* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pharm Chapter 10 [4-20
5-HT3 antagonist wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
NMDA receptor wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Toxicodynamics wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Norepinephrine wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
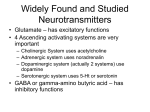
Pharm Chapter 10: Adrenergic Pharm Adrenergic pharm focuses on pathways mediated by the catecholamines norepinephrine, epinephrine, and dopamine The sympathetic nervous system is the major source of catecholamines, and catecholamines are the major effectors of symps Effects of catecholamines: - Increasing heart rate and force of contraction Regulating peripheral resistance of arteries Inhibiting insulin release Stimulating liver release of glucose Increasing adipocyte release of fatty acids Catecholamine synthesis, storage, and release: - - - - Catecholamines are made from tyrosine at the symp nerve endings or in chromaffin cells of the adrenal medulla Symps make norepinephrine as their main neurotransmitter Tyrosine is moved into neurons by an amino acid transporter that uses the sodium gradient across the neuron membrane o The transporter also moves phenylalanine, tryptophan, and histidine The first step of making a catecholamine is tyrosine hydroxylase converting tyrosine into dihydroxyphenylalanine (DOPA) o Tyrosine hydroxylase is the rate limiting step in making catecholamines A decarboxylase then converts DOPA into dopamine Dopamine-β-hydroxylase converts dopamine into norepinephrine In tissues that make epinephrine, phenylethanolamine N-methyltransferase (PNMT) adds a methyl to norepinephrine to make epinephrine o Expression of PNMT in the adrenal medulla depends on high concentrations of cortisol, that move into the medulla through veins draining the adrenal cortex Tyrosinedopamine happens in the cytoplasm, and then dopamine is taken to synaptic vesicles by vesicular monamine transporter (VMAT) o Once in the vesicles, dopaminenorepinephrine by dopamine-β-hydroxylase o VMAT 1 and 2 both carry serotonin (5-HT), histamine, and catecholamines o VMAT1 is expressed peripherally in the adrenals and symps o VMAT2 is expressed in the CNS o The vesicular acetylcholine transporter (VAChT) is expressed in cholinergic neurons like motor nerves o All 3 of these use the proton gradient from an H+ATPase in the vesicle membrane to concentrate dopamine inside the vesicle - Norepinephrine made then couples with ATP to stabilize the osmotic pressure from the concentration gradient made o In the adrenal medulla, norepinephrine is moved out of vesicles into the cytoplasm, where PNMT converts it to epinephrine, which then goes back into the vesicle Activation of symps and therefore catecholamines is started by processing area of the CNS, especially the limbic system o These CNS neurons project axons that synapse on symp pregang neurons int eh intermediolateral columns of the spinal cord o The pregang axons then project to symp ganglia The pregangs use ACh to activate nicotinic receptors, leading to depolarization and postsynaptic potential in postgang neurons o Ganglionic blockers like hexamethonium and mecamylamine block the ganglionic nicotinic ACh receptor, without effecting skeletal muscle o The symp postgangs then synapse with target organs o When an action potential gets to postgang symp nerve endings, it opens calcium channels to cause calcium influx, which leads to exocytosis of vesicles that contain catecholamine o Ziconitide is a pain drug that blocks this release o Norepinephrine then diffuses away from the nerve endings and acts on adrenergic receptors The nerve endings also have adrenergic receptors, which can regulate neurotransmitter release Reuptake and metabolism of catecholamines: - - - Once a catecholamine exerts its effect at a postsynaptic receptor, the response is terminated by one of three things: o Reuptake of catecholamine into the presynaptic neuron o Metabolism of catecholamine into an inactive metabolite o Diffusion of catecholamine away from the synaptic cleft o The first two use enzymes, so they can be targeted with drugs Reuptake of catecholamine into the neuron is done by norepinephrine transporter (NET) o Most of the released norepinephrine gets recycled like this o NET uses a sodium gradient to concentrate catecholamines in the cytoplasm of the symp nerve endings Inside the nerve ending, catecholamines are further concentrated into synaptic vesicles by VMAT So the pool of catecholamines available for release comes from molecules made in the vesicle, and recycled molecules MAO-A degrades serotonin, norepinephrine, and dopamine MAO-B degrades dopamine quicker than norepinephrine and serotonin MAO inhibitors are used for depression Catecholamine receptors - - Adrenergic receptors (aka adrenoreceptors) are selective for norepinephrine and epinephrine o 3 main classes: α1 , α2 , and β Each has 3 subtypes So α1A, α1B, α1C ; α2A, α2B, α2C; β1, β2, β3 Each subtype is part of a G protein superfamily α1 and α2 adrenergic receptors o α1 adrenergic receptors usually work by a G protein pathway activating phospholipase C, which cleaves phosphatidylinositol-4,5-bisphosphate into inositol triphosphate (IP3) and diacylglycerol (DAG) IP3 mobilizes intracellular calcium DAG activates protein kinase C This leads to activation of things downstream, like calcium and potassium channels, MAP kinases, and other kinases like phosphatidylinositol 3-kinase α1 adrenergic receptors are expressed in vascular smooth muscle, GU smooth muscle, heart, liver, etc. in vascular smooth muscle, stimulation of α1 adrenergic receptors increases intracellular calcium, via release of endogenous calcium stores, and by influx of calcium from ECF leads to activation of calmodulin, which activates myosin light chain kinase to phosphorylate the myosin light chain, causing myosin to bind to actin, causing muscle contraction So α1 adrenergic receptors are important regulating increases in peripheral vascular resistance, which can increase blood pressure and redistribute blood flow α1 adrenergic antagonists help treat benign prostatic hyperplasia o α2 adrenergic receptors activate GI, an inhibitory G protein that inhibits adenylyl cyclase, which decreases cAMP can also activate potassium channels to hyperpolarize the cell, and can also inhibit calcium channels so α2 adrenergic receptors inhibit neurotransmitter release from the target neuron α2 adrenergic receptors are found on both presynaptic neurons, and postsynaptic cells the presynaptic α2 adrenergic receptors, are autoreceptors to mediate feedback inhibition of symp transmission α2 adrenergic receptors are also found on platelets and pancreas β cells they mediate platelet aggregation and inhibit insulin release α2 adrenergic agonists therefore decrease symp activity, and are used in hypertension o o works at CNS sites to decrease symp outflow to the periphery, resulting in decreased norepinephrine release at symp nerve terminals, causing decreased vascular smooth muscle contraction β adrenergic receptors activate adenylyl cyclase to increase cAMP, which activates protein kinases like protein kinase A, which phosphorylate cellular proteins, including ion channels β1 adrenergic receptors – found mainly in the heart and kidney in the kidney, they’re found on juxtaglomerular cells, where activation causes renin release Heart β1 adrenergic receptors cause an increase in force of contraction and heart rate Force of contraction is regulated by increased phosphorylation of calcium channels, including in the sarcolemma and phoshpolamban in the SR Heart rate is controlled by β1 adrenergic receptor controlled SA node Both increase cardiac output (HR x SV) Activation of β1 adrenergic receptors also increase conduction velocity in the AV node since it causes calcium entry to increase depolarization β2 adrenergic receptors – found in smooth muscle, liver, and skeletal muscle β2 adrenergic receptor activation stimulates adenylyl cyclase, increasing cAMP, and activating protein kinase A Protein kinase A can phosphorylate myosin light chain kinase, reducing it’s affinity for calcium-calmodulin, causing relaxation of muscle β2 adrenergic receptors can also relax bronchial smooth muscle by activating potassium channels, causing hyperpolarization In the liver, activation of a β2 adrenergic receptors cause phosphorylation that leads to activating glycogen phosphorylase, causing glycogenolysis (glycogen breakdown) In skeletal muscle, both glycogenolysis and potassium hyperpolarization are triggered Activating β2 adrenergic receptors in adipose increases lipolysis So α1 and β1 cause symp actions on cardio, and α2 and β2 cause parasymp actions on cardio The ability of the agonists to cause signaling depends on the # of receptors activated - So changes in the # of receptors on the cell surface will affect how effective an agonist is o Includes both short term (desensitization) and long term (down regulation) When an agonist activates an adrenergic receptor, the dissociation of G proteins leads to downstream signaling, and negative feedback to limit tissue responses Accumulation of βγ subunits in the membrane recruits a G protein receptor kinase, which phosphorylates the receptor at inhibitory residues to inhibit it Protein kinase A and protein kinase C can phosphorylate G proteins - Phosphorylated G proteins can bind to a protein called β-arrestin, which inhibits receptor-G protein interaction, inhibiting receptor signaling Down regulation – when the receptor-β-arrestin complex is put into endosomes to be internalized o Uses clathrin coated pits Effects of catecholamines: - - - Epinephrine and norepinephrine act as agonists of α and β adrenergic receptors Epinephrine o At low concentrations, epinephrine has mostly β1 and β2 effects At the β1 receptors – epinephrine increases cardiac output and contractility, increasing systolic blood pressure At the β2 receptors, epinephrine causes vasodilation to decrease diastolic blood pressure by decreasing peripheral resistance Stimulating a β2 also increased blood flow to muscle, relaxes lung smooth muscle, and increases the concentrations of glucose nd free fatty acids in the blood o At higher concentrations, epinephrine has more α effects o Epinephrine is used to treat anaphylaxis o Locally injected epinephrine causes vasoconstriction and prolongs the action of local anesthetics o Epinephrine is ineffective orally due to a big first pass effect o Epinephrine works quickly and has a short lasting effect when given IV Adverse effects to the IV form are arrhythmia and increased blood pressure Norepinephrine o Norepinephrine is an agonist at α1 and β1 receptors (so only symp cardio effects) o So norepinephrine increases both systolic and diastolic blood pressures, and total peripheral resistance o Norepinephrine is used to treat hypotension, usually in shock Dopamine o Exogenously given dopamine has very little effect cause it can’t cross the blood-brain barrier o Dopamine is given by IV o At low doses, dopamine works on mainly D1 dopaminergic receptors of the kidneys, stomach, and heart D1 dopaminergic receptors activate adenylyl cyclase in vascular smooth muscle, which increases cAMP and vasodilation o o o At higher doses, it activates β1 receptors At even higher doses, dopamine acts on α1 adrenergic receptors to cause vasoconstriction Dopamine is used for shock, especially when the kidneys fail Inhibitors of catecholamine making: - Not used often cause they aren’t specific and inhibit all catecholamines α methyltyrosine- structural analogue of tyrosine that is taken into nerve terminals, where it inhibits tyrosine hydroxylase, the first enzyme in the making of catecholamines o Used sometimes to treat hypertension from a pheochromocytoma (tumor of the chromaffin cells of the adrenal medulla) o It’s use is limited because it causes orthostatic hypotension and sedation Inhibitors of catecholamine storage: - - - Catecholamines that work on a receptor come from either being made or being recycled Something that inhibits catecholamine storage can have two effects: o Short term – it increases the release of catecholamines from the synaptic terminal This mimics symp stimulation, so it’s called sympathomimetic o Long term – it inhibits symp activity, called a sympatholytic Reserpine- binds to VMAT and irreversibly inhibits it o So the vesicles then can’t store norepinephrine and dopamine o At low doses, reserpine causes neurotransmitter leak into the cytoplasm, where the catecholamine gets destroyed by MAO o At high doses, the rate of catecholamine leak can be high enough to overwhelm the MAO in the presynaptic neuron When this happens, there’s lots of catecholamine in the cytoplasm, that can be put into the synaptic space by reverse NET, causing a sympathomimetic effect o Reserpine’s inhibition of VMAT is irreversible, new vesicles have to be made to store catecholamines This can take days to weeks o Reserpine can cause severe depression o Reserpine can be used for hypertension, but it’s side effects make it poor choice over other less riskier treatment Tyramine- normal dietary amine usually metabolized by MAO in the GI and liver o When taking an MAO inhibitor, tyramine is taken up by symp neurons and transported by VMAT to vesicles, where it can displace norepinephrine and cause big release of norepinephrine through reversal of NET o Fermented foods like red wine and cheese have lots of tyramine in them o Tyramine itself is poorly held in synaptic vesicles Its metabolite octopamine can be stored at high concentrations in the vesicles Made by vesicular dopamine-β-hydroxylase o - - - - When taking MAO inhibitors and decreasing tyramine intake, norepinephrine can be replaced in the vesicles by octopamine o Octoopamine has little agonist activity at adrenergic receptors, so you have decreased symp effects So MAO inhibitors can cause hypotension by kicking out catecholamines and taking their place instead in the vesicles Guanethidine- works just like tyramine, and is actively transported into vesicles by NET, displacing norepinephrine, and decreasing symp effect o Like octopamine, guanethidine isn’t an agonist at adrenergic receptors o Used to treat hypertension Both MAO inhibotors and guanethidine can cause hypotension after exercise or when standing up (postural hypotension) Guanadrel – another false neurotransmitter similar to guanetidine o Used to treat hypertension Ampthetamine o Jobs: Displaces catecholamines from vesicles It’s a weak inhibitor of MAO Blocks catecholamine reuptake mediated by NET o So amphetamine basically is a thing to kick out catecholamines to cause temporary symp effects, followed by a crash when the catecholomines go away o Although amphetamine binds to postsynaptic adrenergic receptors, it has little agonist action at adrenergic receptors o Amphetamine causes increased alertness, decreased fatigue, depressed appetite, and insomnia o Amphetamine is used to treat depression, narcolepsy (attacks of drowsiness and sleep during the daytime), and to suppress appetite o Has substantial side effects, like fatigue and depression following the stimulation it caused Ephedrine, pseudoephedrine, and phenylpropanolamine o Have some ability to activate adrenergic responses o Phenylpropanolamine was removed from over the counter markets int eh US due to concerns of cerebral hemorrhage o Ephedrine is used to treat hypotension o An herbal source of ephedrine is ma huang, which the Chinese use to treat asthma o Pseudoephedrine is used as an over the counter decongestant in cold remedies Methylphenidate- structural analogue of amphetamine used to treat ADHD o It enhances attention Amphetamine can cause psychological and physiologic dependence, and tolerance o Amphetamine can cause paranoia and hallucinations o Methamphetamine is a drug that’s often abused Inhibitors of catecholamine reuptake - - These have an acute and powerful sympathomimetic effect by prolonging how long the released catecholamine stays in the synaptic cleft Cocaine- strong inhibitor of NET that eliminates catecholamine transport o It’s used sometimes as a local anesthetic because it can inhibit action potentials o Often abused Tricyclic antidepressants- inhibit NET mediated reuptake of norepinephrine into presynaptic terminal, allowing norepinephrine to stay in the synaptic cleft Inihbitors of catecholamine metabolism: - Monoamine oxidase inhibitors (MAOI’s) – prevent secondary deamination of catecholamines at presynaptic terminals or the liver o In the absence of metabolism, more catecholamine accumulates in presynaptic vesicles for release during each action potential o Most MAOIs are oxidized by MAO to intermediates that irreversibly inhibit MAO o Nonselective agents inhibit both MAO-A and MAO-B Includes phenelzine, tranylcypromine, and iproniazid o Clorgyline is selective for MAO-A o Selegiline is selective for MAO-B o Brofaromine, befloxatone, and moclobemide, are reversible inibitors of MAO-A o MAOIs are used to treat depression o Selegiline is also used to treat Parkinson’s o Patients taking MAOIs need to avoid eating fermented foods with tyramine and other monamines, because MAOIs block any inhibiting of monoamines in the GI and liver, allowing them to enter the circulation and cause hypertensive crisis o Don’t mix MAOIs and SSRIs, because it could cause serotonin syndrome Shows restlessness, tremors, seizures, coma, or death o The reversible MAOIs have less adverse effects Adrenergic receptor agonists - These are used to regulate vascular tone, smooth muscle tone, and contractily - So they’re used for hypertension, asthma, and heart conditions α adrenergic agonists o α1 adrenergic agonists- increase peripheral resistance to increase blood pressure can cause bradycardia through activating a reflex vagal response through baroreceptors systemically given α1 adrenergic agonists, like methoxamine, don’t have much clinical use, but are sometimes used for shock - topical α1 adrenergic agonists, like phenylephrine, oxymetazoline, and tetrahydrozoline, are used in nonprescription Afrin and Visine, cause vasoconstriction for nasal congestion and hyperemia, to relieve symptoms Extended use of these can cause damage to the nasal mucosa and hypersensitivity, along with return of symptoms Phenylephrine is used IV to treat shock o α2 adrenergic agonists Clonidine is an α2 adrenergic agonist that lowers blood pressure by acting in brainstem vasomotor centers to suppress symp flow to the periphery Clonidine may decrease heart problems in hypertension, and has a little ability to help with symptoms from alcohol or opiate withdrawal Adverse effects of clonidine are postural hypotension, bradycardia, dry mouth, and sedation, from increase vagus and decreased symps Guanabenz and guanfacine are also α2 adrenergic agonists that similar adverse effects to clonidine Dexmedetomidine- α2 adrenergic agonist that is used to cause sedation in surgery, since it has no respiratory effects Helps to avoid swings in blood pressure during surgery α methyldopa- prodrug precursor of the α2 adrenergic agonist αmethylnorepinephrine Used in hypertension to decrease symp flow from the CNS Rarely used cause it can cause liver toxicity, hemolytic anemia, and CNS problems o Exception is hypertension in pregnancy, where it is the drug of choice β adrenergic agonists o β1 adrenergic agonists - Stimulating a β1 adrenergic agonist increases heart rate and force of contraction to increase cardiac output o β2 adrenergic agonists - stimulating a β2 adrenergic agonist causes relaxation of vascular, bronchial, and GI smooth muscle β2 adrenergic agonists are used to treat asthma They’re good choices because they have less effects at non-target tissues, like the heart Specificity for the lungs only, is further enhanced by delivering the drug through aerosols inhaled directly into the lungs They relax bronchial smooth muscle and decrease airway resistance Adverse effects come from not being completely selective, and therefore skeletal muscle tremor from muscle β2’s, and tachycardia from β1’s o Nonselective β adrenergic agonists Isoproterenol- lowers peripheral resistance and diastolic pressure, while increasing or leaving unchanged the systolic pressure It increases cardiac output by increasing HR and contractility Used to relieve bronchoconstriction in asthma o Use for asthma can cause adverse heart effects, so more selective β2 adrenergic agonists are usually used Isoproterenol can sometimes be used to stimulate heart rate in emergencies with lots of bradycardia, especially when putting in a pacemaker Dobutamine- a β1 agonist Dobutamine increase contractility and cardiac output Dobutamine can be used IV in severe heart failure It’s also used with heart imaging to diagnose ischemic hearts Receptor antagonists: - α-adrenergic antagonists - They cause vasodilation, decreased blood pressure, and decreased peripheral resistance o Block binding to α1 and α2 o The baroreceptor reflex usually attempts to compensate for the fall in blood pressure, causing a reflex increase in heart rate and cardiac output (reflex tachycardia) o Phenoxybenzamine- irreversibly blocks α1 and α2 receptors, and inhibits catecholamine uptake into adrenergic nerves and the tissue Used to treat hypertension and benign prostatic hyperplasia Because it has so many effects on the symps, it’s rarely used clinically Can be used before surgery on a pheochromocytoma to decrease risk for problems during the surgery o Phentolamine- reversible, nonselective α-adrenergic antagonist Used for hypertension and before surgery on a pheochromocytoma o Prazosin- has a much higher affinity for α1 receptors than α2 It’s selective block of α1 causes decreased peripheral resistance, and dilation of veins (called capacitance) Capacitance decreases venous return, and therefore cardiac output Prazosin is an antihypertensive drug A lot of times the first dose of prazosin can cause postural hypotension and syncope, so you start by giving them a low dose o Terazosin and doxazosin work similar to prazosin, but have longer half lives o α1-adrenergic antagonists aren’t often used for hypertension, cause other meds work better o Some α1-adrenergic antagonists are used to treat the symptoms of benign prostatic hyperplasia They are more effective and work faster than other drugs - The main receptor of GU is α1A Tamsulosin- selective antagonist for α1A May have less risk for orthostatic hypotension o Drugs like yohimbine are selective antagonists for α2 receptors, and cause release of norepinephrine, which then stimulates heart β1 receptors and peripheral α1 receptors They also cause insulin resistance by blocking α2 receptors in the pancreatic islets, suppressing insulin secretion Yohimbine has been used to treat erectile dysfunction β-adrenergic antagonists - block catecholamines at β1 receptors, to decrease heart rate and contractility o β-adrenergic antagonists decrease blood pressure in hypertensive patients, but don’t have an effect on people with normal blood pressure o Long term use decreases peripheral resistance o So β-adrenergic antagonists are used to treat hypertension o Nonspecific β-adrenergic antagonists also affect β2’s in the lungs, which can cause life threatening bronchoconstriction in people with asthma o β-adrenergic receptor therapy can be divided into: Nonselective β-adrenergic antagonists Nonselective β and α1 adrenergic antagonists β-adrenergic partial agonists β1-adrenergic antagonists page 141 o Propranolol, nadolol, and timolol are nonselective, and are used to treat hypertension and angina Although nonselective β blockers are usually contraindicated in people with asthma, these ones are good for COPD Nadalol can be used to prevent bleeding from esophageal varices in cirrhosis Good cause it has a long half life, and is excreted by the kidneys o Timolol is a nonselective β blocker used for glaucoma, and can cause adverse effects o Levobunolol and carteolol are nonselective β blockers used in eye drops for glaucoma o Labetalol and carvedilol block α1, and β1 and β2 blockers Labetalol has 4 stereoisomers that make it hard to predict its effect on the patient The α1 part lowers peripheral resistance, and the β block decreases blood pressure So it’s used for hypertension IV Labetalol can cause hepatitis Carvedilol is used for hypertension and systolic heart failure o Pindolol- partial agonist of β1 and β2 Used for hypertension o o o o Since it’s only a partial agonist of β1, it has less of a decrease in heart rate and blood pressure than pure β antagonists Acebutolol- partial agonist of β1 Used for hypertension Esmolol, metoprolol, atenolol, and betaxolol – β1 selective adrenergic antagonists Esmolol has a very short half life of minutes Metoprolol and atenolol have intermediate half lives of hours Becauase of its shorter half life, esmolol may be safer in unstable patients Esmolol gets rapidly metabolized by esterases Metoprolol may increase life expectancy in people with mild heart failure, or who have survived an MI Nebivolol- selective β1 adrenergic antagonist that causes vasodilation with NO Adverse effects of β-adrenergic antagonists are related to their jobs they do Includes worsened bronchoconstriction in asthma, decreased cardiac output in decompensated heart failure, difficulty recovering from hypoglycemia of diabetes Receptors - Alpha 1 – vasoconstriction from phospholipase C Alpha 2 – vasodilation from inhibiting adenylyl cyclase Beta 1 – symps at heart and kidney from activating adenylyl cyclase Beta 2 – muscle relaxation (including vessels and lungs) from protein kinase A inhibiting myosin light chain, and increase gluconeogenesis