* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download For lecture notes click here
Lipid signaling wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Signal transduction wikipedia , lookup
Peptide synthesis wikipedia , lookup
Mitochondrion wikipedia , lookup
Point mutation wikipedia , lookup
Photosynthesis wikipedia , lookup
Microbial metabolism wikipedia , lookup
Light-dependent reactions wikipedia , lookup
Butyric acid wikipedia , lookup
Proteolysis wikipedia , lookup
Genetic code wikipedia , lookup
Metalloprotein wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Photosynthetic reaction centre wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Biosynthesis wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
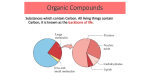
Introduction Cells break down organic molecules to obtain energy energy used to generate ATP cells need oxygen and nutrients for this Oxygen absorbed at lungs; nutrients obtained from digestive tract. energy released inside the cell supports: growth, cell division, contraction, secretion, and other functions metabolism - chemical reactions at cellular level to provide energy and maintain homeostasis for: 1. metabolic turnover 2. growth and cell division 3. special processes, such as secretion, contraction, and action potential propagation. Catabolism breaks down organic substrates, releasing energy proceeds in a series of steps. First step is breakdown of large molecules to small in cytosol,(litlle energy produced) simple molecules absorbed and processed by mitochondria(release high energy) The ATP produced by mitochondria provides energy to support anabolism Anabolism Anabolism is the formation of new chemical bonds. Cells synthesize new organic components for four basic reasons: 1. To perform structural maintenance or repairs 2. To support growth 3. To produce secretions 4. To build nutrient reserves Mitochandria nutrient pool is substrates for both catabolism and anabolism Mitochondria are important, -they provide the energy that supports cellular operations cell feeds mitochondria nutrient, and in return gets ATP mitochondria accept only specific organic molecules for energy production organic nutrients are broken down into smaller fragments acceptable to mitochondria mitochondria break fragments to carbon dioxide, water, and ATP This mitochondrial activity involves two pathways: 1. TCA cycle 2. electron transport system. CHO Metabolism Most cells generate ATP and other high-energy compounds by breaking down carbohydrates, C6H12O6 + 6 O2 6 CO2 + 6 H2O glucose oxygen carbon dioxide water breakdown occurs in a series of steps, several of steps convert ADP to ATP complete catabolism of one molecule glucose provide 36 ATP most of ATP produced in mitochondria, but first steps take place in cytosol ATP production in mitochondria is called aerobic metabolism or cellular respiration GLYCOLYSIS Glycolysis is the breakdown of glucose to pyruvic acid six-carbon glucose (C6H12O6) is broken into two three-carbon molecules of pyruvic acid (CH3 — CO — COOH). each pyruvic acid loses a hydro-gen ion and exists as the negatively charged ion CH3 — CO — COO–. Glycolysis requires: (1) glucose (2) enzymes, (3) ATP and ADP, (4) inorganic phosphates, and (5) NAD (nicotinamide adenine dinucleotide), a coenzyme that removes hydrogen atoms during one of the enzymatic reactions Glycolysis begins when an enzyme phosphorylates glucose creating glucose-6-phosphate this step "costs" cell one ATP, but has two important results: 1. traps glucose within the cell, 2. prepares glucose for further biochemical reactions. second phosphorylation occurs in cytosol before six-carbon chain is broken to 2 three-carbon fragments ATP produced when these fragments are converted to pyruvic acid Glucose + 2 NAD + 2 ADP + 2 Pi 2 Pyruvic acid + 2 NADH + 2 ATP (6-carbon) (3-carbon) MITOCHONDRIAL ATP PRODUCTION mitochondria absorb pyruvic acid and break them down hydrogen atoms of each pyruvic acid molecule are removed by coenzymes and will be the source energy gain for the cell. carbon and oxygen atoms are released as carbon dioxide, (called decarboxylation) Each mitochondrion has two membranes: 1. outer membrane has large-diameter pores 2. inner membrane with carrier protein In mitochondrion, pyruvic acid participates in a complex reaction involving NAD and another coenzyme, coenzyme A reaction yields one molecule of carbon dioxide, one of NADH, and one of acetyl-CoA. acetyl group is transferred from CoA to oxaloacetic acid, producing citric acid. TCA tricarboxylic acid (TCA) cycle/Citric Acid Cycle/ Kerb Cycle formation of citric acid from acetyl-CoA and oxaloacetic acid is the first step in TCA the cycle removes H+ from organic molecules and transfer them to coenzymes in TCA cycle, the two-carbon acetyl group carried by CoA is attached to a four-carbon oxaloacetic acid molecule to make the six-carbon compound citric acid Coenzyme A is released and can thus bind another acetyl group TCA cycle removes two carbon atoms, regenerating the four-carbon chain immediate energy benefit of TCA cycle is formation of one GTP (guanosine triphosphate) formation of GTP from GDP in TCA cycle is an example of substrate-level phosphorylation Oxidative phosphorylation generation of ATP within mitochondria in a reaction sequence that requires coenzymes and consumes oxygen This process produces over 90 percent of the ATP used by our cells Oxidation, Reduction, and Energy Transfer enzymatic steps of oxidative phosphorylation involve oxidation and reduction The loss of electrons is oxidation; the acceptance of electrons is reduction electron donor is oxidized (loss energy) and electron recipient reduced (gain energy) reduced molecule does not acquire all the energy released by oxidized molecule - released as heat, and formation of ATP coenzyme acts as intermediary that accepts electrons from one molecule and transfer it to another In TCA NAD and FAD remove hydrogen atoms from organic substrates NADH and FADH2, the reduced forms of NAD and FAD, transfer their hydrogen to other coenzymes protons are released, and the electrons, which carry the chemical energy, enter a sequence of oxidation– reduction reactions The Electron Transport System electron transport system (ETS) or respiratory chain, is a sequence of proteins called cytochromes Each cytochrome has: 1. a protein - embedded in the inner membrane of a mitochondrion, surrounds the pigment complex, which contains a metal io 2. a pigment STEP1: coenzyme strips a pair of hydrogen atoms from a substrate molecule. STEP2: NADH and FADH2 deliver hydrogen atoms to coenzymes embedded in the inner membrane of a mitochondrion. STEP3: Coenzyme Q accepts hydrogen atoms from FMNH2 and FADH2 and passes electrons to cytochrome b. STEP4: Electrons are passed along the electron transport system, losing energy in a series of small steps. The sequence is cytochrome b to c to a to a3. STEP5: At the end of the ETS, an oxygen atom accepts the electrons, creating an oxygen ion (O–). This ion has a very strong affinity for hydrogen ions (H+); water is produced. ATP Generation For each pair of electrons removed by NAD from a substrate in the TCA cycle, six hydrogen ions are pumped across the inner membrane of the mitochondrion and into the intermembrane space Their reentry into the matrix provides the energy to generate three molecules of ATP For each pair of electrons removed by FAD from a substrate in the TCA cycle, four hydrogen ions are pumped across the inner membrane and into the intermembrane space Their reentry into the matrix provides the energy to generate two molecules of ATP. Oxidative phosphorylation is the most important mechanism for the generation of ATP Cells obtain oxygen by diffusion from the extracellular fluid. If the supply of oxygen is cut off, mitochondrial ATP production will cease, because reduced cytochrome a3 will have no acceptor for its electrons Summery Glycolysis. During glycolysis, the cell gains 2 molecules of ATP directly for each glucose molecule broken down anaerobically to pyruvic acid. Two molecules of NADH are also produced. In most cells, electrons are passed from NADH to FAD by means of an intermediate in the intermembrane space and then to CoQ and the electron transport system. This sequence of events ultimately provides an additional 4 ATP molecules. The electron transport system. The TCA cycle breaks down the 2 pyruvic acid molecules, transferring hydrogen atoms to NADH and FADH2. These coenzymes provide electrons to the ETS; each of the 8 molecules of NADH yields 3 ATP and 1 water molecule; each of the 2 FADH2 molecules yields 2 ATP and 1 water molecule. Thus the shuffling from the TCA cycle to the ETS yields 28 molecules of ATP. The TCA cycle. Each of the two revolutions of the TCA cycle required to break down both pyruvic acid molecules completely yields 1 molecule of ATP by way of GTP. This cycling provides an additional gain of 2 molecules of ATP. Summing up, for each glucose molecule processed, the cell gains 36 molecules of ATP: two from glycolysis, 4 from the NADH generated in glycolysis, 2 from the TCA cycle (by means of GTP) and a total of 28 from the ETS. Your cardiac muscle cells and liver cells are able to gain an additional 2 ATP molecules for each glucose molecule broken down. This gain is accomplished by increasing the energy yield from the NADH generated during glycolysis from 4 ATP to 6 ATP molecules GLUCONEOGENESIS Pyruvic acid or other three-carbon molecules can be used to synthesize glucose cell can create glucose from other carbohydrates, lactic acid, glycerol, or some amino acids Gluconeogenesis is the synthesis of glucose from noncarbohydrate precursors, such as lactic acid, glycerol, or amino acids Fatty acids and many amino acids cannot be used for gluconeogenesis, because their catabolic pathways produce acetyl-CoA the liver and in skeletal muscle, glucose molecules are stored as glycogen. The process of glycogen formation from glucose is known as glycogenesis Lipid Metabolism Like carbohydrates, lipid molecules contain carbon, hydrogen, and oxygen, but the atoms are present in different proportions During lipid catabolism, or lipolysis, lipids are broken down into pieces that can be either converted to pyruvic acid or channeled directly into the TCA cycle triglyceride is first split into its component parts by hydrolysis This step yields one molecule of glycerol and three fatty acid molecules Glycerol enters the TCA cycle after enzymes in the cytosol convert it to pyruvic acid Beta-Oxidation Fatty acid molecules are broken down into two-carbon fragments in a sequence of reactions known as betaoxidation This process occurs inside mitochondria, so the carbon chains can enter the TCA cycle immediately Each step generates molecules of acetyl-CoA, NADH, and FADH2, leaving a shorter carbon chain bound to coenzyme A For each two-carbon fragment removed from the fatty acid, the cell gains 12 ATP molecules from the processing of acetyl-CoA in the TCA cycle, plus 5 ATP molecules from the NADH and FADH2 The cell can therefore gain 144 ATP molecules from the breakdown of one 18-carbon fatty acid molecule Lipids and Energy Production important as an energy reserve, because they can provide large amounts of ATP They are insoluble, so lipids can be stored in compact droplets in the cytosol (This storage method saves space, but when the lipid droplets are large, it is difficult for water-soluble enzymes to get at them. Lipid reserves are therefore more difficult to access than carbohydrate reserves) cells with modest energy demands can shift to lipid-based energy production when glucose supplies are limited LIPID SYNTHESIS The synthesis of lipids is known as lipogenesis synthesis of most other types of lipids, including nonessential fatty acids and steroids, begins with acetylCoA. Lipogenesis can use almost any organic substrate, because lipids, amino acids, and carbohydrates can be converted to acetyl-CoA. Fatty acid synthesis involves a reaction sequence quite distinct from that of beta-oxidation Your cells cannot build every fatty acid they can break down. Linoleic acid and linolenic acid, both 18carbon unsaturated fatty acids, cannot be synthesized (called essential FA, generated by plants) LIPID TRANSPORT AND DISTRIBUTION Like glucose, lipids are needed throughout the body: to maintain their cell membranes, steroid hormones most lipids are not soluble in water, special transport mechanisms are required they circulate through the bloodstream as lipoproteins (lipid–protein complexes that contain large insoluble glycerides and cholesterol with a superficial coating of phospholipids and proteins) The proteins and phospholipids make the entire complex soluble Lipoproteins are usually classified according to size and the relative proportions of lipid versus protein The following five major groups of lipoproteins are recognized: 1. Chylomicrons. Roughly 95 percent of the weight of a chylomicron consists of triglycerides. Chylomicrons are the largest lipoproteins, ranging in diameter from 0.03 to 0.5 µm. They are produced by intestinal epithelial cells. Chylomicrons carry ab-sorbed lipids from the intestinal tract to the bloodstream. The other lipoproteins shuttle lipids among various tissues. The liver is the primary source of all other types of lipoproteins. 2. Very low-density lipoproteins (VLDLs). Very low-density lipoproteins contain triglycerides manufactured by the liver plus small amounts of phospholipids and cholesterol. The primary function of VLDLs is to transport these triglycerides to peripheral tissues. The VLDLs range in diameter from 25 to 75 nm (0.025– 0.075 µm). 3. Intermediate-density lipoproteins (IDLs). Intermediate-density lipoproteins are intermediate in size and lipid composition between VLDLs and low-density lipoproteins (LDLs). They contain smaller amounts of triglycerides than do VLDLs and relatively more phospholipids and cholesterol than do LDLs. 4. Low-density lipoproteins (LDLs). Low-density lipoproteins contain cholesterol, lesser amounts of phospholipids, and very few triglycerides. These lipoproteins, which are about 25 nm in diameter, deliver cholesterol to peripheral tissues. Because this cholesterol may wind up in arterial plaques, LDL cholesterol is often called "bad cholesterol." 5. High-density lipoproteins (HDLs). High-density lipoproteins, about 10 nm in diameter, have roughly equal amounts of lipid and protein. The lipids are largely cholesterol and phospholipids. The primary function of HDLs is transporting excess cholesterol from peripheral tissues back to the liver for storage or excretion in the bile. Because HDL cholesterol is returning from peripheral tissues and will not cause circulatory problems, it is called "good cholesterol." Actually, applying the terms good and bad to cholesterol can be misleading, for cholesterol metabolism is complex and variable. (For more details, see the discussion "Dietary Fats and Cholesterol") The liver controls the distribution of other lipoproteins in following steps: STEP 1: Liver cells synthesize VLDLs for discharge into the bloodstream. STEP 2: In peripheral capillaries, lipoprotein lipase removes many of the triglycerides from VLDLs, leaving IDLs; the triglycerides are broken down into fatty acids and monoglycerides. STEP 3: When IDLs reach the liver, additional triglycerides are removed and the protein content is altered. This process creates LDLs, which then returns to peripheral tissues to deliver cholesterol. STEP 4: LDLs leave the bloodstream through capillary pores or cross the endothelium by vesicular transport. STEP 5: Once in peripheral tissues, the LDLs are absorbed by means of receptor-mediated endocytosis. The amino acids and cholesterol then enter the cytoplasm. STEP 6: The cholesterol not used by the cell in the synthesis of lipid membranes or other products diffuses out of the cell. STEP 7: The cholesterol then reenters the bloodstream, where it is absorbed by HDLs and returned to the liver. STEP 8: In the liver, the HDLs are absorbed and their cholesterol is extracted. Some of the cholesterol recovered will be used in the synthesis of LDLs, and the rest will be excreted in bile salts. STEP 9: The HDLs stripped of their cholesterol are released into the bloodstream to travel into peripheral tissues and absorb additional cholesterol. Protein Metabolism: The body can synthesize 100,000 to 140,000 different proteins with various forms, functions, and structures each protein contains some combination of the same 20 amino acids Under normal conditions, cellular proteins are continuously recycled Peptide bonds are broken, and the free amino acids are used in new proteins. This recycling occurs in the cytosol. If other energy sources are inadequate, mitochondria can break down amino acids in the TCA cycle to generate ATP The first step in amino acid catabolism is the removal of the amino group (—NH2). This process requires a coenzyme derivative of vitamin B6 (pyridoxine). The amino group is removed by transamination or deamination. Transamination attaches the amino group of an amino acid to a keto acid A keto acid resembles an amino acid except that the second carbon binds an oxygen atom rather than an amino group Transamination converts the keto acid into an amino acid that can enter the cytosol and be used for protein synthesis reactions enable a cell to synthesize many of the amino acids needed for protein synthesis Deamination preparing an amino acid for breakdown in the TCA cycle Deamination is the removal of an amino group and a hydrogen atom in a reaction that generates an ammonia (NH3) molecule or an ammonium ion (NH4+). Ammonia molecules are highly toxic, even in low concentrations. Your liver, the primary site of deamination, has the enzymes needed to deal with the problem of ammonia generation. Liver cells convert the ammonia to urea When glucose supplies are low and lipid reserves are inadequate, liver cells break down internal proteinsto provide ATP Proteins and ATP Production Three factors make protein catabolism an impractical source of quick energy: 1. Proteins are more difficult to break apart than are complex carbohydrates or lipids. 2. One of the byproducts, ammonia, is a toxin that can damage cells. 3. Proteins form the most important structural and functional components of any cell. Extensive protein catabolism therefore threatens homeostasis at the cellular and systems levels. PROTEIN SYNTHESIS body can synthesize roughly half of the various amino acids needed to build proteins are 10 essential amino acids. You cannot synthesize eight of them (isoleucine, leucine, lysine, threonine, tryptophan, phenylalanine, valine, and methionine); the other two (arginine and histidine) can be synthesized but in amounts that are insufficient for growing children Nuclic Acid Metabloism Cells contain both DNA and RNA RNA in the cell is involved in protein synthesis RNA molecules are broken down and replaced regularly. In the breakdown of RNA, the bonds between nucleotides are broken and the molecule is disassembled into individual nucleotides. The nucleotides are usually recycled into new nucleic acids. However, they can be catabolized to simple sugars and nitrogenous bases RNA catabolism makes a relatively insignificant contribution to the total energy budget of the cell Most cells synthesize RNA, but DNA synthesis occurs only in cells preparing for mitosis and cell division Metabolic Interactions From a metabolic standpoint, we can consider the body in terms of five distinctive components: the liver, adipose tissue, skeletal muscle, neural tissue, and other peripheral tissues: 1. The liver. The liver is the focal point of metabolic regulation and control. Liver cells contain a great diversity of enzymes, and they can break down or synthesize most of the carbohydrates, lipids, and amino acids needed by other body cells. Liver cells have an extensive circulatory supply, so they are in an excellent position to monitor and adjust the nutrient composition of circulating blood. The liver also contains significant energy reserves in the form of glycogen deposits. 2. Adipose tissue. Adipose tissue stores lipids, primarily as triglycerides. Adipocytes are located in many areas; in previous chapters, we noted the presence of fat cells in areolar tissue, in mesenteries, within red and yellow marrows, in the epicardium, and around the eyes. 3. Skeletal muscle. Skeletal muscle accounts for almost half of an individual’s body weight, and these cells maintain substantial glycogen reserves. In addition, their contractile proteins can be broken down and the amino acids used as an energy source if other nutrients are unavailable. 4. Neural tissue. Neural tissue has a high demand for energy, but the cells do not maintain reserves of carbohydrates, lipids, or proteins. Neurons must be provided with a reliable supply of glucose, because they are generally unable to metabolize other molecules. If blood glucose becomes too low, neural tissue in the central nervous system cannot continue to function, and the individual becomes unconscious. 5. Other peripheral tissues. Other peripheral tissues do not maintain large metabolic reserves, but they are able to metabolize glucose, fatty acids, or other substrates. Their preferred source of energy varies with the instructions provided by the endocrine system. THE ABSORPTIVE STATE The Liver - regulates the levels of glucose and amino acids in the blood arriving in the hepatic portal vein before that blood reaches the inferior vena cava Adipose Tissue - During the absorptive state, adipocytes remove fatty acids and glycerol from the bloodstream, Lipids continue to be removed from the blood for 4–6 hours after you have eaten a fatty meal. Over this period, the presence of chylomicrons may give the plasma a milky appearance, a characteristic called lipemia. Skeletal Muscle, Neural Tissue, and Other Peripheral Tissues - When blood glucose and amino acid concentrations are elevated, insulin is released from the pancreatic islets, and all tissues increase their rates of absorption and utilization. Glucose is catabolized for energy, and the amino acids are used to build proteins. THE POSTABSORPTIVE STATE period when nutrient absorption is not under way and your body must rely on internal energy reserves to continue meeting its energy demands Metabolic activity in the postabsorptive state is focused on the mobilization of energy reserves and the maintenance of normal blood glucose levels These activities are coordinated by several hormones, including glucagon, epinephrine, glucocorticoids, and growth hormone The Liver As the absorptive state ends, your intestinal cells stop providing glucose to the portal circulation First glucose from the blood is used, when blood glucose levels begin to decline below 80 mg/dl, breaki down of glycogen (75-100g) to glucos starts (glucagons, epinephrine). This glycogenolysis occurs in response to a rise in circulating levels of glucagon and epinephrine. (As glycogen reserves decline and plasma glucose levels fall to about 70 mg/dl, liver cells begin to make glucose in an attempt to stabilize blood glucose levels. The shift from glycogenolysis to gluconeogenesis occurs under stimulation by glucocorticoids, steroid hormones from the adrenal cortex) Gluconeogenesis iver cells synthesize glucose molecules from smaller carbon fragments any carbon fragment that can be converted to pyruvic acid or one of the three-carbon compounds involved in glycolysis in the cytoplasm can be used to synthesize glucose Utilization of Lipids Some of the acetyl-CoA molecules deliver their two-carbon acetyl fragments to the TCA cycle, where they are broken down. The ATP generated can then be used to support gluconeogenesis. In addition, some of the molecules of acetyl-CoA are converted to special compounds that can be utilized by peripheral tissues. These compounds, called ketone bodies, are organic acids that are also produced during the catabolism of amino acids. Utilization of Amino Acids Before an amino acid can be used for either gluconeogenesis or energy production by means of breakdown in the TCA cycle, the amino group (—NH2) must be removed After deamination, some amino acids can be converted to molecules of pyruvic acid or to one of the intermediary molecules of the TCA cycle Other amino acids—including most of the essential amino acids—can be converted only to acetyl-CoA and must be either broken down further or converted to ketone bodies. Ketone Bodies During the postabsorptive state, liver cells conserve glucose and break down lipids and amino acids. Both lipid catabolism and amino acid catabolism generate acetyl-CoA. As the concentration of acetyl-CoA rises, ketone bodies begin to form. There are three ketone bodies 1. acetoacetate, 2. acetone, 3. betahydroxybutyrate ketone bodies, diffuse through the cytoplasm and into the general circulation. Cells in peripheral tissues then absorb the ketone bodies and reconvert them to acetyl-CoA for introduction into the TCA cycle. Summery during the postabsorptive state your liver attempts to stabilize blood glucose concentrations, first by the breakdown of glycogen reserves and later by gluconeogenesis. Over the remainder of the postabsorptive state, the combination of lipid and amino acid catabolism provides the necessary ATP and generates large quantities of ketone bodies that diffuse into the bloodstream. VITAMINS Vitamins are assigned to either of two groups 1. Fat-Soluble Vitamins (A, D, E, and K) - Because they dissolve in lipids, fat-soluble vitamins normally diffuse into cell membranes and other lipids in the body, including the lipid inclusions in the liver and adipose tissue 2. Water-Soluble Vitamins - Most of the water-soluble vitamins are components of coenzymes (e.g. NAD is derived from niacin, FAD from vitamin B2 (riboflavin), and coenzyme A from vitamin B5 (pantothenic acid). Water-soluble vitamins are rapidly exchanged between the fluid compartments of the digestive tract and the circulating blood, and excessive amounts are readily excreted in urine