* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
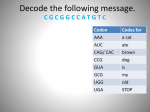
Download The location and type of mutation predict
Pharmacogenomics wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Genetic code wikipedia , lookup
Protein moonlighting wikipedia , lookup
Koinophilia wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
No-SCAR (Scarless Cas9 Assisted Recombineering) Genome Editing wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
Microevolution wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Epigenetics of neurodegenerative diseases wikipedia , lookup
Oncogenomics wikipedia , lookup
© 2000 Oxford University Press Human Molecular Genetics, 2000, Vol. 9, No. 20 3019–3028 The location and type of mutation predict malformation severity in isolated lissencephaly caused by abnormalities within the LIS1 gene Carlos Cardoso1,+, Richard J. Leventer1,2,+, Naomichi Matsumoto4, Julie A. Kuc1, Melissa B. Ramocki1, Stephanie K. Mewborn1, Laura L. Dudlicek1, Lorraine F. May1, Patti L. Mills1, Soma Das1, Daniela T. Pilz5, William B. Dobyns1,2,3 and David H. Ledbetter1,3,§ Departments of 1Human Genetics, 2Neurology and 3Pediatrics, University of Chicago, 920 East 58th Street, Chicago, IL 60637, USA, 4Department of Human Genetics, Nagasaki University School of Medicine, Sakamoto 1-12-4, Nagasaki 852-8523, Japan and 5Institute for Medical Genetics, University Hospital of Wales, Heath Park, Cardiff CF14 4WX, UK Received 9 August 2000; Revised and Accepted 18 October 2000 Lissencephaly is a cortical malformation secondary to impaired neuronal migration resulting in mental retardation, epilepsy and motor impairment. It shows a severity spectrum from agyria with a severely thickened cortex to posterior band heterotopia only. The LIS1 gene on 17p13.3 encodes a 45 kDa protein named PAFAH1B1 containing seven WD40 repeats. This protein is required for optimal neuronal migration by two proposed mechanisms: as a microtubuleassociated protein and as one subunit of the enzyme platelet-activating factor acetylhydrolase. Approximately 65% of patients with isolated lissencephaly sequence (ILS) show intragenic mutations or deletions of the LIS1 gene. We analyzed 29 non-deletion ILS patients carrying a mutation of LIS1 and we report 15 novel mutations. Patients with missense mutations had a milder lissencephaly grade compared with those with mutations leading to a shortened or truncated protein (P = 0.022). Early truncation/deletion mutations in the putative microtubule-binding domain resulted in a more severe lissencephaly than later truncation/deletion mutations (P < 0.001). Our results suggest that the lissencephaly severity in ILS caused by LIS1 mutations may be predicted by the type and location of the mutation. Using a spectrum of ILS patients, we confirm the importance of specific WD40 repeats and a putative microtubule-binding domain for PAFAH1B1 function. We suggest that the small number of missense mutations identified may be due to underdiagnosis of milder phenotypes and hypothesize that the greater lissencephaly severity seen in Miller–Dieker syndrome may be secondary to the +These §To loss of another cortical development gene in the deletion of 17p13.3. INTRODUCTION Lissencephaly (LIS) is a diffuse cortical malformation resulting from incomplete neuronal migration during early brain development. It encompasses a continuous spectrum of malformations from complete agyria to variable degrees of agyria and pachygyria to subcortical band heterotopia (SBH) only (1). Clinical manifestations range from profound mental retardation, intractable epilepsy, spasticity and reduced longevity (2) to milder forms with infrequent seizures and intellectual disability only (3). Lissencephaly is one component of the contiguous gene deletion disorder known as Miller– Dieker syndrome (MDS) or may occur as an isolated brain malformation in patients with isolated lissencephaly sequence (ILS) (2). The clinical severity generally correlates with the degree of agyria and cortical thickening (4). Approximately 80% of typical LIS spectrum patients show abnormalities of either the LIS1 gene or the DCX gene (alternatively known as XLIS) (5). The majority of patients with LIS show deletions or mutations of the LIS1 gene whereas the majority of patients with typical SBH show mutations of the DCX gene (5). Patients with MDS and ILS have been shown to carry heterozygous mutations or deletions of LIS1 suggesting haplo-insufficiency of the LIS1 gene product as the pathogenic mechanism (6). The functions of the LIS1 protein in normal brain development are currently being elucidated, yet our understanding of the functional domains within this protein and the biological basis for the phenotypic spectrum of LIS remains incomplete. LIS1, located on chromosome 17p13.3, encodes a protein of 410 amino acids named PAFAH1B1, which contains seven WD40 repeats and has a molecular weight of ∼45 kDa (7). PAFAH1B1 is highly conserved showing only a single amino acid difference between mouse and human (8), three amino acid differences between human and bovine (9), 70% identity with authors contributed equally to this work whom correspondence should be addressed. Tel: +1 773 834 0525; Fax: +1 773 834 0505; Email: [email protected] 3020 Human Molecular Genetics, 2000, Vol. 9, No. 20 Drosophila LIS1 (10) and 29% homology with the yeast homolog, PAC1 (11). In addition, it shares 42% homology with the nuclear migration protein NudF in Aspergillus nidulans (12). PAFAH1B1 forms the non-catalytic subunit of the G protein-like heterotrimeric cytosolic platelet-activating factor acetylhydrolase (PAF-AH) brain isoform Ib (PAFAH1B1) (13). Together with the 29 kDa subunit (PAFAH1B3) and the 30 kDa subunit (PAFAH1B2), PAFAH1B1 forms a trimeric complex. This protein complex regulates the level of platelet-activating factor (PAF) in the brain through the removal of the acetyl group of PAF at the sn-2 position to produce biologically inactive lyso-PAF (14). Optimal concentrations of PAF may be necessary for correct neuronal migration. The precise role of PAF in neuronal migration is uncertain, although it has been proposed that PAF affects migrating neurons by influencing cell morphology or adhesion properties (15). Studies demonstrate that addition of PAF or inhibition of PAF-AH decreases migration of cerebellar granule cells in vitro (16,17) and addition of PAF to cultured hippocampal neurites produces growth cone collapse, neurite retraction and neurite varicosity formation (18). The three subunits of PAF-AH are co-expressed in the developing brain in regions containing migrating neurons. The highest expression level for each of the three subunits is concomitant with peak times of neuronal migration (15,19). The targeted knockout of the LIS1 gene created a mouse model for LIS. Homozygous null mice die early in embryogenesis whereas heterozygous mice survive, showing evidence of delayed neuronal migration (cortical, hippocampal, cerebellar and olfactory bulb disorganization) confirmed by in vitro and in vivo cell migration assays (20). Recent evidence suggests that an important domain for PAFAH1B1 function may be localized to the second WD40 repeat at the region where interactions with the other two PAFAH subunits occur (21,22). Apart from its role as a subunit of PAF-AH, PAFAH1B1 may enhance neuronal migration by acting as a microtubule-associated protein (MAP). Evidence for this role comes from studies that demonstrate the co-localization and interaction of PAFAH1B1 with tubulin, the major component of microtubules. This interaction results in the developmentally regulated phosphorylation of PAFAH1B1 (23). The co-assembly of PAFAH1B1 with microtubules results in a reduction of microtubule catastrophic events, and thus an increase in the length of microtubules (24). This would be predicted to enhance and maintain microtubule elongation, a process necessary for optimal nuclear (and thus neuronal) migration. In vitro studies show that the microtubule-associated protein-binding domain (MAP-D) of the PAFAH1B1 protein is near the N-terminus (23), but the precise boundaries and characteristics of this domain are not well defined. As part of our ongoing lissencephaly research project, we have collected a large number of patients with lissencephaly secondary to abnormalities of the LIS1 gene. The goal of this study was to investigate patients with ILS and a mutation within LIS1 to determine the pathophysiological basis of the spectrum of brain malformations seen in patients with LIS1 mutations. To do this, we performed an analysis of the correlation between mutation type and phenotype (lissencephaly severity grade) assessed by magnetic resonance imaging (MRI) or computed tomography (CT). We performed detailed mutation analysis using direct gene sequencing, Southern blot and RT–PCR analysis and identified 15 novel mutations, not previously reported, the majority of which result in protein truncation or shortening due to intragenic deletion, frameshift or exon skipping (herein referred to as ‘truncation/deletion mutations’). By comparing mutation type and location to the lissencephaly severity grade, we show that missense mutations are usually less severe than truncation/deletion mutations and that more 5′ truncation/deletion mutations produce a more severe phenotype than similar mutations located towards the 3′ region of LIS1. Our results, based on the study of a large number of patients with a spectrum of LIS phenotypes, demonstrate that the mutation type and location predict malformation severity and that this correlation is consistent with the current understanding of the functional domains of the LIS1 gene. RESULTS Range and distribution of LIS1 mutations in ILS Among 65 patients with ILS and no LIS1 deletion by fluorescence in situ hybridization (FISH), we found 29 unrelated patients (18 boys and 11 girls) carrying a heterozygous LIS1 mutation, 15 of which have not been reported previously. Mutation analysis was performed by direct sequencing and confirmed in both the forward and reverse directions. In five of these patients (LP85-002, LP88-009, LP90-012, LP97-064 and LP91-022), we detected a LIS1 rearrangement by Southern blot analysis and used a restriction map from the genomic sequence of the LIS1 gene (see Materials and Methods) to determine the extent of the coding region deletions (Fig. 1 and Table 1). For patients LP85-002 and LP91-022, subsequent RT–PCR analysis followed by direct sequencing of the cDNA confirmed the deletion of exon 2 for LP85-002 and the deletion of exons 3–6 for LP91-022 that was previously detected by Southern analysis (Fig. 1). Lymphoblastoid cell lines were not available on patients LP88-009, LP90-012 and LP97-064; therefore, further studies to delineate the deletion boundaries could not be performed. For the remaining 24 patients, direct sequencing detected five missense mutations, six splicing defects confirmed by RT–PCR analysis, five nonsense mutations and eight frameshift mutations (Fig. 2, Tables 1 and 2). Only two mutations were recurrent, including a splice donor site change (T→C) in intron 6, and a C→T substitution at position 817 in exon 8 resulting in a protein truncation (R273X). Each of these two mutations was found in two unrelated patients. Missense mutations were found in exons 3, 6 and 9, with three (H149R, G162S and S169P) clustered in exon 6 which corresponds to the coding region for the second WD40 repeat (Fig. 2 and Table 2). Four of the five missense mutations were demonstrated to be de novo (Table 2). For patient LP98-063 (amino acid change D317H), parental samples were unavailable for further analysis but the mutation was not found in 100 normal chromosomes sequenced (Table 2). Large intragenic deletions were clustered between exons 2 and 6. Other mutation types (nonsense mutations, small insertions and deletions and splicing mutations) were found scattered throughout the gene except in the third WD40 repeat encoded by exon 7. Sequencing was performed on the available parents and showed that the mutations were de novo. Human Molecular Genetics, 2000, Vol. 9, No. 20 3021 Figure 1. Example of LIS1 mutation detection demonstrated using patient LP91-022 with an intragenic deletion of LIS1 detected by the sequential use of Southern analysis, RT–PCR and direct cDNA sequencing. (a) Southern blot analysis using EcoR1, showing a band at ∼20 kb (double asterisk) which is absent in the control. The stronger band at ∼7.5 kb (single asterisk) corresponds to the LIS1 pseudogene localized to chromosome 2 (37) and the other bands correspond to the LIS1 cDNA (see Materials and Methods). (b) RT–PCR, showing the presence of an abnormal transcript of LIS1 of 250 bp (arrow). (c) Direct sequencing chromatogram of the abnormal transcript in b shows the absence of exons 3–6 as indicated in the overlying schematic representation of LIS1. Table 1. LIS1 protein truncation mutations and lissencephaly severity grade found in ILS patients Patients Sex Exon Mutation Type of mutation LIS grade LP85-002 Female 2 ∆exon 2 Deletion 2 This report LP88-009 Female 2+3 Rearrangement Southern blot Deletion 2 This report LP90-012 Female 3+4+5 Rearrangement Southern blot Deletion 2 5 LP97-064 Female 3+4+5 Rearrangement Southern blot Deletion 2 5 LP91-022 Male 2–7 ∆exons 3, 4, 5 and 6 Deletion 3 This report LP97-068 Female 4 162insA Frameshift 2 5 LP99-053 Male 4 166delA Frameshift 4 This report LP99-058 Male 5 R89X Nonsense 3 This report LP97-078 Male 6 R144X Nonsense 3 5 LP99-014 Male 6+7 569–10 bp T→C Splicing defect 3 This report LP99-088 Female 6+7 569–10 bp T→C Splicing defect 3 This report LP97-071 Female 8 703delGA Frameshift 3 5 LP91-019 Female 8 805delA Frameshift 3 5 LP89-005 Male 8 R273X Nonsense 3 6 DP-0201 Male 8 R273X Nonsense 4 This report LP97-086 Female 8 S289X Nonsense 3 This report LP99-039 Male 8 881delCT Frameshift 3 This report LP97-021 Male 9 903insT Frameshift 3 5 LP93-005 Male 9 988del 22bp Splicing defect 4 6 LP91-012 Male 9 + 10 1002+1 bp G→A Splicing defect 3 This report LP97-069a Female 9 + 10 1002+5 bp G→A Splicing defect 3 5 LP90-014 Male 10 1018insT Frameshift 4 5 LP98-100 Male 10 1049insG Frameshift 3 This report LP90-020 Male 10 + 11 1159+3 bp ins CA Splicing defect 3 5 aIn Pilz et al. (5), LP97-069 was incorrectly numbered as LP97-067. Reference 3022 Human Molecular Genetics, 2000, Vol. 9, No. 20 Figure 2. Summary of LIS1 mutations in 29 ILS patients. Missense mutations are denoted by green circles above the gene and nonsense and frameshift mutations by blue arrows, splicing defects by orange boxes and deletions by solid black lines (indicating the deleted region) below the gene. An asterisk denotes recurrent mutations. Red shading of the gene indicates the putative microtubule associated protein-binding domain and gray shading indicates the seven WD40 repeats. Table 2. LIS1 missense mutations and lissencephaly severity grade found in ILS patients Patients Sex Exon Mutation Nucleotide change Domain De novo LIS grade Reference LP97-077 Female 3 F31S 92T→C MAP-D Yes 4 This report LP93-012 Male 6 H149R 446A→G WD2 Yes 3 5 LP99-127 Male 6 G162S 486C→T WD2 Yes 4 This report LP94-051 Male 6 S169P 499T→C WD2 Yes 6 36 LP98-063 Male 9 D317H 949G→C WD5 – 4 This report Two silent polymorphic variants, an A→T change at nucleotide position 687 in exon 8 (T229) and a C→T change at nucleotide position 1188 in exon 11 (V396) were found in two unrelated boys and their mothers. We also identified two polymorphisms in the 3′ untranslated region (UTR) of the LIS1 transcript, a C→T substitution at nucleotide position 1250 (24) and a T→G substitution at nucleotide position 1236 which we have observed in normal individuals (unpublished data). Characterization of the putative MAP-D In vitro and in vivo analyses show that PAFAH1B1 interacts with tubulin at the N-terminal region (23,25). By in silico analysis (see Materials and Methods) we attempted to determine whether this region contains a domain with homology to other motifs allowing protein–protein interaction. We found a coiled-coil domain in the N-terminal region (Fig. 3a and b) conserved in all LIS1 proteins and also present in the LIS1 homolog NudF (Fig. 3c). We also identified the presence of a moderate number of basic amino acids (such as lysine, arginine and histidine), one specific KKEX motif and three related KKXX repeats characteristic of the MAP 1B (26) (Fig. 3c). Genotype–phenotype correlation MRI scans were available for review on 26 patients and CT scans were available for the remaining 3 patients. The lissencephaly severity ranged from grade 2 to grade 6, excepting grade 5 (see Materials and Methods; Fig. 4). Of these, 17% had diffuse agyria with shallow sulci over the frontal and temporal poles (grade 2), 55% had posterior agyria and frontal pachygyria (grade 3), 24% had diffuse pachygyria that was more severe posteriorly (grade 4) and 4% had posterior subcortical band heterotopia (grade 6). Patients with missense mutations were grades 3, 4 and 6, and those with other mutations ranged from grade 2 to grade 4 (Tables 1 and 2). As shown in Table 3, patients with missense mutations had a significantly milder mean lissencephaly severity grade compared with those with truncation/deletion mutations (P = 0.022). Patients with truncation/deletion mutations were Human Molecular Genetics, 2000, Vol. 9, No. 20 3023 Figure 3. Delineation of the putative microtubule-associated protein domain of PAFAH1B1. (a) Graphical representation of the output from the coils program (see Materials and Methods) demonstrating that PAFAH1B1 (GenBank accession no. P43034) has a 1.0 probability of forming a coiled-coil structure in the N-terminal region. (b) The region of PAFAH1B1 corresponding to amino acids 44–78 are listed corresponding to their position within each heptad repeat of the coiled-coil structure. The boxed regions contain the hydrophobic amino acids which are predicted to lie in positions a and d of the heptad repeat forming the coiled-coil motif (4-3 hydrophobic repeat). (c) Conservation of the coiled-coil domain in PAFAH1B1 in the species bovine (GenBank accession no. P43033), chicken (AAF18938), mouse (P43035), Drosophila (AAD38390), Caenorhabditis elegans (AAF82632) and two homologous proteins in Aspergillus nidulans (NudF; AAA91301) and yeast (PAC1; S67166). For LIS1 from rat and zebrafish, the protein sequences were predicted using the translation of the expressed sequence tag available in GenBank. The N-terminal region of PAFAH1B1 shows homology to MAP-1B, which is lysine- and arginine-rich and the occurrence of one specific KKEX and three related KKXX repeats (denoted by boxed regions). Figure 4. Axial T2-weighted MRI of four patients representing the four lissencephaly grades found in patients in this study. The lissencephaly grade is noted in the upper left-hand corner of each image. Lissencephaly severity decreases with increasing grade (left to right). Grade 2 shows predominant agyria (lack of gyri) with minimal pachygyria (broadened gyri), grade 3 shows mixed agyria/pachygyria, grade 4 shows pachygyria only and grade 6 shows subcortical band heterotopia (arrows). 3024 Human Molecular Genetics, 2000, Vol. 9, No. 20 Table 3. Mean lissencephaly severity grade by LIS1 gene mutation type Lissencephaly grade Missense mutations (n = 5) Truncating mutations P value (n = 24) 4.20 2.96 0.022 Table 4. Mean lissencephaly severity grade by location of truncating LIS1 gene mutation Lissencephaly grade Early truncating (n = 6) Late truncating (n = 18) P value 2.43 3.18 <0.001 divided into two groups based on an estimate of the boundary of the putative MAP-D spanning exon 2 to the beginning of exon 5 (at the end of the coiled-coil domain) (24). Mutations in this region predicted to compromise the MAP-D were named ‘early truncation/deletion’ mutations, whereas the remaining were named ‘late truncation/deletion’ mutations. As shown in Table 4, patients with early truncation/deletion mutations had a significantly more severe mean lissencephaly grade compared with those with late truncation/deletion mutations (P < 0.001). The functional consequences of the LIS1 mutation in patient LP99-053 are uncertain as he has a relatively mild LIS grade despite a mutation at the end of the putative MAP-D. Mutant PAFAH1B1 protein was not detected in patients with truncation or deletion mutations In an attempt to detect the presence of mutant PAFAH1B1 protein in patients with mutations leading to a truncated or deleted protein that could correlate with the different lissencephaly grades, we performed western blot analysis on a subset of 11 patients. For our experiments, we used a commercial polyclonal antibody directed against the N-terminal region of PAFAH1B1 on total cellular protein extracts from lympho- blastoid cell lines of three normal individuals as negative controls, three patients carrying missense mutations as positive controls (LP97-077, LP93-012, LP94-051) and eight patients with truncation or deletion mutations (LP90-012, LP97-068, LP97-078, LP91-019, LP89-005, LP97-021, LP93-005 and LP97-069). A band of ∼45 kDa, attributable to PAFAH1B1, was detected in the normal control and in all patients. However, we were unable to detect the presence of truncated or abnormal proteins (<45 kDa) in any of these patients (Fig. 5). We also performed simultaneous and sequential hybridization of PAFAH1B1 with a monoclonal antibody directed against actin (as an internal normalization control of protein expression) to determine whether the expression level of PAFAH1B1 was reduced in these patients. Although patients with truncation/deletion mutations appear to have a reduction of PAFAH1B1 by this method, the differences in the levels between patient groups could not be consistently discriminated within the sensitivity of densitometry, indicating that the polyclonal PAFAH1B1 antibody might not be suitable for accurate quantitative analysis. DISCUSSION Lissencephaly is one disorder in a large group of malformations of cortical development with increased recognition since the widespread use of MRI scanning. Although individually rare, collectively these malformations are responsible for a significant proportion of epilepsy and chronic neurological disability, especially in childhood. Through molecular genetic analysis of these patients, it is possible to identify genes that are essential to normal cortical development. Once these genes are identified, the task is to determine the precise function of the protein products in complex cortical development pathways, especially during the stage of neuronal migration. Elucidation of the aberrant developmental mechanisms that generate these malformations requires the study of affected patients and mutant models to complement the studies of normal protein function. Optimal functioning of the PAFAH1B1 protein appears to be a critical requirement for normal development of the human Figure 5. Immunoblot analysis of ILS patients carrying missense mutations and mutations predicted to produce truncated or shortened proteins. All ILS patients with mutations leading to a shortened or truncated protein (LP90-012, LP97-068, LP97-078, LP91-019, LP89-005, LP97-021, LP93-005 and LP97-069) showed expression of an ∼45 kDa PAFAH1B1 protein similar to controls (normal individuals) or the patients with missense mutations (LP97-077, LP93-012 and LP94051) and did not show the presence of abnormal or shortened PAFAH1B1 mutant protein. Human Molecular Genetics, 2000, Vol. 9, No. 20 3025 cortex. The fact that PAFAH1B1 is so highly conserved across species confirms its evolutionary importance. It was not until very recently that the spectrum of malformation severity in lissencephaly was appreciated. There are few human data available to explain the functional basis of this range of malformation severity. Such data will have important implications both to elucidate the functional regions of PAFAH1B1 and to improve diagnosis and genetic counseling. This is the largest study to date of ILS patients with abnormalities within the LIS1 gene that attempts to explain the spectrum of severity seen in ILS based on the nature of the mutation and its functional consequences. Functional domains of PAFAH1B1 Recent studies suggest the existence of two important functional domains within PAFAH1B1. We divided our patients into three groups (missense mutations, early truncation/ deletion and late truncation/deletion mutations) according to the predicted functional consequences of their mutations based on these domains. The first of these is a poorly defined MAP-D at the N-terminal region (24). Based on in vitro studies, this region of PAFAH1B1 may interact with tubulin, leading to microtubule assembly and elongation, a process critical to neuronal migration (24). Using in silico analysis we confirmed the presence of a coiled-coil domain spanning most of the Nterminal region that may act as a domain for protein–protein interaction (27). This domain is also present in PAFAH1B1 of other species and in two homologous proteins, NudF and PAC1 (11,28). Such domains allow proteins such as PAFAH1B1 to interact with themselves to form homodimers, or with other proteins (such as tubulin) to form heterodimers (29). This finding is consistent with experiments performed by Sapir et al. (24) that suggest the presence of a domain of interaction between PAFAH1B1 and tubulin at the N-terminal region of PAFAH1B1. Further studies, such as a yeast twohybrid analysis using constructs expressing different portions of the N-terminal region and site-directed mutagenesis analysis, will be required to better define the amino acids within this domain that are essential for the interaction with tubulin or other proteins. The second proposed functional domain of PAFAH1B1 is the region containing seven WD40 repeats, with greatest functional significance involving the second WD40 repeat encoded by exon 6. This particular part of the domain appears to be critical for the correct interaction of PAFAH1B1 with the other two subunits of PAF-AH (21,22). As hypothesized, the three groups of patients that we defined according to the predicted consequences of their mutations within these functional domains have a statistically different phenotype as measured by lissencephaly severity grade. Patients with missense mutations We report five missense mutations among the 29 patients of which three are not previously reported. The low number of missense mutations strongly suggests that patients with such mutations may be underdiagnosed. An alternative explanation is that most missense mutations are lethal, although our finding of milder phenotypes among patients with missense mutations argues against this. With the exception of patient LP93-012, who has a point mutation which alters the critical histidine amino acid in the second WD40 repeat, all missense mutations result in a relatively mild phenotype (grades 4 and 6), including one patient with posterior band heterotopia and another with occipital pachygyria only. Three of the five missense mutations affect the second WD40 repeat, a domain necessary for the interaction of PAFAH1B1 with the other two subunits of PAF-AH (22). These mutations are predicted to result in either a partial alteration or a complete loss of PAFAH activity. Although the patient numbers are small, we found a significant difference in malformation severity between patients with missense and truncation/deletion mutations (P = 0.022) suggesting that missense mutations generally produce a less severe phenotype. Analysis of a greater number of patients with missense mutations is required. Ascertainment of such patients will require an increased referral of patients with milder phenotypes (such as partial band heterotopia and localized pachygyria) for LIS1 sequencing. Patients with mutations leading to a truncated or shortened protein Our observation that the majority of LIS1 mutations result in protein truncation confirms the published results of previous studies (5,6,30). For patients with truncation/deletion mutations, our data show that mutations resulting in the most severe phenotype (grade 2) cluster in the N-terminal region of the LIS1 gene from exon 2 to 5. All such patients have deletions or mutations that compromise the putative MAP-D or the MAP-D and the PAF-AH subunit interaction domain, producing a more severe defect of neuronal migration and thus a more severe LIS grade. Although the numbers are small, this trend is supported by results showing that patients with 5′ truncation/deletion mutations have a more severe LIS grade than do patients with later truncation/deletion mutations (P < 0.001), which would be predicted to spare the MAP-D. Evidence from patients with ILS secondary to large deletions of 17p13.3 supports the hypothesis that the N-terminal region of LIS1 contains a domain of functional significance. A review of our FISH data shows that the majority of patients with a telomeric deletion including the 5′ end of LIS1 (defined by a deletion of the D17S379 probe and/or the c37E9 cosmid) have grade 2 LIS and the majority of patients with a deletion of the 3′ end of LIS1 only (defined by a deletion of the c120A7 cosmid) have grade 3 or 4 LIS (31) (unpublished data). Unfortunately, the boundaries of the large deletions observed in these patients are not precisely defined. The most severe form of lissencephaly (grade 1) has been found only in patients with MDS, which is a contiguous gene deletion syndrome of 17p13.3 including a deletion of LIS1. This may suggest the presence of a second gene required for neuronal migration located within the MDS deletion in addition to the deletion of LIS1. Deletion of these two genes would explain the severe LIS seen in MDS. Identification of this second gene will require an improvement of the physical and transcriptional map of 17p13.3 followed by testing of candidate genes in suitable patients. Graded function of PAFAH1B1 in patients with intragenic mutations or internal deletions of the LIS1 gene The data from our patient group support the conclusions of previous studies suggesting haploinsufficiency of LIS1 as the cause of LIS in most patients (2). In addition, our data suggest 3026 Human Molecular Genetics, 2000, Vol. 9, No. 20 that the location and type of mutation of the LIS1 gene may account for the phenotypic variability now evident in patients with LIS. This further implies that patients with missense mutations and mutations predicted to lead to a truncated or shortened protein should result in the production of a partially functional protein. According to our genotype–phenotype correlation data, we expect the mutant PAFAH1B1 proteins caused by missense mutations to be more stable and functional than those caused by truncation/deletion mutations and 3′ mutations should result in a more stable or functionally active protein than 5′ mutations. We did not observe an altered protein by western blot analysis of 11 patients. Fogli et al. (30), have previously performed a similar analysis using cells from four LIS patients, all of whom had a mutation predicted to lead to protein truncation or shortening. They reported reduced PAFAH1B1 protein levels with truncation mutations but no abnormal protein product in three of four patients. For these 14 patients, it is possible that mutant proteins were not detected due to instability and rapid protein degradation (32). Alternatively, it is possible that such proteins are expressed and functionally active only during development in the time window of neuronal migration. We are aware of other studies that fail to show partial PAFAH1B1 recombinant protein products, even when the truncation or deletion is small (A. Wynshaw-Boris, personal communication). Further studies of PAFAH1B1 expression are required to detect differences in PAFAH1B1 levels between patients with different mutation types. Such studies should include western blots using a specific monoclonal antibody directed against PAFAH1B1 and immunocytofluorescence techniques designed to detect the localization and distribution of PAFAH1B1. One patient, LP99-053, has a relatively mild LIS grade (grade 4) despite a truncation mutation located within the latter part of the putative MAP-D. Further study of this patient may help in defining the precise 3′ boundary of the region of the PAFAH1B1 domain that is essential for the interaction with tubulin or other proteins required for cell migration. For our analysis, we included this sample as an early truncation/ deletion mutation, but further elucidation of the boundaries of this domain may classify this sample as a late truncation/ deletion mutation. An additional important observation from our data is the absence of any mutations in exon 7 (coding for the third WD40 repeat). This raises the question of whether this domain has great functional importance (with mutations resulting in lethality through a dominant negative effect) or little functional importance. The answer to this question will come only with further functional studies of PAFAH1B1 or with the identification of patients with mutations within exon 7. Using data derived from a large number of ILS patients, our results suggest that the phenotypic spectrum observed in these patients may be a result of the functional consequences of the specific location and type of mutation. Our results support the hypothesis that PAFAH1B1 may contain two important functional domains. However, an understanding of the relative importance of these domains in the complex process of cortical development remains incomplete. Further studies are required to determine the precise role of PAF (and consequently PAF-AH) in neuronal migration. Evidence from the study of other human cortical malformations such as band and nodular heterotopia demonstrates the importance of cytoskeletal proteins such as doublecortin (33) and filamin 1 (34) in neuronal migration. Consideration of PAFAH1B1 as a MAP is strengthened by the presence of an appropriate functional domain at the N-terminal region and our finding that patients with the most severe LIS grade had mutations that compromise this domain. Whether PAFAH1B1 interacts directly with tubulin or indirectly through other proteins remains unknown at present. Appropriate functional experiments combined with the study of patients with cortical malformations, may help in answering this question as well as in identifying other genes involved in cortical development pathways. MATERIALS AND METHODS Patients Patients were ascertained through the ongoing Lissencephaly Research Project from a variety of sources including clinical referrals from physicians, contact through the Lissencephaly Network and direct inquiry from parents of affected children. Patients were included in the study if they had ILS and a mutation of the LIS1 gene. ILS patients with deletions detected by FISH were excluded from the study, as determination of the precise boundaries of their deletions could not always be assessed with certainty. MRI (n = 26) and CT (n = 3) scans were reviewed and each patient’s malformation was classified using an established classification scheme for LIS which involves both the severity (grades 1–6) and the gradient (1). According to this scale, LIS grade ranges from generalized agyria (grade 1), to variable degrees of agyria and pachygyria (grades 2 and 3), to generalized pachygyria (grade 4), to mixed pachygyria and SBH (grade 5) to SBH alone (grade 6). The LIS gradient may be either posterior→anterior (‘a’ gradient) as observed with LIS1 mutations, or anterior→posterior (‘b’ gradient) as observed with DCX mutations. The precise mutation data were not available to the investigators at the time of neuroimaging review. Blood samples from probands were obtained with informed consent and all protocols were approved by the appropriate Institutional Review Board Human Subjects Committee. DNA extraction, PCR amplification and direct DNA sequencing DNA was extracted from lymphoblast cell lines or peripheral blood using a Puregene DNA isolation kit (Gentra System, Minneapolis, MN) according to the manufacturer’s protocol. Ten LIS1 exons covering the coding region (exons 2–11) were amplified by PCR. PCR was cycled 35 times at 94°C for 30 s, 58°C for 30 s, 72°C for 1 min in a volume of 50 µl, containing 1× PCR buffer with 1.5 mM MgCl2, 0.2 mM each dNTP, 1 µM each primer and 2.5 U of TaqGold polymerase (PE Applied Biosystems, Foster, CA). Primer sequences have been described previously (5). PCR products were purified using the QIAquick PCR purification kit (Qiagen, Chatsworth, CA) and sequenced on both strands with BigDye Terminator chemistry by a standard protocol (PE Applied Biosystems) as described previously (5). The resulting sequences from the patients and normal controls were aligned and compared with the published sequences deposited in GenBank (accession nos U72333– U72342). Human Molecular Genetics, 2000, Vol. 9, No. 20 3027 RT–PCR Protein extraction and western blot analysis RNA isolated from the cell lines of patients with a LIS1 splice site mutation or an intragenic LIS1 deletion and normal control RNA was reverse transcribed using the Advantage RT for PCR kit (Clontech, Palo Alto, CA). Transcription was undertaken with both the random hexamer and oligo(dT)18 primers. cDNA (5 µl) was used for the PCR reaction. cDNA primers were designed to cover the entire LIS1 coding region. PCR conditions were as follows: 50 µl reaction containing 1× PCR buffer, 2.5 mM MgCl2, 0.2 mM of each dNTP, 0.1 µM of each primer and 1 U of TaqGold polymerase (PE Applied Biosystems). The reactions were denatured at 95°C for 10 min, followed by 35 cycles of 94°C for 45 s, 55 or 58°C for 30 s and 72°C for 1 min. For patients LP90-020, LP97-069 and LP93-005, PCR products were separated on a 4% polyacrylamide gel and the DNA extracted from the aberrant band. The DNA was then sequenced using DyeTerminator chemistry (PE Applied Biosystems). The primers used to amplify the aberrant RT–PCR products are as follows: patient LP85-002, LIS1-ex1F2 (5′-CGGTGGATGGGAGTGAAGGA-3′) and LIS1-ex7R (5′-CCAGTTTGCACTTCCCACAT-3′); patient 91-022, LIS1-ex2F (5′-TGTGGAAGACACTTAGTGGCATA-3′) and LIS1-ex7R; and the products were sequenced directly by DyeTerminator chemistry (PE Applied Biosystems). Proteins were extracted from lymphoblastoid cell lines of normal individuals and patients carrying missense and truncation/deletion mutations using a modified lysis buffer (50 mM Tris–HCl pH 5.4), 100 mM NaCl, 0.4% NP-40, pepstatine 10 µg/ml, 10 mM β-mercaptoethanol, 50 mM NaF, 1 mM Na3VO4, 30 mM pyrophosphate, 1 mM phenylmethylsulfonyl fluoride and protease inhibitors (CompleteMini; Boehringher Mannheim, Indianapolis, IN) by mixing for 5 min at 4°C. The extracts were centrifuged for 35 000 r.p.m. 160 000 g for 30 min at 4°C in an ultracentrifuge tube and the supernatant was frozen at –80°C. Protein expression was assessed by western blot analysis. In brief, samples were boiled and resolved by SDS–PAGE on 10% gels, which were subsequently transferred to an ECL nylon membrane (Amersham, Piscataway, NJ) for 1 h 30 min at 20 V using the genie electrophoretic blotter (Idea Scientific, Minneapolis, MN) in a buffer of Tris–glycine/20% methanol. The membrane was blocked for 1 h in 5 or 10% skim milk powder in Tris–buffered saline with 0.05% Tween 20 (TBST) at room temperature. The membranes were then incubated only with primary polyclonal anti-LIS1 (N-19) or monoclonal antiActin (C-2) antibodies or with both simultaneously (Santa Cruz Biotechnolgy, Santa Cruz, CA) for 1 h. HRP-conjugated secondary antibodies were incubated with the blot for 45 min at room temperature. Enhanced chemiluminescence reagents were used for detection (ECL plus; Amersham). An optical scanner (Storm 860; Molecular Dynamics) was used to image the western blot or alternatively X-ray films of western blots were scanned and densitometry was performed by using ImageQuant version 1.2 for Macintosh (Molecular Dynamics). Southern blot analysis Aliquots of genomic DNA (8 µg) from the patients and normal controls were digested with the restriction enzymes EcoRI, BamHI and HindIII and separated on a 1.0% agarose gel. The LIS1 cDNA clone 47 (20) was digested with EcoRI and the insert was used as a probe. Southern transfer, radiolabeling of the cDNA probe, hybridization to Southern blots and washes were performed as described previously (35). Computer database analysis using NCBI (http://www.ncbi.nlm.nih.gov/blast/ ) against human throughput genome sequences database (HTGS) indicated that the complete LIS1 gene is contained within the RPCI-11 BAC clones 135N5 (AC015799) and 74E22 (NT_000744) (unpublished data). BAC 135N5 contains the promoter region of the LIS1 gene and exons 1 and 2 only. BAC 74E22 overlaps BAC 135N5 in intron 2 and contains LIS1 exons 3–11 and the 3′ UTR. The complete genomic sequence of these two BACs is known. This sequence was used to generate an EcoRI restriction map. Southern blot hybridization was performed on EcoRI digests of control genomic DNA using each of the LIS1 exons as probes and compared with the same Southern blots hybridized with the complete LIS1 cDNA (clone 47) (31). Based on these data, we assigned each LIS1 exon to a specific band of the EcoRI digest. Therefore, Southern blot hybridization of EcoRI digests of patient genomic DNA was used to determine the extent of coding region deletions. The intronic borders of the deletions are unknown. An optical scanner (Storm 860; Molecular Dynamics, Sunnyvale, CA) was used to image the blot and the software ImageQuant (Molecular Dynamics) was used for densitometric analysis. Computer and statistical analysis The region of the coiled-coil domain was predicted with Stripe (version 2.0b1) (http://www.york.ac.uk/depts/biol/units/coils/ coilcoil.html ) using length 28 residues. Stripe employs algorithms described by Lupas et al. (36). These findings were confirmed using COILS version 2.2 (http://www.ch.embnet.org/ software/coils ). Due to the discreteness of lissencephaly severity grade, for which only four distinct values occurred among the 29 patients, categorical data methods were used to describe severity within each LIS1 genotype and to compare severity between genotypes. Within genotypes, the proportion of patients at each severity grade was tabulated. For comparisons, patients were cross-classified by severity grade and mutation type and Fisher’s exact test was applied to test the hypothesis of no association between genotype and phenotype. Fisher’s exact test is a method of performing inference in two-way contingency tables using exact distributions, when small sample sizes proscribe the use of χ2 tests. The Mann–Whitney U-test, an alternative non-parametric approach, produced the same qualitative results, both with and without adjustment for tied ranks. Statistical analysis was performed in Stata 6.0 (Stata, College Station, TX). ACKNOWLEDGEMENTS We would like to thank the patients with lissencephaly and their families as well as their physicians who referred them for 3028 Human Molecular Genetics, 2000, Vol. 9, No. 20 study. We gratefully acknowledge the help of Dr Melinda Drum and Dr Amy Elkund with the statistical analysis and Dr Francesca Zazzeroni with technical advice. This work was supported in part by a grant from the National Institutes of Health to W.E.B. and D.H.L. (PO1 NS39404) and the Lissencephaly Network. C.C. is supported by an INSERM Fellowship and the David and Janice Katz Fellowship in Human Genetics. R.J.L. is supported by the Australian College of Pediatrics Nestle Traveling Scholarship. REFERENCES 1. Dobyns, W.B., Truwit, C.L., Ross, M.E., Matsumoto, N., Pilz, D.T., Ledbetter, D.H., Gleeson, J.G., Walsh, C.A. and Barkovich, A.J. (1999) Differences in the gyral pattern distinguish chromosome 17-linked and Xlinked lissencephaly. Neurology, 53, 270–277. 2. Dobyns, W.B., Reiner, O., Carrozzo, R. and Ledbetter, D.H. (1993) Lissencephaly: a human brain malformation associated with deletion of the LIS1 gene located at chromosome 17p13. J. Am. Med. Assoc., 23, 2838– 2842. 3. Barkovich, A.J., Guerrini, R., Battaglia, A., Kalifa, G., N’Guyen, T., Parmeggiani, A., Santucci, M., Giovanardi-Rossi, P., Granata, T. and D’Incerti, L. (1994) Band heterotopia: correlation of outcome with magnetic resonance imaging parameters. Ann. Neurol., 36, 609–617. 4. Barkovich, A.J., Koch, T.K. and Carrol, C.L. (1991) The spectrum of lissencephaly: report of ten patients analyzed by magnetic resonance imaging. Ann. Neurol., 30, 139–146. 5. Pilz, D.T., Matsumoto, N., Minnerath, S.R., Mills, P., Gleeson, J.G., Allen, K.M., Walsh, C.A., Barkovich, A.J., Dobyns, W.B., Ledbetter, D.H. and Ross, M.E. (1998) LIS1 and XLIS (DCX) mutations cause most classical lissencephaly, but different patterns of malformation. Hum. Mol. Genet., 7, 2029–2037. 6. Lo Nigro, C., Chong, C.S., Smith, A.C., Dobyns, W.B., Carrozzo, R. and Ledbetter, D.H. (1997) Point mutations and an intragenic deletion in LIS1, the lissencephaly causative gene in isolated lissencephaly sequence and Miller–Dieker syndrome. Hum. Mol. Genet., 6, 157–164. 7. Reiner, O., Carrozzo, R., Shen, Y., Wehnert, M., Faustinella, F., Dobyns, W.B., Caskey, C.T. and Ledbetter, D.H. (1993) Isolation of a Miller– Dieker lissencephaly gene containing G protein beta-subunit-like repeats. Nature, 364, 717–721. 8. Peterfy, M., Gyuris, T., Basu, R. and Takacs, L. (1994) Lissencephaly-1 is one of the most conserved proteins between mouse and human: a single amino-acid difference in 410 residues. Gene, 150, 415–416. 9. Hattori, M., Adachi, H., Aoki, J., Tsujimoto, M., Arai, H. and Inoue, K. (1995) Cloning and expression of a cDNA encoding the beta-subunit (30 kDa subunit) of bovine brain platelet-activating factor acetylhydrolase. J. Biol. Chem., 270, 31345–31352. 10. Liu, Z., Xie, T. and Steward, R. (1999) LIS1, the Drosophila homolog of a human lissencephaly disease gene, is required for germline cell division and oocyte differentiation. Development, 126, 4477–4488. 11. Rohan, P.J., Davis, P., Moskaluk, C.A., Kearns, M., Krutzsch, H., Siebenlist, U. and Kelly, K. (1993) PAC-1: a mitogen-induced nuclear protein tyrosine phosphatase. Science, 259, 1763–1766. 12. Morris, N.R., Efimov, V.P. and Xiang, X. (1998) Nuclear migration, nucleokinesis and lissencephaly. Trends Cell Biol., 8, 467–470. 13. Hattori, M., Adachi, H., Tsujimoto, M., Arai, H. and Inoue, K. (1994) Miller–Dieker lissencephaly gene encodes a subunit of brain platelet-activating factor acetylhydrolase. Nature, 370, 216–218. [Erratum (1994) Nature, 370, 391.] 14. Hattori, M., Aoki, J., Arai, H. and Inoue, K. (1996) PAF and PAF acetylhydrolase in the nervous system. J. Lipid Mediators Cell Signal., 14, 99– 102. 15. Albrecht, U., Abu-Issa, R., Ratz, B., Hattori, M., Aoki, J., Arai, H., Inoue, K. and Eichele, G. (1996) Platelet-activating factor acetylhydrolase expression and activity suggest a link between neuronal migration and platelet-activating factor. Dev. Biol., 180, 579–593. 16. Adachi, T., Aoki, J., Manya, H., Asou, H., Arai, H. and Inoue, K. (1997) PAF analogues capable of inhibiting PAF acetylhydrolase activity suppress migration of isolated rat cerebellar granule cells. Neurosci. Lett., 235, 133–136. 17. Bix, G.J. and Clark, G.D. (1998) Platelet-activating factor receptor stimulation disrupts neuronal migration in vitro. J. Neurosci., 18, 307–318. 18. Clark, G.D., McNeil, R.S., Bix, G.J. and Swann, J.W. (1995) Platelet-activating factor produces neuronal growth cone collapse. Neuroreport, 6, 2569–2575. 19. Reiner, O., Albrecht, U., Gordon, M., Chianese, K.A., Wong, C., GalGerber, O., Sapir, T., Siracusa, L.D., Buchberg, A.M., Caskey, C.T. et al. (1995) Lissencephaly gene (LIS1) expression in the CNS suggests a role in neuronal migration. J. Neurosci., 15, 3730–3738. 20. Hirotsune, S., Fleck, M.W., Gambello, M.J., Bix, G.J., Chen, A., Clark, G.D., Ledbetter, D.H., McBain, C.J. and Wynshaw-Boris, A. (1998) Graded reduction of Pafah1b1 (LIS1) activity results in neuronal migration defects and early embryonic lethality. Nature Genet., 19, 333–339. 21. Sapir, T., Eisenstein, M., Burgess, H.A., Horesh, D., Cahana, A., Aoki, J., Hattori, M., Arai, H., Inoue, K. and Reiner, O. (1999) Analysis of lissencephaly-causing LIS1 mutations. Eur. J. Biochem., 266, 1011–1020. 22. Sweeney, K.J., Clark, G.D., Prokscha, A., Dobyns, W.B. and Eichele, G. (2000) Lissencephaly associated mutations suggest a requirement for the PAFAH1B heterotrimeric complex in brain development. Mech. Dev., 92, 263–271. 23. Sapir, T., Cahana, A., Seger, R., Nekhai, S. and Reiner, O. (1999) LIS1 is a microtubule-associated phosphoprotein. Eur. J. Biochem., 265, 181– 188. 24. Koch, A., Tonn, J., Albrecht, S., Sorensen, N., Wiestler, O.D. and Pietsch, T. (1996) Frequent intragenic polymorphism in the 3′ untranslated region of the lissencephaly gene 1 (LIS1). Clin. Genet., 50, 527–528. 25. Sapir, T., Elbaum, M. and Reiner, O. (1997) Reduction of microtubule catastrophe events by LIS1, platelet-activating factor acetylhydrolase subunit. EMBO J., 16, 6977–6984. 26. Lien, L.L., Boyce, F.M., Kleyn, P., Brzustowicz, L.M., Menninger, J., Ward, D.C., Gilliam, T.C. and Kunkel, L.M. (1991) Mapping of human microtubule-associated protein 1B in proximity to the spinal muscular atrophy locus at 5q13. Proc. Natl Acad. Sci. USA, 88, 7873–7876. 27. Harbury, P.B., Zhang, T., Kim, P.S. and Alber, T. (1993) A switch between two-, three- and four-stranded coiled coils in GCN4 leucine zipper mutants. Science, 262, 1401–1407. 28. Xiang, X., Osmani, A.H., Osmani, S.A., Xin, M. and Morris, N.R. (1995) NudF, a nuclear migration gene in Aspergillus nidulans, is similar to the human LIS1 gene required for neuronal migration. Mol. Biol. Cell, 6, 297– 310. 29. Smeal, T., Angel, P., Meek, J. and Karin, M. (1989) Different requirements for formation of Jun:Jun and Jun:Fos complexes. Genes Dev., 3, 2091–2100. 30. Fogli, A., Guerrini, R., Moro, F., Fernandez-Alvarez, E., Livet, M.O., Renieri, A., Cioni, M., Pilz, D.T., Veggiotti, P., Rossi, E. et al. (1999) Intracellular levels of the LIS1 protein correlate with clinical and neuroradiological findings in patients with classical lissencephaly. Ann. Neurol., 45, 154–161. 31. Chong, S.S., Pack, S.D., Roschke, A.V., Tanigami, A., Carrozzo, R., Smith, A.C., Dobyns, W.B. and Ledbetter, D.H. (1997) A revision of the lissencephaly and Miller–Dieker syndrome critical regions in chromosome 17p13.3. Hum. Mol. Genet., 6, 147–155. 32. Capecchi, M.R., Capecchi, N.E., Hughes, S.H. and Wahl, G.M. (1974) Selective degradation of abnormal proteins in mammalian tissue culture cells. Proc. Natl Acad. Sci. USA, 71, 4732–4736. 33. Gleeson, J.G., Lin, P.T., Flanagan, L.A. and Walsh, C.A. (1999) Doublecortin is a microtubule-associated protein and is expressed widely by migrating neurons. Neuron, 23, 257–271. 34. Fox, J.W., Lamperti, E.D., Eksioglu, Y.Z., Hong, S.E., Feng, Y., Graham, D.A., Scheffer, I.E., Dobyns, W.B., Hirsch, B.A., Radtke, R.A. et al. (1998) Mutations in filamin 1 prevent migration of cerebral cortical neurons in human periventricular heterotopia. Neuron, 21, 1315–1325. 35. Kubota, T., Sutcliffe, J.S., Aradhya, S., Gillessen-Kaesbach, G., Christian, S.L., Horsthemke, B., Beaudet, A.L. and Ledbetter, D.H. (1996) Validation studies of SNRPN methylation as a diagnostic test for Prader–Willi syndrome. Am. J. Med. Genet., 66, 77–80. 36. Lupas, A., Van Dyke, M. and Stock, J. (1991) Predicting coiled coils from protein sequences. Science, 252, 1162–1164. 37. Fogli, A., Giglio, S., Arrigo, G., Lo, N.C., Zollo, M., Viggiano, L., Rocchi, M., Archidiacono, N., Zuffardi, O. and Carrozzo, R. (1999) Identification of two paralogous regions mapping to the short and long arms of human chromosome 2 comprising LIS1 pseudogenes. Cytogenet. Cell Genet., 86, 225–232.