* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Differential Impairment of Individuated Finger Movements in
Survey
Document related concepts
Cortical cooling wikipedia , lookup
Microneurography wikipedia , lookup
Eyeblink conditioning wikipedia , lookup
Environmental enrichment wikipedia , lookup
Aging brain wikipedia , lookup
Neuroplasticity wikipedia , lookup
Dual consciousness wikipedia , lookup
Metastability in the brain wikipedia , lookup
Cognitive neuroscience of music wikipedia , lookup
Time perception wikipedia , lookup
Muscle memory wikipedia , lookup
Embodied language processing wikipedia , lookup
Transcript
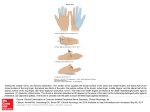
J Neurophysiol 90: 1160 –1170, 2003; 10.1152/jn.00130.2003. Differential Impairment of Individuated Finger Movements in Humans After Damage to the Motor Cortex or the Corticospinal Tract Catherine E. Lang1,2 and Marc H. Schieber1– 4 1 Departments of Neurology, 2Neurobiology and Anatomy, and 3Physical Medicine and Rehabilitation, University of Rochester School of Medicine and Dentistry, and the 4Brain Injury Rehabilitation Program, St. Mary’s Hospital, Rochester, New York 14642 Submitted 10 February 2003; accepted in final form 24 March 2003 The motor cortex and the corticospinal tract are crucial for the control of relatively independent finger movements (Porter and Lemon 1993). Lawrence and Kuypers (1968a) observed that after permanent lesions to the corticospinal tract, monkeys recovered the ability to use the upper limb when walking and climbing, but were left with an inability to move the fingers independently when retrieving food morsels and grooming. These early observations have been extended using more quantitative techniques, such as force recordings and electromyography (Hepp-Reymond and Wiesendanger 1972; Hepp-Reymond et al. 1974). More recently, similar deficits in fine finger movements have been produced temporarily by reversible inactivation of small portions of the primary motor cortical hand representation (Brochier et al. 1999; Kubota 1996; Schieber and Poliakov 1998). How relatively selective lesions of the motor cortex or corticospinal tract affect the independence of finger movements in humans has not been examined in detail, for two reasons. First, many studies of hand control after lesions to the motor system have used heterogeneous patients with relatively nonspecific lesions, and with a wide range of motor and nonmotor abnormalities (Carroll 1965; Wade et al. 1983). Pure motor hemiparesis, a relatively homogeneous clinical syndrome, is characterized by paresis on one side of the body without sensory, cognitive, or language disturbance (Fisher and Curry 1964; Fisher 1979, 1982). This syndrome most frequently results from relatively isolated ischemic lesions affecting the corticospinal tract unilaterally in the basis pontis or in the posterior limb of the internal capsule. Here, we investigated how lesions relatively restricted to the motor cortex or corticospinal tract affect independent finger movements by studying people with pure motor hemiparesis. Second, in reports where lesions have been restricted to the motor cortex or corticospinal tract, the capacity to move each finger independently has not been measured quantitatively. Most case reports provide only descriptive observations of finger strength or finger movements (Aguilar 1969; Back and Mrowka 2000; Kim et al. 2002; Lee et al. 1998; Phan et al. 2000; Ropper et al. 1979; Schieber 1999; Tereo et al. 1993). Fries and colleagues used a standardized clinical test of arm function (Fries et al. 1993), which provided a global score of arm and hand function but could not provide quantitative information about the fingers (Lincoln and Leadbitter 1979). Here, we used kinematic analyses to quantify the independence of each finger. We questioned whether damage to the motor cortex or corticospinal tract would impair the ability to move each finger to the same degree or would affect some fingers more than others. Although we expected that the independence of the thumb would be the most affected given its relative cortical magnification compared with the other fingers (Penfield and Boldrey 1937; Penfield and Rasmussen 1950; Woolsey et al. 1952), our results showed the opposite. In our subjects with residual pure motor hemiparesis, the independence of the thumb was normal; the independence of the index finger was slightly impaired, while the independence of the middle, ring, and little fingers was substantially impaired. Address for reprint requests: C. E. Lang, University of Rochester Medical Center, 601 Elmwood Ave., Box 603, Rochester, NY 14642 (E-mail: [email protected]). The costs of publication of this article were defrayed in part by the payment of page charges. The article must therefore be hereby marked ‘‘advertisement’’ in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. INTRODUCTION 1160 0022-3077/03 $5.00 Copyright © 2003 The American Physiological Society www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 Lang, Catherine E. and Marc H. Schieber. Differential impairment of individuated finger movements in humans after damage to the motor cortex or the corticospinal tract. J Neurophysiol 90: 1160 –1170, 2003; 10.1152/jn.00130.2003. The purpose of this study was to quantify the long-term loss of independent finger movements in humans with lesions relatively restricted to motor cortex or corticospinal tract. We questioned whether damage to the motor cortex or corticospinal tract would permanently affect the ability to move each finger to the same degree or would affect some fingers more than others. People with pure motor hemiparesis due to ischemic cerebrovascular accident were used as our experimental sample. Pure motor hemiparetic and control subjects were tested for their ability to make cyclic flexion/extension movements of each finger independently. We recorded their finger joint motion using an instrumented glove. The fingers of control subjects and of the unaffected hands (ipsilateral to the lesion) of hemiparetic subjects moved relatively independently. The fingers of the affected hands (contralateral to the lesion) of hemiparetic subjects were differentially impaired in their ability to make independent finger movements. The independence of the thumb was normal; the independence of the index finger was slightly impaired, while the independence of the middle, ring, and little fingers was substantially impaired. The differential long-term effects of motor cortical or corticospinal damage on finger independence may result from rehabilitative training emphasizing tasks requiring independent thumb and index movements, and from a greater ability of the spared components of the neuromuscular system to control the thumb independently compared with the other four fingers. DIFFERENTIAL FINGER MOVEMENT IMPAIRMENT AFTER STROKE METHODS Subjects TABLE affected hands of the hemiparetic group (see Table 1 for individual affected hemiparetic values). Although the z-scores appear to indicate severe impairment in some of the affected hands of hemiparetic subjects (Table 1), all subjects completed all the items on the test, and therefore, the high z-scores mainly reflect the increased time taken for task completion. In addition, four of our hemiparetic subjects (H-01, H-05, H-06, H-07, see Table 1) were evaluated with the upper extremity FuglMeyer scale (Fugl-Meyer et al. 1975). The Fugl-Meyer is a clinical rating scale that tests tendon reflexes and voluntary movements in and out of synergistic limb postures. Possible scores range from 0 to 66, where 66 means there was no observable deficit. Fugl-Meyer scores for these four subjects ranged from 64/66 (H-01) to 35/66 (H-07L). Arm function as measured by the Fugl-Meyer test was highly correlated with hand function as measured by the Jebsen Test (Pearson correlation ⫽ ⫺0.986, P ⫽ 0.015). For example, H-01 had a Jebsen z-score of 1.8 and a Fugl-Meyer score of 64/66. Likewise, H-07L had a Jebsen z-score of 24.6 and a Fugl-Meyer score of 35/66. For subsequent analyses examining relationships between function and finger independence, we used the Jebsen Test because we felt it was a better tool for evaluating the typical use of the hand. Experimental procedures To probe the function of the motor cortex and corticospinal tract in our subjects, we tested their ability to make individuated finger movements (i.e., their ability to move each finger while keeping the other fingers still). If possible, subjects with pure motor hemiparesis were tested on both the affected side, contralateral to lesion, and the unaffected side, ipsilateral to lesion. Two hemiparetic subjects were tested only on the affected side, H-01 (time constraints) and H-06 (MRI report of old lacune). For subject H-07 (bilateral internal capsule lesions), both sides were tested and both sets of data were included in the affected group. Control subjects were tested on one side only, except for one who was tested on both sides as a match for H-07. In sum, we evaluated 8 affected hands (6 right, 2 left), 4 unaffected hands (1 right, 3 left), and 10 control hands (6 right, 4 left). All of our control subjects and five of seven hemiparetic subjects reported being right-handed. Because previous work has shown that the ability to independently produce finger movements or finger forces is not different in the dominant versus nondominant hand (Hagar-Ross and Schieber 2000; Reilly and Hammond 2000), data from right and left hands were pooled for all analyses. Subjects were seated with the elbow and forearm on a table. The forearm was positioned in neutral pronation/supination and the wrist was positioned in approximately 15° extension. Figure 2A shows a schematic of the forearm and wrist supported and stabilized with a vacuum cast (VersaForm, Sammons Preston Inc., Bolingbrook, IL). Subjects wore a right- or left-handed instrumented glove (Cyber- 1. Characteristics of subjects with pure motor hemiparesis Subject Age Gender Lesion Locationa Time Since Stroke H-01 H-02 H-03 H-04 H-05 H-06 H-07L H-07R 70 72 66 55 71 65 49 49 M F M M M M F F L precentral gyrusc L corona radiata, descending fibers L basis pontis L basis pontis R basis pontise L internal capsule, posterior limbf L internal capsule, posterior limb R internal capsule, genu 34 months 29 months 7 months 2 months 21 months 25 months 2 months 19 months Initial Hemiparesis in: Face, Face, Face, Face, Face, Face, Face, Face, arm, arm, arm, arm, arm, arm, arm, arm, hand hand, hand, hand, hand, hand, hand, hand, leg leg leg leg leg leg leg Residual Hemiparesis in: Hand Arm, hand Arm, hand, Arm, hand, Arm, hand Arm, hand, Arm, hand, Arm, hand leg leg leg leg Jebsen Test z-Scoreb 1.8 ⫾ 0.7 (FM ⫽ 64/66)d 11.0 ⫾ 1.4 2.1 ⫾ 0.9 22.0 ⫾ 8.8 2.3 ⫾ 0.8 (FM ⫽ 58/66)d 15.9 ⫾ 3.8 (FM ⫽ 45/66)d 24.6 ⫾ 7.0 (FM ⫽ 35/66)d 3.4 ⫾ 1.0 Values are means ⫾ SE. L, left; R, right. a See Fig. 1 for magnetic resonance images for each subject. b z-Score compared to age-, gender-, and hand dominant-appropriate means on the Jebsen Test of Hand Function; higher scores reflect increased time to complete test items (see text for details). c Extends into white matter beneath. d Fugl-Meyer Upper Extremity scale was used to evaluate 4 hemiparetic subjects, normal arm function ⫽ 66. e Extends up into pontine tegmentum. f Extends into white matter above and into the posterior of the putamen. J Neurophysiol • VOL 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 Seven subjects with pure motor hemiparesis (age range 49 –72 yr, Table 1) and nine neurologically intact, control subjects (age range 19 –52 yr) participated in this study. The study protocol was approved by the Research Subjects Review Board of the University of Rochester Medical Center, Rochester, NY. Informed consent was obtained from all subjects prior to participation. Figure 1 shows the magnetic resonance image (MRI) that best illustrates the lesion that produced pure motor hemiparesis in each subject. Our sample consisted of five subjects with classic lesions (2 with unilateral lesions of the basis pontis and 3 with lesions in the posterior limb of the internal capsule) and findings of contralateral hemiparesis in the face, arm, and leg. We also included subjects with isolated lesions in the genu of the internal capsule (H-07R), in the corona radiata adjacent to the lateral ventricle (H-02), and in the precentral gyrus (H-01). Clinically, these three subjects presented with pure motor hemiparesis affecting the contralateral face, arm, and leg, except for H-01 (lesion to the precentral gyrus), who had only face and arm weakness. The MRI for H-06 showed signal changes consistent with old, asymptomatic lacunes in both the left and the right putamen in addition to the internal capsule lesion responsible for the hemiparesis. Another subject, H-07, had bilateral internal capsule lesions that occurred 17 mo apart. The lesion on the left side was in the middle portion of the posterior limb of the internal capsule. The lesion on the right side was in the genu of the internal capsule. Hemiparetic subjects underwent a clinical neurological examination to rule out sensory impairments and involvement of other motor system structures. As part of this examination, we evaluated light touch sensation of the hand using a five-filament mini-set (Semmes Weinstein, North Coast Medical, Campbell, CA) and evaluated kinesthesia of the wrist and fingers. Potential subjects with sensory or cognitive loss or movement disorders suggesting involvement of other motor structures were excluded from participation. At the time of testing, the hemiparetic subjects reported substantial recovery compared with the severity of their initial symptoms. Mild residual paresis persisted in most subjects, as indicated in Table 1. Functionally, all hemiparetic subjects could use a precision grip to hold a pen with the affected hand and could walk short distances with an assistive device. For five of eight subjects, hand function remained impaired as measured by the Jebsen Test of Hand Function (Jebsen et al. 1969), a standardized clinical test measuring timed performance on seven items that simulate common activities. The seven test items are as follows: 1) writing a sentence; 2) turning index cards; 3) picking up small objects; 4) using a spoon; 5) stacking checkers; 6) lifting light food cans; and 7) lifting heavy food cans. The mean Jebsen z-score was 1.6 ⫾ 0.2 (SE) for the control group, 3.53 ⫾ 0.94 for the unaffected hands of the hemiparetic group, and 10.4 ⫾ 3.3 for the 1161 1162 C. E. LANG AND M. H. SCHIEBER Data analysis Off-line, glove data were low-pass filtered at 6 Hz. We used data from 14 of the 22 glove sensors: metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) sensors for the index, middle, and ring fingers (9 sensors), MCP and PIP for the little finger (2 sensors), and MCP, PIP, and opposition sensors for the thumb (3 sensors). The thumb opposition sensor best captured the movement about the carpometacarpal (CMC) joint in the flexion/ extension plane of the thumb phalanges. Sensor data were transformed FIG. 1. Magnetic resonance images (MRIs) illustrating lesions in subjects with pure motor hemiparesis. Each lesion (white) is emphasized by a surrounding black circle. Images are presented such that the left side of the brain appears on the right side of the page. Axial, flair images, obtained at initial presentation of symptoms, are shown for all hemiparetic subjects except H-04, for whom an axial, diffusion-weighted image is shown. Lesion locations were as follows. H-01: left precentral gyrus extending into white matter beneath; H-02: left corona radiata, descending fibers adjacent to the lateral ventricle; H-03: left basis pontis; H-04: left basis pontis; H-05: right basis pontis, extending into the pontine tegmentum above; H-06: left internal capsule, posterior limb, extending into white matter above and into the posterior putamen anteriorly, also note a small fluid filled cyst in the left putamen, just anterior to the new lesion, consistent with an old lacune; H-07L: left internal capsule, posterior limb; H-07R: right internal capsule, genu. Glove, Virtual Technologies, Palo Alto, CA). Prior to testing, glove sensor output and goniometric joint measurements were obtained in standard positions to calibrate the glove sensors for each tested hand (Hager-Ross and Schieber 2000). Glove sensor output was linearly related to joint position for all sensors except the little finger distal J Neurophysiol • VOL FIG. 2. A: schematic of testing position. B: definitions of joint angles and (X, Y) coordinate frames for the 4 fingers. For the thumb, joint angles are defined in the same manner and the carpometacarpal (CMC) joint is defined as (0, 0). 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 interphalangeal (DIP) sensor. Our calibrations indicated that the little finger DIP sensor data did not accurately reflect movement of the little finger DIP joint; thus data from this sensor were not used. Spike2 software and a Micro 1401 interface (Cambridge Electronic Design, Cambridge, UK) were used to collect glove data, with each sensor sampled at 78 Hz. Subjects were asked to make cyclic flexion-extension movements of one finger at a time. We instructed them to move one finger, at a “comfortable pace,” through a “comfortable range of motion,” and to keep the other fingers still. In general, the noninstructed fingers tended to remain in a relaxed, flexed posture during motion of an instructed finger. The hand was in full view of the subject at all times so they were able to see the movements of the instructed and noninstructed fingers. Subjects practiced each movement prior to recording trials to be sure that they understood the task and the instructions. All subjects reported an awareness of movement in the noninstructed fingers when it occurred. After practicing an instructed movement, a 10-s trial was recorded. We recorded two consecutive trials for each instructed finger. The order of instructed fingers was varied between subjects. DIFFERENTIAL FINGER MOVEMENT IMPAIRMENT AFTER STROKE 冋冉冘 n II j ⫽ 1 ⫺ 册冒 兩Dij兩⫺1 i⫽1 共n⫺1) where IIj is the individuation index the jth finger, Dij is the normalized path distance of the ith finger during the jth instructed movement, and n is the number of fingers (here n ⫽ 5). One is subtracted from the sum of the normalized path distances in the numerator and from n in the denominator to remove the normalized path distance of the instructed finger itself. The individuation index will be close to 1 for an ideally individuated movement in which the instructed finger moves with no movement of noninstructed fingers and closer to 0 the more noninstructed finger movement occurs simultaneously with instructed finger movement. The stationarity index is a measure of how well a finger is able to remain motionless, when it is not the instructed finger. The stationarity index was calculated as 1 minus the average normalized path distance of that finger whenever it was the noninstructed finger, or 冋冉冘 册冒 m SI i ⫽ 1 ⫺ 兩Dij兩 ⫺ 1 共m ⫺ 1兲 j⫽1 where SIi is the stationarity index for the ith finger during the m instructed movements. One is subtracted from the sum of the normalJ Neurophysiol • VOL ized path distances in the numerator and from m in the denominator to remove the normalized path distance of the ith finger when it was instructed. The stationarity index will be close to 1 for a finger that remains stationary whenever it is the noninstructed finger and closer to 0 the more the finger moves when it is a noninstructed finger. We compared individuation indices and stationarity indices using 3 ⫻ 5 analyses of variance (ANOVAs) to look for differences between groups (control, affected hand, nonaffected hand) and between fingers (thumb, index, middle, ring, and little). All statistical tests were performed using Prism (GraphPad Software, San Diego, CA) and significance levels were set at P ⬍ 0.05. When significant effects were found in the ANOVAs, means were evaluated using t-test, with Bonferroni error corrections for multiple comparisons. Additionally, we looked for relationships between function of the hand (as measured by the Jebsen Test of Hand Function z-score) and the independence of each finger (as measured by the individuation index) using Spearman rank correlation coefficients. All of the analyses on the individuation index data yielded the same statistical results and inferences as the analyses on the stationarity index data. We therefore present only the individuation index data in RESULTS. Two other kinematic variables were also investigated. First, to test whether differences in indices could be explained by rate of movement, we calculated and compared movement frequency for each finger during its instructed movement. Second, to test whether differences in indices could be explained by range of movement, we calculated and compared maximum joint excursions for each finger during its instructed movement. These variables were compared using ANOVAs. RESULTS We tested 8 affected hands, 4 unaffected hands, and 10 control hands. MRIs (Fig. 1) illustrate the lesions of the motor cortex or corticospinal tract that caused paresis in the affected hands. Sensory testing revealed that no hands (in any group) had deficits in the modalities of light touch or kinesthesia. Clinical neurological testing showed that the affected hand/side of the hemiparetic subjects exhibited signs consistent with motor cortical or corticospinal tract damage (e.g., hyperreflexia, residual weakness on one side of the body) and did not exhibit signs (e.g., ataxia, tremor), suggesting involvement of other motor structures. Fingers of the affected hands of hemiparetic subjects moved less independently than fingers of control hands and of unaffected hands. Figure 3 shows plots of joint position versus time for a control hand, and the affected and unaffected hands of a hemiparetic subject (H-03) during a single trial of instructed ring finger movement. All three hands showed movement of the instructed ring finger, as expected. The affected hand (middle column) showed greater movement of the noninstructed fingers (thumb, index, middle, and little) compared with the control and unaffected hands. Figure 4 shows plots of fingertip position and the corresponding normalized path distance for the unaffected (Fig. 4A) and affected hand (Fig. 4B) of a hemiparetic subject (H-02) during single trials of instructed movement of each finger. Fingertip position is shown on the left and normalized path distance is shown on the right for each hand. The top row shows instructed thumb movement, followed by the instructed movements of the index, middle, ring, and little (bottom) fingers in descending order. Movement of the fingertips are color-coded similar to a rainbow, such that red ⫽ thumb, orange ⫽ index, yellow ⫽ middle, green ⫽ ring, and blue ⫽ little. Horizontal bars in each plot of normalized path distance 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 into joint angles, using the offset and gain values for each sensor for each subject as derived from calibration procedures. We defined the finger joint angles such that 0° at each joint was a straight finger; positive numbers indicated flexion (curled finger), and negative numbers indicated hyperextension (Fig. 2B). Finger segment lengths (measured from hand tracings) and joint angles were used to calculate fingertip position in the flexion/extension plane of each finger. Fingertip position was defined such that the origin of the x- and y-axes was at the center of the MCP joint for each of the four fingers (Fig. 2B) and at the CMC joint for the thumb. Our laboratory has previously used relative motion slopes to quantify the movement of the noninstructed fingers compared with the instructed fingers (Hagar-Ross and Schieber 2000; Schieber 1991). This methodology works well when the relative motion between a pair of fingers is linear (i.e., when plotting the motion of one finger vs. the motion of the other finger, the result is a straight line). For the majority of finger pairs in the current data, the relative motion between a pair of fingers was best described by a nonlinear function. This may be due to the fact that our subjects were moving through greater excursions at each joint compared with monkeys (Schieber 1991) and compared with previously studied normal human subjects (Hagar-Ross and Schieber 2000). At larger joint excursions, biomechanical coupling between the digits may have a greater effect on the linearity of the motion between pairs of digits and on the independence of finger movements. Therefore to determine the relative motion of instructed versus noninstructed fingers, we used the normalized path distance. We defined the average path distance as the total distance a fingertip traveled during the 10-s trial divided by the number of completed cycles, where one cycle was considered flexion and extension of the finger (Fig. 2B). The average path distance was calculated for each fingertip during each 10-s trial. The average path distance values were normalized by dividing the values by the average path distance of that finger when it was the instructed finger. Thus the normalized path distance equals 1 when a finger is the instructed finger and is usually ⬍1 when it is a noninstructed finger. We then used the normalized path distances to derive two indices to quantify finger independence, the individuation index and the stationarity index (Schieber 1991). The individuation index is a measure of how well a finger is able to move independently (i.e., without the other fingers moving). The individuation index was calculated as 1 minus the average normalized path distances of the noninstructed fingers, or 1163 1164 C. E. LANG AND M. H. SCHIEBER are ordered: thumb (top), index, middle, ring, and little (bottom). The instructed finger always has a normalized path distance of 1 (see METHODS). The unaffected hand (Fig. 4A) showed little movement of the noninstructed fingers. For example, during instructed middle finger movement in the unaffected hand (middle row of Fig. 4A), the normalized path distances of the noninstructed thumb, index, ring, and little fingers are all ⬍0.1. The small amount of movement in the noninstructed fingers in Fig. 4A was similar to that in our control subjects and to data from previously reported normal subjects (Hagar-Ross and Schieber 2000). In comparison, the affected hand (Fig. 4B) showed substantial movement of the noninstructed fingers, particularly during the instructed movements of the middle, ring, and little fingers. This can be seen in the traces of fingertip position and in the normalized path distance plots. For example, during instructed middle finger movement in the affected hand (middle row of Fig. 4B), the normalized path distance of the ring finger was also equal to 1, indicating that the ring finger moved as much during instructed middle finger movements as it did during instructed ring finger movements. An ideally independent finger would move without any accompanying motion of the other fingers. We used the individuation index to quantify the degree to which the noninstructed fingers moved when they were supposed to be still (see METHODS). The individuation index will be 1 for an instructed finger that moves alone and will be closer to 0 the more the J Neurophysiol • VOL noninstructed fingers move. Figure 5A shows the individuation indices for hemiparetic subject H-02. The unaffected hand had individuation indices around 0.9. On the affected hand, the thumb had an individuation index of 0.907, but the index, middle, ring, and little fingers had individuation indices that were much lower, 0.706, 0.593, 0.447, and 0.639, respectively. This subject illustrates a finding typical of the affected hands: the individuation index of the thumb was normal, and the individuation index of the index finger was slightly below normal, while the individuation indices for the middle, ring, and little fingers were substantially below normal. Figure 5B shows group individuation indices (mean ⫾ SE) for each finger. The control group and the unaffected group had mean individuation indices around 0.9, indicating that the fingers on these hands moved almost independently. The individuation indices of the affected hands were normal for the thumb but were substantially lower in the more ulnar fingers, indicating that the noninstructed fingers moved more during instructed movement of the more ulnar fingers. A 3 ⫻ 5 (group ⫻ finger) ANOVA revealed a significant group ⫻ finger interaction (P ⬍ 0.0001). Post-hoc testing showed no differences existed between the control and unaffected groups or between their fingers (P ⬎ 0.05). The affected group had individuation indices for the thumb that were not significantly different from the control and unaffected groups (P ⫽ 0.831). The affected group individuation indices for the index, middle, ring, and little fingers were significantly lower than the control 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 FIG. 3. Single trials of joint position vs. time for a control (left), and the affected (middle), and unaffected hand (right) of a hemiparetic subject (H-03). The ring finger was instructed to move during these 3 trials. Joint traces from the thumb are on top, followed by the index, middle, ring, and little (bottom) fingers in descending order. The thick line shows metacarpophalangeal (MCP) movement; the thin line shows proximal interphalangeal (PIP) movement, and the dotted line shows distal interphalangeal (DIP) movement. For the thumb, the dotted line shows CMC movement. Although little finger DIP data were not used in our analysis (see METHODS), we show little finger DIP motion here because the little finger DIP sensor accurately transduced DIP movement in these 3 hands, due to the size of the hands and the fit of the instrumented glove. DIFFERENTIAL FINGER MOVEMENT IMPAIRMENT AFTER STROKE 1165 and unaffected groups (Pindex ⫽ 0.017, Pmiddle ⫽ 0.003, Pring ⫽ 0.0002, Plittle ⫽ 0.0001). The finding of relatively normal individuation of the thumb compared with the other four fingers was consistent across hemiparetic subjects. Individuation indices for each affected hand and means for each group are provided in Table 2. The thumb moved relatively independently for the subject with damage to the motor cortex (H-01) and for subjects with damage to the corticospinal tract in the internal capsule (e.g., H-06) or in the pons (e.g., H-04). An interesting observation in our data was that hemiparetic subject H-07R, who had damage to the genu of the internal capsule, also had relatively normal independence of the thumb and pronounced deficits in the other four fingers. The individuation index data show that damage relatively restricted to the motor cortex or to the corticospinal tract impaired the ability to make independent finger movements. The affected fingers were not uniformly impaired, however. The independence of the thumb was normal, and the indepenJ Neurophysiol • VOL dence of the index finger was slightly impaired, while the independence of the middle, ring, and little fingers was the most impaired. Relationships between finger independence and function We next asked whether the ability to make individuated finger movements was related to function. Subjects that had greater functional deficits (higher Jebsen z-scores) were generally the same subjects that moved their fingers less independently. We therefore used nonparametric Spearman rank-order correlations to look for relationships, in the entire data set, between finger independence, as measured by the individuation index, and hand function, as measured by the Jebsen Test of Hand Function (see METHODS). Our data indicated that hand function was related to finger independence. Spearman r values between the Jebsen z-score and the individuation index for each finger were ⫺0.528 for the thumb (P ⫽ 0.012), ⫺0.516 for the index finger (P ⫽ 0.014), ⫺0.431 for the middle finger 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 FIG. 4. Single trials of fingertip position and normalized path distance for instructed movements of each finger for the unaffected (A) and affected hand of a hemiparetic subject (H-02). Fingertip position (cm) is shown on the left and normalized path distance is shown on the right for each hand. The top row shows instructed thumb movement, followed by the instructed movements of the index, middle, ring, and little (bottom) fingers. Movement of the fingertips are color-coded similar to a rainbow, such that red ⫽ thumb, orange ⫽ index, yellow ⫽ middle, green ⫽ ring, and blue ⫽ little. Horizontal bars in each plot of normalized path distance are ordered: thumb (top), index, middle, ring, little (bottom). 1166 C. E. LANG AND M. H. SCHIEBER expected because the Jebsen test items require wrist, forearm, elbow, and shoulder control as well as finger control. Frequency and range of movement (P ⫽ 0.045), ⫺0.538 for the ring finger (P ⫽ 0.010), and ⫺0.507 for the little finger (P ⫽ 0.016). Note that the relationships are negative because a lower Jebsen z-score signifies better hand function. The r values show small-to-moderate correlations, indicating that other variables, in addition to finger independence, would be needed to accurately describe hand function. The fact that other variables are needed is TABLE 2. Individuation indices for each affected hand and means for each group Subject H-01 H-02 H-03 H-04 H-05 H-06 H-07L H-07R Group Affected (n ⫽ 8) Control (n ⫽ 10) Unaffected (n ⫽ 4) Thumb Index Middle Ring Little 0.851 0.907 0.837 0.899 0.798 0.847 0.914 0.849 0.886 0.706 0.666 0.875 0.797 0.683 0.812 0.738 0.623 0.593 0.619 0.753 0.694 0.339 0.702 0.331 0.668 0.447 0.663 0.727 0.641 0.567 0.405 0.735 0.688 0.639 0.830 0.693 0.708 0.667 0.630 0.697 0.862 ⫾ 0.015 0.936 ⫾ 0.010 0.851 ⫾ 0.042 0.770 ⫾ 0.030 0.888 ⫾ 0.023 0.880 ⫾ 0.023 0.582 ⫾ 0.057 0.882 ⫾ 0.017 0.839 ⫾ 0.027 0.607 ⫾ 0.044 0.892 ⫾ 0.016 0.890 ⫾ 0.020 0.694 ⫾ 0.022 0.896 ⫾ 0.016 0.879 ⫾ 0.019 Values are means ⫾ SE. J Neurophysiol • VOL 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 FIG. 5. A: individuation indices for each finger for the affected (filled triangles) and unaffected (filled circles) hand of the same hemiparetic subject (H-02) shown in Fig. 4. Each data point is the mean of 2 trials. B: individuation indices for each finger for the control (open circles), affected (filled triangles), and unaffected (filled circles) groups. Each data point is the group mean ⫾ SE. Our subjects were told to move the instructed finger “at a comfortable pace, through a comfortable range” (see METHODS). During practice of each movement prior to a recording, subjects had the opportunity to experience different movement frequencies and different ranges of joint motion that they felt would best meet the requirements of the task (i.e., “move one finger, while keeping the others still”). Thus each subject’s data presumably reflect their best ability to make individuated movements at each finger. Because we tested only the selfselected movement frequencies and joint excursions, we are unable to determine whether the pattern of differential deficits and the magnitude of these deficits would be the same at other movement frequencies or other joint excursions. We did, however, examine the self-selected frequencies and joint excursions to see if they could account, in part, for our results. To exclude the possibility that self-selected movement frequency could account for some of the impairments in independent finger movement seen in our affected hands, we compared movement frequencies between fingers and between groups. Figure 6A shows movement frequencies (mean ⫾ SE) for each group. Instructed fingers were moved cyclically back and forth at a rate of approximately 0.7 Hz. Within each group, the range of frequencies was large. Frequencies ranged from 0.21 to 1.21 Hz in the control group, 0.32 to 1.24 Hz in the unaffected group, and 0.21 to 2.74 Hz in the affected group. Although the movement frequencies chosen by our subjects appear rather slow, the fingers moved through ⬎50% of the available range at each joint and average joint speeds were well within the typical ranges used during functional tasks of the hand and fingers in normal subjects (C. E. Lang, unpublished observations). Interestingly, most of the variance in self-selected frequency could be attributed to differences between subjects (⬎70%), while only a small portion (12%) could be attributed to differences within subjects (i.e., within the five fingers of one hand). Thus subjects in all three groups appeared to select a particular frequency and move each finger near that frequency. The self-selected movement frequencies were not significantly different among the five fingers and three groups (P ⬎ DIFFERENTIAL FINGER MOVEMENT IMPAIRMENT AFTER STROKE 1167 DISCUSSION FIG. 6. A: movement frequencies for instructed movement of each finger. B: joint excursions for instructed movement of each finger. Data points are group means ⫾ SE. The control group is shown with open circle; the affected group is shown with filled triangles, and the unaffected group is shown with filled circles. 0.05) nor did we find any relationship between self-selected frequencies and finger individuation indices in the affected group (Spearman rank-order correlations, thumb ⫽ ⫺0.095, index ⫽ 0.276, middle ⫽ ⫺0.429, ring ⫽ 0.323, and little ⫽ J Neurophysiol • VOL Asking subjects to move each finger by itself, we probed a crucial function of the motor cortex and corticospinal tract. Our results were obtained from subjects who reported substantial recovery from their initial hemiparesis and who were tested several months to several years after the lesion occurred. Independent finger movements were differentially impaired in humans with lesions relatively restricted to the motor cortex or corticospinal tract. In the affected hands, the independence of the thumb was normal, and the independence of the index finger was slightly impaired, while the independence of the middle, ring, and little fingers was substantially impaired. The lesions in our hemiparetic subjects all disrupted the wellknown pathway of the corticospinal system; lesions were located in the motor cortex itself, in the corona radiata adjacent to the posterior body of the lateral ventricle, in the internal capsule, or in the basis pontis. Although we found no clinical signs of involvement of other structures, lesions in the present subjects may have included subclinical damage to additional pathways. For example, unilateral lesions in the basis pontis may have damaged portions of the pontine nuclei. Likewise, lesions in the internal capsule may have damaged thalamocortical fibers. Nevertheless, the observed pattern of impairments was consistent across subjects. We infer that the differential pattern of impairments in finger independence resulted predominately from damage to the motor cortex or the corticospinal tract. The differential deficits in our hemiparetic subjects presumably reflect corticospinal function for which spared components of the neuromuscular system could not compensate. We therefore consider several factors that might have contributed to the normal independence of the thumb and the diminished independence of the more ulnar fingers: 1) structural independence, 2) incomplete lesions, and 3) recovery of function. Possible explanations for the normal independence of the thumb The normal independence of the thumb may be partially explained by the architecture of the hand and forearm. The thumb is the most structurally independent digit. All the muscles which move the thumb act on no other digits, while each of the other four 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 0.276, all P values ⬎0.05). We conclude that movement frequency could not account for the differences in individuation indices described above. We also considered the possibility that the self-selected range through which the instructed fingers moved could account for some of the impairments seen in our affected hands. Figure 6B shows joint excursions (mean ⫾ SE) during instructed finger movement for each group. Joint excursions of the instructed fingers were not significantly different among the three groups (P ⬎ 0.05). The plots in Fig. 6B illustrate that the most excursion typically occurred at the PIP joint of each finger (approximately 85°), followed by the MCP joint (approximately 55°), and then the DIP joint (approximately 20°). The thumb shows a slightly different pattern with similar excursions occurring at the MCP and IP joints (approximately 55°), and a smaller excursion occurring at the CMC joint (approximately 30°). Thus these data indicate that the impairments in independent finger movements in the affected hands cannot be explained by differences in self-selected joint excursions. 1168 C. E. LANG AND M. H. SCHIEBER J Neurophysiol • VOL immediate days and weeks after the lesion occurs, then somatopically complete, but partial tissue damage might account for the deficits observed here. Rehabilitation, plasticity, and compensation might explain the differential impairments Clinical observations suggest that patients with pure motor hemiparesis typically have uniform involvement of all the fingers in the affected hand in the first hours and days after their stroke (M. H. Schieber, unpublished observations). Although longitudinal quantitative data on the recovery of finger independence are not available on the present subjects, we consider the possibility that the thumb recovered independence more than the other fingers. All of our hemiparetic subjects received extensive rehabilitation services after their stroke. After stroke, rehabilitative training of the upper extremity generally focuses on functional use of the hand and fingers. Common tasks such as picking small objects off the table, buttoning a shirt, or writing require more independent control of the thumb and index finger than of the middle, ring, and little fingers. Thus the differential impairments we observed may be explained in part by practice-induced recovery during the rehabilitation process that emphasized tasks requiring independent movements of the index finger and thumb. Repetition of tasks requiring independent thumb and index finger movements could lead to plastic changes in the primary motor cortex, compensation by other descending pathways, and/or compensation by nonprimary cortical motor areas. Task-specific training (Nudo et al. 1996a), ischemic lesions (Nudo and Milliken 1996), and ischemic lesions plus taskspecific training (Nudo et al. 1996b) all induce plastic changes in the primary motor cortex hand and forearm representation in nonhuman primates. In humans with hemiparesis due to corticospinal tract lesions, primary motor cortex activation is preserved and the magnitude of activation is similar to healthy control subjects (Cramer et al. 2002). Our hemiparetic subjects had sufficient time and task-specific training after their injuries for plastic changes to occur in the hand and forearm representation of the primary motor cortex. If rehabilitative training emphasized independent thumb and index finger movements, the thumb and index finger representation in the primary motor cortex might have expanded at the expense of the representations of the more ulnar fingers. If the crossed corticospinal tract were destroyed completely, how might plastic reorganization in the primary motor cortex contribute to recovery of function? Descending pathways other than the crossed corticospinal tract may provide alternate routes for motor commands to reach the spinal cord (Fries et al. 1991; Kuypers 1987; Woolsey et al. 1972). An intact ipsilateral corticospinal tract may contribute to functional recovery after stroke (Cao et al. 1998; Fisher 1992), although ipsilateral axons are likely to exert more control over proximal rather than distal musculature (Colebatch and Gandavia 1989; Kuypers and Brinkman 1970). The rubrospinal tract and the reticulospinal tract, which both receive input from the motor cortex, also have been implicated in recovery of function after pyramidal tract lesions in nonhuman primates (Belhaj-Saif and Cheney 2000; Kuypers 1982; Lawrence and Kuypers 1968a,b). Although the extent of the rubrospinal tract and its relative importance in humans remain unclear (Nathan and Smith 1982), we cannot 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 fingers is moved, in large part, by multitendoned muscles (i.e., flexor digitorum profundus, flexor digitorum superficialis, and extensor digitorum communis). Physiologic and anatomical evidence in humans suggest that these multitendoned muscles may not be fully compartmentalized to exert force on just one finger at a time (Kilbreath and Gandevia 1994; Kilbreath et al. 2002; Reilly and Schieber 2001, 2002; Segal et al. 2002). Biomechanically, the finger web space and the connections between tendons (e.g., juncturae tendinum of the extensor tendons) place greater restrictions on independent movement of the index, middle, ring, and little fingers than of the thumb (Austin et al. 1989; Gonzalez et al. 1997; Von Schroeder et al. 1990; Von Schroeder and Botte 1993). Thus due to the architecture of the hand itself, any surviving neural control may be able to move the thumb more independently than the other digits. Given that the motor cortex and corticospinal tract are believed to have a greater influence on the thumb than on the other fingers (Penfield and Boldrey 1937; Penfield and Rasmussen 1950; Woolsey et al. 1952), we did not expect the independence of the thumb to be normal in patients recovering from pure motor hemiparesis. The possibility exists that the normal independence of the thumb was due to incomplete lesions of the hand representation in the motor cortex or the corticospinal tract. Incomplete lesions can take the two following forms: 1) the tissue affected by the lesion was destroyed completely, but the lesion failed to affect the entire hand representation; or 2) the tissue affected by the lesion included the entire hand representation but the lesion damaged the tissue only partially. In the first scenario, a portion of the hand representation in the motor cortex or corticospinal tract might have been completely destroyed, but that destroyed portion did not contain all the neurons or axons controlling the thumb. One hemiparetic subject (H-01) had a lesion relatively restricted to the hand knob of the motor cortex (Yousry et al. 1997). He initially had paresis of the face and hand, with only mild paresis of the arm. We cannot rule out the possibility that his lesion permanently damaged the portion of the motor cortex representing the more ulnar digits and spared the portion representing more radial digits, as has been reported previously (Kim et al. 2002; Phan et al. 2000; Schieber 1999; Takahashi et al. 2002). Involvement of the face makes this possibility unlikely, however, because the thumb representation would be expected to lie between the representation of the more ulnar fingers and the representation of the face. For the other seven hands affected by subcortical lesions, hemiparesis uniformly involved the face, arm, and leg, making selective sparing of axons controlling the thumb quite unlikely. Thus lesions that completely destroyed the affected tissue while sparing the representation of the thumb are unlikely to account for the differential impairments observed here. In the second scenario, the entire hand representation in the motor cortex or corticospinal tract might have been damaged, but the damage would have been only partial. If the thumb normally has a greater representation in the motor cortex and the corticospinal tract compared with the other four fingers, then partial damage would spare more neurons and/or axons controlling the thumb. Although we find it unlikely that such partial damage would yield the same consistent pattern of differential impairments across our hemiparetic subjects, we do not have data to exclude this possibility. Future studies can test this possibility by measuring finger independence shortly after lesions occur. If the independence of the thumb is normal in the DIFFERENTIAL FINGER MOVEMENT IMPAIRMENT AFTER STROKE J Neurophysiol • VOL The authors thank K. T. Reilly for helpful suggestions throughout this project. DISCLOSURES This work was supported by National Institute of Neurological Disorders and Stroke Grants F32 NS-44584 and R01 NS-27686. REFERENCES Aguilar MJ. Recovery of motor function after unilateral infarction of the basis pontis. Am J Phys Med 48: 279 –288, 1969. Austin GJ, Leslie BM, and Ruby LK. Variations of the flexor digitorum superficialis of the small finger. J Hand Surg [Am] 14: 262–267, 1989. Axer H and Keyserlingk DG. Mapping of fiber orientation in human internal capsule by means of polarized light and confocal scanning laser microscopy. J Neurosci Methods 94: 165–175, 2000. Back T and Mrowka M. Infarction of the “hand knob” area. Neurology 57: 1143, 2000. Belhaj-Saif A and Cheney PD. Plasticity in the distribution of the red nucleus output to forearm muscles after unilateral lesions of the pyramidal tract. J Neurophysiol 83: 3147–3153, 2000. Brochier T, Boudreau M-J, Pare M, and Smith AM. The effects of muscimol inactivation of small regions of motor and somatosensory cortex on independent finger movements and force control in the precision grip. Exp Brain Res 128: 31– 40, 1999. Cao Y, D’Olhaberriague L, Vikingstad EM, Levine SR, and Welch KMA. Pilot study of functional MRI to assess cerebral activation of motor function after poststroke hemiparesis. Stroke 29: 112–122, 1998. Carroll D. Hand function in hemiplegia. J Chronic Dis 18: 493–500, 1965. Colebatch JG and Gandavia SC. The distribution of muscular weakness in upper motor neuron lesions affecting the arm. Brain 112: 749 –763, 1989. Cramer SC, Mark A, Barquist K, Nhan H, Stegbauer KC, Price R, Bell K, Odderson IR, Esselman P, and Maravilla KR. Motor cortex activation is preserved in patients with chronic hemiplegic stroke. Ann Neurol 52: 607– 616, 2002. Dum RP and Strick PL. Spinal cord terminations of the medial wall motor areas in Macaque monkeys. J Neurosci 16: 6513– 6525, 1996. Ehrsson HH, Kuhtz-Buschbeck JP, and Forssberg H. Brain regions controlling non-synergistic versus synergistic movement of the digits: a functional magnetic resonance imaging study. J Neurosci 22: 5074 –5080, 2002. Fisher CM. Capsular infarcts: the underlying vascular lesions. Arch Neurol 36: 65–73, 1979. Fisher CM. Lacunar strokes and infarcts: a review. Neurology 32: 871– 876, 1982. Fisher CM. Concerning the mechanism of recovery in stroke hemiplegia. Can J Neurol Sci 19: 57– 63, 1992. Fisher CM and Curry HB. Pure motor hemiplegia. Trans Am Neurol Assoc 89: 94 –97, 1964. Fries W, Danek A, Scheidtmann K, and Hamburger C. Motor recovery following capsular stroke: role of descending pathways from multiple motor areas. Brain 116: 369 –382, 1993. Fries W, Danek A, and Witt TN. Motor responses after transcranial electrical stimulation of cerebral hemispheres with a degenerated pyramidal tract. Ann Neurol 29: 646 – 650, 1991. Fugl-Meyer AR, Jaasko L, Leyman I, Olsson S, and Steglind S. The post-stroke hemiplegic patient. I. A method for evaluation of physical performance. Scand J Rehab Med 7: 13–31, 1975. Gonzalez MH, Whittum J, Kogan M, and Weinzweg N. Variations of the flexor digitorum superficialis tendon of the little finger. J Hand Surg [Br] 22: 277–280, 1997. Hager-Ross CK and Schieber MH. Quantifying the independence of human finger movements: comparisons of digits, hands, and movement frequencies. J Neurosci 20: 8542– 8550, 2000. Hepp-Reymond M-C, Trouche E, and Wiesendanger M. Effects of unilateral and bilateral pyramidotomy on a conditioned rapid precision grip in monkeys (Macaca fascicularis). Exp Brain Res 21: 519 –527, 1974. Hepp-Reymond M-C and Wiesendanger M. Unilateral pyramidotomy in monkeys: effect on force and speed of a conditioned precision grip. Brain Res 36: 117–131, 1972. Jebsen RH, Taylor N, Trieschman RB, Trotter MJ, and Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil 50: 313–319, 1969. 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 rule out contributions from this pathway. The reticulospinal tract appears to descend at least to the thoracic spinal cord in man (Nathan et al. 1996) and has been hypothesized to assist, along with the ipsilateral corticospinal tract, in the recovery of function after partial cordotomy (Nathan and Smith 1973) and capsular stroke (Fries et al. 1991). If these alternate descending tracts do contribute to recovery of function in humans, then the present results suggest that more independent control of the thumb and index fingers than of the more ulnar digits may be achieved over these pathways. Besides the primary motor cortex, nonprimary cortical motor areas may also contribute to recovery of hand function. Premotor, supplementary, and cingulate motor areas contain representations of the hand and forearm, are interconnected with the primary motor cortex, and send corticofugal projections to subcortical centers, including the spinal cord (see, for review, Passingham 1997; Picard and Strick 2001; Rizzolatti et al. 1998). Although it has not been documented in neurophysiological studies, the possibility exists that the thumb might have a greater representation than the other digits in these areas, as it does in the primary motor cortex. When the thumb is moved independently of the other fingers, premotor, supplementary motor, and cingulate motor areas are more active than when the thumb is moved synergistically with the other fingers, as shown in a recent imaging study (Ehrsson et al. 2002). Other imaging studies indicate that premotor and supplementary motor areas may be more active during finger movements in hemiparetic subjects compared with control subjects (Seitz et al. 1998; Weiller et al. 1992, 1993). Neurons in nonprimary cortical motor areas are more frequently related to bilateral movements than neurons in the primary motor cortex (Tanji et al. 1988) and thus may be able to exert control via an intact ipsilateral corticospinal tract. Additionally, axons from the nonprimary cortical motor areas project to the contralateral spinal cord via a more anterior route through the internal capsule compared with the primary motor cortex axons (Axer and Keyserlink 2000; Fries et al. 1993; Morecraft et al. 2002) and these more anterior axons may have been spared in some of our hemiparetic subjects. Our subject with damage to the genu of the internal capsule (H-07R) had finger impairments that were similar to other hemiparetic subjects. This case supports the idea that nonprimary cortical motor areas also play a role in the control of independent finger movements. Although the functional significance of the spinal connections from the nonprimary cortical motor areas is still controversial (Dum and Strick 1996; Maier et al. 2002; Rouiller et al. 1996), these areas may have contributed to the differential impairments in finger independence seen here. In sum, our results show that independent finger movements were differentially impaired in humans with substantial recovery from motor cortical or corticospinal tract damage. The independence of the thumb was normal, and the independence of the index finger was slightly impaired, while the independence of the middle, ring, and little fingers was substantially impaired. We hypothesize that the differential impairments remaining after damage to the motor cortex or corticospinal tract may result from rehabilitative training emphasizing tasks requiring independent thumb and index movements, and from a greater ability of the spared components of the neuromuscular system to control the thumb independently compared with the other four fingers. 1169 1170 C. E. LANG AND M. H. SCHIEBER J Neurophysiol • VOL Reilly KT and Schieber MH. Prog No. 938.3. Electromyographic activity of functional subdivisions in human multitendoned finger muscles. Abstract Viewer and Itinerary Planner. Washington, DC: Soc Neurosci CD-ROM, 2001. Reilly KT and Schieber MH. Prog No. 768.17. The functional distribution of force by motor units in the human FDP. Abstract Viewer and Itinerary Planner. Washington, DC: Soc Neurosci CD-ROM, 2002. Rizzolatti G, Luppino G, and Matelli M. The organization of the cortical motor system: new concepts. Electroencephalogr Clin Neurophysiol 106: 283–296, 1998. Ropper AH, Fisher CM, and Kleinman GM. Pyramidal infarction in the medulla: a cause of pure motor hemiplegia sparing the face. Neurology 29: 91–95, 1979. Rouiller EM, Moret V, Tanne J, and Boussaoud D. Evidence for direct connections between the hand region of the supplementary motor area and cervical motoneurons in the Macaque monkey. Eur J Neurosci 8: 1055– 1059, 1996. Schieber MH. Individuated finger movements of Rhesus monkeys: a means of quantifying the independence of the digits. J Neurophysiol 65: 1381–1391, 1991. Schieber MH. Somatotopic gradients in the distributed organization of the human primary motor cortex hand area: evidence from small infarcts. Exp Brain Res 128: 139 –148, 1999. Schieber MH. Constraints on somatotopic organization in the primary motor cortex. J Neurophysiol 86: 2125–2143, 2001. Schieber MH and Poliakov AV. Partial inactivation of the primary motor cortex hand area: effects on individuated finger movements. J Neurosci 18: 9038 –9054, 1998. Segal RL, Catlin PA, Krauss EW, Merick KA, and Robilotto JB. Anatomical partitioning of three human forearm muscles. Cells Tissues Organs 170: 183–197, 2002. Seitz RJ, Hoflich P, Binkofski F, Tellmann L, Herzog H, and Freund H-J. Role of the premotor cortex in recovery from middle cerebral artery infarction. Arch Neurol 55: 1081–1088, 1998. Takahashi N, Kawamura M, and Araki S. Isolated hand palsy due to cortical infarction: localization of the motor hand area. Neurology 58: 1412–1414, 2002. Tanji J, Okano K, and Sato KC. Neuronal activity in cortical motor areas related to ipsilateral, contralateral, and bilateral digit movements of the monkey. J Neurophysiol 60: 325–343, 1988. Tereo Y, Hayashi H, Kanda T, and Tanabe H. Discrete cortical infarction with prominent impairment of thumb flexion. Stroke 24: 2118 –2120, 1993. Von Schroeder HP and Botte MJ. The functional significance of the long extensors and juncturae tendinum in finger extension. J Hand Surg [Am] 18: 641– 647, 1993. Von Schroeder HP, Botte MJ, and Gellman H. Anatomy of the juncturae tendinum of the hand. J Hand Surg [Am] 15: 595– 602, 1990. Wade DT, Langton-Hewer R, Wood VA, Skilbeck CE, and Ismail HM. The hemiplegic arm after stroke: measurement and recovery. J Neurol Neurosurg Psychiatry 46: 521–524, 1983. Weiller C, Chollet F, Friston KJ, Wise RJS, and Frackowiak RSJ. Functional reorganization of the brain in recovery from striatocapsular infarction in man. Ann Neurol 31: 463– 472, 1992. Weiller C, Ramsay SC, Wise RJS, Friston KJ, and Frackowiak RSJ. Individual patterns of functional reorganization in the human cerebral cortex after capsular infarction. Ann Neurol 33: 181–189, 1993. Woolsey CN, Gorska T, Wetzel A, Erickson TC, Earls FJ, and Allman JM. Complete unilateral section of the pyramidal tract at the medullary level in the Macaca mulatta. Brain Res 40: 119 –123, 1972. Woolsey CN, Settlage PH, Meyer DR, Sencer W, Hamuy TP, and Travis AM. Patterns of localization in precentral and “supplementary” motor areas and their relation to the concept of a premotor area. Res Publ Assoc Res Nerv Ment Dis 30: 238 –264, 1952. Yousry TA, Schmid UD, Alkadhi H, Schmidt D, Peraud D, Buettner A, and Winkler P. Localization of the motor hand area to a knob on the precentral gyrus: a new landmark. Brain 120: 141–157, 1997. 90 • AUGUST 2003 • www.jn.org Downloaded from http://jn.physiology.org/ by 10.220.33.4 on August 12, 2017 Kilbreath SL and Gandevia SC. Limited independent flexion of the thumb and fingers in human subjects. J Physiol 479: 487– 497, 1994. Kilbreath SL, Gorman RB, Raymond J, and Gandevia SC. Distribution of the forces produced by motor unit activity in the human flexor digitorum profundus. J Physiol 543: 289 –296, 2002. Kim JS, Chung JP, and Ha SW. Isolated weakness of index finger due to small cortical infarction. Neurology 58: 985–986, 2002. Kubota K. Motor cortical muscimol injection disrupts forelimb movement in freely moving monkeys. Neuroreport 7: 2379 –2384, 1996. Kuypers HGJM. A new look at the organization of the motor system. Prog Brain Res 57: 381– 403, 1982. Kuypers HGJM. Some aspects of the organization of the output of the motor cortex. In: Motor Areas of the Cerebral Cortex, edited by Bock G, O’Conner M, and Marsh J. Sussex, UK: John Wiley, 1987. Kuypers HGJM and Brinkman J. Precentral projections to different parts of the spinal intermediate zone in the rhesus monkey. Brain Res 24: 29 – 48, 1970. Lawrence DG and Kuypers HGJM. The functional organization of the motor system in the monkey. I. The effects of bilateral pyramidal lesions. Brain 19: 1–14, 1968a. Lawrence DG and Kuypers HGJM. The functional organization of the motor system in the monkey. II. The effects of lesions of the descending brain-stem pathways. Brain 15–36, 1968b. Lee PH, Han SW, and Heo JH. Isolated weakness of the fingers in cortical infarction. Neurology 50: 823– 824, 1998. Lincoln N and Leadbitter D. Assessment of motor function in stroke patients. Physiotherapy 65: 48 –51, 1979. Maier MA, Armand J, Kirkwood PA, Yang H-W, Davis JN, and Lemon RN. Differences in the corticospinal projection from primary motor cortex and supplementary motor area to Macaque upper limb motoneurons: an anatomical and electrophysiological study. Cereb Cortex 12: 281–296, 2002. Morecraft RJ, Herrick JL, Stilwell-Morecraft KS, Louie JL, Schroeder CM, Ottenbacher JG, and Schoolfield MW. Localization of arm representation in the corona radiata and internal capsule in the non-human primate. Brain 125: 176 –198, 2002. Nathan PW and Smith MC. Effects of two unilateral cordotomies on the motility of the lower limbs. Brain 96: 471– 494, 1973. Nathan PW and Smith MC. The rubrospinal and central tegmental tracts in man. Brain 105: 223–269, 1982. Nathan PW, Smith M, and Deacon P. Vestibulospinal, reticulospinal and descending propriospinal nerve fibres in man. Brain 119: 1809 –1833, 1996. Nudo RJ and Milliken GW. Reorganization of movement representations in primary motor cortex following focal ischemic infarcts in adult squirrel monkeys. J Neurophysiol 75: 2144 –2149, 1996. Nudo RJ, Milliken GW, Jenkins WM, and Merzenich MM. Use-dependent alterations of movement representations in primary motor cortex of adult squirrel monkeys. J Neurosci 16: 785– 807, 1996a. Nudo RJ, Wise BM, SiFuentes F, and Milliken GW. Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science 272: 1791–1794, 1996b. Passingham R. Functional organization of the motor system. In: Human Brain Function, edited by Frackowiak RSJ, Friston KJ, Frith CD, and Dolan RJ. San Diego: Academic Press, 1997. Penfield W and Boldrey E. Somatic motor and sensory representation in the cerebral cortex of man as studied by electrical stimulation. Brain 37: 389 – 443, 1937. Penfield W and Rasmussen T. The Cerebral Cortex of Man. New York: MacMillan, 1950. Phan TG, Evans BA, and Huston J. Pseudoulnar palsy from a small infarct of the precentral knob. Neurology 54: 2185, 2000. Picard N and Strick PL. Imaging the premotor areas. Curr Opin Neurobiol 11: 663– 672, 2001. Porter R and Lemon R. Corticospinal Function and Voluntary Movement. New York: Oxford Univ. Press, 1993. Reilly KT and Hammond GR. Independence of force production by digits of the human hand. Neurosci Lett 290: 53– 65, 2000.