* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Inflammation
Endomembrane system wikipedia , lookup
Cell encapsulation wikipedia , lookup
Cell growth wikipedia , lookup
Cytokinesis wikipedia , lookup
Programmed cell death wikipedia , lookup
Cell culture wikipedia , lookup
Cellular differentiation wikipedia , lookup
Extracellular matrix wikipedia , lookup
Tissue engineering wikipedia , lookup
Hyaluronic acid wikipedia , lookup
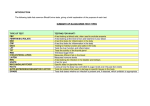
Section 2 Basic Pathologic Changes The basic pathologic changes of inflammation in the site of injury are alteration, exudation, and proliferation. 1. Alteration (1) Definition: The tissues or cells in the inflammatory site become degeneration and/or necrosis. (2) Causes and mechanism: Be damaged by inflammatory factors directly. Local blood circulation disturbance Be affected by inflammatory mediators. (3) Morphology Parenchyma cells: edema, fatty change, necrosis etc. Interstitium: edema, mucoid degeneration, fibrinoid degeneration, necrosis, etc. 2. Vascular changes (hyperemia and exudation) (1) Changes in vascular flow and caliber ① Changes in caliber Transient arteriolar constriction Persistent vasodilatation ② Changes in flow a. Initially rapid as a result of vasodilatation (active hyperemia) b. Slowing and disturbance of axial flow as a result of increased blood viscosity secondary to loss of plasma into the tissue (congestion and edema) 炎症是血液动力学变化模式图 (参照 武忠弼 病理学规划教材第一版 人民卫生出版社,修改) ③ Changes in the endothelium Increased vascular permeability leading to the escape of a protein-rich fluid (exudates) into the interstitium. a. Endothelial cell contraction, or increased transcytosis across the endothelial cytoplasm. b. Direct endothelial injury, resulting in endothelial cell necrosis and detachment c. Leakage from regenerating capillaries (2) Fluid exudate Normally the walls of small blood vessels are freely permeable to water and crystalloids but relatively impermeable to plasma proteins. The formation of protein-rich fluid exudates is facilitated by separation of the intercellular junction of the endothelium. The fluid exude carries into the inflamed area the following important constituents: ① Serum bactericidal factors a. Antibodies which act by opsonising bacteria prior to phagocytosis and by neutralizing exotoxins b. Components of the complement system ② Interferon: a non-specific antiviral agent ③ Fibrinogen which is converted to fibrin. Fibrin is important in providing: a. Cement substance uniting severed tissues b. Scaffold for repair processes c. Barrier to the spread of organisms d. Surface against which phagocytosis of adherent organisms is enhanced ④ Therapeutic agents-antibiotics, antiinflammatory drugs, etc. (3) Leukocyte exudates and phagocytosis ① Leukocytic margination,rolling ② Adhesion:by the binding of adhesion molectures (selections, immunoglobulins, intergrins, mucin-like glycoproteins) ③ Emigrating It refers to the process by which motile white cells migrate out of blood vessels. Although all leukocytes are more or less motile, the most active are the neutrophils and monocytes; the most sluggish are the lymphocytes. While cell emigration is an active, energy-dependent process. * Red blood cell out of blood vessels, called diapedesis, is believed to be passive loss of red blood cells through the points of rupture (blooding). The molecular mechanism of Leukocyte emigration (引自 Robbins Basic Pathology,2003) White cell transmigration It is include following handings: WBC margination WBC adhesion with endothelial surface adhesion molecule WBC transmigration 2-12 minute EM: White cell transmigration (参照武忠弼 病理学规划教材第一版,修改) Leukocyte exudates ④ Chemotaxis Following extravasations, leukocytes emigrate in tissues toward the site of injury by a process called chemotaxis. Exogenous chemo attractants: bacterial products, etc. Endogenous chemo attractants: components of the (LTB4), cytokines, etc. ⑤ Phagocytosis Recognition and attachment of the particle to the surface of the phagocyte→ engulfment→ killing and degradation The mode of Phagocytosis (引自 Robbins Basic Pathology,2003,稍改) Types of leukocyte (inflammatory cells): Leukocytes are out of blood vessels that are known as inflammatory cells. a. Neutrophils: Small phagocytic cell The two types of granules in the cytoplasm: Azurophil granules and specific granules. The first cells to appear in perivascular spaces are the neutrophils. Commonly seen in early stage of inflammation, and acute inflammation, and purulent inflammation. b. Macrophages: Tissue macrophages are derived from blood monocytes that emigrate from blood vessels under influence of chemotactic factors. Commonly seen in later stage of inflammation, chronic inflammation, non-purulent inflammation, and viral, or protozoal, or fungal infections. And macrophages are also related to specific immune response. dusty cell Macrophages could Formation Langhan’s giant cell foamy cell epithelioid cell heart failure cell Multinucleate giant-cells foreign-body giant cell c. Eosinophilia Commonly seen in hypersensitivity reaction and human parasitological infections. d. Lymphocytes and plasma cells Commonly seen in virus infection and chronic inflammation. e. Basophilic and mast cell MacrM 3. Proliferation Proliferate constitution: Endothelium, macrophages, and fibroblasts commonly seen in later stage of inflammation