* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Kawasaki disease wikipedia , lookup
Anti-nuclear antibody wikipedia , lookup
Inflammation wikipedia , lookup
Complement system wikipedia , lookup
DNA vaccination wikipedia , lookup
Autoimmunity wikipedia , lookup
Immune system wikipedia , lookup
Schistosomiasis wikipedia , lookup
Adaptive immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Innate immune system wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
HYPERSENSITIVITY
TISSUE REACTIONS AND
PATHOLOGICAL CHANGES
MEDIATED BY
ANTIBODY - ANTIGEN REACTIONS.
PATHOLOGICAL REACTIONS
• Pathological (hypersensitivity) reactions refers
to undesirable (damaging, fatal) reactions
produced by the normal immune system.
• Hypersensitivity reactions require a presensitized (immune) state of the host.
• Frequently, a particular clinical condition
(disease) may involve more than one type of
reaction.
Intro cont.
• Pathological reactions mediated by antibody
antigen reaction (hypersensitivity reactions
are grouped in to 4 categories.
NOTE: HYPERSENSITIVITY REACTION ARE GROUPED IN TO 4 CLASSES BUT THOSE DUE
TO ab-ag COMPLEXES ARE 3 TYPES
• These may be due to abnormal reactions to
exogenous antigen or to self tissue molecules
which are recognized as antigens by the
antibodies.
• Type 1 - immediate (or atopic, or
anaphylactic)
• Type 2 - antibody-dependent
• Type 3 - immune complex
• Type 4 - cell-mediated (Delayed-Type
Hypersensitivity, DTH)
• Type 5 - stimulatory
Type I Hypersensitivity
• It is also known as immediate or anaphylactic
hypersensitivity.
• The reaction may involve
– Skin (urticaria and eczema),
– eyes (conjunctivitis),
– nasopharynx (rhinorrhea, rhinitis),
– bronchopulmonary tissues (asthma) and
– gastrointestinal tract (gastroenteritis)
– Systemic.
• The reaction may cause from minor
inconvenience to death.
• The reaction may be:
– immediate (immediate phase takes 15-30 minutes
from the time of exposure to the antigen.
– delayed (late phase) takes 10-12 hours
Mechanism of reaction
• The primary cellular component in this
hypersensitivity is mast cell or basophil. The
reaction is modified by platelets,neutrophils
and eosinophils.
• The mechanism of reaction involves
preferential production of IgE, in response to
certain antigens, allergens which binds to its
receptor on mast cells and basophils.
• A subsequent exposure to the same allergen
cross links the cell-bound IgE and triggers the
release of various pharmacologically active
substances. Mast cell degranulation is
preceded by increased Ca++ influx, which is a
crucial process;
– ionophores which increase cytoplasmic
Ca++ also promote degranulation, whereas,
agents which deplete cytoplasmic Ca++
suppress degranulation.
• Mast cells may be triggered by other stimuli
such as exercise, emotional stress, chemicals
(e.g., photographic developing medium,
calcium ionophores,
Pathogenesis
Examples
• Allergic asthma
• Allergic conjunctivitis
• Allergic rhinitis("hay fever")
• Anaphylaxis
• Atopic dermatitis(eczema)
• Urticaria(hives)
Type 2 - antibody-dependent
• In type 2 hypersensitivity, the antibodies
produced by the immune response bind to
antigens on the patient's own cell surfaces.
• The antigens recognized in this way may be;
– intrinsic ("self" antigen, innately part of the
patient's cells) or
– extrinsic (absorbed onto the cells during
exposure to some foreign antigen, possibly
as part of infection with a pathogen).
• These cells are recognised by macrophages or
dendritic cells which act as antigen presenting
cells, this causes a B cell response where
antibodies are produced against the foreign
antigen.
Mechanism of reaction
An example here is the reaction to penicillin
where the drug can bind to red blood cells
causing them to be recognised as different,
B cell proliferation will take place and
antibodies to the drug are produced.
IgG and IgM antibodies bind to these
antigens to form complexes that activate
the classical pathway of complement
activation for eliminating cells presenting
foreign antigens. That is, mediators of acute
inflammation are generated at the site
cause cell lysis and death. The reaction
takes hours to a day.
• Another form is called Antibody Dependent
Cell Mediated Cytotoxicity (ADCC). Here, cells
exhibiting the foreign antigen are tagged with
antibodies (IgG or IgM). These tagged cells are
then recognized by Natural Killer (NK) cells
and macrophages leading to phagocytosis
Examples
• Hemolytic anemia
• Rheumatic fever
• SLE
Type 3 - immune complex
• In type 3 hypersensitivity, soluble immune
complexes (aggregations of antigens and IgG
and IgM antibodies) form in the blood and are
deposited in various tissues
– skin,
– kidney and
– joints
They may trigger an immune response according to
the classical pathway of complement activation.
The reaction takes hours to days to develop.
Mechanism of reaction
• There are 2 types;
– Arthus reaction which is localized:
• Immune complex may cause
inflammatory tissue injury in specific sites
like hemorragic vasculitis and edema in
vessel injury
– Serum sickness which systemic
• Immune complex stimulate inflammatory
process in the blood and tissues leading
to fever, splenomegaly,
lymphadenopathy, arthralgia urticaria etc
Examples
• Immune complex glomerulonephritis
• Rheumatoid arthritis (post GABHS - M protein)
• Subacute bacterial endocarditis
• Symptoms of malaria
• Systemic lupus erythematosus (hydralazine)
Type 4 hypersensitivity
• Is often called delayed type as the reaction
takes two to three days to develop.
• Unlike the other types, it is not antibody
mediated but rather is a type of cell-mediated
response.
• CD8+ cytotoxic T cells and CD4+ helper T cells
recognise antigen in a complex with either
type 1 or 2 MHC. The APC in this case are
macrophages which secrete IL-1, which
stimulates the proliferation of further CD4+ T
cells. CD4+ T cells secrete IL-2 and IF gamma,
further inducing the release of other Type 1
cytokines, thus mediating the immune
response.
• Activated CD8+ T cells destroy target cells on
contact while activated macrophages produce
hydrolytic enzymes and, on presentation with
certain intracellular pathogens, transform into
multinucleated giant cells.
Examples:
• Contact dermatitis (poison ivy rash)
• Temporal arteritis
• Symptoms of leprosy
• Symptoms of tuberculosis
• Transplant rejection
• Coeliac disease
Rheumatoid arthritis (RA)
• RA is a chronic, inflammatory, systemic disease
often affecting articular and extra-articular
tissues throughout the body including the skin,
blood vessels, heart, lungs, and muscles.
• About 60% of RA patients are unable to work
10 years after the onset of their disease.
• The name is derived from the Greek.
Rheumatos means "flowing", and this initially
gave rise to the term 'rheumatic fever', an
illness that can follow throat infections and
which includes joint pain.
• The suffix -oid means "resembling", i.e.
resembling rheumatic fever. Arthr means
"joint" and the suffix -itis, a "condition
involving inflammation".
– Thus rheumatoid arthritis was a form of
joint inflammation that resembled
rheumatic fever
Features
• Polyarthritis.
–
The joints are usually affected initially
asymmetrically and then in a symmetrical
fashion as the disease progresses. The pain
generally improves with use of the affected
joints, and there is usually stiffness of all
joints in the morning that lasts over 1 hour.
Thus, the pain of rheumatoid arthritis is
usually worse in the morning compared to
the classic pain of osteoarthritis where the
pain worsens over the day as the joints are
used.
• Extra-articular manifestations also distinguish
this disease from osteoarthritis (hence it is a
multisystemic disease).
– For example, most patients also suffer with
anemia, either as a consequence of the
disease itself (anaemia of chronic disease)
or as a consequence of gastrointestinal
bleeding as a side effect of drugs used in
treatment, especially NSAIDs used for
analgesia.
• Hepatosplenomegaly may occur with
concurrent leukopaenia (Felty's syndrome),
and lymphocytic infiltration may affect the
salivary and lacrimal glands (Sjögren's
syndrome).
– Pericarditis, pleurisy, alveolitis, scleritis and
subcutaneous nodules are other features
Pathophysiology
Causes
• The cause of RA is still unknown to this day, but has long been
suspected to be infectious. It could be due to food allergies or
external organisms. Mycoplasma, Erysipelothrix, EBV,
parvovirus B19 and rubella have been suspected but never
supported in epidemiological studies.
• As in other autoimmune diseases, the "mistaken identity"
theory suggests that an offending organism causes an
immune response that leaves behind antibodies that are
specific to that organism.
• The antibodies are not specific enough, though (can react
with self tissue proteins).
Asthma
Pathophysiology:
• Asthma is a condition characterized by
paroxysmal narrowing of the bronchial
airways due to inflammation of the bronchi
and contraction of the bronchial smooth
muscle. The inflammatory component is
central to the pathogenesis of symptoms:
dyspnea, cough, and wheezing.
• Another mechanism underlying acute asthma
involves antigen-antibody interactions, which
activate membrane phospholipase and result
in production of arachidonic acid. Arachidonic
acid is metabolized by cyclooxygenase to
vasoactive prostaglandins (eg, thromboxanes,
prostacyclins) or leukotrienes and their
precursors. Several are potent smooth muscle
contractors that produce airway
hyperresponsiveness and inflammation.
• Causes of acute asthma includes;
– viral upper respiratory infections
– exposure to allergens (eg, dustmites, animal
dander)
– smoke inhalation; and cold, dry weather
– A strong association had been thought to exist in
women between the perimenstrual phase of their
cycle and asthma symptoms.
Rheumatic fever
• Rheumatic fever causes chronic progressive
damage to the heart and its valves. Until 1960,
it was a leading cause of death in children and
a common cause of structural heart disease.
• The association between sore throat and
rheumatic fever was not made until 1880. The
connection with scarlet fever was made in the
early 1900s. In 1944, the Jones criteria were
formulated to assist disease identification.
These criteria, with some modification, remain
in use today.
• The introduction of antibiotics in the late
1940s allowed for the development of
treatment and preventive strategies. The
dramatic decline in the incidence of rheumatic
fever is thought to be largely owing to
antibiotic treatment of streptococcal infection
Pathophysiology
• ARF is a sequela of a previous group A
streptococcal infection, usually of the upper
respiratory tract.
• The disease involves the heart, joints, central
nervous system (CNS), skin, and subcutaneous
tissues. It is characterized by an exudative and
proliferative inflammatory lesion of the
connective tissue, especially that of the heart,
joints, blood vessels, and subcutaneous tissue.
• It occurs during school years when
streptococcal pharyngitis is most prevalent.
Similarly, prevalence is higher in the colder
months of the year when streptococcal
pharyngitis is most likely to occur.
• Sex: No sex predilection exists, except that MV
prolapse and Sydenham chorea occur more
often in females than in males.
• Age: Although individuals of any age group
may be affected, most cases are reported in
persons aged 5-15 years.
Clinical features
•
ARF is associated with 2 distinct patterns of presentation.
– The first pattern of presentation is sudden onset. It
typically begins as polyarthritis 2-6 weeks after
streptococcal pharyngitis and is usually characterized by
fever and toxicity.
– If the initial abnormality is mild carditis, ARF may be
insidious or subclinical.
• Age at onset influences the order of complications. Younger
children tend to develop carditis first, while older patients
tend to develop arthritis first.
• Diagnosis of ARF requires a high index of suspicion.
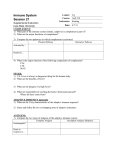
Diagnosis
• In addition to evidence of a previous
streptococcal infection, the diagnosis requires
2 major Jones criteria or 1 major plus 2 minor
Jones criteria.
– Major criteria
• Carditis: This occurs in as many as 40% of
patients and may include cardiomegaly,
new murmur, congestive heart failure,
and pericarditis, with or without a rub
and valvular disease.
• Migratory polyarthritis: This condition
occurs in 75% of cases and is
polyarticular, fleeting, and involves the
large joints.
• Subcutaneous nodules (ie, Aschoff
bodies): These nodules occur in 10% of
patients and are edematous, fragmented
collagen fibers. They are firm, painless
nodules on the extensor surfaces of the
wrists, elbows, and knees.
• Erythema marginatum: This condition
occurs in about 5% of cases. The rash is
serpiginous and long lasting.
• Chorea (also known as Sydenham chorea
and "St Vitus dance"): This characteristic
movement disorder occurs in 5-10% of
cases. Sydenham chorea consists of rapid,
purposeless movements of the face and
upper extremities. Onset may be delayed
for several months and may cease when
the patient is asleep.
– Minor criteria
• Clinical findings include arthralgia, fever
and previous history of ARF
• Laboratory findings include elevated
acute phase reactants (eg, erythrocyte
sedimentation rate, C reactive protein), a
prolonged PR interval, and supporting
evidence of antecedent group A
streptococcal infections (ie, positive
throat culture or rapid streptococcal
screen and an elevated or rising
streptococcal antibody titer).
Causes:
– ARF has been linked definitely with a preceding
streptococcal infection, usually of the upper
respiratory tract
Lab Studies:
• No specific confirmatory laboratory tests exist.
However, several laboratory findings indicate
continuing rheumatic inflammation. Some are part of
the Jones minor criteria.
– Streptococcal antibody tests disclose preceding
streptococcal infection.Isolate group A
streptococci via throat culture.
– Acute phase reactants (eg, erythrocyte
sedimentation rate [ESR], C-reactive protein [CRP]
in serum and leukocytosis) may show an increase
in serum complement, mucoproteins, alpha-2,
and gamma globulins. Anemia usually is caused by
suppression of erythropoiesis.
– PR interval prolongation is present in
approximately 25% of all cases and is neither
specific to nor diagnostic of ARF.
– Troponins have not been shown to be helpful in
making the diagnosis since ischemia and necrosis
are not the major cardiac problems.
TREATMENT
• Medical therapy involves the following 5
areas:
– Treat group A streptococcal infection
regardless of organism detection.
– Steroids and salicylates are useful in the
control of pain and inflammation.
– Heart failure may require digitalis.
– Administer prophylaxis to patients who have
developed ARF. Patients with ARF should receive
prophylaxis against future GABHS infections.
Available regimens include benzathine penicillin G
1.2 million U IM every month, penicillin V 200,000
U or 250 mg PO bid, or erythromycin 250 mg PO
bid. Most authorities suggest that prophylaxis be
given for 5 years. For those who have rheumatic
carditis, some authorities suggest life-long
prophylaxis.
– Haloperidol may be helpful in controlling chorea
Complications:
• Carditis
• Mitral stenosis
• Congestive heart failure (CHF)
Prognosis:
• Sequelae are limited to the heart and are dependent
upon the severity of the carditis during the acute
attack.
THANKS FOR
YOUR PATIENCE