* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ABCA3 Gene Mutations in Newborns with Fatal
Genetic code wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Tay–Sachs disease wikipedia , lookup
Genome evolution wikipedia , lookup
Gene expression profiling wikipedia , lookup
Gene nomenclature wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Protein moonlighting wikipedia , lookup
Gene therapy wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Public health genomics wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Genome (book) wikipedia , lookup
Designer baby wikipedia , lookup
Oncogenomics wikipedia , lookup
Microevolution wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
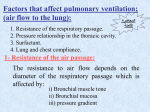
The new england journal of medicine original article ABCA3 Gene Mutations in Newborns with Fatal Surfactant Deficiency Sergey Shulenin, Ph.D., Lawrence M. Nogee, M.D., Tarmo Annilo, Ph.D., Susan E. Wert, Ph.D., Jeffrey A. Whitsett, M.D., and Michael Dean, Ph.D. abstract background From the Human Genetics Section, Laboratory of Genomic Diversity, National Cancer Institute — Frederick, Frederick, Md. (S.S., T.A., M.D.); the Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore (L.M.N.); and Cincinnati Children’s Hospital Medical Center and the Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati (S.E.W., J.A.W.). Address reprint requests to Dr. Dean at Bldg. 560, Rm. 21-18, NCI — Frederick, Frederick, MD 21702, or at [email protected]. N Engl J Med 2004;350:1296-303. Copyright © 2004 Massachusetts Medical Society. Pulmonary surfactant forms a lipid-rich monolayer that coats the airways of the lung and is essential for proper inflation and function of the lung. Surfactant is produced by alveolar type II cells, stored intracellularly in organelles known as lamellar bodies, and secreted by exocytosis. The gene for ATP-binding cassette transporter A3 (ABCA3) is expressed in alveolar type II cells, and the protein is localized to lamellar bodies, suggesting that it has an important role in surfactant metabolism. methods We sequenced each of the coding exons of the ABCA3 gene in blood DNA from 21 racially and ethnically diverse infants with severe neonatal surfactant deficiency for which the etiologic process was unknown. Lung tissue from four patients was examined by high-resolution light and electron microscopy. results Nonsense and frameshift mutations, as well as mutations in highly conserved residues and in splice sites of the ABCA3 gene were identified in 16 of the 21 patients (76 percent). In five consanguineous families with mutations, each pair of siblings was homozygous for the same mutation and each mutation was found in only one family. Markedly abnormal lamellar bodies were observed by ultrastructural examination of lung tissue from four patients with different ABCA3 mutations, including nonsense, splice-site, and missense mutations. conclusions Mutation of the ABCA3 gene causes fatal surfactant deficiency in newborns. ABCA3 is critical for the proper formation of lamellar bodies and surfactant function and may also be important for lung function in other pulmonary diseases. Since it is closely related to ABCA1 and ABCA4, proteins that transport phospholipids in macrophages and photoreceptor cells, it may have a role in surfactant phospholipid metabolism. 1296 n engl j med 350;13 www.nejm.org march 25, 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. abca3 gene mutations in newborns with fatal surfactant deficiency p ulmonary surfactant is a complex mixture of lipids and proteins that is essential for normal lung function. Surfactant lowers surface tension at the air–liquid interface, thereby preventing end-expiratory atelectasis. It is stored within alveolar type II cells in organelles containing multiple phospholipid layers, known as lamellar bodies, and is secreted into the alveoli by exocytosis. The production of pulmonary surfactant is developmentally regulated, and the respiratory distress syndrome may develop in premature infants owing to the lack of surfactant. Homozygous loss-of-function mutations in the gene encoding the hydrophobic surfactant protein B (SFTPB) results in fatal surfactant deficiency in full-term newborns.1 Fatal respiratory disease has been reported in full-term infants with symptoms of surfactant deficiency in whom a deficiency of surfactant protein B was excluded, and the occurrence of familial cases suggests that there are additional genetic mechanisms.2 The genes for ATP-binding cassette (ABC) transporters encode membrane proteins involved in the transport of compounds across biologic membranes, and 14 ABC genes have been associated with distinct genetic diseases in humans.3 Several ABC transporters are involved in the transport of phospholipids and sterols. The gene encoding ABC transporter 1 (ABCA1) is mutated in Tangier disease, a disorder involving the accumulation of cholesterol in macrophages and peripheral tissues and a deficiency of high-density lipoproteins.4-6 The ABCA4 gene is expressed in photoreceptors and encodes a protein that has been implicated in transporting retinal–phosphatidylethanolamine complexes in the photoreceptor membrane disks of rods.7,8 The ABCA4 gene is mutated in several recessive disorders that involve retinal degeneration, including macular dystrophy due to Stargardt’s disease, most recessive forms of cone–rod dystrophy, and some recessive forms of retinitis pigmentosa.9,10 The ABCG5 and ABCG8 genes are expressed in the liver and intestine and are mutated in patients with sitosterolemia, a disorder involving the accumulation of cholesterol and other sterols.11,12 The ABCA3 gene encodes a 1704-amino-acid protein highly expressed in the lung, which has been localized to the limiting membrane of lamellar bodies,13,14 implicating ABCA3 as possibly important in the maturation of lamellar bodies and surfactant production. Because of the probable role of ABCA3 in lipid transport, its location within n engl j med 350;13 alveolar type II cells, and the association of other ABC genes with human diseases, we conducted a study to determine whether ABCA3 is involved in surfactant phospholipid metabolism and whether ABCA3 is a candidate gene for unexplained surfactant deficiency in full-term infants. methods patients From July 1995 until April 2003, blood samples were collected from 337 infants with severe respiratory disease as part of a study to identify inherited abnormalities of surfactant metabolism. The infants were of northern and southern European, African American, Asian, and Middle Eastern origin. All infants were born after a gestation of at least 36 weeks and had persistent hypoxemic respiratory failure, with no known cause for their respiratory disease identified at the time of enrollment. The onset of respiratory symptoms had occurred within hours after birth, and all infants had clinical or radiographic findings (or both) that were consistent with surfactant deficiency. A cause of the lung disease was subsequently identified in 15 infants: alveolar capillary dysplasia in 4, total anomalous pulmonary venous return in 4, viral pneumonia in 3, acinar dysplasia in 2, pulmonary lymphangiectasia in 1, and mucopolysaccharidosis type II in 1. In 47 infants (14 percent), hereditary deficiency of surfactant protein B was identified as the basis of the lung disease, as determined by the identification of loss-of-function mutations on both alleles of the SFTPB gene. Deficiency of surfactant protein B was ruled out in the remaining 275 infants by a combination of protein analyses of lung fluid and tissue and genetic studies.15,16 Among these infants, 121 were analyzed for mutations in the gene for surfactant protein C (SFTPC); 6 of these infants were found to carry such mutations. Of the remaining 115 infants, a subgroup of 21 infants from 14 families who were likely to have a genetic basis for their lung disease, on the basis of a family history of a similarly affected sibling, consanguinity, or both, or who had fatal disease in association with low surfactant protein levels in tracheal-aspirate fluid, was selected for analysis of the ABCA3 gene. These infants included six pairs of siblings, one of which was known to have abnormal lamellar bodies.17 The majority of these infants died within a month after birth (Table 1). www.nejm.org march 25, 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. 1297 The new england journal of medicine Table 1. Characteristics of Full-Term Infants with Clinical Surfactant Deficiency.* Patient No. Race or Ethnic Group Sex Family No. Family History/ Consanguinity Outcome Histologic Findings ABCA3 Mutation 1 White F 1 Yes/Yes Death within 3 mo after birth DIP, PAP W1142X/W1142X 2 White F 1 Yes/Yes Death during neonatal period DIP, PAP W1142X/W1142X 3 Black M 2 Yes/Yes Death during neonatal period NA L101P/L101P 4 Black M 2 Yes/Yes Death during neonatal period NA L101P/L101P 5 White F 3 Yes/No Death during neonatal period NA 4552insT/L1580P 6 White F 3 Yes/No Death during neonatal period NA 4552insT/L1580P 7 White M 4 Yes/No Death within 3 mo after birth PAP G1221S/L982P 8 White M 4 Yes/No Death during neonatal period PAP G1221S/L982P 9 Middle Eastern M 5 Yes/Yes Death during neonatal period DIP, PAP L1553P/L1553P 10 Middle Eastern M 5 Yes/Yes Death during neonatal period NA L1553P/L1553P 11 White M 6 Yes/No Recovery from RDS NA None found 12 White M 6 Yes/No Recovery from RDS NA None found 13 Middle Eastern M 7 No/Yes Unknown NA 1644delC/1644delC 14 Middle Eastern M 8 Yes/No Death during neonatal period DIP, PAP R106X/R106X 15 Asian F 9† Yes/Yes Death during neonatal period NA 4909+1G>A/4909+1G>A 16 White M 10 Yes/Yes Death during neonatal period NA None found 17 White M 11 No/No Recovery from RDS NA None found 18 White F 12 No/No Death during neonatal period NA None found 19 White M 13 Yes/No Chronic lung disease CPI, DIP Q1591P/—‡ 20 Hispanic M 14 No/No Death after lung transplantation PAP N568D/—‡ 21 Asian F Yes/Yes Death during neonatal period PAP 4909+1G>A/4909+1G>A 9† * DIP denotes desquamative interstitial pneumonitis, PAP pulmonary alveolar proteinosis, NA not available, RDS respiratory distress syndrome, and CPI chronic pneumonitis of infancy. Race or ethnic group was self-assigned by the parents. † Patients 15 and 21 were cousins. ‡ No mutation was identified on one allele. DNA was prepared from whole blood from the infants with the use of a commercially available kit (Gentra Systems). The protocol was approved by the institutional review boards of the participating institutions, and written informed consent was obtained from the parents for genetic studies. detection of mutations both SeqMan software (DNAStar) and Mutation Explorer software (SoftGenetics). Variants were identified by comparing each sequence with the reference ABCA3 sequence.18 Parental DNA was sequenced when samples were available, and nonsynonymous mutations were analyzed in at least 100 racially or ethnically matched subjects (200 chromosomes). None of the nonsynonymous mutations were found in either the public data base of singlenucleotide polymorphisms (http://www.ncbi.nlm. nih.gov/SNP/) or the Celera data base, which is made up of sequences from two European Americans, one African American, one Mexican American, and one Chinese subject. Primers were designed to amplify each of the 30 coding exons of the ABCA3 gene (see Supplementary Appendix 1, available with the full text of this article at www.nejm.org), and the purified polymerase-chain-reaction products spanning the exons and their respective splice junctions were sequenced on both strands with the use of ABI BigDye Terminator sequencing reagents (Applied Biosys- phylogenetic analysis tems) and an ABI 3730 sequencer (Applied Biosys- To analyze the evolutionary (phylogenetic) relation tems). The results were analyzed with the use of between ABCA3 and related proteins from differ- 1298 n engl j med 350;13 www.nejm.org march 25 , 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. abca3 gene mutations in newborns with fatal surfactant deficiency ent organisms, we used the deduced amino acid sequence of ABCA3 (GenBank accession number NP_001080) to search the sequence data base using the BLAST program (http://www.ncbi.nlm.nih. gov/blast/). Similar proteins were also identified in other vertebrate as well as invertebrate species. The amino acid sequences were aligned with the use of the Clustal X program.19 The alignment was used for phylogenetic analyses involving the Mega2 program (http://www.megasoftware.net/).20 This method generates a dendrogram (or tree) indicating the extent to which the sequences are evolutionarily related. To test the reliability of the tree, a bootstrap test with 1000 replications was implemented in the Mega2 program. In this test, the same number of amino acids as in the original data set are randomly sampled from the set of sequences and analyzed. The percentage of the times each branch of the tree has the same topology as the original set of sequences is reported. A bootstrap value of 95 percent or higher provides strong supporting evidence of an evolutionary relation between the particular branch of the tree and the original set of sequences. used to assess the concordance of the six pairs of siblings for ABCA3 haplotypes. One pair of siblings could be excluded from the analysis of recessive mutations in ABCA3, since the siblings were discordant for ABCA3 haplotypes (Fig. 1). The remaining five pairs of siblings were concordant for ABCA3 haplotypes, and the affected infants from consanguineous families were all homozygous for ABCA3 haplotypes. Mutations were identified in the ABCA3 gene in 16 of the 21 infants (76 percent) (Fig. 2 and Table 2). These included homozygous nonsense mutations in codons 106 and 1142, a homozygous frameshift mutation, and heterozygous insertion mutations and splice-site mutations. Seven missense mutations were identified in conserved amino acids (Fig. 2), including homozygous substitutions of proline for leucine in codons 101 and 1553 (L101P and L1553P, respectively) and heterozygous substitutions of aspartic acid for asparagine at position 568 (N568D), proline for leucine at position 982 (L982P), serine for glycine at position 1221 (G1221S), proline for leucine at position 1580 (L1580P), and proline for glutamine at position 1591 (Q1591P). These missense alleles were not ultrastructural analysis found in control subjects. Several polymorphisms Tissue for electron microscopy was fixed in modi- in the introns and exons were also identified (Table fied Karnovsky’s fixative (2 percent paraformalde- 2). The N568 residue is within the N-terminal ATPhyde plus 2 percent glutaraldehyde in 0.1 M sodi- binding domain and is conserved in the mammalium cacodylate buffer), post-fixed with 1 percent osmium tetroxide, stained en bloc with cold 4 perFamily 1 Family 2 Family 3 cent uranyl acetate to preserve the lamellar-body phospholipids, and embedded in EMbed 812 (Electron Microscopy Services) as described previously.21 Plastic sections that were 1 µm thick were 22 22 11 11 12 12 stained with 1 percent toluidine blue (in 1 percent sodium borate in water) and assessed with the use Family 4 Family 5 Family 6 of a wide-field microscope (Nikon FXA-Microphot). Plastic sections that were 0.1 µm thick were cut from the same blocks as the semithin sections, stained 23 23 44 44 14 24 with uranyl acetate and lead citrate, and photographed with a transmission electron microscope Figure 1. Pedigrees of Patients with Surfactant Deficiency. (Jeol 1230, Jeol). Solid symbols indicate patients. The haplotype of ABCA3 polymorphisms is results dna sequencing of abca3 To test the hypothesis that the ABCA3 gene is mutated in some infants with surfactant deficiency, we sequenced each of the coding exons of the gene and the flanking splice sites in samples from 21 infants. Polymorphisms identified in this study were first n engl j med 350;13 shown below each child (triangular symbols) in the pedigree. In Family 6, the two siblings are discordant for ABCA3 haplotypes, ruling out this gene as the cause of the disorder. All other families have at least one mutation identified in the gene. The haplotype is composed of the following polymorphisms: exon 10–20C/T, F353F(1058C/T), exon 14+33G/A and P585P(1755C/G). Haplotype 1 is C-C-A-C for these polymorphisms in the order given. Haplotype 2 is C-C-G-C, haplotype 3 is T-T-G-G, and haplotype 4 is C-C-G-G. Double lines indicate consanguinity. Circles denote female family members, and squares male family members. www.nejm.org march 25, 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. 1299 The of medicine 4909+1G>A A4771C(Q1591P) T4739C(L1580P) T4657C(L1553P) 4552insT G3661A(G1221S) G3426A(W1142X) 1644delC Missense T2945C(L982P) Splice A1702G(N568D) Frameshift C316T(R106X) T301C(L101P) Nonsense new england journal ATP-binding domains Human Mouse Rat Puffer fish Zebra fish L101P N568D ETVRRALVIN NGAGKTT ETVKREFMIK NGAGKTT EAVRREFMIK NGAGKTT EDVRGKLELS NGAGKTT QDVQQNLVRG NGAGKTT L982P QQLSEHL QQLSENL QQLSEHL G1221S LSGIAT LSGIAT LSGIAT L1553P L1580P VARRLL ECEALC VARRLL ECEALC VARRLL ECEALC VARRLL Q1591P LAIMVQGQFKC LAIMVQGQFKC LAIMVQGQFKC LAVMVNGQFKC LAVMVNGQFKC Figure 2. Location of ABCA3 Mutations. Exons encoding the ATP-binding domains are shown in green. The chart below the diagram shows the degree of conservation of residues involved in missense mutations in the ABCA3 protein, predicted on the basis of the sequences in various murine and vertebrate species. The sequences of the puffer fish and the zebra fish are not complete, resulting in some gaps in this information in the case of L982P, G1221S, L1552P, L1553P, and L1580P. The first three noncoding exons are not shown. an and fish ABCA3 genes as well as almost all other members of the ABC type A subfamily (Fig. 2). The corresponding residue is mutated in ABCA1 in patients with Tangier disease and in ABCA4 in patients with Stargardt’s disease. ultrastructural analysis Histologic findings in the nine patients with ABCA3 mutations from whom lung tissue was obtained (Table 1) included hyperplasia of alveolar type II cells, accumulations of alveolar macrophages in distal air spaces with various amounts of proteinaceous material and interstitial thickening, findings consistent with the presence of infantile desquamative interstitial pneumonitis, and neonatal alveolar proteinosis. Plastic sections that were 1 µm thick and stained with toluidine blue were obtained from four patients (Patients 1, 8, 9, and 21), and light-microscopical examination demonstrated alveolar type II cells with homogeneous cytoplasm, without the typical inclusions of lamellar bodies. Electron micrographs of lung tissue from Patient 21 (who was ho- 1300 n engl j med 350;13 mozygous for the 4909+1G>A mutation) revealed lamellar bodies (Fig. 3) that were smaller than those from control lung tissue, with more densely packed membranes and eccentrically placed, dense inclusion bodies, similar to those previously described in Patients 1 and 2, who were homozygous for the W1142X mutation.17 Similarly abnormal lamellar bodies were observed in lung tissue from Patient 8 (who was heterozygous for the G1221S and L982P mutations) and Patient 9 (who was homozygous for the L1553P mutation). evolutionary analysis of abca3 A missense variant may be a benign polymorphism instead of a deleterious mutation. The variant is more likely to be a deleterious mutation if it is absent in controls and if it affects an amino acid residue that is conserved across species. We therefore aligned the human, mouse, and rat amino acid sequences of ABCA3 with partial abca3 sequences of the puffer fish (Takifugu rubripes) and zebra fish (Danio rerio). Nearly all the missense mutations we iden- www.nejm.org march 25 , 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. abca3 gene mutations in newborns with fatal surfactant deficiency tified occur in residues that are highly conserved (Fig. 2). The amino acid alignment was used to produce a phylogenetic tree of the ABCA3-related proteins showing the relation of the proteins from different organisms (see Supplementary Appendix 2, available with the full text of this article at www. nejm.org). The fish ABCA3 proteins cluster with the mammalian ABCA3 proteins and are distinct from other, more distant ABCA-family proteins, such as the mouse Abca14, Abca15, and Abca16 proteins and the sea-urchin ABCA proteins (see Supplementary Appendix 2. These latter genes are all expressed exclusively in testes and are therefore distinct from ABCA3 genes in both structure and expression. discussion We have demonstrated that the ABCA3 gene is frequently mutated in patients with severe neonatal lung disease and symptoms of surfactant deficiency. Our patients were from several major racial or ethnic groups and our findings therefore indicate that such mutations are not confined to a single group. Most of our patients had mutations predicted to inactivate the gene or protein and died shortly after birth. Electron micrographs of patients’ lung tissue demonstrated abnormal lamellar bodies, a finding that is consistent with a role of ABCA3 in the formation of lamellar bodies. All the infants presented with clinical and radiographic findings of surfactant deficiency. Since ABCA3 is related to other transporters of phospholipids and cholesterol, our findings suggest that ABCA3 transports phospholipids that are critical for surfactant function into lamellar bodies. Defective transport of one or more components would be expected to lead to ineffective assembly of the structure and abnormal surfactant. Alternatively, ABCA3 could transport lipids that are deleterious to the function of surfactant out of lamellar bodies. Missense variants in conserved amino acids were identified in some patients. We were unable to find these same variants in the public polymorphism data bases or in 100 racially or ethnically matched controls, but in the absence of a functional test, we cannot rule out the possibility that these are neutral variants. In the case of the L101P and L1553P mutations, each of which affected one pair of siblings from two different families, the two pairs of siblings were both homozygous for the variant and homozygous for all other polymorphisms that we found in the gene — findings that are consistent n engl j med 350;13 Table 2. Mutations and Polymorphisms Identified in the ABCA3 Gene. Site Affected Patient No. Nucleotide Affected* or Outcome SNP No.† Variant Mutation Exon 5 3, 4 T301C L101P‡ Exon 5 14 C316T R106X‡ Exon 14 20 A1702G N568D Exon 14 13 1644delC Frameshift‡ Exon 21 7, 8 T2945C L982P Exon 23 1, 2 G3426A W1142X‡ Exon 24 7, 8 G3661A G1221S Exon 30 9, 10 T4657C L1553P Exon 30 5, 6 4552insT Frameshift Exon 31 15, 21 4909+1G>A Splice site‡ Exon 31 5, 6 T4739C L1580P Exon 31 19 A4772C Q1591P Exon 5 Multiple Exon 5+50A/G Intron Exon 6 20 393C/T A131A Exon 6 18 Exon 6+119G/A Intron Exon 7 19 Exon 7–14C/G Intron Exon 8 14 681C/T A227A Exon 10 Multiple Exon 10–105C/A Intron Exon 10 Multiple Exon 10–20C/T Intron Exon 10 Multiple 1058C/T F353F Exon 14 Multiple Exon 14+33G/A Intron rs170447 Exon 15 Multiple 1755C/G P585P rs323043 Exon 18 13 Exon 18–17G/A Intron Exon 18 1 2340C/T H780H Exon 21 Multiple Exon 21–20C/G Intron rs313908 Exon 21 Multiple Exon 21+34C/T Intron rs313909 Exon 27 Multiple 4116C/T S1372S rs149532 Exon 32 11 4944C/T V1648V Polymorphism rs46725 rs323059 rs323066 * Nucleotides are numbered from the ATG start codon. † Polymorphisms with entries in the public data base of single-nucleotide polymorphisms (SNPs) (http://www.ncbi.nlm.nih.gov/SNP/) are indicated. ‡ This sample was homozygous for the mutation. with the occurrence of a recessive mutation in these consanguineous families. The N568D mutation is in a highly conserved residue in the ATP-binding domain, and it almost certainly disrupts the function of the protein. The clinical phenotype and histopathological findings in patients with missense mutations were similar to those in patients with apparent loss-of-function mutations, supporting the notion that the mutations were deleterious rather than neutral variants. www.nejm.org march 25, 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. 1301 The new england journal A B C Figure 3. Ultrastructure of Alveolar Type II Cells. A representative electron micrograph of normal lung tissue shows normal lamellar bodies (Panel A, ¬15,000). In lung tissue from Patient 21, who was homozygous for an ABCA3 splicing mutation (4909+1G>A), cytoplasmic lamellar bodies are smaller and denser (arrowheads in Panel B, ¬15,000), and many have dense peripheral inclusions (Panel C, ¬80,000). In two patients, a mutation was identified on only one allele. Although the ABCA3 sequence variants in these children may have been unrelated to their lung disease, the similarity of their clinical presentation and the severe nature of their lung disease 1302 n engl j med 350;13 of medicine suggest that these children probably had a second mutation on the other allele, which may have been mutations within introns or regulatory regions or large rearrangements or deletions. These variations would not have been detected by our sequencing strategy. Similar rates of detection of mutations have been reported among patients with mutations in the genes for other ABC transporters such as the cystic fibrosis transmembrane conductance regulator and ABCA4.22,23 These findings indicate that families in which mutations are identified may benefit from genetic counseling and prenatal or preimplantation diagnoses. We found different mutations in the different families, suggesting that there are no common alleles that confer this condition. One patient, who had a missense mutation (Q1591P) on one allele and an unknown mutation on the other allele, is still alive at six years of age and has chronic lung disease, suggesting that some ABCA3 mutations are not fatal. ABCA3 is thus a candidate gene for other pulmonary disorders involving surfactant dysfunction, including the neonatal respiratory distress syndrome and disorders with a later onset, such as asthma and the acute respiratory distress syndrome. There is considerable heterogeneity in the presentation and severity of the respiratory distress syndrome in premature infants, and different ABCA3 variants could influence the severity of that condition. We did not find many nonsynonymous variants in ABCA3 that represent candidate single-nucleotide polymorphisms for the respiratory distress syndrome and other disorders. However, the ABCA3 gene is hormonally regulated,13,14 and genetic variants (in other genes) that indirectly affect its regulation might also be important. ABCA3 mutations were identified in 16 of our 21 patients (76 percent), and 3 of the 5 patients without ABCA3 mutations recovered completely from their initial lung disease and thus did not have the identical phenotype. The high percentage of patients with ABCA3 mutations in the group of 21 infants suggests that ABCA3 deficiency may account for a substantial number of cases of fatal lung disease among full-term infants for which no specific cause can be identified, but further study is needed to address the relative contributions of mutations in SFTPB, SFTPC, and ABCA3 to neonatal lung disease. The absence of mutations in some full-term infants with fatal surfactant deficiency indicates that other, as yet unidentified genes are essential for surfactant production. This possibility is not surpris- www.nejm.org march 25 , 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. abca3 gene mutations in newborns with fatal surfactant deficiency ing, given the complex nature of surfactant and the many different types of proteins in lamellar bodies. We observed distinct ultrastructural changes in lamellar bodies in association with ABCA3 mutations, and abnormal lamellar bodies were also seen in association with a deficiency of surfactant protein B.24 These findings illustrate the potential importance of electron microscopy in the examination of lung tissue from infants who are dying from a lung disease of unclear causation. The ABCA3 gene is highly conserved in both mammals and fish, suggesting that its role in the production of surfactants predates the development of the lung. This possibility is consistent with morphologic studies showing that the surfactants in the swim bladders of teleost (bony) fish contain phospholipids and proteins similar to those found in the mammalian lung.25 Surfactants are also found in the airways of reptiles, salamanders, and lungfish. The conservation of the ABCA3 gene across diverse vertebrate species supports a role of the ABCA3 protein in surfactant lipid metabolism and cellular homeostasis, although the protein may have other functions as well. Supported by grants from the National Institutes of Health (HL54703, to Dr. Nogee, and HL-56387, to Drs. Wert, Nogee, and Whitsett) and from the Eudowood Foundation (to Dr. Nogee). We are indebted to Bernard Gerrard and Georgianne Cirado for technical assistance, to the families who participated in these studies, to the physicians and nurses who cared for the children, and to Henry Shuman for helpful suggestions. references 1. Nogee LM. Surfactant protein-B defi- 10. Cremers FP, van de Pol DJ, van Driel M, ciency. Chest 1997;111:Suppl:129S-135S. 2. Tredano M, Griese M, de Blic J, et al. Analysis of 40 sporadic or familial neonatal and pediatric cases with severe unexplained respiratory distress: relationship to SFTPB. Am J Med Genet 2003;119A:324-39. 3. Dean M, Rzhetsky A, Allikmets R. The human ATP-binding cassette (ABC) transporter superfamily. Genome Res 2001;11: 1156-66. 4. Bodzioch M, Orso E, Klucken J, et al. The gene encoding ATP-binding cassette transporter 1 is mutated in Tangier disease. Nat Genet 1999;22:347-51. 5. Brooks-Wilson A, Marcil M, Clee SM, et al. Mutations in ABC1 in Tangier disease and familial high-density lipoprotein deficiency. Nat Genet 1999;22:336-45. 6. Rust S, Rosier M, Funke H, et al. Tangier disease is caused by mutations in the gene encoding ATP-binding cassette transporter 1. Nat Genet 1999;22:352-5. 7. Mata NL, Tzekov RT, Liu X, Weng J, Birch DG, Travis GH. Delayed dark-adaptation and lipofuscin accumulation in abcr+/mice: implications for involvement of ABCR in age-related macular degeneration. Invest Ophthalmol Vis Sci 2001;42:1685-90. 8. Sun H, Molday RS, Nathans J. Retinal stimulates ATP hydrolysis by purified and reconstituted ABCR, the photoreceptor-specific ATP-binding cassette transporter responsible for Stargardt disease. J Biol Chem 1999;274:8269-81. 9. Allikmets R, Singh N, Sun H, et al. A photoreceptor cell-specific ATP-binding transporter gene (ABCR) is mutated in recessive Stargardt macular dystrophy. Nat Genet 1997;15:236-46. [Erratum, Nat Genet 1997; 17:122.] et al. Autosomal recessive retinitis pigmentosa and cone-rod dystrophy caused by splice site mutations in the Stargardt’s disease gene ABCR. Hum Mol Genet 1998;7:355-62. 11. Berge KE, Tian H, Graf GA, et al. Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science 2000;290:1771-5. 12. Lu K, Lee MH, Hazard S, et al. Two genes that map to the STSL locus cause sitosterolemia: genomic structure and spectrum of mutations involving sterolin-1 and sterolin-2, encoded by ABCG5 and ABCG8, respectively. Am J Hum Genet 2001;69:278-90. 13. Mulugeta S, Gray JM, Notarfrancesco KL, et al. Identification of LBM180, a lamellar body limiting membrane protein of alveolar type II cells, as the ABC transporter protein ABCA3. J Biol Chem 2002;277: 22147-55. 14. Yamano G, Funahashi H, Kawanami O, et al. ABCA3 is a lamellar body membrane protein in human lung alveolar type II cells. FEBS Lett 2001;508:221-5. 15. Nogee LM, Wert SE, Proffit SA, Hull WM, Whitsett JA. Allelic heterogeneity in hereditary surfactant protein B (SP-B) deficiency. Am J Respir Crit Care Med 2000;161: 973-81. 16. Nogee LM, Dunbar AE III, Wert SE, Askin F, Hamvas A, Whitsett JA. A mutation in the surfactant protein C gene associated with familial interstitial lung disease. N Engl J Med 2001;344:573-9. 17. Tryka AF, Wert SE, Mazursky JE, Arrington RW, Nogee LM. Absence of lamellar bodies with accumulation of dense bodies characterizes a novel form of congenital surfactant defect. Pediatr Dev Pathol 2000; 3:335-45. n engl j med 350;13 www.nejm.org 18. Connors TD, Van Raay TJ, Petry LR, Klinger KW, Landes GM, Burn TC. The cloning of a human ABC gene (ABC3) mapping to chromosome 16p13.3. Genomics 1997;39:231-4. 19. Thompson JD, Gibson TJ, Plewniak F, Jeanmougin F, Higgins DG. The CLUSTAL_X windows interface: flexible strategies for multiple sequence alignment aided by quality analysis tools. Nucleic Acids Res 1997; 25:4876-82. 20. Kumar S, Tamura K, Jakobsen IB, Nei M. MEGA2: Molecular Evolutionary Genetics Analysis software. Bioinformatics 2001; 17:1244-5. 21. Na C-L, Beck DC, Breslin JS, Wert SE, Weaver TE. An en bloc staining protocol improves the preservation of lamellar bodies in alveolar type II cells for transgenic mice expressing modified pulmonary surfactant protein B. Microsc Microanal 1998;4:Suppl 2: 852-3. 22. Zielenski J, Tsui LC. Cystic fibrosis: genotypic and phenotypic variations. Annu Rev Genet 1995;29:777-807. 23. Lewis RA, Shroyer NF, Singh N, et al. Genotype/phenotype analysis of a photoreceptor-specific ATP-binding cassette transporter gene, ABCR, in Stargardt disease. Am J Hum Genet 1999;64:422-34. 24. deMello DE, Heyman S, Phelps DS, et al. Ultrastructure of lung in surfactant protein B deficiency. Am J Respir Cell Mol Biol 1994; 11:230-9. 25. Wood PG, Lopatko OV, Orgeig S, Joss JM, Smits AW, Daniels CB. Control of pulmonary surfactant secretion: an evolutionary perspective. Am J Physiol Regul Integr Comp Physiol 2000;278:R611-R619. Copyright © 2004 Massachusetts Medical Society. march 25, 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. 1303 Who Should Receive Myeloablative Therapy for Lymphoma? PERSPECTIVE conventional-dose therapy and can be pushed toward cure by very intensive therapy. The results constitute a modest advance, and it is questionable whether they justify recommending such therapy for all patients with diffuse large-B-cell lymphoma of low-to-intermediate risk. Clearly, at least two thirds of the patients who have been cured in this way would have been cured with CHOP alone and were therefore overtreated, with an approach that must be associated with greater short-term and long-term morbidity and mortality. Such overtreatment cannot be good for the individual patient or for the health care system. Better prognostic indexes are needed — and may soon be at hand, with the aid of molecular technology. As Milpied et al. themselves point out, in determining how to act on their results, we must remember that CHOP is no longer the gold standard for the treatment of the most common of the aggressive lymphomas, diffuse large-B-cell lymphoma. The combination of anti-CD20 (rituximab) and CHOP has been shown to be superior to CHOP alone in both older and younger patients with non-Hodgkin’s lymphoma; chemoimmunotherapy is becom- ing the order of the day. Shortening the interval between cycles of CHOP by a week (from 21 days to 14 days) is also finding favor. What result would have been obtained had Milpied et al. compared CHOP plus rituximab administered every 14 days with myeloablative therapy? Is myeloablative therapy appropriate for the substantial proportion of patients who present in later life with coexisting conditions? The answers to these questions notwithstanding, this critique does not devalue the relevance of the data presented by Milpied et al. These investigators have shown that considerable intensification of treatment is feasible for most patients with aggressive lymphoma of low-to-intermediate risk and that the fraction of patients who are cured may well be increased. It is incumbent on us to build on this information, in the context of the new treatments available today and our new tools for understanding the nature and prognoses of this heterogeneous group of diseases, so that we can continue to make incremental improvements in care. From the Department of Medical Oncology, St. Bartholomew’s Hospital, London. Lung Surfactant, Respiratory Failure, and Genes Mikko Hallman, M.D., Ph.D. After the first observation of surfactant deficiency in infants who were dying of the respiratory distress syndrome (also known as hyaline membrane disease), a series of investigations led to effective therapies, including surfactant therapy given at birth. These therapies, in turn, have led to a dramatic decrease in mortality associated with the respiratory distress syndrome, from nearly 100 percent to less than 10 percent. Most infants who die from the syndrome are preterm. Surfactant therapy is usually not required beyond the first day of life, because the turnover of surfactant is slow in newborns, and the rapid differentiation of alveolar tissue leads to sufficient endogenous secretion within days after birth in most cases. However, there are still some cases of the respiratory distress syndrome that are resistant to treatment, and an understanding of 1278 what causes them may lead to strategies for prevention and new therapies. The synthesis, storage, secretion, recycling, and catabolism of alveolar surfactant take place in alveolar type II cells (see Figure), which are characterized by lamellar bodies — organelles containing concentric, onion-like layers of surfactant. Alveolar macrophages also mediate the catabolism of surfactant. In the alveolar lining, surfactant released by lamellar bodies (when the limiting membrane fuses with the cell membrane) is transformed into aggregates made up of tubular myelin that can both enter the air–water interface exceptionally quickly by means of adsorption and nearly eliminate the surface tension of that interface. Low surface tension in the lining of the tiny spherical air spaces prevents generalized atelectasis (collapse) and its devastat- n engl j med 350;13 www.nejm.org Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. march 25, 2004 Lung Surfactant, Respiratory Failure, and Genes PERSPECTIVE (SP-C). In this issue of the Journal, Shulenin et al. (pages 1296–1303) describe a third genetic cause in 16 cases: recessive mutations in the gene encoding the ATP-binding cassette (ABC) transporter A3 (ABCA3).1 Close examination of alveolar tissue from four patients uncovered small, abnormal lamellar bodies, leading the authors to propose that ABCA3 is critical to the formation of lamellar bodies. Although the molecular action of ABCA3 is un- ing consequences. Ninety percent of the surfactant complex consists of specific lipids enriched with dipalmitoyl phosphatidylcholines that form the film at the air–water interface. Of the four surfactant proteins A, B, C, and D, three (hydrophobic transmembrane surfactant proteins B and C and collectin surfactant protein A) bind to surfactant lipids. Hereditary respiratory failure in term infants has been attributed to mutations in the genes encoding surfactant protein B (SP-B) and surfactant protein C Alveolar space Monolayer–multilayer film Adsorption Surfactant Tubular myelin ABCA3 protein Lipid vesicle Secretion Air Turnover Lamellar body Liquid Recycling Golgi complex Multivesicular bodies Clearance Alveolar macrophage Alveolar type II cell Alveolar type I cell Figure. Lung Surfactant and the Lamellar Body. The composition of lung surfactant is critical to lung function, and the subcellular lamellar body of the type II alveolar cell has a major role in maintaining the composition of surfactant. The distribution of ATP-binding cassette (ABC) transporter A3 (ABCA3) is shown in red. It is possible that ABCA3 targets surfactant-containing vesicles to the lamellar bodies. The lamellar body is formed through the fusion of several multivesicular bodies, and its lipid bilayers are converted to tubular myelin as they are turned out into the alveolar space. Surfactant protein A, secreted primarily by a constitutive pathway that does not involve the lamellar body, is required for the formation of tubular myelin. Surfactant aggregate, such as tubular myelin, is the precursor of surfactant at the air–water interface (inset). Cationic transmembrane proteins (surfactant protein B or surfactant protein C or both [not depicted in the monolayer–multilayer film]) together with anionic phospholipids (phosphatidylglycerol or phosphatidylinositol or both [green]) facilitate the entry of dipalmitoyl phosphatidylcholines (blue) into the monolayer at the interface, maintaining a low surface tension. During tidal breathing, tubular myelin surfactant is converted to smaller aggregates that are taken up by type II cells and alveolar macrophages. Arrows depict the direction of surfactant flux. n engl j med 350;13 www.nejm.org march 25, 2004 Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. 1279 Lung Surfactant, Respiratory Failure, and Genes PERSPECTIVE clear, we know about the biologic behavior of other ABCA proteins, which may be relevant to that of ABCA3. The ABCA subfamily consists of 12 transporter genes, some of which are known to mediate ATP-driven lipid transport across a lipid-bilayer membrane. Tangier disease, a multiorgan hyperlipidemia syndrome, is caused by a loss-of-function mutation in the ABCA1 gene; ABCA1 controls the extrusion of the membrane lipid toward extracellular acceptors, the apolipoproteins. Stargardt’s disease, which affects the retina, is caused by loss-offunction mutations in the ABCA4 gene. This protein serves as a “flippase”; it catalyzes a 180° rotation of a specific phospholipid derivative and simultaneously moves it from the inner leaflet of the lipid bilayer to the outer leaflet within the disk membrane of the rod cell. ABCA3 is found in the outer limiting membrane of lamellar bodies, multivesicular bodies, and segments of luminal plasma membrane of alveolar type II cells. This pattern of expression, together with the known functions of ABCA1 and ABCA4, is consistent with the possibility that ABCA3 mediates the targeting of surfactant-containing vesicles to the lamellar bodies. The phenotype of the patients characterized by Shulenin et al. resembles that of patients with mutations of the SP-B gene: both groups of patients have fatal respiratory failure and highly abnormal lamellar bodies, and in both, histologic analysis reveals neonatal alveolar proteinosis.2 In contrast, the phenotypes of patients with a mutation of the SP-C gene are varied: some have mild respiratory symptoms, whereas others have severe respiratory failure. Histologic analysis reveals interstitial lung disease.2 In fatal respiratory failure due to the absence of surfactant protein B, surfactant protein C precursor protein is not cleaved to form mature surfactant protein C, so the precursor protein accumulates in the alveolar space. A dominant negative mutation of 1280 SP-C, on the other hand, may result in the aggregation of misfolded surfactant protein C precursor protein and subsequent injury and inflammation. The lungs of the patients studied by Shulenin et al. showed hyperplasia of alveolar macrophages and alveolar type II cells, as well as indications of desquamative interstitial pneumonitis or alveolar proteinosis. The abnormally small, densely packed lamellar bodies suggest the presence of abnormal surfactant that probably does not have the near-zero surface tension required for alveolar stability. Further study to determine the distribution of surfactant and other membrane components in bronchoalveolar lavage fluid and in lung compartments — together with experimental studies using mouse models — will contribute to a more accurate picture of ABCA3 deficiency. Although heritable cases of the respiratory distress syndrome can be prevented through genetic counseling and prenatal diagnosis, we may not be aware of all the genes that can fatally affect the surfactant system. Nor do we yet know the proportion of cases of the respiratory distress syndrome that are caused by a mutation of ABCA3, which may be similar to the proportion caused by a mutation of the SP-B gene (in the range of 1 case in 1 million newborns). It is also possible that the common allelic variants of the genes encoding the surfactant proteins, together with environmental factors, influence susceptibility to serious respiratory disease.3 From the Biocenter Oulu and the Department of Pediatrics, University of Oulu — both in Oulu, Finland. 1. Shulenin S, Nogee LM, Annilo T, Wert SE, Whitsett JA, Dean M. ABCA3 gene mutations in newborns with fatal surfactant deficiency. N Engl J Med 2004;350:1296-303. 2. Whitsett JA, Weaver TE. Hydrophobic surfactant proteins in lung function and disease. N Engl J Med 2002;347:2141-8. 3. Haataja R, Hallman M. Surfactant proteins as genetic determinants of multifactorial pulmonary diseases. Ann Med 2002;34: 324-33. n engl j med 350;13 www.nejm.org Downloaded from www.nejm.org at UNIV OF PENN LIBRARY on August 26, 2004. Copyright © 2004 Massachusetts Medical Society. All rights reserved. march 25, 2004