* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Mechanism of drug action
CCR5 receptor antagonist wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug discovery wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
NMDA receptor wikipedia , lookup
Toxicodynamics wikipedia , lookup
Pharmacokinetics wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
Theralizumab wikipedia , lookup
Drug design wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Psychopharmacology wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
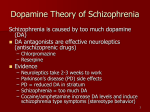
Pharmacodynamics Pharmacodynamics is the study of the biochemical and physiologic effects of drugs and their mechanisms of action. Mechanisms of Drug Action How does a drug work drugs and endogenous ligands molecular target drugs and endogenous ligands Molecular Target alters tissue function Types of mechanism of drug action (1) Physical and chemical reaction Antacids neutralizing gastric acid Mechanism of drug action (2)Joining or interfering with cell metabolism Vitamins, iron preparations and some anticancer drugs whose chemical structure resemble purine or pyrimidine are called counterfeit incorporation or antimetabolite. Mechanism of drug action (3) Affecting transportation of physical substances Reserpine affect the uptake of norepinephrine Mechanism of drug action (4) Affecting enzyme activity Neostigmine exerts its cholinergic effect by inhibiting activity of AChE Mechanism of drug action (5) Affecting ion channels on the cell membrane Mechanism of drug action (6) Affecting immunology function The immunosuppressive and immunomodulating agents result in efficiency by influencing body immunity function. glucocorticoids or cyclosporin Active immunity obtained by using vaccine Mechanism of drug action (7) Affecting nucleotide metabolism Many anticancer drugs exert effective action on cancer cells by interrupting DNA and RNA metabolism of cancer cells. Mechanism of drug action (8). Receptors Receptors are specialized target macromolecules, present on the cell surface or intracellular; that bind drugs and mediate their pharmacologic actions. Receptors have become the central focus of investigation of drug effects and their mechanisms of action. Many drug receptors have been isolated and characterized in detail, thus opening the way to precise understanding of the molecular basis of drug action. Receptors Largely determine the quantitative relations between dose or concentration of drug and pharmacologic effects. Be responsible for selectivity of drug action. Mediate the actions of pharmacologic agonists and antagonists. Development of receptor theory a.Langley(1878): Intercounter of atropine with pilocarpine in salivary excretion. "There is some substance or substances in the nerve ending or gland cell with which both atropine and pilocarpine are capable of forming compounds." b. Langley(1905):Intercounter tubocurarine with nicotine in skeletal muscle – “receptive substance” Development of receptor theory c. Ehrlich(1905): “ receptor” trying to develop specific drugs to treat parasitic infections trying to understand the basis of selectivity of agents a drug could have a therapeutic effect only if it has the “right sort of affinity.” "... that combining group of the protoplasmic molecule to which the introduced group is anchored will hereafter be termed receptor.“ Each cell would have particular characteristics to recognize particular molecules. Development of receptor theory c. Ehrlich(1905): “lock and key” drug drug receptor Only the correctly shaped key opens a particular lock. Interaction between receptor and drug (receptor theory) (1) Occupation theory Simple occupancy theory - - “ Intensity of response to a drug is proportional to the number of receptors occupied by that drug” Maximal response occurs when all available receptors have been occupied 2. Modified Occupancy Theory a. Affinity binding- strength of the attraction between drug and receptor. Drugs with low affinity require higher concentrations to bind to receptor b. Intrinsic activity- ability of a drug to activate its receptor. High intrinsic activity relates to high maximal efficacy Kinetics of Receptor and Drug Drug + Receptor↔ Drug-receptor complex → Biologic effect Factors Affecting Drug-Target Interactions Drug + Receptor Drug-receptor complex Affinity Biologic effect Intrinsic Activity Two basic properties of the drug-receptor interaction contribute to drug responses the ability of the drug to bind to its receptor the ability of the drug to alter the activity of its receptor Receptor Binding Affinity: the ability of a drug to bind to the receptor (just bind). Covalent bonds = strong bonds and long-lasting or irreversible effects Hydrogen Ionic Weak Hydrophobic Reversible Van der Waals Receptor Binding and Affinity Drug + Receptor The Affinity Drug-receptor complex ability of a drug to bind a receptor A measure of how strongly that drug binds to the receptor Determined by the dissociation constant (KD) Dissociation Constant (KD) KD = [D] x [R] [DR] Affinity is the inverse of the KD (1/KD) The smaller the KD, the greater affinity a drug has for its receptor Receptor Binding and Affinity [ D].[ R] KD [ DR ] Receptor Binding and Affinity Total number of receptors: Rt = [R] + [DR] [R] = Rt – [DR] KD [ D].( Rt [ DR ]) [ D].Rt [ D].[ DR ] [ DR ] [ DR ] After rearrangement: [ D ].Rt [ DR ] K D [ D] [ DR ] [ D] Rt K D [ D] When [D] = KD [DR] = 0.5 RT [ DR ] [ D] Rt K D [ D] 1.00 [DR]/Rt 0.75 KD is the concentration of drug when half of the receptor population is occupied. 0.50 0.25 0.00 0 5 10 15 20 [D] KD Receptor Binding and Affinity high Receptor Binding and Affinity KD high concentration for occupying half of the receptor low affinity low Every drug/receptor combination will have a characteristic KD. KD lower concentrations for occupying half of the receptor high affinity Two drugs that have equal affinities (binding) for a specific target but have different efficacies (degree of response) Other factors, in addition to affinity and receptor occupancy, determine the strength of response. Intrinsic activity (Efficacy) Activation of the Molecular Target The ability of drug-receptor complex to activate the receptor and initiate downstream events, leading to an effect Be not directly related to receptor affinity Drugs categorized based on their intrinsic activity at a given receptor Agonist has affinity plus full intrinsic activity Antagonist has affinity but no intrinsic activity Agonist A compound that binds to the receptor and alters the receptor state resulting in a biological response Mimics the response to the endogenous ligand e.g.: Pilocarpine Receptor Some Effect Pilocarpine A Cell Agonist Increasing concentrations of the agonist will increase the biological response until there are no more receptors for the agonist to bind or a maximal response has been reached. Types of agonists Full agonists: high affinity and high efficacy ( α = 1) Partial agonists :high affinity and lower intrinsic activity (0﹤α﹤1 ) This designation of full vs. partial agonist is system-dependent Inverse agonists inhibit rather than activate the receptor Antagonists to receptors but do not activate them(α = 0) Have no effect of their own Prevent agonists from binding the receptors Block or reverse the effect of an agonist eg: Atropine, β-blockers Bind Dude, you’re in my way! Atropine Acetylcholine Agonists alone Full activation Antagonists alone No activation Agonists + Antagonists Less activation Partial agonists High affinity and lower intrinsic activity (0﹤α﹤1). Cannot bring about the same maximum response as full agonists even at very high doses Partial agonist Oh!!!, I should Have been here Full agonist Submaximal effect Partial agonists Possess some of the properties of both antagonists and full agonists When used alone, a partial agonist will act like a weak agonist In the presence of a full agonist, a partial agonist will act like an antagonist Full agonists alone Full activation Partial agonists alone Partial activation Full agonists + Partial agonists Less activation Inverse agonist Any drug that binds to a receptor and produces an opposite effect as that of an agonist Inverse agonists inhibit rather than activate the receptor. Receptor Effect opposite to that of the true agonist Inverse agonist A Cell Drug Receptor Interactions The two-state model of receptor activation ‘In the unbound state a receptor is functionally silent’ Some receptor systems display constitutive activity in absence of the ligand two-state model The receptor is in two conformational states, ‘resting’ (R) and ‘active’ (R*), which exist in equilibrium. Normally, when no ligand is present, the equilibrium lies far to the left, and a few receptors are found in the R* state. For constitutively active receptors, an appreciable proportion of receptors adopt the R* conformation in the absence of any ligand. Resting state Active state two-state model An agonist has higher affinity for R* than for R A neutral antagonist has equal affinity for R and R* An inverse agonist has higher affinity for R than for R* Resting state Active state Inverse agonists vs Antagonists Elicit similar effects because both types of drugs will reverse the effects of endogenous ligands Antagonists have no activity in the absence of agonists or inverse agonists Antagonists block the effects of both the agonists and inverse agonists Spare Receptors A pharmacological system has spare receptors if a full agonist can cause a maximum response when occupying only a fraction of the total receptor population Not all of the receptors in the tissue are required to achieve a maximal response with some high efficacy agonists Spare Receptors Spare receptors are exhibited by insulin receptors, where it has been estimated that 99 percent of the receptors are “spare.” The “spare” receptors are not nonfunctional. When they are occupied they can be coupled to response. Receptor reserve Quantifying Drug-Target Interactions: DOSE-RESPONSE RELATIONSHIPS A mathematic relationship between the dose of a drug and the body's reaction to it. Can be illustrated as a graph called a doseresponse curve. dose-response curve Effect Concentration (in vitro) Dose (in vivo) Two basic types of dose-response curves Graded • Continuous scale • the effect of various doses of a drug on an individual • Relates dose to intensity of effect Quantal • All-or-none pharmacologic effect • the effect of various doses of a drug on a population of individuals • Relates dose to frequency of effect Graded dose–response relations The response is continuous and gradual Describe the effect of various doses of a drug on an individual Graded Dose-Response Curve rectangular hyperbola Effect C Graded Dose-Response Curve sigmoid curve (S-shaped curve) 80 Effect % slope 20 lgC Advantages of this curve: Show a much larger range of concentrations The portion of the curve between 20 and 80% of Emax is approximately a straight line. It is more easier to quantitative values Phase 1: occurs at low doses Curve is flat because response is too low to measure Phase 2: increase in doses elicits increase in response Phase 3: occurs at high dose (maximum response) Higher dose does not increase extra therapeutic effects, but increases the risk of adverse effects 100 Maximal effect Effect % (efficacy) 50 Minimal Effective Concentration (MEC) Slope EC50 lgC Half Maximal Effective Concentration Minimal Effective Concentration (MEC) A minimum plasma concentration that will produce an effect. Maximal response (efficacy, Emax ) Maximal response or efficacy of the drug Slope (the rise in response with changes in concentration) A steep slope indicates a small increase in drug dosage produces a large change in responses. A shallow slope indicates a much larger increase in dose is required to cause the same increase in response. EC50 (Half Maximal Effective Concentration ) The molar concentration of an agonist that produces 50% of the maximal possible effect of that agonist. ED50 (best reserved for in vivo use )is sometimes used interchangeably with EC50 EC50 Concentration Potency An expression of the activity of a drug, in terms of the concentration or amount needed to produce a defined effect. A measure of how much drug is required to elicit a given response Commonly designated as the EC50 Potency EC50 Concentration Potency The potency of a drug is inversely related to its EC50. The smaller is the EC50, the lower the dose required to give a response, the more potent is the drug. Farther to the left = more potent Potency pEC50 (pD2): The negative decade logarithm of the EC50 of an agonist pD2= pEC50 = logEC50 pD2 is taken as the measure of potency The higher pD2, the higher potency ! Potency vs. Efficacy (Maximal Effect ) Potency The amount of drug required to achieve a defined biological effect Given by the position of the doseresponse curve along the x-axis Efficacy The maximal response a drug can produce Given by the peak of the doseresponse curve Maximal Effect EFFICACY POTENCY ED50 Log [Dose] Potency vs. Maximal Effect (Efficacy) Potency has nothing to do with efficacy Efficacy is not related to potency "Relative Pharmacological Potency" and the "Maximal Efficacy" In most cases the efficacy is more important than the potency in drug selection. Greater potency or efficacy does not necessarily mean that one drug is preferable to another. Quantal Dose–Response Relationships Describes the distribution of responses to different doses in a population of individuals Quantal responses are all-or-none responses to a drug Even graded responses can be considered to be quantal if a predetermined level of the graded response is designated as the point at which a response occurs or not. Y-axis is the percentage of individuals experiencing sleep at any given dose. Number of Individuals Many Sensitive Individuals Minimal Effect Majority of Individuals Resistant Individuals Average Effect Maximal Effect Few Mild Response to SAME dose Extreme Quantal dose-response curves describe the relationship between drug dosage and the frequency with which a biologic effect occurs. Quantal Dose–Response Relationships Cumulative Effect % sigmoidal curve lgD Quantal Dose–Response Relationships This type of sigmoidal curve yields useful safety information when the all-or-nothing responses are defined as therapeutic maximal responses, toxic responses, or lethal responses. individuals individuals individuals individuals ED50 Median effective doses TD 50 Median toxic doses LD50 Median lethal doses (in animals) Two Definitions of ED50 – one for whole animal vs population studies ED50 (Half maximal effective concentration) : the dose that produces 50% of the maximal response to that drug (the response is graded) ED50 (Median effective dose) : the effective dose at which 50% of the test subjects produce effective response (the response is all-or-none) Drug Safety & the Therapeutic Index Therapeutic index = LD50/ ED50 A statement of relative safety of a drug Large values of TI indicate that the doses that produce death are much greater than those that produce a therapeutic effect When a drug’s therapeutic index is less than 10, then the drug is defined as having a narrow therapeutic window. when the therapeutic index is low, it is possible to have a range of concentrations where the effective and toxic responses overlap. Penicillin is safe and common to give doses in excess (often about ten-fold excess) of that which is minimally required to achieve a desired response. The TI may be misleading as to safety, depending on the slope of the dose-response curves for therapeutic and lethal effects. A1 A2 100 Cumulative Effect % B1 B2 50 ED50 LD50 lgD Certain Safety Factor = LD1/ED99 Therapeutic window : the plasma concentrations range between minimum effective concentration and minimum toxic concentration DRUG ANTAGONISM Types of Antagonism /1/ Chemical antagonism 2/ Physiological antagonism / /3/ Pharmacokinetic antagonism /4/ Antagonism by receptor block /1/ Chemical antagonism Interaction of two substance based on their chemical properties. Example : Chelating agents (e.g., dimercaprol) that bind heavy metals to form an inactive complex, and thus reduce their toxicity. 2/ Physiological antagonism / Two drugs act on separate physiological systems and produce opposite actions. Example : Histamine acts at H1 receptors on bronchial smooth muscle to cause bronchoconstriction, whereas adrenaline is an agonist at the β2 receptors bronchial smooth muscle, which causes bronchodilation. /3/ Pharmacokinetic antagonism One drug accelerates the metabolism or elimination of another. Example: phenobarbital (enzyme induction) accelerates the rate of metabolic degradation of the anticoagulant warfarin. /4/ Antagonism by receptor block The antagonists may block the ability of agonists to bind to the receptor by competing for the same receptor site or may bind to another site on the receptor that blocks the action of the agonist Pharmacologic Antagonists Competitive reversible antagonism (competitive surmountable antagonism) Binds reversibly with receptors at the same site as the agonist Inhibition can be overcome by increasing agonist concentration (i.e., inhibition is reversible) Competitive reversible antagonism In the competitive presence of the antagonist, the agonist curve is shifted to the right (parallel shift) without change in slope or maximum. Maximal response occurs at a higher agonist concentration than in the absence of the antagonist Primarily affects agonist potency = Agonist = Antagonist = Agonist = Antagonist = Agonist = Antagonist pA2 The negative logarithm of the antagonist concentration at which it is necessary to double the concentration of agonists in order to produce the same response as if there were no antagonists. Be used to measures the potency of competitive antagonists Competitive irreversible antagonism (competitive insurmountable antagonism) Binds to same site on receptor as agonist Forms covalent bond with the receptor The antagonist dissociates from the receptors very slowly, or not at all Inhibition cannot be overcome by increasing agonist concentration Competitive irreversible antagonism Maximal response (Emax)is depressed The slope of the curve will be reduced The agonist dose-response curve will be shifted to the right Agonist potency may or may not be affected = Agonist = Antagonist Phenoxybenzamine (irreversible α–adrenoreceptor antagonist) If overdose occurs, α–adrenoreceptor blockade cannot be overcome by agonist. The effects must be antagonized physiologically by using a pressor agent that does not act via α–adrenoreceptors Competitive Irreversible Antagonism Noncompetitive antagonism (allotropic or allosteric antagonism) Does not bind to the same receptor sites as the agonist. Impair the ability of an agonist to bind to or activate the receptor Inhibition cannot be overcome by increasing agonist concentration (irreversible) Noncompetitive antagonism Maximal response will be depressed The slope of the curve will be reduced The agonist dose-response curve will be shifted to the right Agonist potency may or may not be affected Noncompetitive antagonism Noncompetitive antagonists will exert functional effects similar to those of competitive irreversible antagonists in that both types of antagonist will decrease the Emax or efficacy of the agonist. Signaling Transduction Mechanism The cellular process in which a signal is conveyed to trigger a change in the activity or state of a cell Agonist binding to a receptor are normally only the first of many steps required to produce a pharmacological effect. MAJOR RECEPTOR FAMILIES 1. Ligand-gated ion channels 2. G-protein-coupled receptors (GPCRs) 3. Kinase-linked receptors 4. Nuclear receptors Ligand-gated ion channels Receptor-operated channels Acetylcholine causes the opening of the ion channel in the nicotinic acetylcholine receptor G protein-coupled receptors Exposed at the extracellular surface of the plasma membrane, traverse the membrane, and possess intracellular regions that activate a unique class of signaling molecules Bind the guanine nucleotides GTP and GDP G protein-coupled receptors G protein-coupled receptors have seven transmembrane regions within a single polypeptide chain G proteins haveα and βγ subunits that are noncovalently linked in the resting state Stimulation of a GPCR causes its cytoplasmic domain to bind and activate a nearby G protein → the α subunit of the G protein exchanges GDP for GTP → the α-GTP subunit dissociates from the βγ subunit → the α or βγ subunit diffuses along the inner leaflet of the plasma membrane to interact with a number of different effectors. Adenylyl Cyclase Effectors Guanylyl Cyclase Cyclic Adenosine-3′,5′Monophosphate (cAMP) Cyclic Guanosine-3′,5′Monophosphate (cGMP) Second Messenger Diacylglycerol (DAG) Effectors Activates protein kinase C Phospholipase C Second Messenger (PLC) Inositol-1,4,5-trisphosphate (IP3) Increasing the cytosolic Ca 2+ concentration β-adrenergic receptor The receptors are stimulated by the binding of endogenous catecholamines→induces a conformational change in the receptor → activating G proteins associated with the cytoplasmic domain of the receptor → activates adenylyl cyclase → increased intracellular cAMP levels and downstream cellular effects. Transmembrane Receptors with Enzymatic Cytosolic Domains These receptors transduce an extracellular ligand-binding interaction into an intracellular action through the activation of a linked enzymatic domain Receptors have an intracellular enzymatic domain. These enzymatic cytosolic domains form dimers or multisubunit complexes to transduce their signals by adding or removing phosphate groups to or from specific amino acid residues. Receptor Tyrosine Kinases insulin receptor Intracellular receptors Lipophilic drugs passively cross the cell membrane The transcription regulatory factors are important cytosolic receptors that are targeted by lipophilic drugs. Transcription of many genes is regulated, in part, by the interaction between lipid-soluble signaling molecules and transcription regulatory factors. Steroid hormones diffuse through the plasma membrane → bind to transcription factors in the cytoplasm or nucleus → activate or inhibit transcription → alter the intracellular or extracellular concentrations of specific gene products → have a profound effect on cellular function. Receptor Regulation Receptors can undergo dynamic changes with respect to their density (number per cell) and their affinity for drugs and other ligands. Receptor Desensitization Receptor Hypersensitization RECEPTOR DESENSITIZATION Repeated or continuous administration of an agonist may lead to changes in the responsiveness of the receptor. Clinical sketch A middle-aged man has always suffered from anxiety and insomnia. He has been taking diazepam during the day and temazepam at night for many year. The doses of both drugs have gradually been increased (on the patient’s request) over the years because of diminishing effectiveness. Clinical sketch Comment: this inappropriate long-term use of sedatives can sometimes be hard to avoid. However, the drugs have probably become part of the problem instead of offering any therapeutic benefit. The diminishing effectiveness of the drug is termed ‘tolerance’ Tachyphylaxis or desensitization refers to the relatively rapid (minutes, hours) diminishing response caused by repeated drug administration. Tolerance generally refers to reductions in responsiveness that occur over a longer time frame (days or longer) caused by prolonged drug administration. Mechanisms of Desensitization I.Decreased sensitivity of receptors The receptors are still present on the cell surface but are unresponsive to the ligand The mechanisms protecting a cell from excessive stimulation. Mechanisms of Desensitization II. Down-regulation The receptor undergoes endocytosis and is sequestered from further agonist interaction. These receptors may be recycled to the cell surface, restoring sensitivity, or may be further degraded, decreasing the total number of receptors available. β2 adrenergic agonists Receptor Hypersensitization Continuous or repeated exposure to antagonists initially can increase the response of the receptor. With chronic exposure to antagonists, the number of receptors on the membrane surface (density) increases via up-regulation. Clinical sketch A 70-year –old man has been taking beta-blockers for many years for his angina. He develops intermittent claudication, and his doctor stops the betablocker suddenly. His angina worsens within days, and he is admitted to hospital with a myocardial infarction. Clinical sketch Comments:it is likely that receptor numbers are increased (‘upregulated’) in the presence of prolonged ‘blocking’. Sudden withdrawal of the drug can produce marked effects, as here. RECEPTOR CLASSIFICATION Specificity Specificity of drug action relates to the number of different mechanisms involved. Examples : atropine (a muscarinic antagonist), salbutamol (a β2adrenoceptor agonist), phenoxybenzamine (an α-adrenergic blocking agent), and cimetidine (an H2-receptor antagonist). Nonspecific drugs result in drug effects through several mechanisms of action. Examples : Phenothiazine, which causes blockade of D2dopamine receptors, α-adrenergic receptors, and muscarinic receptors. Structure-Activity Relationship The chemical structure of a drug determines its affinity for the receptor and ability to elicit a response The drug and receptor must be structurally complementary to recognize each other and initiate an effect. The specificity of such interaction raises the concept of molecular recognition. Drug receptors or targets must have molecular domains that are spatially and energetically favorable for binding specific drug molecules. Structure-Activity Relationship Proteins undergo folding to form threedimensional structures so that a minimum three point attachment of a drug to a receptor site is required. Drug binding to receptors often exhibits stereoselectivity, in which stereoisomers of a drug that are chemically identical, but have different orientations around a single bond, can have very different affinities. RECEPTOR CLASSIFICATION Receptors are commonly named after the natural agonist that activates them. Each receptor family typically contains multiple subtypes that may be characterized pharmacologically by the use of selective agonists, antagonists, or both. Few drugs are entirely specific for one receptor Epinephrine 1 Receptors in Heart 2 Receptors in Bronchioles Clinical Selectivity No drug causes only a (Selectivity of Drug Responses) single effect A drug's ability to preferentially produce a particular effect Be related to the structural specificity of drug binding to receptors. Selectivity of pharmacological effect is not equal to specificity of drug action Tissue Distribution of Receptors Even if a drug binds to only one kind of receptor, the biochemical processes controlled by such receptors would take place in many cell types and would be coupled to many other biochemical functions. Only those tissues possessing receptors will respond to the drug. Atropine Muscarinic acetylcholine receptor antagonist Higher specificity of drug action Lower selectivity of pharmacological effect Broad distribution of muscarinic acetylcholine receptor in the body (gland, eyes, smooth muscle, heart, blood vessels, and CNS) Clinical Selectivity (Selectivity of Drug Responses) Clinical Connection: Knowledge of receptor subtypes and their regional distribution can assist in drug selection. In clinic, we often choose a drug with higher selectivity to decrease side effects of the drug.