* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download parasympathetic divisions
Nervous system network models wikipedia , lookup
Premovement neuronal activity wikipedia , lookup
Synaptic gating wikipedia , lookup
Feature detection (nervous system) wikipedia , lookup
Axon guidance wikipedia , lookup
Synaptogenesis wikipedia , lookup
Development of the nervous system wikipedia , lookup
Circumventricular organs wikipedia , lookup
Neuroanatomy wikipedia , lookup
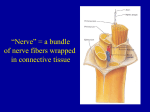
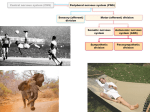
15 PART 1 The Autonomic Nervous System Pages 468-480 PowerPoint® Lecture Presentations prepared by Leslie Hendon University of Alabama, Birmingham © 2014 Pearson Education, Inc. The ANS and Visceral Sensory Neurons • The ANS—a system of motor neurons • Regulates visceral functions • Heart rate • Blood pressure • Digestion • Urination • The ANS is the • General visceral motor division of the PNS © 2014 Pearson Education, Inc. The Autonomic Nervous System and Visceral Sensory Neurons © 2014 Pearson Education, Inc. Figure 15.1 Comparison of Autonomic and Somatic Motor Systems • Somatic motor system • One motor neuron extends from the CNS to skeletal muscle • Axons are well myelinated, conduct impulses rapidly • Autonomic nervous system • Chain of two motor neurons • Preganglionic neuron • Postganglionic neuron • Conduction is slower than somatic nervous system due to • Thinly myelinated or unmyelinated axons • Motor neuron synapses in a ganglion © 2014 Pearson Education, Inc. Figure 15.2 Comparing Somatic Motor and Autonomic Innervation © 2014 Pearson Education, Inc. Autonomic and Somatic Motor Systems SOMATIC NERVOUS SYSTEM Cell bodies in central nervous system Peripheral nervous system Neurotransmitter Effector at effector organs Effect Single neuron from CNS to effector organs ACh Stimulatory Heavily myelinated axon Skeletal muscle SYMPATHETIC NE ACh Unmyelinated postganglionic axon Lightly myelinated Ganglion preganglionic axons Epinephrine and ACh norepinephrine Adrenal medulla PARASYMPATHETIC AUTONOMIC NERVOUS SYSTEM Two-neuron chain from CNS to effector organs Blood vessel ACh Lightly myelinated preganglionic axon © 2014 Pearson Education, Inc. Unmyelinated Ganglion postganglionic axon ACh Smooth muscle (e.g., in gut), glands, cardiac muscle Stimulatory or inhibitory, depending on neurotransmitter and receptors on effector organs Divisions of the Autonomic Nervous System • Sympathetic and parasympathetic divisions • Chains of two motor neurons • Innervate mostly the same structures • Cause opposite effects • Sympathetic division mobilizes the body during extreme situations • Parasympathetic division controls routine maintenance functions © 2014 Pearson Education, Inc. © 2014 Pearson Education, Inc. Divisions of the Autonomic Nervous System • Sympathetic—“fight, flight, or fright” • Activated during EXTREME situations • Sympathetic responses help us respond to dangerous situations • Increase heart rate and breathing rate • Increases blood and oxygen to skeletal muscles • Dilates pupils and airways • Motility of the digestive tract and urinary tracts are inhibited © 2014 Pearson Education, Inc. Divisions of the Autonomic Nervous System • Parasympathetic division • Active when the body is at rest • Concerned with conserving energy • Directs “housekeeping” activities • Heart rate and breathing are at low-normal levels • Gastrointestinal tract digests food • Pupils are constricted © 2014 Pearson Education, Inc. © 2014 Pearson Education, Inc. Anatomical Differences in Sympathetic and Parasympathetic Divisions Parasympathetic • Issue from different regions of the CNS • Sympathetic—also called the thoracolumbar division • Parasympathetic— also called the craniosacral division Sympathetic Eye Brain stem Salivary glands Heart Eye Skin* Cranial Sympathetic ganglia Salivary glands Cervical Lungs Lungs T1 Heart Stomach Thoracic Stomach Pancreas Pancreas L1 Liver and gallbladder Lumbar Adrenal gland Liver and gallbladder Bladder Bladder Genitals Genitals © 2014 Pearson Education, Inc. Sacral Figure 15.3 Anatomical Differences in Sympathetic and Parasympathetic Divisions • Length of postganglionic fibers • Sympathetic—long postganglionic fibers • Parasympathetic—short postganglionic fibers • Branching of axons • Sympathetic axons—highly branched • Influences many organs • Parasympathetic axons—few branches • Localized effect © 2014 Pearson Education, Inc. Biochemical Differences in Sympathetic and Parasympathetic Divisions • Neurotransmitter released by postganglionic axons • Sympathetic • Most release norepinephrine (adrenergic) • Parasympathetic • Release acetylcholine (cholinergic) © 2014 Pearson Education, Inc. Parasympathetic and Sympathetic Divisions © 2014 Pearson Education, Inc. Table 15.1 The Parasympathetic Division • Cranial outflow • Comes from the brain • Innervates • Organs of the head, neck, thorax, and abdomen • Sacral outflow • Innervation supplies • Remaining abdominal and pelvic organs © 2014 Pearson Education, Inc. Cranial Outflow (Parasympathetic) • Preganglionic fibers run via • Oculomotor nerve (III) • Facial nerve (VII) • Glossopharyngeal nerve (IX) • Vagus nerve (X) • Cell bodies of preganglionic neurons located in cranial nerve nuclei in the brain stem © 2014 Pearson Education, Inc. The Parasympathetic Division Ciliary ganglion CN III CN VII CN IX CN X Eye Lacrimal gland Nasal mucosa Pterygopalatine ganglion Submandibular ganglion Otic ganglion Submandibular and sublingual glands Parotid gland Heart Cardiac and pulmonary plexuses Lung Celiac plexus Liver and gallbladder Stomach Pancreas S2 Large intestine S4 Small intestine Pelvic splanchnic nerves Inferior hypogastric plexus Rectum Urinary bladder and ureters Genitalia (penis, clitoris, and vagina) Preganglionic Postganglionic © 2014 Pearson Education, Inc. CN Cranial nerve Figure 15.4 Outflow via the Oculomotor Nerve (III) • Parasympathetic fibers innervate smooth muscles in the eye • Cause pupil constriction • Preganglionic cell bodies • Located in the oculomotor nucleus in the midbrain • Post ganglionic cell bodies • Lie in the ciliary ganglion © 2014 Pearson Education, Inc. Outflow via the Facial Nerve (VII) • Parasympathetic fibers stimulate secretion of glands in the head • Lacrimal nucleus • Located in the pons • Synapse in the pterygopalatine ganglion • Superior salivatory nucleus • Located in the pons • Synapse in the submandibular ganglion © 2014 Pearson Education, Inc. The Parasympathetic Division Ciliary ganglion CN III CN VII CN IX CN X Eye Lacrimal gland Nasal mucosa Pterygopalatine ganglion Submandibular ganglion Otic ganglion Submandibular and sublingual glands Parotid gland Heart Cardiac and pulmonary plexuses Lung Celiac plexus Liver and gallbladder Stomach Pancreas S2 Large intestine S4 Small intestine Pelvic splanchnic nerves Inferior hypogastric plexus Rectum Urinary bladder and ureters Genitalia (penis, clitoris, and vagina) Preganglionic Postganglionic © 2014 Pearson Education, Inc. CN Cranial nerve Figure 15.4 Outflow via the Glossopharyngeal Nerve (IX) • Parasympathetic fibers • Stimulate secretion of parotid gland • Inferior salivatory nucleus—located in the medulla • Synapse in the otic ganglion © 2014 Pearson Education, Inc. Outflow via the Vagus Nerve (X) • Fibers innervate visceral organs of the thorax and most of the abdomen • Stimulates: • Digestion, reduction in heart rate, and reduction in blood pressure • Preganglionic cell bodies • Located in dorsal motor nucleus in the medulla • Postganglionic neurons • Confined within the walls of organs being innervated • Cell bodies form intramural ganglia © 2014 Pearson Education, Inc. The Parasympathetic Division Ciliary ganglion CN III CN VII CN IX CN X Eye Lacrimal gland Nasal mucosa Pterygopalatine ganglion Submandibular ganglion Otic ganglion Submandibular and sublingual glands Parotid gland Heart Cardiac and pulmonary plexuses Lung Celiac plexus Liver and gallbladder Stomach Pancreas S2 Large intestine S4 Small intestine Pelvic splanchnic nerves Inferior hypogastric plexus Rectum Urinary bladder and ureters Genitalia (penis, clitoris, and vagina) Preganglionic Postganglionic © 2014 Pearson Education, Inc. CN Cranial nerve Figure 15.4 Path of the Vagus Nerve • Sends branches through • Autonomic nerve plexuses • Cardiac plexus • Pulmonary plexus • Esophageal plexus • Celiac plexus • Superior mesenteric plexus © 2014 Pearson Education, Inc. Autonomic nerves, plexuses and ganglia Superior cervical ganglion Middle cervical ganglion Stellate ganglion Sympathetic cardiac nerves Aortic arch Sympathetic trunk ganglia Esophagus Thoracic splanchnic nerves Adrenal (suprarenal) gland Kidney Lumbar and sacral splanchnic nerves © 2014 Pearson Education, Inc. Left vagus nerve Cardiac branches of the vagus Trachea Thoracic spinal nerves (ventral rami) Cardiac plexus Pulmonary plexus on the bronchus Aorta Vagus nerve Esophageal plexus Diaphragm Stomach with vagus nerve Celiac ganglion and plexus Superior mesenteric ganglion and plexus Aortic plexus Inferior mesenteric ganglion and plexus Superior hypogastric plexus Inferior hypogastric (pelvic) plexus Pelvic sympathetic trunk Figure 15.5 Sacral Outflow • Emerges from S2–S4 • Innervates organs of the pelvis and lower abdomen • Preganglionic cell bodies • Located in visceral motor region of spinal gray matter • Axons run in ventral roots to ventral rami © 2014 Pearson Education, Inc. Gray Matter of the Spinal Cord and Spinal Roots Dorsal root (sensory) Dorsal horn (interneurons) Dorsal root ganglion SS Somatic sensory neuron Visceral sensory neuron Visceral motor neuron Somatic motor neuron VS VM SM Spinal nerve Ventral root (motor) Ventral horn (motor neurons) Interneurons receiving input from somatic sensory neurons Interneurons receiving input from visceral sensory neurons Visceral motor (autonomic) neurons Somatic motor neurons © 2014 Pearson Education, Inc. Figure 13.27 Anatomy of the Spinal Cord Dorsal funiculus White matter Ventral funiculus Lateral funiculus Dorsal median sulcus Gray commissure Dorsal horn Gray Ventral horn matter Lateral horn Dorsal root ganglion Spinal nerve Dorsal root (fans out into dorsal rootlets) Ventral root (derived from several ventral rootlets) Central canal Ventral median fissure Pia mater Arachnoid mater Spinal dura mater (b) The spinal cord and its meningeal coverings © 2014 Pearson Education, Inc. Figure 13.26 The Sympathetic Division • Basic organization • Issues from T1–L2 • Preganglionic fibers form the lateral gray horn • Supplies visceral organs and structures of superficial body regions • Contains more ganglia than the parasympathetic division; sympathetic trunk ganglia & collateral ganglia © 2014 Pearson Education, Inc. Sympathetic Trunk Ganglia • Located on both sides of the vertebral column • Linked by short nerves into sympathetic trunks • Sympathetic trunk ganglia are also called • Chain ganglia • Joined to ventral rami by white and gray rami communicantes © 2014 Pearson Education, Inc. Sympathetic Trunk Ganglia Spinal cord Lateral horn (visceral motor zone) Dorsal root Dorsal root Ventral root Dorsal root ganglion Rib Dorsal ramus of spinal nerve Ventral ramus of spinal nerve Gray ramus communicans White ramus communicans Sympathetic trunk ganglion Sympathetic trunk Ventral ramus of spinal nerve Gray ramus communicans White ramus communicans Thoracic splanchnic nerves (a) Location of the sympathetic trunk Skin (arrector pili muscles and sweat glands) Ventral root Sympathetic trunk ganglion Sympathetic trunk 1 Synapse at the same level To effector Blood vessels Splanchnic nerve Collateral ganglion (such as the celiac) Skin (arrector pili muscles and sweat glands) Target organ in abdomen (e.g., intestine) To effector Blood vessels 2 Synapse at a higher or lower level 3 Synapse in a distant collateral ganglion anterior to the vertebral column (b) Three pathways of sympathetic innervation © 2014 Pearson Education, Inc. Figures 15.6 & 15.7 Sympathetic Pathways • Preganglionic axons follow one of three pathways 1. Synapes with a postganglionic neuron at the same level and exit on a spinal nerve at that level 2. Axon ascends or descends in the sympathetic trunk to synapse in another ganglion 3. Axon passes through the sympathetic trunk and exits on a splanchnic nerve © 2014 Pearson Education, Inc. Sympathetic Pathways to Organs Eye Lacrimal gland Nasal mucosa Pons Sympathetic trunk (chain) ganglia Superior cervical ganglion Middle cervical ganglion Inferior cervical ganglion T1 Blood vessels; skin (arrector pili muscles and sweat glands) Salivary glands Heart Cardiac and pulmonary plexuses Lung Greater splanchnic nerve Lesser splanchnic nerve Celiac ganglion L2 Liver and gallbladder Stomach White rami communicantes Superior mesenteric ganglion Spleen Adrenal medulla Kidney Sacral splanchnic nerves Lumbar splanchnic nerves Inferior mesenteric ganglion Small intestine Large intestine Rectum Preganglionic Postganglionic © 2014 Pearson Education, Inc. Genitalia (uterus, vagina, and penis) and urinary bladder Figure 15.8 The Role of the Adrenal Medulla in the Sympathetic Division • Major organ of the sympathetic nervous system • Constitutes largest sympathetic ganglia • Secretes great quantities of norepinephrine and adrenaline • Stimulated to secrete by preganglionic sympathetic fibers © 2014 Pearson Education, Inc. The Adrenal Medulla Sympathetic trunk Spinal cord: Ventral T8–L1 root Thoracic splanchnic nerves Kidney Adrenal medulla © 2014 Pearson Education, Inc. Adrenal gland Epinephrine and norepinephrine Adrenal medulla cells Capillary Figure 15.9 © 2014 Pearson Education, Inc. Table 15.2 (1 of 3) © 2014 Pearson Education, Inc. Table 15.2 (2 of 3) © 2014 Pearson Education, Inc. Table 15.2 (3 of 3)