* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download a role for mitochondrial enzymes in inherited neoplasia and beyond
Therapeutic gene modulation wikipedia , lookup
Tay–Sachs disease wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Public health genomics wikipedia , lookup
Population genetics wikipedia , lookup
Cancer epigenetics wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Polycomb Group Proteins and Cancer wikipedia , lookup
Genome evolution wikipedia , lookup
BRCA mutation wikipedia , lookup
Koinophilia wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Genome (book) wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Mitochondrial DNA wikipedia , lookup
Microevolution wikipedia , lookup
Designer baby wikipedia , lookup
Frameshift mutation wikipedia , lookup
Human mitochondrial genetics wikipedia , lookup
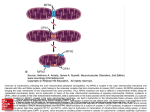
REVIEWS A ROLE FOR MITOCHONDRIAL ENZYMES IN INHERITED NEOPLASIA AND BEYOND Charis Eng*‡, Maija Kiuru§, Magali J. Fernandez* and Lauri A. Aaltonen§ Mitochondrial defects have been associated with neurological disorders, as well as cancers. Two ubiquitously expressed mitochondrial enzymes — succinate dehydrogenase (SDH) and fumarate hydratase (FH, fumarase) — catalyse sequential steps in the Krebs tricarboxylic-acid cycle. Inherited heterozygous mutations in the genes encoding these enzymes cause predispositions to two types of inherited neoplasia syndromes that do not share any component tumours. Homozygous mutations in the same genes result in severe neurological impairment. Understanding this link between inherited cancer syndromes and neurological disease could provide further insights into the mechanisms by which mitochondrial deficiencies lead to tumour development. *Clinical Cancer Genetics Program, Human Cancer Genetics Program, Comprehensive Cancer Center, and Division of Human Genetics, Department of Internal Medicine, The Ohio State University, 420 W. 12th Avenue, Ste 690 TMRF, Columbus, Ohio 43210, USA. ‡ Cancer Research UK Human Cancer Genetics Research Group, University of Cambridge, Cambridge CB2 2XZ, UK. § Department of Medical Genetics, Biomedicum Helsinki, P.O.Box 63 (Haartmaninkatu 8), Helsinki FIN-00014, Finland. Correspondence to C. E. e-mail: eng-1@ medctr.osu.edu doi:10.1038/nrc1013 NATURE REVIEWS | C ANCER Mitochondria have traditionally been viewed as the powerhouse organelles in eukaryotic cells, charged with the role of energy production. Much of its machinery — the enzymes that catalyse energy production — have been studied in this role. In general, therefore, inherited mitochondrial defects, whether nuclear- or mitochondrial-encoded, result in severe clinical sequelae that affect the entire organism, or at least affect the main organs, such as the central nervous system and the heart, which have the highest energy consumption. The central nervous system is the most commonly affected, and patients experience seizures, fluctuating encephalopathy, stroke-like episodes, migraines, dementia and ataxia. Nonetheless, the spectrum of the clinical manifestations is heterogeneous. Some patients develop symptoms that are characteristic of a specific syndrome, whereas others cannot be clearly categorized. Mitochondrial enzymes were not directly implicated in hereditary neoplasias until recently. Germline heterozygous mutations in the autosomally encoded mitochondrial enzyme subunits SDHD, SDHC and SDHB cause the inherited syndromes phaeochromocytoma and paraganglioma. Mutations in FH, which encodes fumarase, cause a predisposition to cutaneous and uterine leiomyomas, as well as to kidney cancers. Together, the four subunits of succinate dehydrogenase (SDH) — SDHA, SDHB, SDHC and SDHD — comprise mitochondrial complex II (also known as succinate:ubiquinone oxydoreductase), which is involved in electron transport and the Krebs tricarboxylic-acid cycle (BOX 1). Complex II catalyses the energy-dependent conversion of succinate to fumarate. Fumarate is converted to malate by fumarase as the next step (BOX 1). Homozygous mutations in SDHA and FH result in severe neurological dysfunction. This is often explained by the fact that the developing nervous system is very sensitive to any perturbation in metabolism or homeostasis (BOX 1). There are fundamental differences between the neoplasia and neurological disorders, however. In individuals with the neurodegenerative disorders, there is virtually complete loss of SDHA or FH activity, and its consequences are experienced throughout development. The inherited neoplastic syndromes are associated with reductions in SDH or FH gene dosage, and complete or nearcomplete loss of enzyme function occurs only in the somatic cells that comprise the tumour. The mitochondrial effects of reduced SDHA or FH activity might affect apoptosis and angiogenesis induction, which are both hallmarks of tumorigenesis. VOLUME 3 | MARCH 2003 | 1 9 3 REVIEWS Summary • Germline heterozygous mutations in the autosomally encoded mitochondrial enzyme subunits of succinate dehydrogenase (SDH), SDHB, SDHC and SDHD, are associated with hereditary predisposition to phaeochromocytoma and paraganglioma. By contrast, homozygous germline mutations in the catalytic active-site-bearing subunit SDHA causes Leigh syndrome, which is characterized by severe neurological dysfunction and seizures. • Germline heterozygous mutations in another autosomally encoded mitochondrial enzyme — fumarate hydratase (fumarase, FH) — are associated with hereditary predisposition to papillary renal-cell carcinoma and leiomyomatosis, whereas homozygous FH mutations cause neurodegeneration. • SDH and FH catalyse sequential steps in the Krebs tricarboxylic-acid cycle, which generates ATP — the cell’s currency of energy. SDH is a component of complex II of the respiratory electron-transport chain. • The hereditary neurological diseases might be explained by complete or near-complete lack of energy generation during development, leading to free-radical formation and mitochondrial-mediated apoptotic cell death. • Little data exist to explain the mechanism of predisposition to cancer. Hypotheses invoke free-radical formation, leading to activation of the HIF/angiogenesis pathway and mitochondrial-mediated anti-apoptotic activity. • The link between mitochondrial-associated inherited neurological disease and inherited cancer might be exploited for uncovering novel functions and mechanisms for mitochondrial enzymes beyond energy production, for novel gene discovery and for clinical utility. Mitochondrial defects and inherited cancer MATERNALLY IMPRINTED Genes come in pairs (alleles) — one inherited from the father and one from the mother. Maternal imprinting occurs when the maternal allele is transcriptionally silenced, usually because of promoter hypermethylation. In this situation, only the paternal allele is expressed. FOUNDER EFFECT When a germline mutation occurs in a community that has been isolated from the outside, or where little emigration or immigration has occurred for many decades or centuries, this ‘founding’ germline mutation is established and perpetrated for generations. 194 The first inherited neoplasia syndrome that was attributed to germline mutations in nuclear-encoded mitochondrial enzymes involved tumours of the adrenal medulla and paraganglia. Phaeochromocytomas are catecholamine-secreting tumours that are benign in ~90% of cases. Phaeochromocytomas usually arise within the adrenal medulla but can develop in extra-adrenal sympathetic ganglia ~10% of the time. Extra-adrenal phaeochromocytoma are sometimes referred to as paraganglioma. Vascular head and neck tumours, which usually arise from the carotid body, are referred to as head and neck paragangliomas, glomus tumours or chemodectomas. Inherited cancer syndromes with phaeochromocytoma can be a component feature of several inherited syndromes, each with distinct genetic aetiologies1–3 (TABLE 1). Familial clustering of glomus tumours was first brought to common attention when reported in 1964 (REF. 4), although the earliest report might have been in 1937. After studying such families, these and other investigators noted that glomus tumours were inherited from the paternal line5,6. Clinical observations indicated that the gene that caused familial glomus tumours was MATERNALLY IMPRINTED (paternally expressed). Working on this premise, these investigators mapped a gene for familial glomus tumours to 11q23 and showed that this predisposition was most likely due to a FOUNDER EFFECT in the Dutch population6,7. This locus was labelled PGL1. PGL1 was subsequently identified as SDHD 8, and germline mutations are associated with familial and isolated paragangliomas and phaeochromocytomas8–11 (FIG. 1). | MARCH 2003 | VOLUME 3 It also became obvious that there exist familial clusterings of paragangliomas — of the head and neck region, and elsewhere — which were not linked to PGL1 and were not maternally imprinted. Germline mutations in SDHB (PGL4) and to a much lesser extent SDHC (PGL3) were subsequently found in some families with paragangliomas and phaeochromocytomas, and these are not associated with imprinting11–14. PGL2 — another locus for familial paragangliomas in a large Dutch family — has yet to be precisely identified. Diagnosis with this cancer usually occurs when patients are in their mid-20s (range 5–60 years)10. Interestingly, germline heterozygous mutations of FH, which encodes an enzyme that catalyses the next step after SDH in aerobic metabolism, cause a completely different autosomal-dominant syndrome — hereditary leiomyomatosis and type 2 papillary renal-cell carcinoma (HLRCC). The clinical and histopathological characteristics of the renal-cell carcinomas supported a common hereditary background for these malignancies, which are distinct from other known inherited kidney cancer syndromes (TABLE 2). The apparently dominantly inherited tumours are solitary and aggressive, and usually occur early in life (between the ages of 26 and 48 years). A key feature of these tumours is their histopathology — all component renal carcinomas that have been examined have a peculiar papillary histology15,16, with resemblance to the rare papillary type 2 histology17. Phenotypic features can vary among families. Some families only develop cutaneous and uterine leiomyomatosis without renal cancer, which are sometimes referred to as multiple cutaneous leiomyomatosis (MCL). The HLRCC susceptibility gene was mapped to 1q42–q43 and germline mutations in FH were subsequently identified15,16,18–20 (FIG. 2). It is not clear why germline mutations in genes that encode two enzymes that act sequentially (BOX 1), and that are ubiquitously expressed, result in two inherited neoplasia syndromes with non-overlapping component tumours. Virtually all tumours that are associated with both syndromes have been shown to have lost the remaining wild-type allele 8,15,21–23. Further research is required to determine how loss of the wild-type allele occurs. The observation that germline mutations in genes that encode mitochondrial enzymes are associated with inherited cancer syndromes is relatively recent. In addition, somatic and non-somatic mutations and variants in the mitochondrial genome of sporadic neoplasias have been described (BOXES 1 and 2). Although no precise mechanism has been elucidated, hypotheses regarding the mitochondrial role in both energy metabolism and apoptosis have been proposed (BOX 3). Mitochondrial (dys)function I: SDH Traditionally, the mitochondria are viewed as organelles that generate energy (typically ATP) for cellular metabolism. ATP is generated via two inter-linked mitochondrial pathways — the electron-transport (or respiratory) chain and the Krebs tricarboxylic-acid cycle. There are www.nature.com/reviews/cancer REVIEWS five mitochondrial complexes that participate in the electron-transport chain (BOX 1). Complex II consists of SDH — a four-subunit enzyme that straddles the inner mitochondrial membrane, such that it can easily participate in both the electron-transport chain (membrane-associated) and Krebs cycle (mitochondrial-matrix-associated). This complex is anchored to the membrane by two membrane-spanning proteins — SDHC and SDHD. The peripheral portion of this complex is made up of a flavoprotein (SDHA) and an iron–sulphur subunit (SDHB), and projects into the mitochondrial matrix. The presence and proper functioning of both SDHA and SDHB are required for catalytic activity. The active site of the enzyme is located within SDHA and contains covalently bound FAD (BOX 1). SDH catalyses the conversion of succinate to fumarate, which, in turn, is converted to malate by fumarase. Fumarase is located in the mitochondrial matrix and participates in the Krebs cycle. Defects in the Krebs cycle have been observed to affect the nervous system and the skeletal muscles, resulting in early-onset symptoms when oxidative metabolism is impaired. This reflects the dependence of neurons and muscle cells on oxidative phosphorylation for energy requirements. Evidence also indicates that neurodegenerative diseases, such as Huntington’s disease, Parkinson’s disease and Friedreich ataxia, are Box 1 | Mitochondrial complexes I–V in health and disease The diagram shows the five complexes that are involved in the mitochondrial electron-transport chain. Complexes I–IV are the electron-transport complexes, whereas complex V synthesizes adenosine triphosphate (ATP). Electrons are passed down the four complexes (black arrows) to molecular oxygen and then complex V generates one ATP molecule from ADP and inorganic phosphate (Pi). The blue arrows show where the protons are pumped to the cytosolic side of the intermembrane to generate an electrochemical gradient, and where proton movement back across complex V (the ATP synthase) is used to drive ATP synthesis. Complex II is made up of the four components of SDH. It not only resides within the mitochondrial membrane as an active participant of the electron-transport chain, but also contacts the mitochondrial matrix, where it participates in the Krebs tricarboxylic-acid cycle. In this case, it converts succinate to fumarate. Fumarate hydratase catalyses the subsequent step in the Krebs cycle, of fumarate to malate. SDHA mutations have been associated with Leigh syndrome, paraganglioma and phaeochromacytoma. Mutations in genes that encode complex I proteins, such as NDUFV1, have been associated with leukodystrophy and epilepsy47. NDUFS2 mutations have also been associated with leukodystrophy48 and cardioencephalomyopathy (CMP)49. BCS1 mutations disrupt complex III function, and have been described in patients with tubulopathy, encephalopathy and hepatopathy50. Nuclear DNA mutations in genes such as SURF1, SCO1, SCO2 and COX10 disrupt complex IV function, and are associated with Leigh syndrome, cardioencephalomyopathy, hepatic failure and encephalopathy51,52. Disorders caused by heritable mitochondrial DNA (mtDNA) mutations have broad manifestations53. In addition to Leigh syndrome, mtDNA mutations in genes that encode mitochondrial proteins have been associated with chronic progressive external ophthalmoplegia, Kearns–Sayre syndrome, Leber hereditary optic neuropathy, and neurogenic weakness with ataxia and retinitis pigmentosa. Heritable mutations that affect mtDNA-encoded tRNA have been associated with mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes, as well as myoclonic epilepsy with ragged red fibres. Cytosol H+ H+ H+ Cyt c H+ c Fe-S FMN Mitochondrial matrix NADH CoQ FADH Fe-S FAD+ and H+ SDH NAD+ and H+ Fe-S Cu-a b Cu-a3 H2O 1/2 O2 Succinate Fumarate Fumarate Hydratase ADP and Pi ATP Malate NATURE REVIEWS | C ANCER Complex I II III IV V Nuclear gene mutations NDU FS1, 2, 4, 7,8 NDU FV1 SDHA, B, C, D BCS1L SURF1, SCO1, SCO2, COX10 Phenotype Leigh syndrome Leukodystrophy Epilepsy Cardioencephalomyopathy Hepatopathy Leigh syndrome Encephalopathy Paraganglioma Phaeochromocytoma Leigh syndrome Cardioencephalomyopathy Hepatopathy Cardioencephalomyopathy Hepatopathy VOLUME 3 | MARCH 2003 | 1 9 5 REVIEWS Table 1 | Inherited cancer syndromes with phaeochromocytoma as a component Syndrome Other component neoplasias Susceptibility gene(s) Von Hippel–Lindau disease Renal-cell carcinoma, retinal angioma, central nervous system haemangioma/haemangioblastoma VHL Multiple endocrine neoplasia type 2 Medullary thyroid carcinoma, parathyroid hyperplasia/adenoma RET Type 1 neurofibromatosis Plexiform neurofibroma, schwannoma, astrocytoma, juvenile chronic myeloid leukaemia, breast carcinoma NF1 Phaeochromocytoma– paranganglioma syndrome None SDHD, SDHC, SDHB associated with mitochondrial dysfunction. It has been postulated that respiratory-chain dysfunction and free-radical formation, together with mitochondrial defects, result in cell damage and apoptosis24 (BOX 3). Homozygous mutations in SDHA cause a markedly different phenotype than heterozygous mutations in the genes that encode the other three SDH subunits. SDHA mutations cause a predisposition to Leigh syndrome — a neurodegenerative disorder that is characterized by subacute necrotizing encephalomyelopathy during infancy25, failure to thrive and developmental delays. Lactic acidosis, seizures, ataxia and multiple brain lesions are also part of the phenotype, and the basal ganglia, midbrain and brainstem are frequently involved. Mutations of SDHA usually result in inactivation of the catalytic subunit, resulting in loss of, or markedly reduced, enzymatic activity. Half of the reported mutations (such as A524V and R554W) occur in the 3′ end of the gene and disrupt a SDHD R92Y L95P L139P P81L C.33-36delTG R38X C11X IVS1+2t>g R22X Q36X W5X 1 1 R70G 2 3 c.54InsC b SDHB 4 c.123InsC W43X R90X C.207-210InsC R46G C101Y R27X Q59X 2 Q109X c.381-383delG H102L Q121X 3 4 C.334-7delGACT P131R 5 P198R R242H C192R C.847del4 C249Y C196Y 6 7 8 Figure 1 | Schematic diagram of the SDHD and SDHB genes and germline heterozygous mutations found in the phaeochromocytoma–paraganglioma syndromes. Both truncating and missense mutations have been associated with disease phenotypes. SDHD R92Y and L139P are Dutch founder mutations (stars). Germline mutations in SDHB are most commonly associated with adrenal phaeochromocytoma, whereas mutations in SDHD are most commonly associated with extra-adrenal paraganglioma. Mutations at the 5′ end of SDHD are also believed to be associated with adrenal phaeochromocytoma. Yellow bars represent the length of the coding region of the gene, which is divided into exons (numbered). Green squares denote mutations that are associated with adrenal phaeochromocytoma, and blue circles signify mutations that are associated with extra-adrenal disorders. Each unit square or circle denotes a single family or proband that has been reported to have that mutation. 196 | MARCH 2003 | VOLUME 3 the carboxy-terminal region of the enzyme26,27. This region of the protein folds around the highly conserved catalytic core, and serves as gatekeeper by opening or closing the active site28. Such carboxy-terminal mutations result in loss of catalytic activity without alterations in substrate binding26–28. In other words, not only do these mutations result in loss of function, but they also serve as dominant negatives or ‘substrate sinks’. Post-mitotic cells, such as those of the central nervous system, have the highest energy requirements and oxygen consumption. Because of the latter, these cells also have the highest potential for superoxide production. So, loss of SDHA function results in decreased or loss of energy production from both the electron-transport chain and the Krebs cycle, as well as overproduction of free radicals, and this leads to severe early-onset neurodegeneration. Mutations away from the carboxy-terminal domain result in partial loss of enzymatic activity, decreased energy production and later-onset neurodegeneration. Unlike those associated with Leigh syndrome, phaeochromocytoma- and paraganglioma-associated mutations in the non-catalytic subunits of complex II are likely to result in destabilization and perhaps even loss of structural integrity of this complex14. Mutations that affect the anchor proteins SDHC and SDHD are predicted to result in complex disassembly. So far, only one SDHC mutation that alters the first amino acid has been described — in a single family with paragangliomas12. This mutation destroys the translational start site and so, the protein must initiate translation at the next methionine at residue 9. This truncated protein lacks the first few amino acids, which act as the signal peptide/presequence, and is therefore unable to insert itself into the mitochondrial membrane. Because this is a heterozygous germline mutation, only half of the SDHC peptides are affected, and, probably, no physiological sequelae occur. However, loss of the remaining wild-type SDHC allele occurs in the paragangliomas12, thereby resulting in complete lack of SDHC in complex II. Because both the anchor polypeptides — SDHC and SDHD — are required to bind and hold SDHA and SDHB within the membrane28, only SDHD would remain in the complex if SDHC were absent. With the available data, it seems that three-quarters of all individuals with phaeochromocytoma and germline SDHD mutations possess mutations in the 5′ portion of SDHD (FIG. 1). Head and neck paragangliomas, by contrast, are associated with mutations in the 3′ region of this gene. Interestingly, approximately www.nature.com/reviews/cancer REVIEWS Table 2 | Syndromes associated with heritable epithelial renal carcinomas Syndrome Typical renal histological type Other component neoplasias Von Hippel–Lindau disease Clear-cell renal-cell carcinoma Hereditary papillary renal-cell carcinoma Susceptibility gene Phaeochromocytoma, retinal VHL angioma, central nervous system haemangioma/haemangioblastoma Type 1 papillary renal-cell carcinoma Papillary thyroid carcinoma (rarely) MET Hereditary leiomyomatosis Type 2 papillary renal-cell carcinoma Uterine and cutaneous leiomyoma renal-cell carcinoma FH Birt–Hogg–Dube syndrome Chromophobe renal carcinomas; oncocytomas Folliculin 50% of all germline SDHD mutations occur in the first two exons and the beginning of exon 3 (up through codon 63) (FIG. 1). Disruption of this region would result in alterations of the presequence (signal peptide) and inability to insert into the mitochondrial membrane. The inability to insert into the mitochondrial membrane would also occur in the presence of truncating mutations even after amino acid 63. Therefore, the ultimate consequence of most naturally occurring germline SDHD mutations is to cause disassembly of complex II, leaving only SDHC present in the membrane and absence of its catalytic activity21. Missense mutations that occur after codon 63 (FIG. 1) would not be expected to cause complete disassembly of complex II, and so are not predicted to completely inactivate the complex. For example, whereas the common P81L and L139P mutations (FIG. 1) are expected to perturb the α-helical structure of SDHD, even complete loss of the α-helix around L139 does not completely inactivate the yeast complex29. In view of these functional sequelae, we conclude that complete disassembly of complex II causes the predisposition to phaeochromocytoma, whereas Fibrofolliculoma, colorectal carcinoma (?) partial inactivation of its catalytic activity leads to head and neck paragangliomas. SDHB is the iron–sulphur subunit that is required to act together with SDHA during catalysis. SDHB cysteine-197 serves as the ligand to the iron–sulphur moiety. Together with proline-198 and surrounding residues (exons 6 and 7), they form the key interface with anchor proteins SDHC and SDHD30. So, the phaeochromocytoma-susceptibility-associated germline SDHB mutations in exons 6 and 7 or truncating mutations before residue 197 (FIG. 1) are expected to prevent the assembly of the catalytic complex31,32. The physiological consequence would be a mixture of wild-type complex II and complexes that only contain SDHC and SDHD28,32, resulting in loss of enzymatic activity22. In addition to complex II integrity and catalytic activity, other mechanisms must also come into play in neoplasia. The carotid body contains oxygen chemoreceptors, so it is possible that chronic hypoxia (low oxygen tension) could account for the sporadic occurrence of glomus tumours in individuals who live at high N64T K187del K187R 541delAG H137R R190H G239V Q142R IVS5-15T->G A74P H153R R58X 121delTG(s) 48delC R8E (s) Q4X 1 2 3 66del174 4 5 6 K187R R190H R190C Nonsense Missense Deletion (frameshift) Deletion (in-frame) E319D(s) R300X R300X(s) M285R(s) 7 A265T F269C 1220delG 8 E319Q 9 1302insAAA D283V 10 W458X Insertion (in-frame) Deletion (whole gene) Splice-site mutation Figure 2 | The FH gene and disease-associated mutations. The yellow bar represents the structure of the FH gene, with the numbers denoting the ten exons. Heterozygous mutations in FH have been detected in 27 probands that have a predisposition to cancer19. In patients with tumour predisposition, the mutations seem to cluster at the 5′ end of FH (mutations noted above the bar), whereas mutations associated with FH deficiency tend to cluster in the 3′ half of the gene (p <0.0001, mutations shown below the bar). However, both sets of mutations seem to cause very similar reductions in FH activity. In addition to germline changes, the figure includes somatic mutation(s) detected in tumours. NATURE REVIEWS | C ANCER VOLUME 3 | MARCH 2003 | 1 9 7 REVIEWS Box 2 | Somatic alterations of mitochondrial genes in sporadic cancers In addition to energy metabolism, the mitochondrial role in apoptosis43,54 led investigators to consider genes within the mitochondrial genome as putative sporadic cancer-associated genes. This was a particularly attractive hypothesis for the so-called oncocytic tumours, which are characterized by their abundance of mitochondria. The kidney and thyroid are the two most common sites for oncocytic tumours. Because of the size of the mitochondrial genome (16.6 kb), only one study was able to systematically examine virtually all the coding sequence in oncocytic tumours — specifically in thyroid tumours55. In that study, 23% of papillary thyroid carcinomas were found to have somatic mitochondrial gene mutations. More interestingly, the distribution and spectra of non-somatic mitochondrial gene variants seemed to differ between individuals with thyroid cancer compared to normal controls, with complex I variants favoured amongst cancer cases. Together, these observations indicated that somatic mitochondrial gene mutations might be involved in thyroid tumorigenesis, and that accumulation of mitochondrial DNA variants might be related to tumour initiation or progression in the thyroid. This hypothesis seemed to be corroborated when sequencing of the entire mitochondrial genome in colorectal cancers revealed 12 different somatic mutations and 88 non-somatic sequence variants56. Subsequently, mutations and variation in the mitochondrial genome have been identified in various solid tumours, including those of the ovaries, stomach, breast, brain and prostate57–61. Because of the size of the mitochondrial genome, most of these analyses were limited to parts of the genome only. altitude. Chronic hypoxia could also explain the mechanism whereby mutations in SDHX proteins lead to hereditary paragangliomas, and by extrapolation, to phaeochromocytomas8,14,33. Mitochondria generate reactive oxygen species (ROS), which activate the transcription factor hypoxia-inducible factor-1 (HIF-1). HIF-1 is a heterodimeric protein that consists of two subunits — HIF-1α and HIF-1β. Whereas HIF-1β is constitutively expressed, the expression of HIF-1α is induced by low oxygen concentrations. HIF-1 activates the transcription of genes encoding vascular endothelial growth factor (VEGF) and glycolytic enzymes34, which promote angiogenesis — a necessary component of tumour growth. Gimenez-Roqueplo and colleagues examined HIF1 activity in phaeochromocytoma samples from a family with germline SDHD R22X mutations, compared to eight sporadic phaeochromocytomas (which did not contain SDHD mutations)21. The phaeochromocytoma cells from the patient with hereditary disease had lost the remaining wild-type allele, and were disrupted in complex II electron-transfer activity. Levels of HIF-1α, HIF-2α/EPAS1, VEGF and its receptor VEGF-R1 were shown to be increased only in the SDHD-related phaeochromocytoma. The sporadic phaeochromocytomas, conversely, retained full activity of complex II. Most sporadic phaeochromocytomas contain somatic mutations and/or deletions of the tumour suppressor von Hippel–Lindau protein (VHL). VHL inhibits HIF-1 activity by inducing degradation of one of its subunits23 (TABLES 1 and 2). Interestingly, naturally occurring VHL mutations that are associated with phaeochromocytoma have not been shown not to impair HIF-1α ubiquitylation or subsequent degradation35,36. So, there seem to be different downstream consequences of SDHD-related and sporadic phaeochromocytomas. 198 | MARCH 2003 | VOLUME 3 Mitochondrial (dys)function II: FH Heterozygous germline mutations in FH that have been observed in HLRCC families are loss-of-function mutations that cause either truncating or missense changes at highly conserved residues19 (FIG. 2). All mutations (11 of 16 different germline mutations) examined had defects in fumarase activity19. The activities were similar to those observed in heterozygous first-degree relatives of fumarase-deficiency patients. Interestingly, missense mutations resulted in more severely reduced fumarase activity than truncating mutations, including a whole gene deletion. This is conceivable because fumarase functions as a homotetramer37, and a missense mutation in one allele results in only 1 out of 16 fully wild-type homotetramers. There are three distinct domains, including a five-helical α-helix and a lysase domain, in each fumarase subunit. These domains are characteristic for this class of protein superfamily, which includes fumarase, aspartase, argininosuccinate lyase, adenylosuccinate lyase and crystalline. Alphahelixes from the four subunits form a superhelical structure in the core of the tetramer, which is a putative active site. The lyase domain (amino acids 364–373 in human FH) sequence motif (GSX(x2)MX(x2)KN) is thought to be involved in catalytic activity of the protein. It is conceivable that mutations in FH might affect multimerization of the gene product, resulting in defective catalytic activity and affecting other putative functions of FH. In general, the mutations that are associated with HLRCC occur in the 5′ of the gene, whereas, the FH-deficiency mutations tend to occur in the 3′ end (p <0.0001)18,19 (FIG. 2). However, there is some overlap. For example, a homozygous R190H mutation has been described in FH deficiency and a heterozygous R190H mutation in HLRCC. The phenotypes are also, at least to some extent, overlapping; heterozygous parents of patients that are recessive for fumarase deficiency are predisposed to tumours 19. One obvious explanation for the observed difference in the mutation spectra could be the degree of fumarase deficiency involved, in that 3′ mutations result in more severe enzymatic deficiencies. However, this simple explanation is unlikely, because the activities seen in the context of tumour-predisposing mutations are very similar to those in the recessive fumarase deficiency. The preferential mutation spectrum is intriguing and implies that the molecular basis of FHdeficient tumorigenesis might not simply relate to the enzymatic defect. Considering the findings from the studies of SDHX genes, the association of FH with HLRCC was not a complete surprise. FH acts in the Krebs cycle, in the step following that of the SDH complex (BOX 1). Unlike SDH, FH has no known role in the electron-transport chain. Given this fact, the mechanisms of tumorigenesis that are driven by FH defects can only be speculated about. It has been proposed that DNA mutations that result from oxidative damage could promote tumorigenesis, but this remains unproven19. Another suggestion has been that blockage of the tricarboxylic-acid cycle leads to www.nature.com/reviews/cancer REVIEWS feedback on oxidative metabolism, and subsequently on the cell cycle, through angiogenic pathways19. Other unknown functions of SDH and FH might also be involved in tumour suppression. Neoplasia or neurodegeneration? The observation that homozygous loss-of-function germline mutations in SDHA or FH lead to neurodegeneration, without cancer, whereas heterozygous germline mutations in three out of four SDHD genes or FH lead to cancer susceptibility is at first puzzling. This apparent paradox deepens when we consider the observation that, at the cellular level, loss of the remaining wild-type allele occurs in component neoplasias that have germline heterozygous mutations in the respective genes. In other words, why does complete or near-complete loss of enzymatic function in SDHA and FH lead to neurodegeneration, yet a similarly complete loss of enzymatic function effected by germline heterozygous mutation followed by somatic loss of the wild-type allele in the transforming cells result in cancer? When this conundrum is considered at the organismal, organ and cellular levels, several plausible explanations begin to emerge. At the organismal and organ levels, homozygous mutations in either SDHA or FH lead to complete or near-complete loss of activity (see above) in every cell of the body throughout development and shortly after birth — crucial times in neurological development. Given the particularly high oxygen and energy demands in the developing nervous system, it becomes plausible that this chronic lack of oxygen and energy would lead to severe neurological dysfunction. That Leigh syndrome and fumarase deficiency are consequences of a nervous system that is starved of energy are supported by the observation that mutations in both the mitochondrial-encoded enzymes and non-complex-II respiratory-chain components also result in similarly devastating neurological manifestations. These genes include NDUFS4 (REF. 38) , NDUFS8 (REF. 39) and NDUFS7 (REF. 40) (which are all part of complex I), as well as SURF1 (REF. 41) and COX10 (REF. 42), which comprise complex IV. Heterozygous germline mutations in SDH or FH, by contrast, only reduce gene dosages. These reduced dosages are adequate for normal neurological development, as heterozygous individuals do not have neurological deficits. Box 3 | Mitochondria mediate energy-dependent and energy-independent apoptosis Energy-independent apoptosis is mediated by oxygen Mitochondrial membrane (O2) free radicals. When mitochondrial function is impaired, severe energy deficits occur and large amounts Mitochondrial of oxygen free radicals are generated. When membrane disruption mitochondria sense the presence of oxygen free radicals (FH, SDHX mutation) (hypoxia), hypoxia-inducible factors (HIFs), such as HIF-1, are activated and translocated to the nucleus Complex II disassembly where they induce gene expression. HIF-1 gene targets encode proteins that promote cellular proliferation or FH prevent apoptosis, leading to neoplasia. This might Procaspases SDH explain the cancer predisposition that are observed in APAF1 Cytosol patients with hereditary leiomyomatosis and type 2 Cytochrome c papillary renal-cell carcinoma and inherited phaeochromocytoma–paraganglioma syndrome. Some Energy Nucleus depletion HIF-1 target genes are pro-apoptotic, such as TP53, which activates cell death. This might explain the Caspases neurodegeneration that is observed as a result of SDHA or fumarase deficiency. This mechanism of neuronal-cell Induction of anti-apoptotic, damage and death might lead to the manifestations of O2 free Apoptosis pro-proliferative radicals Leigh syndrome and fumarase deficiency. genes (TGFβ, Conversely, it is plausible that heterozygous mutations PDGF, EGFR) Hypoxia HIF HIF in SDHX, which leads to partial complex assembly or complete complex II disassembly, result in sufficient alteration in membrane composition to allow for some resistance to apoptosis and might explain, at least partially, cancer predisposition. It is also plausible that mutant forms of SHD that do not insert in the mitochondrial membrane have anti-apoptotic activity. Another caspase-independent, energy-independent pathway (not shown) of apoptosis is mediated by apoptosisinducing factor (AIF) and endonuclease-G (endoG), which are believed to be released from the mitochondrial intermembrane on apoptosis induction and translocate to the cytosol and then the nucleus43,44. Once AIF reaches the nucleus, it causes peripheral-chromatin condensation and DNA fragmentation. Unlike AIF, endoG is believed to require other cofactors, perhaps other DNases, to mediate DNA degradation and apoptosis. Energy-dependent apoptosis involves the activity of caspases. When the mitochondrial membrane is breached or its composition altered, the proteins that reside between the inner and outer mitochondrial membranes, such as procaspases, apoptosis-inducing factor (APAF1) and cytochrome c, are released. Pro-caspases are then cleaved to caspases in an energy-dependent reaction, and these enzymes mediate apoptosis. NATURE REVIEWS | C ANCER VOLUME 3 | MARCH 2003 | 1 9 9 REVIEWS For example, whereas a child with homozygous FH mutations developed neurological disorders, the child’s heterozygous mother developed only HLRCC, without neurological signs or symptoms19. One explanation for this is that in cases of inherited cancer syndromes, somatic loss of the respective remaining allele occurs later in life, and these cells then become transformed. But the mechanism by which the eventual loss of SDH and FH activity leads to neoplasia is not understood. One explanation could be that individuals suffering from severe neurological dysfunction due to homozygous SDHA or FH mutations die in childhood or early teens, before the age in which heterozygous SDH- and FH-related tumours develop. Although this might be true for patients with FH, who develop tumours in their mid-20s, the youngest ages at which heterozygous SDH-related tumours develop can be as young as 5 years old (average 25 years)10. It is possible that energy depletion or free-radical generation triggered by mitochondrial dysfunction underlie the cellular basis of neurodegeneration and tumorigenesis. A paradox seems to exist regarding the ability of mitochondria and free radicals to both promote and prevent apoptosis. Partial or complete loss of SDH or FH activity leads to energy depletion and freeradical formation. Mitochondrial-mediated apoptosis can be energy dependent or independent (BOX 3). It is conceivable that partial decreases in activity, as would be the case in the heterozygous cancer-predisposing states, would lead to chronic, low-level reductions in energy production, which are insufficient to cause overt symptoms but could contribute to inefficient energydependent apoptosis43,44. The subsequent loss of the wild-type allele in the cell could lead to complete loss of energy-dependent apoptosis. The integrity of the mitochondrial outer membrane is also crucial to maintaining cellular homeostasis. Once the membrane is breached or undergoes a change in composition, an energy-independent apoptotic cascade occurs that involves release of cytochrome c and procaspases43,44 (BOX 3). Presumably, if SDH components disassemble or become disorganized within the membrane, the membrane composition might be altered, and the cell might be able to resist apoptosis. With reductions in complex II or FH function, free-radical production also increases and is sensed by the mitochondria as hypoxia45. This leads to stabilization of HIF-1, its translocation to the nucleus and activation of its target genes45. The HIF-1 gene targets include transforming growth-factor-β (TGFβ), platelet-derived growth-factor-receptor-β (PDGFβ) and a ligand for the epidermal growth-factor receptor (EGFR) — all of which have oncogenic properties and induce cellular proliferation. Furthermore, elevated ROS levels that are secondary to dysfunctional mitochondria often lead to activation of other signaltransduction pathways, such as the mitogen-activated protein kinase (MAPK) pathway, which is central to tumorigenesis. Together with oncogenic-pathway activation, elevated ROS levels result in resistance to apoptosis — probably due to more effective antioxidant defences — and also contribute to neoplasia. 200 | MARCH 2003 | VOLUME 3 What of neurodegeneration? Unfortunately, there is little data to explain the precise mechanism that leads to neurodegeneration in Leigh syndrome or fumarase deficiency. It is believed that when oxidative phosphorylation is shut down, large quantities of ROS are produced. In this situation, peroxidation of the mitochondrial membrane occurs and apoptosis ensues, as a result of membrane breakdown (BOX 3). Crosstalk between the HIF-1 and other pathways might also occur. Reactive oxygen species such as nitric oxide and carbon monoxide prevent HIF-1 induction and binding to DNA. In cases of severe hypoxia or anoxia, which can occur during Leigh syndrome or fumarase deficiency, HIF-1 can induce expression of the pro-apoptotic genes, such as TP53 (REF. 45), which mediate neuronal-cell death. So, the yin and yang of the ‘life-giving’ energy-producing side and the ‘death-promoting’ side of mitochondria, gene dosage, timing and exposure time to loss-of-function as well as tissue sensitivities could explain the different phenotypic manifestations of complex II or FH dysfunction. However, how the cell decides which route to take is still unknown. Finally, it is plausible that beyond their traditional enzymatic functions in the electron-transport chain and Krebs cycle, SDH and FH might have other independent functions. A good model that might shed some light on this possibility comes from studies of the apoptosis-inducing factor (AIF). AIF is believed to induce nuclear apoptosis independent of the caspases (BOX 3). In addition to its apoptotic function, AIF can independently catalyse the reduction of cytochrome c in the presence of NADH46, and stably bind FAD. So, AIF can be considered to be a flavoprotein that has oxydoreductase activity — properties that are similar to those of SDH. By analogy, it is also possible that SDH can act independently of its energy-generating functions to mediate apoptosis directly. In this regard, given that most heterozygous mutations in SDHB, SDHC and SDHD prevent the entire complex from assembling within the mitochondrial membranes, or disrupt assembly, it is possible that it is the non-membraneassociated/cytosolic, or the truncated SDH subunits, that are released and have anti-apoptotic activities. These hypotheses need to be empirically investigated. Future directions The unexpected association between two nuclearencoded mitochondrial enzymes, FH and SDH, and human cancer should inspire further research into the genetic, cellular and clinical aspects of mitochondrial function. Although the traditional activities of the electron-transport chain and Krebs cycle seemed rudimentary, and are first learned at the secondary school level, there is a clear lack of understanding about how mitochondrial deficiencies lead to tumour development. Although SDH and FH are known to act in tandem in electron transport and the Krebs cycle (BOX 1), and are both ubiquitously expressed, the cancer syndromes that develop when their function is disrupted (phaeochromocytoma–paraganglioma syndromes and www.nature.com/reviews/cancer REVIEWS HYPERBARIC OXYGEN Oxygen that is delivered at high tension/pressure, which is well above atmospheric oxygen tension at sea level (defined as 1 atm). HLRCC/MCL) are quite different. Because of the association of mitochondria with energy production and apoptosis, hypotheses involving free radicals, hypoxia, angiogenesis, cell damage and apoptosis are invoked (BOX 3). Apart from scant data, little else is known. So can we exploit our knowledge of SDH and FH for routine clinical application? In the case of SDH, in addition to molecular diagnosis and predictive testing in known phaeochromocytoma–paraganglioma families, recent data indicate that genetic analysis for mutations in SDHX genes should be performed routinely on patients that develop phaeochromocytomas and paragangliomas10,23. Such evidence-based changes in medical practice will improve diagnosis, prognostic analysis and prophylactic surgery decisions for the patients involved and their families. Although HLRCC/MCL families are rare, the challenge for using routine FH clinical testing is to delineate the extent of such germline mutations in individuals with uterine leiomyomas. Uterine leiomyomas are one of the most common tumours in humans, and although benign, require a tremendous amount of health-care resources. So, mechanistic understanding of FH’s role in neoplasia might provide important insights into medical management either by early diagnosis, prevention and/or therapy. Examination of gene–gene and gene–environment interactions might also reveal new preventative measures. For instance, studies have shown that individuals living at high altitude, such as the Andes, have a higher incidence of carotid-body paragangliomas, presumably as a result of chronic (relative) hypoxia associated with neoplastic 1. Latif, F. et al. Identification of the von Hippel–Lindau disease tumor suppressor gene. Science 260, 1317–1320 (1993). 2. Mulligan, L. M. et al. Specific mutations of the RET protooncogene are related to disease phenotype in MEN 2A and FMTC. Nature Genet. 6, 70–74 (1994). 3. Eng, C. et al. The relationship between specific RET protooncogene mutations and disease phenotype in multiple endocrine neoplasia type 2: International RET Mutation Consortium analysis. JAMA 276, 1575–1579 (1996). 4. Kroll, A. J., Alexander, B., Cochios, F. & Pechet, L. Hereditary deficiencies of clotting factors VII and X associated with carotid-body tumors. N. Engl. J. Med. 270, 6–13 (1964). 5. van der Mey, A. G., Maaswinkel-Mooy, P. D., Cornelisse, C. J., Schmidt, P. H. & van de Kamp, J. J. Genomic imprinting in hereditary glomus tumours: evidence for new genetic theory. Lancet 2, 1291–1294 (1989). 6. Heutink, P. et al. A gene subject to genomic imprinting and responsible for hereditary paragangliomas maps to 11q23qter. Hum. Mol. Genet. 1, 7–10 (1992). 7. Heutink, P., van Schothorst, E. M. & van der Mey, A. G. L. Further localization of the gene for hereditary paragangliomas and evidence for linkage in unrelated families. Eur. J. Hum. Genet. 2, 148–158 (1994). 8. Baysal, B. E. et al. Mutations in SDHD, a mitochondrial complex II gene, in hereditary paraganglioma. Science 287, 848–851 (2000). Identification of SDHD as the susceptiblity gene for 11q-linked hereditary paraganglioma families. SDHD is the first nuclear gene that encodes a mitochondrial component and that has been shown to be involved in a cancer-susceptiblity syndrome. 9. Gimm, O., Armanios, M., Dziema, H., Neumann, H. P. H. & Eng, C. Somatic and occult germline mutations in SDHD, a mitochondrial complex II gene, in non-familial pheochromocytomas. Cancer Res. 60, 6822–6825 (2000). 10. Neumann, H. P. H. et al. Germ-line mutations in nonsyndromic pheochromocytoma. N. Engl. J. Med. 346, 1459–1466 (2002). NATURE REVIEWS | C ANCER 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. enlargement of the carotid body 33. Therefore, should individuals who are found to carry germline SDHX mutations be advised to migrate to lower altitudes or be exposed to HYPERBARIC OXYGEN. Iron is necessary for the proper functioning of the iron–sulphur moiety that is integral to complex II, which, in turn, affects the function of fumarase (BOX 1). Would supplementation with elemental iron prevent neoplasia in individuals with heterozygous germline SDHX or FH mutations? Along the same lines, could addition of increased oxygen tension, in addition to iron supplementation, also prevent disease? Another possibility is to provide fumarate supplements to individuals with heterozygous SDHX mutations, and malate supplements to those with HLRCC/MCL, to prevent cancer. Finally, the recent associations of inherited cancer syndromes with neurological disorders, both caused by germline defects in the same genes, indicate an interesting bioinformatics exercise for new cancer-predisposition gene discovery. Germline homozygous mutations in many of the nuclear-encoded mitochondrial components have been delineated. It would be ideal if the gene-expression profiles of patients with SHDX/ phaeochromocytoma–paraganglioma syndromes/ Leigh syndrome and FH/HLRCC-MCL/fumarase deficiency could be studied, to determine common and distinct profiles in inherited neoplasia compared to neurological disease. This might be extrapolated to sporadic neoplasias as well, given that mitochondrial genome variation has been described both in neuromuscular disorders and somatically in some sporadic solid tumours (BOXES 1 and 2). Population-based study showing that 25% of unrelated non-syndromic, non-familial phaeochromocytoma cases are due to germline mutations in one of four genes, including SDHD and SDHB. Baysal, B. E. et al. Prevalence of SDHB, SDHC and SDHD in clinic patients with head and neck paragangliomas. J. Med. Genet. 39, 178–183 (2002). Niemann, S. & Muller, U. Mutations in SDHC cause autosomal dominant paraganglioma. Nature Genet. 26, 141–150 (2000). Astuti, D. et al. Mutations in the mitochondrial complex II subunit SDHB cause susceptibility to familial paraganglioma and pheochromocytoma. Am. J. Hum. Genet. 69, 49–54 (2001). Identification of SDHB as the susceptibility gene for familial paraganglioma and/or phaeochromocytoma. Baysal, B. E. Hereditary paraganglioma targets diverse paranglia. J. Med. Genet. 39, 617–622 (2002). Kiuru, M. et al. Familial cutaneous leiomyomatosis is a two-hit condition associated with renal cell cancer of characteristic histopathology. Am. J. Pathol. 159, 825–829 (2001). Launonen, V. et al. Inherited susceptibility to uterine leiomyomas and renal cell cancer. Proc. Natl Acad. Sci. USA 98, 3387–3392 (2001). Delahunt, B. & Eble, J. N. Renal cell neoplasia. Pathology 34, 13–20 (2002). Kiuru, M. et al. Few FH mutations in sporadic counterparts of tumor types observed in hereditary leiomyomatosis and renal cell cancer families. Cancer Res. 62, 4554–4557 (2002). Tomlinson, I. P. M. T. et al. Germline mutations in the fumarate hydratase gene predispose to dominantly inherited uterine fibroids, skin leiomyomata and renal cell cancer. Nature Genet. 30, 406–410 (2002). Identification of germline heterozygous mutations in FH that cause susceptibility to HLRCC. Alam, N. A. et al. Localization of a gene (MCUL1) for multiple cutaneous leiomyomata and uterine fibroids to chromosome 1q42.3-q42. Am. J. Hum. Genet. 68, 1264–1269 (2001). Gimenez-Roqueplo, A.-P. et al. The R22X mutation of the SDHD gene in hereditary paraganglioma abolishes enzymatic activity of the complex II mitochondrial respiratory 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. chain and activates the hypoxia pathway. Am. J. Hum. Genet. 69, 1186–1197 (2001). First demonstration of loss of enzymatic activity as a consequence of SDHD mutation and consequent alterations in molecules in the HIF pathway. Gimenez-Roqueplo, A. P. et al. Functional consequences of a SDHB gene mutation in an apparently sporadic pheochromocytoma. J. Clin. Endocrinol. Metab. 87, 4771–4774 (2002). Maher, E. R. & Eng, C. The pressure rises: update on the genetics of phaeochromocytoma. Hum. Mol. Genet. 11, 2347–2354 (2002). Schapira, A. H. Mitochondrial dysfunction in neurodegenerative disorders. Biochim. Biophys. Acta 1366, 225–233 (1998). Leigh, D. Subacute necrotizing encephalomyelopathy in an infant. J. Neurol. Neurosurg. Psychiatr. 14, 216–221 (1951). Bourgeron, T. et al. Mutation of the fumarase gene in two siblings with progressive encephalopathy and fumarase deficiency. J. Clin. Invest. 93, 2514–2518 (1994). Parfait, B. et al. Compound heterozygous mutations in the flavoprotein gene of the respiratory chain complex II in a patient with Leigh syndrome. Hum. Genet. 106, 236–243 (2000). Ackrell, B. A. C. Progress in understanding structurefunction relationships in respiratory chain complex II. FEBS Lett. 466, 1–5 (2000). Oyedotun, K. S. & Lemire, B. D. The quinone-binding sites of the Saccharomyces cerevisiae succinateubiquinone oxidoreductase. J. Biol. Chem. 276, 16936–16943 (2001). Iverson, T. M., Luna-Chavez, C., Cecchini, G. & Rees, D. C. Structure of the Escherichia coli fumarate reductase complex. Science 284, 1961–1966 (1999). Vinogradov, A. D., Ackrell, B. A. C. & Singer, T. P. On the possible interrelations of the reactivity of soluble succinate dehydrogenase with ferricyanide, reconstitution activity and the Hipip iron-sulfur center. Biochem. Biophys. Res. Comm. 67, 803–809 (1975). VOLUME 3 | MARCH 2003 | 2 0 1 REVIEWS 32. Schmidt, D. M., Saghbini, M. & Scheffler, I. E. The C-terminus of the succinate dehydrogenase IP peptide of the Saccharomyces cerevisiae is signficiant for assembly of complex II. Biochemistry 31, 8442–8448 (1992). 33. Arias-Sella, J. & Valcarcel, J. Chief cell hyperplasia in the human carotid body at high altitudes; physiologic and pathologic significance. Hum. Pathol. 7, 361–373 (1976). 34. Chandel, N. S. et al. Mitochondrial reactive oxygen species trigger hypoxia-induced transcription. Proc. Natl Acad. Sci. USA 95, 11715–11720 (1998). 35. Clifford, S. C. et al. Contrasting effects on HIF-1α regulation by disease-causing pVHL mutations correlate with patterns of tumourigenesis in von Hippel–Lindau disease. Hum. Mol. Genet. 10, 1029–1038 (2001). 36. Hoffman, M. A. et al. von Hippel–Lindau protein mutants linked to type 2C VHL disease preserve the ability to downregulate HIF. Hum. Mol. Genet. 10, 1019–1027 (2001). 37. Teipel, J. W. & Hunt, R. L. The subunit interactions of fumarase. J. Biol. Chem. 246, 4859–4865 (1971). 38. van den Heuvel, L. et al. Demonstration of a new pathogenic mutation in human complex I deficiency: a 5-bp duplication in the nuclear gene encoding the 18kD (AQDQ) subunit. Am. J. Hum. Genet. 62, 262–268 (1998). 39. Loeffen, J. et al. The first nuclear-encoded complex I mutation in a patient with Leigh syndrome. Am. J. Hum. Genet. 63, 1598–1608 (1998). 40. Triepels, R. H., van den Heuvel, L. & Loeffen, J. Leigh syndrome associated with a mutation in the NDUFS7 (PSST) nuclear encoded subunit of complex I. Ann. Neurol. 45, 787–790 (1999). 41. Tiranti, V. et al. Mutations of SURF-1 in Leigh disease associated with cytochrome c oxidase deficiency. Am. J. Hum. Genet. 63, 1609–1621 (1998). 42. Valnot, I., von Kleist-Retzow, J. C. & Barrientos, A. A mutation in the human heme A:farnesyltransferrase gene (COX 10) causes cytochrome c oxidase deficiency. Hum. Mol. Genet. 9, 1245–1249 (2000). 43. van Loo, G. et al. The role of mitochondrial factors in apoptosis: a Russian roulette with more than one bullet. Cell Death Differ. 9, 1031–1042 (2002). 44. Ravagnan, L., Roumier, T. & Kroemer, G. Mitochondria, the killer organelles and their weapons. J. Cell. Physiol. 192, 131–137 (2002). 45. López-Barneo, J., Pardal, R. & Ortega-Sáez, P. Cellular mechanisms of oxygen sensing. Annu. Rev. Physiol. 63, 259–287 (2001). 202 | MARCH 2003 | VOLUME 3 46. Miramar, M. D. et al. NADH-oxidase activity of mitochondrial apoptosis inducing factor (AIF). J. Biol. Chem. 276, 16391–16398 (2001). 47. Scheulke, M., Smeitink, J. & Mariman, E. Mutant NDUFV1 subunit of mitochondrial complex I causes leukodystrophy and myoclonic epilepsy. Nature Genet. 21, 260–261 (1999). 48. Benit, P. et al. Large-scale deletion and point mutations of the nuclear NDUFV1 and NDUFS1 genes in mitochondrial complex I deficiency. Am. J. Hum. Genet. 68, 1344–1352 (2001). 49. Loeffen, J. et al. Mutations in the complex I NDUFS2 gene of patients with cardiomyopathy and encphalomyopathy. Am. J. Hum. Genet. 49, 195–201 (2001). 50. de Lonlay, P. et al. A mutant mitochondrial respiratory chain assembly protein causes complex III deficiency in patients with tubulopathy, encephalopathy and liver failure. Nature Genet. 29, 57–60 (2001). 51. Papadopoulou, L. C., Sue, C. M. & Davidson, M. Fatal infantile cardioencephalomyopathy with cytochrome c oxidase (COX) deficiency due to mutations in SCO2, a human COX assembly gene. Nature Genet. 23, 333–337 (1999). 52. Valnot, I., Ormond, S. & Gigarel, N. Mutations of the SCO1 gene in mitochondrial cytochrome c oxidase (COX) deficiency with neonatal-onset hepatic failure and encephalopathy. Am. J. Hum. Genet. 67, 1104–1109 (2000). 53. Servidei, S. Mitochondrial encephalomyopathies: gene mutation. Neuromuscul. Disord. 12, 224–229 (2001). 54. Green, D. R. & Reed, J. C. Mitochondria and apoptosis. Science 281, 1309–1312 (1998). 55. Yeh, J. J. et al. Two-dimensional gene scanning of the mitochondrial genome reveals somatic mutations in papillary thyroid carcinomas and multiple sequence variants in cases with sporadic thyroid tumors. Oncogene 19, 2060–2066 (2000). 56. Polyak, K. et al. Somatic mutations of the mitochondrial genome in human colorectal tumours. Nature Genet. 20, 291–293 (1998). 57. Jeronimo, C. et al. Mitochondrial mutations in early state prostate cancer and bodily fluids. Oncogene 20, 5195–5198 (2001). 58. Kirches, E. et al. High frequency of mitochondrial DNA mutations in glioblastoma multiforme identified by direct sequence comparison to blood samples. Int. J. Cancer 93, 534–538 (2001). 59. Liu, V. W. et al. High incidence of somatic mitochondrial DNA mutations in human ovarian carcinomas. Cancer Res. 61, 5998–6001 (2001). 60. Maximo, V. et al. Microsatellite instability, mitochondrial DNA large deletions, and mitochondrial DNA mutations in gastric carcinoma. Gene Chromosom. Cancer 32, 136–143 (2001). 61. Parrella, P. et al. Detection of mitochondrial DNA mutations in primary breast cancer and fine-needle aspirates. Cancer Res. 61, 7623–7626 (2001). Acknowledgements C. E. is a recipient of the Doris Duke Distinguished Clinical Scientist Award and is supported by grants from the National Institutes of Health, National Cancer Institute, American Cancer Society, US Department of Defense Breast and Prostate Cancer Research Programs, Susan G. Komen Breast Cancer Research Foundation and Jimmy V Golf Classic Translational Cancer Research Award from the V Foundation. M. K. is supported by the Finnish Cancer Society, Duodecim, Kidney Foundation, Paulo Foundation, Maud Kuistila Foundation, Ida Montin Foundation, Finnish Oncology Foundation, Research and Science Foundation of Pharmos, and AstraZeneca. L. A. A. is supported by the Finnish Cancer Society, Sigrid Juselius Foundation, Helsinki Central Hospital and the Academy of Finland’s Center of Excellence Award. Online links DATABASES The following terms in this article are linked online to: Cancer.gov: http://www.cancer.gov/cancer_information/ head and neck tumours | kidney cancer LocusLink: http://www.ncbi.nih.gov/LocusLink/ AIF | BCS1 | COX10 | FH | HIF-1α | HIF-1β | NDUFS4 | NDUFS7 | NDUFS8 | NDUFV1 | PGL1 | PGL2 | SCO1 | SCO2 | SDHA | SDHB | SDHC | SDHD | SURF1 | VHL OMIM: http://www.ncbi.nlm.nih.gov/Omim/ Friedrich ataxia | HLRCC | Huntingdon’s disease | Leigh syndrome | MCL | paraganglioma | Parkinson’s disease | phaeochromocytoma FURTHER INFORMATION Medical Genetics Information Resource: www.geneclinics.org Access to this interactive links box is free online. www.nature.com/reviews/cancer