* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 10 Pharmacologic Management Of Parkinsonism
Survey
Document related concepts
Atypical antipsychotic wikipedia , lookup
Prescription costs wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Drug interaction wikipedia , lookup
Toxicodynamics wikipedia , lookup
NMDA receptor wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Norepinephrine wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Chlorpromazine wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Transcript
CHAPTER 28
Pharmacologic Management of
Parkinsonism and Other
Movement Disorders
Neurodegenerative Diseases
• Neurodegenerative
diseases are characterized by the
progressive and irreversible loss of selected neurons in
discrete brain areas, resulting in characteristic disorders of
movement, cognition, or both
• The
neurodegenerative disorders include Alzheimer's
disease, Parkinson's disease, Huntington's disease, and
amyotrophic lateral sclerosis
Neurodegenerative Diseases
• Most neurodegenerative disorders are of unknown etiology,
affect the elderly, & are progressive
• Drug therapy is currently very limited, except in the case of
Parkinson's disease (PD)
• There are some inherited forms of these disorders; however,
most are sporadic occurrences (idiopathic) with genetic
predisposition, environmental factors, and aging contributing
as risk factors
Overview of Parkinson's Disease
• PD is a progressive neurological disorder of muscle movement,
characterized by combination of rigidity, bradykinesia, resting
tremor, and postural instability. Cognitive decline occurs as
the disease advances
• It generally affects the elderly and is estimated to afflict more
than 1% of individuals over the age of 65
• PD is correlated with destruction of dopaminergic neurons in
the substantia nigra with a consequent reduction of dopamine
actions in the corpus striatum
Overview of Parkinson's Disease
• Thus, the normal modulating inhibitory influence of dopamine
on cholinergic neurons in the neostriatum is significantly
diminished, resulting in overproduction or a relative
overactivity of acetylcholine by the stimulatory neurons
• This triggers a chain of abnormal signaling, resulting in loss of
the control of muscle movements
• The mechanisms responsible for the degeneration of dopamine
neurons are not known, but it may be the result of cerebral
ischemia, viral encephalitis or other types of pathological
damage
Overview of Parkinson's Disease
• The pathophysiologic basis of the idiopathic disorder may
relate to exposure to some unrecognized neurotoxin or to
oxidation reactions free radicals generation
• Genes?? Studies in twins suggest that genetic factors may be
important, especially in patients under age 50
• Drugs?? Dopamine receptor antagonists (eg, antipsychotic
agents) or drugs that lead to destruction of the dopaminergic
nigrostriatal
neurons
(e.g.
1-methyl-4-phenyl-1,2,3,6tetrahydropyridine [MPTP] may induce parkinsonian syndrome
Strategy of treatment
• Since there is no cure for PD, the aim of pharmacological
therapy is to provide symptomatic relief to alleviate many
of the motor features of the disorder
• This
is
obtained
re-establishing
the
correct
dopamine/acetylcholine balance through the use of drugs
that either increase dopaminergic actions or antagonizing
the excitatory effect of cholinergic neurons
Drugs Used in Parkinson's Disease
• Drugs used in Parkinson’s disease include:
1) Levodopa-carbidopa
2) Dopamine agonists
3) Monoamine oxidase (MAO) inhibitors
4) Cathechol-O-methyl transferase (COMT( inhibitors
5) Anticholinergic agents
6) Amantadine
Levodopa-carbidopa
• Dopamine does not cross the BBB…..if given into the peripheral
circulation has no therapeutic effect in parkinsonism
• Levodopa (the immediate metabolic precursor of DA) is the
single most effective agent in the treatment of PD
• Oral levodopa is absorbed rapidly from the small intestine and
transported into the brain by the transport system for aromatic
amino acids
• Levodopa is itself largely inert
• Therapeutic and adverse effects of levodopa result from its
decarboxylation to dopamine
Levodopa-carbidopa
• Certain a.as from ingested food can compete with levodopa for
absorption from gut & for transport from blood to brain
• About 1–3% of administered levodopa actually enters the brain
unaltered; the remainder is metabolized extracerebrally,
predominantly by decarboxylation to dopamine in the
periphery……does not penetrate the BBB???
• …….It is combined with a peripheral dopa decarboxylase
inhibitor (e.g. carbidopa)
Levodopa-carbidopa
• A dopa decarboxylase inhibitor that does not cross the
BBB
• Carbidopa:
a.
b.
c.
d.
e.
Reduce the metabolism of L-dopa in the GIT and periphery
Plasma levels are higher, and plasma half-life is longer
Increases the availability of levodopa to the CNS
Reduce the daily requirements of levodopa by
approximately 75%
Decreases the severity of the side effects arising from
peripherally formed dopamine
Levodopa-carbidopa
Clinical use
• Levodopa is widely used for treatment of all types of PD except
those associated with antipsychotic drug therapy
• Levodopa substantially reduces the severity of all the signs and
symptoms of PD in the first few years of treatment
• Patients then typically experience a decline in response after 3
or 4 years of therapy…….due to progression of the disease and
loss of striatal dopamine nerve terminals as well as reduction of the
daily dose to avoid adverse effects
Levodopa
ADRs
A. Gastrointestinal tract (GIT)
• Anorexia, nausea, and vomiting (likely due to dopamine’s
stimulation of the CTZ but outside the BBB)
• Minimized by taking the drug in divided doses, with or
immediately after meals, and increasing the total daily dose
very slowly. Antacids 30–60 min before levodopa may also be
beneficial
• When levodopa is given in combination with carbidopa,
adverse GIT effects are much less frequent & patients can
tolerate proportionately higher doses
Levodopa
ADRs
B. Cardiovascular effects
• Cardiac arrhythmias: caused by increased catecholamine
formation peripherally (incidence is low)
• Peripheral decarboxylation of levodopa and release of DA into
the circulation may activate vascular DA receptors and produce
orthostatic hypotension
• Administration with nonspecific MAOI, accentuates the actions
of levodopa and may precipitate life-threatening hypertensive
crisis
• Incidence reduced if taken with carbidopa
Levodopa
ADRs
C. Dyskinesias
• Occur in up to 80% of patients receiving levodopa for more
than 10 years
• Choreoathetosis of the face and distal extremities is the most
common presentation
• The development of dyskinesias is dose-related but there is
considerable individual variation in the dose required to
produce them
Levodopa
ADRs
E. Fluctuations in Response
• Ooccur with increasing frequency as treatment continues…
I.
Wearing-off phenomenon/ end-of-dose akinesia:
• Related to the timing of levodopa intake
• Each dose of levodopa effectively improves mobility for a
period of time (1–2 hrs), but rigidity and akinesia return
rapidly at the end of the dosing interval
• Increasing the dose and frequency of administration can
improve this situation
Levodopa
ADRs
E. Fluctuations in Response
On-off phenomenon
• Fluctuations in response unrelated to timing of doses
II.
• Off-periods of marked akinesia alternate with on-periods of
improved mobility but often marked dyskineisa
• Lower incidence occur when levodopa is administered more
continuously
Levodopa
ADRs
F. Behavioral Effects
• Depression, anxiety, agitation, insomnia, somnolence,
confusion, delusions, hallucinations, nightmares, euphoria, and
other changes in mood or personality
• More common in patients taking levodopa in combination with
carbidopa (higher levels are reached in the brain)
• Several “atypical” antipsychotic agents with low D2 affinity are
now available and effective in the treatment of psychosis
Drug Interactions of levodopa
• Pyridoxine (vitamin B6): increase extracerebral metabolism of
levodopa and may prevent its therapeutic effect unless
carbidopa is also taken
• Nonspecific MAO inhibitors (e.g. phenelzine):
• Accentuates the actions of levodopa and may precipitate life-
threatening hypertensive crisis
• MAO inhibitors must be discontinued at least 14 days before
levodopa is administered
Levodopa
• Contraindications:
Psychotic patients
2) Angle-closure glaucoma (cause severe mydriasis)
1)
• Careful management in patients with:
a) History of cardiac arrhythmias or recent cardiac
infarction….(+ carbidopa)
b) Active peptic ulcer must be managed carefully (GI
bleeding occasionally occurred with levodopa)
c) History of melanoma or with suspicious undiagnosed
skin lesions (precursor of melanin)
Monoamine Oxidase Inhibitors
• Two types of monoamine oxidase in the nervous system:
(MAO-A and MAO-B)….non-selective & selective
• The isoenzyme MAO-B is the predominant form in the striatum
and is responsible for most of the oxidative metabolism of
dopamine in the brain
• Blockade of dopamine metabolism makes more dopamine
available for stimulation of its receptors
• Selective MAO-B Inhibitors: Selegiline & Rasagiline
Selegiline
• Irreversible inhibitor of MAO-B…..retards the breakdown of
dopamine
• Higher doses lose selectivity
• Used as adjunctive therapy for patients with declining or
fluctuating response to levodopa
• Enhances and prolongs the antiparkinsonism effect of
levodopa (less doses are needed) and may reduce mild onoff or wearing-off phenomena
Rasagiline
• Irreversible and selective inhibitor of brain (MAO) Type B
• It is more potent than selegiline in preventing MPTP-
induced parkinsonism and is being used for early
symptomatic treatment
• Rasagiline is also used as adjunctive therapy to prolong
the effects of levodopa-carbidopa in patients with
advanced disease
Monoamine Oxidase Inhibitors
• Neither selegiline nor rasagiline should be taken by
patients receiving opioid analgesic (stupor, rigidity,
agitation, and hyperthermia)
• They should be used with care in patients receiving TCAs
or SSRIs b/c of the theoretical risk of acute toxic
interactions of the serotonin syndrome type (rare)
• ADEs:
o Most related to the increased levels of dopamine
o Anxiety, insomnia (selegiline)
Catechol-O-Methyltransferase Inhibitors
• Methylation of L-DOPA by catechol-O-methyltransferase
(COMT) to 3-O-methyldopa is a minor pathway
• High 3-OMD levels have been associated with a poor
therapeutic response to levodopa
• 3-OMD competes with L-DOPA for its transportation across
the intestinal mucosa and the BBB…..
• 2 Selective COMT inhibitors: Tolcapone & Entacapone
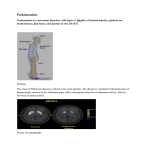
Levodopa
Effect of entacapone on dopa concentration in the central nervous
system (CNS). COMT = catechol-O-methyltransferase
Catechol-O-Methyltransferase Inhibitors
• Are particularly helpful in patients receiving levodopa who
have developed response fluctuations—thus leading to a
smoother response, more prolonged on-time, and the
option of reducing total daily levodopa dose
Catechol-O-Methyltransferase Inhibitors
• Tolcapone is more potent than entacapone with longer
duration of action…..taken 3 times daily while, entacapone
taken with each dose of levodopa, up to five times daily
• In addition tolcapone has both central and peripheral effects,
while entacapone just peripheral
• ADRs:
o Due to high L-DOPA exposure; dyskinesias, nausea & confusion
o Orange discoloration of the urine
o Tolcapone requires signed patient consent….hepatoxicity, and
monitor liver functions
Dopamine Receptor Agonists
• Drugs acting directly on DA receptors may have a beneficial
effect in addition to that of levodopa:
1)
2)
3)
4)
5)
6)
Do not require enzymatic conversion to an active metabolite
Have no potentially toxic metabolites
Do not compete with other substances for active transport into
the blood and across the BBB
Selectively affect certain dopamine receptors
More limited adverse effects than levodopa
Longer durations of action than of levodopa…..thus are effective
in patients exhibiting fluctuations in their response to L-dopa
Dopamine Receptor Agonists
• Dopamine agonists may delay the need to employ levodopa therapy
in early PD and may decrease the dose of levodopa in advanced
Parkinson's disease
• Dopamine receptor agonists:
Ergot derivatives e.g. bromocriptine & pergolide
2. Non-ergot derivatives e.g. apomorphine, pramipexole,
ropinirole, and rotigotine
1.
• The differences between the ergot derivatives and the newer/ non-
ergot agents reside primarily in their adverse effects, and tolerability
Dopamine receptors
• The actions of dopamine in the brain are mediated by a family of
dopamine-receptor proteins
• All the dopamine receptors are heptahelical G protein-coupled
receptors (GPCRs)
• Five dopamine receptors have been identified, and they fall into two
groups on the basis of their pharmacological and structural
properties:
• D1-like receptors (D1 & D5)
• D2-like receptors (D2, D3, D4)
• D1 receptors, which stimulate the synthesis of the intracellular
second messenger cyclic AMP, and D2 receptors, which inhibit cyclic
AMP synthesis
Dopamine receptors
• The benefits of dopaminergic antiparkinsonism drugs depend
mostly on stimulation of D2 receptors located postsynaptically
on striatal neurons and presynaptically on axons in the
substantia nigra belonging to neurons in the basal ganglia
• Whereas certain dopamine blockers that are selective D2
antagonists can induce parkinsonism
• Dopamine receptors of the D1 type are located in the pars
compacta of the substantia nigra and presynaptically on striatal
axons coming from cortical neurons and from dopaminergic
cells in the substantia nigra
Dopamine Receptor Agonists
Ergot derivatives: BROMOCRIPTINE & PERGOLIDE
• Bromocriptine is a D2 receptor agonist, whereas pergolide is an
agonist of both D1 and D2 receptors
• Postural hypotension, nausea, somnolence, and fatigue are
ADRs of both therapy and can limit their use
• Because of these ADRs, the drugs are generally first
administered at low doses and then the dose is gradually
increased over weeks or months as tolerance to the adverse
effects develops
Dopamine Receptor Agonists
Non-ergot derivatives: PRAMIPEXOLE & ROPINIROLE
• Pramipexole has selective activity at D3, whereas ropinirole is a
relatively pure D2 receptor
• Can be initiated more quickly, achieving therapeutically useful
doses in a week or less and generally cause less GI disturbance
than do the ergot derivatives
• Effective as monotherapy for mild parkinsonism, in patients
with advanced disease, permit the dose of levodopa to be
reduced and smoothing out response fluctuations
Dopamine Receptor Agonists
ROTIGOTINE
• Available as a transdermal patch…..administered once-
daily and provides continuous dopaminergic supply
• Used in the Tx of the signs and symptoms of early
stage PD
• Recalled in USA because of crystal formation on the
patches, affecting the availability and efficacy of the
agonist….still available in europe
Dopamine Receptor Agonists
APOMORPHINE (Apokyn®)
• Apomorphine is an injectable (s.c) potent dopamine
agonists
• It is effective for the temporary relief ("rescue") of off-
periods of akinesia in patients on optimized dopaminergic
therapy
• It is rapidly taken up in the blood and then the brain,
leading to clinical benefit that begins within about 10
minutes of injection and persists for up to 2 hours
Dopamine Receptor Agonists
ADRs
A. Gastrointestinal tract effects:
• Anorexia, N & V: can be minimized by taking the
medication with meals
• Constipation,
dyspepsia,
and
symptoms
of
reflux
esophagitis
• Bleeding from peptic ulceration
• N.B: nausea is often severe with apomorphine….pretreatment
with the antiemetic for 3 days is recommended
Dopamine Receptor Agonists
ADRs
B. Cardiovascular effeects:
• Postural hypotension common at the initiation of therapy
especially with the ergot derivatives
• Dose-related
painless digital vasospasm with the ergot
derivatives
• Cardiac arrhythmias (discontinuation)
• Peripheral edema may be problematic
• Cardiac valvulopathy with pergolide (withdrawn in the US)
Dopamine Receptor Agonists
ADRs
C. Dyskinesias: abnormal movements similar to those
introduced by levodopa reversed by reducing the total
dose of dopaminergic drugs
D. Mental Disturbances:
•
Include confusion, hallucinations, delusions, and other
psychiatric reactions which are more common and severe
with dopamine receptor agonists than with levodopa
Dopamine Receptor Agonists
ADRs
E. Miscellaneous Adverse Effects (ergot derivatives)
o Headache, Nasal congestion
o Increased arousal, Pulmonary infiltrates
o Erythromelalgia (red, tender, painful, swollen feet &,
occasionally, hands, at times associated with arthralgia)
….Signs clear within a few days of withdrawal of the causal
drug
Dopamine Receptor Agonists
Contraindications
1. History of psychotic illness
2. Recent MI
3. Active peptic ulceration
4. Peripheral vascular disease (ergot derivatives)
Amantadine
• Antiviral agent, was by chance found to have
antiparkinsonism properties
• Its MOA in parkinsonism is unclear. However it may:
a. Influencing the synthesis, release, or reuptake of dopamine
b. Antagonize the effects of adenosine at adenosine A2A
receptors
c. Release of catecholamines from peripheral stores
• Less effective than L-dopa, benefits is short-lived (few
weeks)
ADRs…..reversible by stopping the drug
1) CNS: restlessness, depression, irritability, insomnia, agitation,
excitement, hallucinations, & confusion
2) Acute toxic psychosis & convulsions (overdosage)
3) Peripheral edema….respond to diuretics
4) HF, Postural hypotension
5) Urinary retention, constipation, & dry mouth
6) GI disturbances: anorexia & nausea
Acetylcholine-Blocking Drugs
• Centrally
acting
antimuscarinic
drugs
include:
benzotropine
mesylate,
biperiden,
orphenadrine,
procyclidine, & trihexphenidyl
• Improve
tremor and rigidity with little effect on
bradykinesia
• Less efficacious than L-DOPA and thus are most commonly
used during the early stages of the disease or as an
adjunct to levodopa therapy
ADRs
• The adverse effects of these drugs are a result of their
anticholinergic properties (CNS & peripheral effects)
1. CNS: mental confusion, delirium, and hallucinations
2. Peripheral: constipation, urinary retention, and blurred
vision through cycloplegia, sinus tachycardia, & dry mouth
• Are contraindicated in patients with glaucoma, prostatic
hyperplasia, or pyloric stenosis