* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Antipsychotics - TOP Recommended Websites
Toxicodynamics wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
NMDA receptor wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Chlorpromazine wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Antipsychotic wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
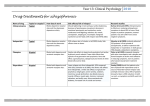
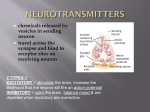
CHEMICAL TRANSMISSION DRUG ACTION IN THE CNS Ján Mojžiš P.J. Šafárik University Faculty of Medicine Department of Pharmacology Košice Neurotransmiters Noradrenaline Acetylcholine Dopamine Serotonin GABA Glutamate Aspartate Noradrenaline relatively large amount of NA hypothalamus and limbic system also present in other brain region Receptors: 1A-C, 2A-C, 1, 2, 3 depression (deficiency of NA) mania (excess of NA) Acetylcholine ACh - widely distributed in the brain Receptors: N, M1-5 some M-receptors act presynaptically ACh release M-antagonists ACh release little information about function of N-receptors in the brain Acetylcholine Dementia and Alzheimer´s disease senile dementia – slowly progressive loss of intellectual ability (5 % over the age of 65, 20% over 80) Alzheimer´s disease – same pathology irrespective of the age of onset selective loss of cholinergic neurons was found in dementia to facilitate cholinergic transmision choline (precursor), donepezil (AChE-I) Acetylcholine Parkinson´s disease, Huntington´s chorea cholinergic neurons of the corpus striatum ACh release from the striatum is strongly inhibited by D hyperactivity of cholinergic neurons (associated with a lack of D) hypokinesia, rigidity, tremor (Parkinson´s d.) - M – antagonists hypoactivity (associated with an excess of dopamine) hyperkinetic movements, hypotonia (Huntington´s chorea) - anticholinesterase Dopamine large amount corpus striatum (coordination of movement) also in limbic system dopaminergic neurons lack dopamine -hydroxylase, and thus do not produce NA Receptors: D1, D5 - of AC; D2 , D3, D4 - of AC Dopamine Motor system Deficiency of dopamine in nigrostriatal pathway Parkinson´s disease (degenerative disorder - lack of dopamine) parkinsonism (e.g. long term use of antipsychotic drugs receptor blockade) rigidity tremor hypokinesia Dopamine Behavioral effects schizophrenia in man is associated with dopaminergic hyperactivity Anterior pituitary gland dopamine and dopamine receptor agonists of prolactin secretion dopamine increases growth hormone secretion paradoxically, dopamine agonists the excessive secretion responsible for acromegaly (bromocriptine) Dopamine Vomiting D2- receptors (in chemoreceptor trigger zone) important role in nausea and vomiting drugs that dopamine release in the brain nausea and vomiting D-antagonists (phenotiazines, metoclopramide) antiemetic activity Serotonin (5-HT) distribution of 5-HT neurons is very similar to that of NA neurons Receptors: 5-HT1A-F, 5-HT2A-C, 5-HT3, 5-HT4, 5-HT5A-B, 5-HT6, 5-HT7 Sleep, mood depletion of 5-HT Insomnia 5-HT, as well as NA, may be involved in the control of mood deficit depression Hallucinatory effects many centrally acting 5-HT antagonists are hallucinogens (LSD) 5-HT neurons inhibitory influence on cortical neurons loss of cortical inhibition (e.g. by LSD) hallucinogenic efect Serotonin Sensory transmission depletion of 5-HT exagerated responses to many forms of sensory stimuly 5-HT exerts an inhibitory effect on pain transmission synergistic effect between 5-HT and opioid analgesics depletion of 5-HT antagonises the analgetic effect of opioids Serotonin Autonomic and endocrine function temperature regulation control of BP control of sexual function Clinical implications depression, anxiety migraine, emesis GABA mainly in the nigrostratial system principal inhibitory transmitter in the brain Receptors GABA-A – part of Cl- channels (BZD, barbiturates, alcohol) GABA-B - presynaptic, G-protein linked - inhibition of transmitter release Clinical implications Insomnia, anxiety alcohol withdrawal Spasticity, epilepsy EXCITATORY AMINO ACIDS (EAA) particularly glutamate and aspartate Receptors: AMPA, Kainate receptors rapid neurotransmission NMDA long-term potentiation excitotoxicity pathogenesis of epilepsy Functional aspects of NMDA receptors long-term potentiation enhancement of synaptic transmission (days or week) in various CNS synapses after short stimulation (learning, memory) excitotoxicity entry of Ca2+ produced by NMDA receptor activation neuronal damage following cerebral ischemia pathogenesis of epilepsy ??? - high concentration of glutamate in areas surrounding an epileptic focus Antipsychotic drugs Features of psychosis Delusions Hallucinations Grossly disorganized speech or behavior Uses of antipsychotic drugs Schizophrenia Manic phase of Bipolar Disorder Major depression with psychotic features others Characteristics of schizophrenia Chronic psychotic illness characterized by disordered thinking and a reduced ability to comprehend reality. Prevalence 0.5–1.0% of population Onset Positive features in late adolescence or early adulthood Aspects of cognitive deficits detectable earlier in life Comorbidity Depression: ∼30–50% Substance abuse: ∼50% Suicide: ∼5–10% Schizophrenia - symptoms Positive Symptoms delusions hallucinations thouhgt disorder Negative Symptoms low motivation, social involvement emotional abnormalities cognitive deficits = attention, planning, memory language problems Schizophrenia - a disease with various aspects Positive Symptoms Delusions Hallucinations Disorganized speech Ca Cognitive Deficits Attention Memory Executive functions (e.g., abstraction) Negative Symptoms Affective flattening Anhedonia Social withdrawal Social/Occupational Dysfunction Work Interpersonal relationships Self-care Mood Symptoms Depression Anxiety Aggression Hopelessness Suicidality Simplify neurocircuitry of dopamine in schizophrenia Mesolimbic pathway Hyperdopaminergia DA D2 Mesocortical pathway Hypodopaminergia DA Limbic Positive symptoms D1 Negative symptoms PFCx The cause of schizophrenia Etiology is unknown..... but... combination of genetic and environmental factors associated with neurodevelopmental disorder affects several brain areas Dopamine theory Dopamine theory Schizophrenia is caused by excess dopaminergic activity Arose in 1950s - 1960s: First effective antipsychotic drugs = dopamine antagonists Other supporting evidence: Reserpine = “dopamine depleter” has some weak antipsychotic activity DA enhancers (anti-Parkinson drugs, amphetamine) mimic some positive symptoms: hallucinations, delusions apomorphine bromocriptine potent D2-receptor agonists produce similar effects exacerbate the symptoms in schizophrenic patients Dopamine theory: contrary evidence D2 antagonists are not specific for schizophrenia reduce psychosis in other conditions, too Growing appreciation of other neurotransmitter systems Glutamate 5-HT Others: ACh, GABA Lot of CSF, urine, serum, postmortem, imaging, functional studies have not yielded consistent support for a primary DA changes in untreated patients Dopamine, still Important Is schizophrenia caused by DA defect ?????? But antipsychotic drugs do act via DA system Which receptors? What brain regions? Role in side effects? Dopamine receptor subtypes D1 - D5 D2 mediates much of ‘typical APD’ therapeutic action . . . . . . and side effects Dopamine pathways in the brain 2 3 1 4 Mesolimbic dopamine system DA worsens delusions, hallucinations D2 blockade alleviates delusions, hallucinations Mesocortical dopamine system DA motivation, reward, other ‘higher functions’ D2 blockade worsens ‘negative symptoms’ Nigrostriatal dopamine system DA Essential for extrapyramidal motor function D2 blockade produces extrapyramidal symptoms Tuberoinfundibular dopamine system DA inhibits prolactin release D2 blockade hyperprolactinemia Antipsychotic drugs Effective with regard to positive symptoms in 20-30% of patients Much weaker effect on negative symptoms than positive symptoms Significant parkinsonian symptoms and anticholinergic effects (poor compliance and potentially disabling) Tardive dyskinesia in a minimum of 20% of patients who receive chronic neuroleptic treatment. At least as effective as typical neuroleptics with regard to positive symptoms More effective than typical agents with regard to negative symptoms Much lower incidence of parkinsonian symptoms and anticholinergic effects than typical agents TD does occur but at much lower incidence Elevated risk of metabolic side effects Typical antipsychotics Chemical classes: Phenothiazines - chlorpromazine, fluphenazine Thioxanthenes - thiothixine Butyrophenones - haloperidol, droperidol Other: loxapine (dibenzoxazepine), molindone Diphenylbutylpiperidines: pimozide Typical antipsychotic drug actions D2 Dopamine antagonism Muscarinic receptor antagonism 1 adrenergic receptor antagonism Histamine H1 receptor antagonism D2 receptor blockade Therapeutic effects Amelioration of the positive signs, symptoms of psychosis, manic symptoms, aggressive behaviors Antiemetic effect D2 receptor blockade Adverse effects Extrapyramidal symptom (EPS) Acute; akathisia, acute dystonia, parkinsonism Late; tardive dyskinesia Endocrine effects: prolactin elevation Weight gain due to increase feeding Late onset Acute onset Spectrum of EPS Acute dystonia Tardive Dystonia vs. Tardive Dyskinesia Tardive dystonia • Strikes younger • Strikes sooner in the course of neuroleptic treatment • Poor prognosis • More males • Patients with mood disorders may be more susceptible • Anticholinergics may improve condition Tardive dyskinesia • Strikes older • Strikes later in the course of neuroleptic treatment • Variable prognosis • More females (?) • Patients with mood disorders may be more susceptible • Anticholinergics usually worsen condition Neuroleptic malignant syndrome NMS is an uncommon but serious and potentially fatal complication of therapy It is a syndrome of EPS, hyperthermia, altered consciousness, and autonomic changes (tachycardia, unstable BP, incontinence) Management Discontinuation of the antipsychotic agents Supportive therapy Bromocriptine may be benificial The onset is sudden and recovery may take 5-10 days after discontinuation of the agent Spectrum-based concept of NMS Anticholonergics Lorazepam Lorazepam Lorazepam Dantrolene Bromocriptine Bromocriptine Amantadine Amantadine Hyperprolactinemia Osteoporosis J Clin Psychopharmacol 2007;27:639–661. M receptor blockade Possible therapeutic effect Anticholinergic activity also has a beneficial effect: Counteracts Parkinsonian side effects of antipsychotic drugs Adverse effects All typical APDs have some muscarinic receptor antagonism Constipation Urinary retention Exacerbation of narrow angle glaucoma Sinus tachycardia Blurred vision Antimuscarinic activity varies greatly among antipsychotic drugs 1 receptor blockade Adverse reactions All typical APDs have some 1 adrenergic receptor antagonism Orthostatic hypotension Acute high doses (e.g. psychiatric emergencies) may produce cardiovascular collapse, death Anti- 1 activity varies greatly among antipsychotic drugs Histamine H1 receptor blockade Adverse reactions Somnolence - can be profound Weight gain Antihistamine activity varies greatly among antipsychotic drugs High-potency vs. Low-potency APDs Antipsychotic drug spectrum: High-potency: e.g. Haloperidol High: EPS Low: antimuscarinic, hypotension, sedation Low-potency: e.g. Chlorpromazine Low: EPS High: antimuscarinic, hypotension, sedation Spectrum of Adverse Effects Caused by Antipsychotic Drugs Low Potency High Potency Fewer extrapyramidal reactions (especially thioridazine) More sedation, more postural hypotension Greater effect on the seizure threshold, electrocardiogram (especially thioridazine) More likely skin pigmentation and photosensitivity Occasional cases of cholestatic jaundice Rare cases of agranulocytosis More frequent extrapyramidal reactions Less sedation, less postural hypotension Less effect on the seizure threshold, less cardiovascular toxicity Fewer anticholinergic effects Occasional cases of neuroleptic malignant syndrome Typical (old fashioned) antipsychotic drugs ‘Typical APD’s - 1950’s to present still used due to low cost & in special situations primarily treat positive symptoms imperfect: fail to help many patients’ positive symptoms tend to make negative symptoms worse have many side effects Despite their problems, they revolutionized treatment of this devastating illness Atypical Antipsychotic Agents: Mechanism D2 receptor antagonism 5-HT2A serotonin receptor antagonism May also involve other actions: most of the atypicals also have substantial affinity for other DA, 5HT, adrenergic receptors Role of 5-HT in Nigrostriatal Dopaminergic Synapse Raphe Sunstantia nigra pars compacta Nigrostriatal tract 5-HT 5-HT2A DA D1 D2 Caudate/putamen Normal function Role of 5-HT in Nigrostriatal Dopaminergic Synapse Raphe Sunstantia nigra pars compacta Nigrostriatal tract 5-HT 5-HT2A DA Typical D1 D2 Caudate/putamen EPS Role of 5-HT in Nigrostriatal Dopaminergic Synapse Raphe Sunstantia nigra pars compacta Nigrostriatal tract 5-HT 5-HT2A DA D1 Atypical D2 Caudate/putamen Less EPS What defines ATYPICAL antipsychotics? Atypical APD’s have some of the following: Positive sympt.: increased therapeutic efficacy i.e. in treatment resistant patients Negative sympt : some therapeutic efficacy motivation, social withdrawl, cognition Side effects: generally less than typical drugs Acute EPS: Parkinsonian, Dyskinesias, Akathisia Chronic EPS: Tardive Dyskinesia Endocrine: Hyperprolactinemia Side Effects of Typical vs. Atypical Neuroleptics “Typical” “Atypical” EPS +/++++ 0/+ Akathisia +/++++ 0/+ Cognitive problems +++ 0/++ NMS + 0/+ Tardive dyskinesia +++ +/++ Hyperprolactinemia +++ 0/++ Side-Effects Extrapyramidal side effects (EPS): Risperidone > Olanzapine = Ziprasidone > Quetiapine > Aripiprazole ?=? Clozapine Anticholinergic: Clozapine > Olanzapine > others Hypotension: Clozapine > > Quetiapine, Risperidone > Ziprasidone, Olanzapine, Aripiprazole Side-Effects Sedation Clozapine > > Olanzapine, Quetiapine > Risperidone, Ziprasidone, Aripiprazole Prolactin elevation Risperidone > others Weight gain Clozapine = Olanzapine > Quetiapine, Risperidone > Ziprasidone, Aripiprazole Agranulocytosis: Clozapine Metabolic effects Weight gain over 1 year (kg) aripiprazole 1 amisulpride 1.5 quetiapine 2–3 risperidone 2–3 olanzapine >6 clozapine >6 Clozapine Few EPS, no TD, no elevated prolactin Can cause life threatening Agranulocytosis and risk of seizures at higher doses Is sedating and causes weight gain Greatest efficacy, but highest side effects of atypical antidepressants Side Effects of Clozapine Highly anticholinergic Strong 1 blocker Agranulocytosis - loss of granulocytes As common as 1-2% Usually occurs in first 6 months of therapy Often fatal (to 35%) Adds significantly to financial cost of therapy - $10k/yr Myocarditis As common as 0.2% Occurs mostly in first month of therapy Risperidone Good at low doses, but mimics conventional neuroleptics at higher doses Used with elderly, children and adolescents due to low dose needs Elevates prolactin May improve cognitive functioning in Alzheimer’s and may improve mood in schizophrenia, manic and depressive phases of bipolar Does not block histamine H1 receptors less weight gain Olanzapine Usually no EPS- even at high doses So used with more severe cases Improved mood in bipolar and improved cog. functioning in schizophrenia and dementia Weight gain, moderate sedation, low prolactin, low TD Expensive Quetiapine Virtually no EPS at any dose, no Prolactin Thus good for patients with Parkinson’s and Psychosis Weight gain, may cause cataracts (animal studies) Mood and cog func. Bipolar, Dementia, Schizophrenia Ziprasidone Low EPS, low prolactin No weight gain Antidepressant and anxiolytic properties due to additional inhibition of 5HT and NE reuptake Cog. and Mood: Bipolar, schizophrenia, Dementia Shift in Risk Perception of Antipsychotics Past Areas of Concern Current Medical Realities Diabetes Weight Gain Weight Gain Sedation Tardive Dyskinesia Insulin Resistance CHD Prolactin Hyperlipidemia Prolactin TD Hyperlipidemia Insulin Resistance Sedation Coronary Heart Disease