* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Immunology - Mosaiced.org
Survey
Document related concepts
Duffy antigen system wikipedia , lookup
DNA vaccination wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Immune system wikipedia , lookup
Complement system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adaptive immune system wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
Transcript
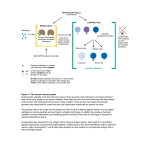
Nikhil Ladwa [email protected] Immunology 1. Host defence overview Define and contrast innate and adaptive/acquired immunity, humoural and cellular immunity. Name the important components of each. Innate immunity: Non antigen specific. This is the rapid, non-specific arm of the immune system, which does not increase in effectiveness on repeated exposure to a repeated pathogen. Elements of innate/ natural immunity to fight disease/ infection include: enzymes, complement, interferons, mucus, acids, phagocytes, natural killer (NK) cells, fever Acquired/ adaptive immunity: The response of antigen-specific lymphocytes to an antigen. It takes several days to develop and results in the proliferation of lymphocytes with the ability to deal with the specific offending antigen, but not any other antigens and with the development of memory cells specific for the antigen in question. Elements include: T lymphocytes, B lymphocytes, Antibody. Humoral immunity: The part of the adaptive immune response mediated by antibodies (antibodies, complement, cytokines) Cellular/ cell-mediated immunity: The part of the adaptive immune response mediated by the production of cytotoxic and helper T cells Define active and passive immunity, antigen and immunogen, primary and secondary immune response. Active immunity is when the body acquires immunity after immunisation with an antigen. Passive immunity is a short-lived immunity acquired by transfer of preformed antibodies, as from mother to foetus across placenta or in vaccination. ANTIGEN: Any molecular feature that an immune system regards as foreign. Antigens stimulate an immune response and this response often includes the production of an antibody specific for the antigen. IMMUNOGEN: This is any substance that generates an immune response. PRIMARY IMMUNE RESPONSE: The part of the adaptive immune response which occurs on initial exposure to an antigen. SECONDARY IMMUNE RESPONSE: This occurs when an individual is exposed to an antigen for a second time. The response is greater and more rapid than the primary immune response and the immunoglobulins produced have higher affinity for antigen. Nikhil Ladwa [email protected] Summarise and give examples of the roles taken in host defence mechanisms by: physical or chemical boundaries, mechnical removal, colonisation resistance, non-specific immune response. PHYSICAL AND CHEMICAL BOUNDARIES: Skin acts as a watertight barrier against infections It releases fatty acids and lysozymes in sweat to combat bacteria/ pathogens Pepsin produced by gut kills pathogens The low pH of the stomach is unstable environment for pathogens Antibacterial peptides are present (paneth cells in intestine) MECHANICAL REMOVAL: Epithelial tight junctions Longitudinal flow of air or fluid (e.g. fluid-flushing? Action of urine in urethra) Movement of mucus by cilia COLONISATION RESISTANCE: Normal flora compete for nutrients/ attachment sites with pathogens. The normal flora are usually resident first so have a survival advantage Production of antibacterial substances by normal flora helps in the fight against pathogens Other non-specific immune responses include avoiding pathogens due to taste, smell, surface environment etc. Outline the principals of adaptive immune response. Macrophage antimicrobial defence mechanisms: Toxic oxygen i.e. O2-, H2O2 Toxic nitrogen oxides i.e. NO Enzymes i.e. lysozyme Antimicrobial peptides i.e. defensins All the above to kill pathogens Chemokines are released. These are- chemoattractive proteins, made by many cell types, cause cell recruitment to inflamed tissues, selective actions on inflammatory subsets, influence the pattern of immunity/ pathology. Adaptive immunity includes phagocytosis, opsonins (membrane around pathogens to encourage engulfment by phagocytes), lymphocytes (T and B), NK killer cells. (make intruders and infected cells die by apoptosis) Nikhil Ladwa [email protected] NK cells can cause: direct binding to microbes, lysis of infected cells, and cytokine secretion. Antibodies released by lymphocytes B cells possess the machinery for immunoglobulin synthesis- antibody secretion. List defence mechanisms operative against major pathogens. Innate defences against bacteria: Surface defences (mechanical and chemical) Antibody opsonisation Activation of complement (alternative pathway) causing lysis/ opsonisation Phagocytosis Trigger release of soluble inflammatory mediators and acute phase proteins by host cells (especially phagocytes) causing fever, opsonisation. Innate defences against viruses: Surface defences (mechanical and chemical) NK cells Interferons Antibody opsonisation (partially effective) Trigger release of soluble inflammatory mediators and acute pahse proteins by host cells (especially phagocytes) causing fever, opsonisation, etc. 2. Immune cells and organs Name the primary and secondary lymphoid organs and briefly differentiate between their functions. THE PRIMARY LYMPHOID ORGANS: Are the major sites of lyphopoiesis. Here lymphoid stem cells differentiate into mature functional lymphocytes. THE THYMUS: Is bilobed in mammals and located in the thorax. Each lobe is organised into lobules with cortex and medulla regions. The cortex contains the immature thymocytes some of which are selected to become mature thymocytes in the medulla. THE BONE MARROW: Bone marrow produces stem cells and Blymphocytes. Those stem cells destined to be T lymphocytes migrate to the thymus throughout life. For B cells, differentiation is centripital with the stem cells under the bone and the most mature phases of the B cell pathway found nearer the centre of the marrow. Nikhil Ladwa [email protected] THE SECONDARY LYMPHOID ORGANS: Provide an environment in which lymphocytes can interact with antigen and with other lymphocytes. They have special vascular adaptations to recruit lymphocytes from the blood. Secondary lymphoid tissue includes the spleen, lymph nodes, and mucosa associated lymphoid tissue. THE SPLEEN: Contains two main types of tissues, the red pulp and the white pulp. The red pulp acts as a general filter and the white pulp is the lymphoid tissues and constitutes the major initiator of responses to blood borne antigens. Around the central arteriole are concentric cuffs of lymphoid tissues = the peri arterial lymphatic sheath. The region nearest the arteriole is a T cell zone. Periodically, there are B cell follicles, either primary or secondary and around this is the marginal zone which seems to be the primary site of entry of B and T cells into the white pulp. HUMAN LYMPH NODES: Are 1- 15 mm across, are round or kidney shaped, lymph arrives at the lymph node through several afferent vessels and leaves through one efferent vessel at the hilus. During passage of lymph through the node there is removal of particulate antigens by the phagocytic cells and then this is transported to the lymphoid regions of the node. The cortex is a B cell area and the paracortex a T cell area. MUCOSAL ASSOCIATED LYMPHOID TISSUE: are aggregates of lymphoid tissue which do not have a tough outer capsule. They are found in the lamina propria, and sub-mucosal areas of the gastrointestinal respiratory and genito-urinary tracts. Typical examples of MALT are tonsils and appendix or Peyer’s patches ( these are organised regions of lymphoid tissue found in the wall of the gut) Draw simple diagrams to illustrate the structure of the thymus, lymph node, spleen, Peyers patch and indicated the changes that occur after stimulation by antigen. The thymus Dividing lymphocyte Lymphoblast Cortex Dense aggregates of cortical small lymphocytes Macrophage Small lymphocytes Medulla Nikhil Ladwa [email protected] B cell area The Spleen Capsule Trabecular vein Trabecular artery T cell area Marginal zone Lymph node Afferent vessels Paracortex Cortex Efferent Vessel Peyers Patch Lumen Gut Wall T Cell B Cell Nikhil Ladwa Outline the re-circulation of lymphocytes. Small B and T lymphocytes which have matured in the bone marrow or thymus and which have not yet encountered antigen are called NAÏVE lymphocytes. These cells circulate constantly from the blood into the secondary lymphoid tissue (the spleen, lymph nodes, mucosal associated lymphoid tissue) and leave the vasculature through a specialised section of the post capillary venule known as the high endothelial venule (HEV) (i.e. they move from the capillary networks into the lymphatic system). They move from the lymph node to the lymphoid vessels and eventually return to the blood via the thoracic duct. In the presence of an infection these cells which recognise the infectious agent are held in the lymphoid tissue where they proliferate and differentiate. Explain the use of CD (cluster of differentiation) markers for distinguishing different immune cell types. [email protected] Clusters of differentiation, are cell surface molecules on white blood cells which are denoted by CD no.s. Some of these cell surface molecules characterise certain subsets of white blood cells i.e. they are ‘phenotypic markers’. E.g. CD8 is expressed on cytotoxic T lymphocytes. However, not all CD antigens are ‘lineage specific’ in this way. Compare and contrast the phenotypic characteristics of T and B lymphocytes and T lymphocyte subsets. T cells: Recognise antigen presented at the cell surface by MHC molecules. Antigen receptor is either or (?) TCR (T cell receptor molecule). All T cells express CD3, T cells express CD4 or CD8. They are produced by the thymus. B cells: Recognise free antigen in the body fluids. Antigen receptor is surface Ig (immunoglobulin) like molecule. They express CD19 and CD20 at surface. They are produced by bone marrow. Give examples of professional antigen presenting cells (APC’s) and state their locations. Cell Langerhans cells (dendritic cells) Follicular dendritic cells B cells Activated macrophages Location Widely spread e.g. skin and mucosal tissue Follicles Lymphoid tissue Lymphoid tissue Presents to T cells B cells T cells T cells Nikhil Ladwa [email protected] 3. Innate immunity Briefly describe the functions of the important phagocytic cells; neutrophils, monocytes/ macrophages. Macrophages: Are less abundant, dispersed throughout the tissues; signal infection by release of soluble mediators (they develop from monocytes) such as cytokines. The macrophage expresses receptors for many bacterial constituents. Bacteria binding to macrophage receptors initiate a response release of cytokine. Macrophages engulf and digest bacteria to which they bind. Phagocytes can be mobile or fixed in a particular location. Phagocytosis involves chemotaxis, adherence, ingestion, digestion, killing. They are also involved with antigen presentation to lyphocytes, where the cells that they phagocytose’s suface antigens are presented on their surface as part of their MHC (major histocompatability complex). Neutrophils: (polymorphonuclear leucocytes), Short lived cells, circulate in blood then migrate into tissues. They are first cells to arrive at a site of tissue damage/ infection. Killing mechanisms of neutrophils: Oxygen independent:: enzymes, lysozyme, hydrolytic enzymes, antimicrobial peptides (defensins). Oxygen dependent: Respiratory burst: toxic metabolites such as superoxide anion, hydrogen peroxide, hydroxyl radical, nitric oxide. Define cytokines and describe their general properties. Cytokines are proteins made by certain cells that affect the behaviour of other cells. Cytokines interact with surface receptors on the surface of target cells. They are the messengers of the immune system. Generally act locally Has biological effects at very low concentrations. Types of cytokine: INTERLEUKINS (IL-x): Communication between leukocytes INTERFERONS (IFN): Antiviral effects CHEMOKINES: Chemotaxis, movement GROWTH FACTORS CYTOTOXIC: Tumor necrosis factor (TNF) Cytokines Inducing Stimulus Biological Effects Cytokine producing cell Target Cell Nikhil Ladwa [email protected] A given cytokine that has different biological effects on different cells is PLEIOTROPIC Cytokines that mediate similar functions are redundant Cytokine synergism occurs when the combined effect is more than additive Antagonism occurs when one cytokine inhibits the effects of another. IL-12 for example directs adaptive immunity and activates NK cells. It is secreted by macrophages. Define complement, list its major functions, and draw a simple diagram of the complement pathways. The complement system is a defensive system consisting of plasma proteins that attack and destroy microbes. The system can be activated in one of two pathways (classical or alternative) both of which are an ordered sequence or cascade of reaction. Both pathways lead to the same events: Inflammation, enhancement of phagocytosis (opsonisation) and bursting of microbes by the MEMBRANE ATTACK COMPLEX. Lectin Pathway Alternative Pathway Classical Pathway MB2 CRP C1 B C4b D P C2a C3b C4a, C3a, C5a Pro-inflammatory molecules C3b is the principal opsonin C5 Cb C7 C8 C9 Membrane Attack Complex cell lysis results The classical pathway- initiated by antigen-antibody complexes The alternate pathway- continuous tick-over production, with full activation upon fixation to pathogen surfaces Nikhil Ladwa The Lectin pathway- antibody-independent activation of classical pathway Classical and alternative pathways converge at C3- meeting point for the adaptive and innate immune systems C3 leads to the final common pathway Ends with the formation of the MEMBRANE ATTACK COMPLEX Major functions of complement: Opsonisation of micro-organisms, to enhance phagocytosis (complement fragments C3b binds to the surface of a microbe and interacts with receptors on phagocytes to promote phagocytosis). Direct lysing of micro-organisms; several complement proteins come together to form a membrane attack complex that inserts into the plasma membrane of the microbe forming large holes which allows fluids to enter causing plasmolysis and then lysis. Promotion of inflammation. Some complement proteins promote this by dilating arteries and causing the release of histamines form mast cells and basophils. Promotes chemotaxis of neutrophils and leukocytes Process Immune Complexes Augments induction of a specific antibody Describe a typical inflammatory response to a localised infection involving recruitment of neutrophils, and phagocytosis and killing of bacteria. [email protected] Cytokines released which encourages chemotaxis (produced by T-cells and macrophages) of neutrophils, lymphocytes, monocytes. Histamine secreted by mast cell *(see diagram in notes) Phagocytosis by activated macrophages Opsonisation of bacteria by complement (complement released) Briefly outline the events involved in a systemic acute phase response. Local inflammatory response may be accompanied by a systemic response, ‘acute phase’ after 1- 2 days Fever, increased production of white blood cells (leukocytosis) and the production of ‘acute-phase’ proteins occur in the liver. This is induced by cytokines The acute phase proteins are: C-reactive protein (CRP): activates complement, level may increase 1000 fold Nikhil Ladwa Mannan binding protein (MBP): opsonin for monocytes, activates complement. Serum Amyloid A Complement Fibrinogen [email protected] Outline the phenotype and functions of natural killer (NK) cells. Natural killer cells are lymphocytes that lack the membrane molecules that identify T and B cells yet have the ability to kill a wide variety of infectious molecules plus certain spontaneous arising tumour cells They are large granulated lymphocytes 10% of the leukocytes in the blood are NK cells NK cells attack cells that display abnormal MHC antigens NK cells achieve cell destruction in at least two ways: by releasing perforins- chemicals which make the plasma membrane of a microbe so leaky that cytolysis occurs by osmosis. Or by binding to the target cell and inflicting damage by direct contact. Cytotoxicity of NK cells activated by the type 1 interferon. NK cells secrete interferon- Are recruited to sites of infection by chemokines 4. Antibodies Describe with the aid of a simple diagram the immunoglobulin molecule, identify the antigen-binding site (Fab) and Fc portions of the molecule. An antibody is a protein that is produced in response to a foreign molecule (antigen) and has the property of binding specifically to the antigen that induced its formation. Antibodies constitute the class of proteins known as immunoglobulins. N Light chain Fab S S N Heavy chain C S S C Fc S S N Constant Fab N Variable Nikhil Ladwa [email protected] Briefly describe the properties of the antigen-binding site. Variable; highly specific Antibodies are said to be bivalent which means flexibility at the hinge (can adopt a T or Y shape) which allows antibodies to simultaneously bind to two different antigens. Distinguish between antibody affinity and antibody avidity. ANTIBODY AFFINITY: Is a measure of the strength of binding between a single binding site of an antibody and its antigen. ANTIBODY AVIDITY: Is the overall strength of binding between antibody and antigen, taking into account the number of binding sites on the antibody and the number of sites on the antigen (antigenic determinats or epitopes) that can be bound. List the immunoglobulin classes and sub-classes in man. Describe their functions and relate these to their individual structure. The classes are G, A, M, E, D. IgG: - Most abundant Ig in blood and tissue spaces and is most important in defence. - IgG neutralises toxins and viruses - It performs a number of functions that are dependent on the nature of its Fc - It binds to bacterium causing opsonisation. Macrophages or neutrophils recognise the Fc (they possess Fc receptors) - It triggers the complement system. - IgG can cross the placenta and protect a newborn child for up to 3 months. IgA: - Makes up 10- 15% of antibodies in blood - Occurs in monomer and dimer form - Important role in seromucous secretions where it binds together with a J chain and secretory component which protect it form degradative enzymes - Secretory IgA can neutralise toxins - By binding to infectious agents it can block their infectivity often by preventing adherence of the agents to the epithelial cell. IgM: - Makes up 5-10% of all antibodies in blood - Is first Ig to be made following contact with an antigen - Its 5 Fab pairs allow it to bind strongly to the surface of bacteria causing agglutination - Like IgG it is adept at activating complement Nikhil Ladwa [email protected] - IgM antibodies also make up the anti-A and anti-B antibodies of the ABO blood typing IgE:- Makes up 0.1% of antibodies in the blood - Mast cells and basophils have a high affinity receptor for the Fc of IgE - When IgE that is bound in this way is cross linked by antigen, degranulation of the cells occurs with release of inflamatory mediators such as histamine. - This process is important in protection against certain parasitic infections but it can be a nuisance giving rise to allergic reactions. IgD: - Makes up some 0.2% of blood antibodies - Found in blood, lymph and on the surface of B cells as antigen receptors - They are involved in the activation of B cells One of the constant heavy domains on the antibodies is a complement binding site which initiates the classical pathway of the complement system.