1979) Trends in four major communicable diseases. S.A. Med. J. 55, 460–473 15 Rieder, H. L., Kelly, G. D., Bloch, A. B., Cauthen, G. M. and Snider, D. E. (1991) Tuberculosis diagnosed at death in the United States. Chest 100, 678–681 16 Heng, B. H. and Tan, K. K. (1991) Three decades of tuberculosis in Singapore. Bull. Int. Union Tuberc. Lung Dis. 66, 125–128 17 Medical Research Council Cardiothoracic Epidemiology Group (1992) National survey of notifications of tuberculosis in England and Wales in 1988. Thorax 47, 770–775 18 Allsopp, C. E. M., Harding, R. M., Taylor, C. et al. (1992) Interethnic genetic differentiation in Africa : HLA class I antigens in The Gambia. Am. J. Hum. Genet. 50, 411–421 19 Bellamy, R., Ruwende, C., Corrah, T., McAdam, K. P. W. J., Whittle, H. C. and Hill, A. V. S. (1998) Assessment of interleukin 1 and other candidate gene polymorphisms in host susceptibility to tuberculosis. Tuberc. Lung Dis. 79, 83–89 20 Bellamy, R., Ruwende, C., Corrah, T., McAdam, K. P. W. J., Whittle, H. C. and Hill, A. V. S. (1998) Variation in the human NRAMP1 gene and human tuberculosis in an African population. N. Engl. J. Med. 338, 640–644 21 Bellamy, R., Ruwende, C., Corrah, T. et al. (1999) Resistance to tuberculosis and chronic hepatitis B virus infection in Africans and variation in the vitamin D receptor gene. J. Infect. Dis. 179, 721–724 22 Bellamy, R., Ruwende, C., McAdam, K. P. W. J. et al. (1998) Mannose binding protein deficiency is not associated with increased susceptibility to malaria, hepatitis B carriage nor tuberculosis in Africans. Q.J. Med. 91, 13–18 23 Plant, J. E. and Glynn, A. (1976) Genetics of resistance to infection with Salmonella typhimurium in mice. J. Infect. Dis. 133, 72–78 24 Bradley, D. J. (1977) Genetic control of Leishmania populations within the host. II. Genetic control of acute susceptibility of mice to L. donovani infection. Clin. Exp. Immunol. 30, 130–140 25 Gros, P., Skamene, E. and Forget, A. (1981) Genetic control of natural resistance to Mycobacterium bovis BCG. J. Immunol. 127, 417–421 26 Goto, Y., Buschman, E. and Skamene, E. (1989) Regulation of host resistance to Mycobacterium intracellulare in vivo and in vitro by the Bcg gene. Immunogenetics 30, 218–221 27 Skamene, E., Gros, P., Forget, A., Patel, P. J. and Nesbitt, M. (1984) Regulation of resistance to leprosy by chromosome 1 locus in the mouse. Immunogenetics 19, 117–120 28 Skamene, E., Gros, P., Forget, A., Kongshavn, P. A. L., St.-Charles, C. and Taylor, B. A. (1982) Genetic regulation 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 of resistance to intracellular pathogens. Nature (London) 297, 506–509 Vidal, S. M., Malo, D., Vogan, K., Skamene, E. and Gros, P. (1993) Natural resistance to infection with intracellular parasites : isolation of a candidate gene for Bcg. Cell 73, 469–485 Vidal, S., Tremblay, M. L., Govoni, G. et al. (1995) The Ity\Lsh\Bcg locus : natural resistance to infection with intracellular parasites is abrogated by disruption of the Nramp1 gene. J. Exp. Med. 182, 655–666 Govoni, G., Vidal, S., Gauthier, S., Skamene, E., Malo, D. and Gros, P. (1996) The Bcg\Ity\Lsh locus : genetic transfer of resistance to infections in C57BL\6J mice transgenic for the Nramp1G"'* allele. Infect. Immun. 64, 2923–2929 Medina, E. and North, R. J. (1996) Evidence inconsistent with a role for the Bcg gene (Nramp1) in resistance of mice to infection with virulent Mycobacterium tuberculosis. J. Exp. Med. 183, 1045–1051 Cellier, M., Govoni, G., Vidal, S. et al. (1994) Human natural resistance-associated macrophage protein : cDNA cloning, chromosomal mapping, genomic organization, and tissue-specific expression. J. Exp. Med. 180, 1741–1752 Blackwell, J. M., Barton, H., White, J. K. et al. (1995) Genomic organization and sequence of the human NRAMP gene : identification and mapping of a promoter region polymorphism. Mol. Med. 1, 194–205 Liu, J., Fujiwara, M., Buu, N. T. et al. (1995) Identification of polymorphisms and sequence variants in the human homologue of the mouse natural resistance-associated macrophage protein gene. Am. J. Hum. Genet. 56, 845–853 Abel, L., Sanchez, F. O., Oberti, J. et al. (1998) Susceptibility to leprosy is linked to the human NRAMP1 gene. J. Infect. Dis. 177, 133–145 Roger, M., Levee, G., Chanteau, S., Gicquel, B. and Schurr, E. (1997) No evidence for linkage between leprosy susceptibility and the human natural resistance-associated macrophage protein 1 (NRAMP1) gene in French Polynesia. Int. J. Leprosy 65, 197–202 Shaw, M. A., Collins, A., Peacock, C. S. et al. (1997) Evidence that genetic susceptibility to Mycobacterium tuberculosis in a Brazilian population is under oligogenic control : linkage study of the candidate genes NRAMP1 and TNFA. Tuberc. Lung Dis. 78, 35–45 Fleming, M. D., Romano, M. A., Su, M. A., Garrick, L. M., Garrick, M. D. and Andrews, N. C. (1998) Nramp2 is mutated in the anaemic Belgrade (b) rat : evidence of a role for Nramp2 in endosomal iron transport. Proc. Natl. Acad. Sci. U.S.A. 95, 1148–1153 Eisman, J. A. (1996) Vitamin D receptor gene variants : implications for therapy. Curr. Opin. Genet. Dev. 6, 361–365 Davies, P. D. O. (1985) A possible link between vitamin D deficiency and impaired host defence to Mycobacterium tuberculosis. Tubercle 66, 301–306 Bellamy, R. J. and Hill, A. V. S. (1998) Host genetic susceptibility to human tuberculosis. In Genetics and Tuberculosis (Chadwick, D. J. and Cardew, G., eds.), pp. 3–23, Wiley, Chichester MacRae, D. E. (1947) Calciferol treatment of lupus vulgaris. Br. J. Dermatol. 59, 333–338 Manolagas, S. C., Yu, X.-P., Girasole, G. and Bellido, T. (1994) Vitamin D and the hematolymphopoietic tissue : a 1994 update. Semin. Nephrol. 14, 129–143 Denis, M. (1991) Killing of Mycobacterium tuberculosis within human monocytes : activation by cytokines and calcitriol. Clin. Exp. Immunol. 84, 200–206 Cadranel, J., Hance, A. J., Milleron, B., Paillard, F., Akoun, G. M. and Garabedian, M. (1988) The production of 1,25(OH) D by cells recovered by bronchoalveolar # role $ of this metabolite in calcium lavage and the homeostasis. Am. Rev. Respir. Dis. 138, 984–989 Roy, S., Frodsham, A., Saha, B., Hazra, S. K., MascieTaylor, C. G. N. and Hill, A. V. S. (1999) Association of vitamin D receptor genotype with leprosy type. J. Infect. Dis. 179, 187–191 Turner, M. W. (1996) Mannose-binding lectin : the pluripotent molecule of the innate immune system. Immunol. Today 17, 532–540 # 2000 The Biochemical Society and the Medical Research Society 249 250 R. Bellamy 49 Mead, R., Jack, D., Pembrey, M., Tyfield, L. and Turner, M. (1997) Mannose-binding lectin alleles in a prospectively recruited UK population. Lancet 349, 1669–1670 50 Garred, P., Harboe, M., Oettinger, T., Koch, C. and Svejgaard, A. (1994) Dual role of mannan-binding protein in infections : another case of heterosis ? Eur. J. Immunogenet. 21, 125–131 51 Newport, M. J., Huxley, C. M., Huston, S. et al. (1996) A mutation in the interferon-γ-receptor gene and susceptibility to mycobacterial infection. N. Engl. J. Med. 335, 1941–1949 # 2000 The Biochemical Society and the Medical Research Society 52 Dorman, S. E. and Holland, S. M. (1998) Mutation in the signal-transducing chain of the interferon-γ receptor and susceptibility to mycobacterial infection. J. Clin. Invest. 101, 2364–2369 53 Altare, F., Durandy, A., Lammas, D. et al. (1998) Impairment of mycobacterial immunity in human interleukin-12 receptor deficiency. Science 280, 1432–1435 54 Altare, F., Lammas, D., Revy, P. et al. (1998) Inherited interleukin 12 deficiency in a child with Bacille Calmette–Guerin and Salmonella enteridis disseminated infection. J. Clin. Invest. 102, 2035–2040