* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download anatomy of the skin lecture1
Cell membrane wikipedia , lookup
Chromatophore wikipedia , lookup
Cell growth wikipedia , lookup
Tissue engineering wikipedia , lookup
Cytokinesis wikipedia , lookup
Endomembrane system wikipedia , lookup
Extracellular matrix wikipedia , lookup
Cell culture wikipedia , lookup
Cell encapsulation wikipedia , lookup
Cellular differentiation wikipedia , lookup
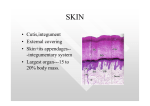
Anatomy of the skin The skin is the interface between the human & his environment, it's the largest organ in the body, weighing an average of 4 kg & covering an area of 2 m2. It is composed of 3 main layers: 1)The epidermis: is the outermost layer, formed by an ordered arrangement of cells called keratinocytes whose basic function is to synthesize keratin, a filamentous protein that serves a protective function. 2) The dermis: is the middle layer, its principal constituent is the collagen. 3) The hypodermis(panniculus): composed of lobules of lipocytes. THE EPIDERMIS: It is avascular, stratified squamous epithelium, varying in thickness from less than 0.1mm. on the eyelid to nearly 1.5mm. on the palms & soles. Composed of 5 cell types: 1- Keratinocytes(squamous cells): It's the main cell type of the epidermis (about 90%), they are of ectodermal origin, its ultimate function is the production of a range of structural proteins on the outer coat of the skin, the hair & nail, including keratin and loricrin. Keratin genes are divided into two subfamilies, basic & acidic, the product of one basic & one acidic keratin gene combine to form the multiple keratins. Mutations in keratin genes can result in many skin diseases. During keratinization, the keratinocytes passes into a synthetic & then a degradative phase on its way to becoming a horn cell, first it accumulates in its cytoplasm intermediate filaments composed of keratin, these tonofilaments are fashioned into bundles which converge on & terminate at the plasma membrane where they end in a specialized attachment plates called desmosomes., the degradative phase of keratinization is characterized by the disappearance of all cell organelles & the consolidation of all cell contents into a mixture of filaments & amorphous cell envelopes. This programmed process of maturation resulting in death of the cell is called Terminal differentiation. The intercellular space between adjacent keratinocytes contains glycoproteins & lipids, which contribute to the cohesion & impermeability of skin. Keratinocytes are arranged in 5 layers: A) Basal layer(stratum germinativum): the proliferative compartment of the epidermis resides in this layer, which is the deepest layer resting on the basement membrane & attached to it by hemi- desmosomes, it's a single layer of nucleated, columnar cells, their main function is cell mitosis & DNA synthesis giving daughter cells which differentiate into keratinocytes & goes up the next layer. B) malpighian or prickle cell layer(stratum spinosum): Lying above the basal layer & is usually 5-8 layers, the cells appear spiny (containing prickles) due to the presence of small interlocking cytoplasmic processes( desmosomes) which are thickenings on the cell membrane of two opposing cell surfaces, allowing the sliding of adjacent cells on each other upon trauma, differentiation continues into the next layer, giving the granular cell layer. C) Granular layer(stratum granulosum): usually 2-3 layers of cells which are flatter than those in the spinous layer, here the nucleus & the cell organelles all begin to degenerate & the cells in addition to the keratin filament system, contain large, irregular, basophilic granules called keratohyaline granules composed of amorphous particulate material of high sulphur protein content, called profillagrin a precursor of fillagrin which is responsible for keratin filament aggregation, D) Horny layer(stratum corneum): compact, flattened dead cells filled with keratin filaments which appear homogenous containing no nucleus or other cell organelles, keratohyaline is hygroscopic & repeated cycles of hydration & dehydration contribute to normal desquamation of the stratum corneum, they desquamate continuously at the surface of the skin being replaced by newer cells from beneath. The epidermal cell cycle from the basal layer to desquamation at the surface takes about 28 days normally. On the palms & soles there is an additional clear layer between granular & horny layer called stratum lucidum. The epidermis acts as a hydrophobic barrier, due to its design, also the keratinocytes play an active role in the immune function of the skin. 2) Melanocyte: The 2nd important cell type in the epidermis, responsible for melanin synthesis from tyrosine through the action of tyrosinase enzyme, they are dendritic & originate from neural crest during embryonic life. Each cell is associated with a number of keratinocytes forming an epidermalmelanin unit. They are situated in the basal cell layer at a rate of 10 to 1 which is fixed in all races. Their cytoplasm contain discrete organelles called melanosomes where the melanin is stored before being injected into surrounding keratinocytes through dendrites, these melanosomes are responsible for the difference in normal skin color between races; being more in number, larger, & more dispersed in negroids than Caucasoid. 3) Langerhan's cell: A dendritic cell originating from bone marrow, found suprabasally with a lobulated nucleus, it contains specific granules in the cytoplasm appearing rod-shaped or racquet-shaped on electron microscopy. They play a key role in immune reactions as an antigen presenting cell, they take up exogenous antigen; process it & present it to T- lymphocytes, and they might have a role in tumor antigen presentation as well. 4) Merkel cells: Non-dendritic cells lying in or near basal cells & act as a modified touch receptor. 5) Indeterminate cells: Of yet-unidentified function. The basement membrane zone: Lies at the interface between the epidermis & the dermis, it appears as a single layer; but under electron microscopy it is composed of 3 layers: 1) The basement membrane of basal cells with its attached hemidesmosomes. 2) Lamina lucida: an electron lucent area composed of laminin, with anchoring filaments extending through this layer to attach it to lamina densa. 3) Lamina densa: an electron dense area rich in collagen IV, from which extend loops of type VII collagen forming anchoring fibrils that fasten the basement membrane to the dermis. The dermis: Lies under the epidermis & supports it both structurally and nutritionally, they interdigitate so that upward projections of the dermis (the dermal papillae) interlock with downward ridges of the epidermis (the rete-pegs), this increases the force of adhesion & the area of contact between the epidermis & dermis. The dermis consists of: A) Interwoven bundles of fibers mainly (70-80%) collagen I & III, with lesser amounts of elastic & reticulin fibers. B) Cells: mostly fibroblasts, but also macrophages, lymphocytes, & mast cells. C) Ground substance consisting of glycoproteins called glycosaminoglycan, whose production & catabolism may be influenced by hormonal changes & ultraviolet radiation. Epidermal appendages: 1) The hair: hairs are classified into 3 main types: a) lanugo hair: fine, long hair, during intrauterine life. b) vellous hair: fine, short hair, covering much of our body. c) Terminal hair: long, coarse, hair as that on the scalp, or pubic area, often influenced by androgenic hormones. In embryonic life the hair follicle is formed by a club-shaped epidermal invagination which grows obliquely into the dermis to be met by a cluster of mesenchymal cells bulging into the lower part of the hair germ to form the hair papilla which contains the blood vessels bringing nutrients to the hair matrix; whose cells make the hair shaft & it's surrounding structures (outer root sheath, inner root sheath, & the cuticle).The hair passes through regular cycles of growth & shedding: 1) Anagen: The active phase of hair production, lasting usually 2-3 years. 2) Catagen: Short phase of conversion from growth to resting phase lasts 2-3 weeks 3) Telogen: A resting phase at the end of which a club hair is shed, it lasts 2-3 months. Also attached to the hair follicle at an oblique angle is the erector pili muscle, supplied by adrenergic fibers causing hair erection during fear, anger, & cold. 2) THE SEBACEOUS GLANDS: The sebaceous gland is an outgrowth at the side of the hair germ making up the pilosebaceous unit , it is a multilobed gland containing cells full of lipid which are disintegrated to shed their sebum (holocrine secretion), the sebum is a complex lipid containing triglycerides, cholesterol, fatty acids, wax esters, & squalene, it lubricates & waterproofs the skin, it is also mildly bactericidal & fungi static, the secretion is stimulated by androgenic hormones. 3) Eccrine (sweat glands): There are 2-3 million glands all over the body, being most numerous on the palms, soles, & axillae. It's composed of a tightly coiled secretory part deep in the dermis with an emerging duct that opens on the surface of the skin independent of the pilo-sebaceous unit. Sweat is important in thermoregulation. Sweat glands are innervated by cholinergic fibers of the sympathetic nervous system. 4) Apocrine glands: Are modified sweat glands limited to the axillae, nipples, periumbilical area, perineum & genitalia.The action of bacteria on apocrine sweat is responsible for body odor, their secretion is influenced by hormones especially androgens 5) The nail: It's composed of: 1) Nail plate: the hard keratinous part on the distal phalanx of each digit. 2) Nail matrix: lying under the proximal nail fold on the back of the terminal phalanx of each digit, responsible for nail synthesis. 3) Nail bed: the pink layer underlying the nail plate. 4) Nail folds: two lateral on each side of the terminal phalanx & a proximal one overlying the nail matrix. 5)The cuticle: is a thin layer running from the free edge of the nail & crossing over the proximal nail fold so as to protect the important underlying matrix. Blood supply of the skin: The blood vessels lie in 2 horizontal layers, the deep plexus is just above the subcutaneous fat & a superficial plexus in the papillary dermis with interconnecting channels between the two.