* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download doc GIT
Premovement neuronal activity wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Molecular neuroscience wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
End-plate potential wikipedia , lookup
Central pattern generator wikipedia , lookup
Electromyography wikipedia , lookup
Proprioception wikipedia , lookup
Synaptogenesis wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Neuromuscular junction wikipedia , lookup
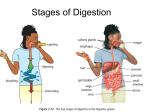
PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler Lecture 02 – March 24th 2006 In the GIT, there are 3 identifiable forms of activity: 1- Motility 2- Secretion 3- Absorption Motility: What brings about propulsion & the physical breakdown of food The key elements involved in the motility are the 2 layers of muscles: longitudinal & circular fibers of the muscularis externa. The uppermost regions (mouth, pharynx and upper 1/3 of the esophagus) as well as the external anal sphincter are striated muscles. They have specific properties. The remaining regions are composed of smooth muscles. Their regulation will be diff. Propulsion (Flow in the GIT) Propulsion in the GIT depends on gradients of pressure (High to Low). Also depends inversely on resistance. The more resistance there is downstream, the more difficult it is to propel some substances downstream. There are 2 types of contractile activity within the GIT: o The length of the GIT periodically contracts at various points which gives rise to sausage-like segments. These are followed by periods of relaxation. → Very effective mixing mvt. They can also be involved in the propulsion of the meal away from the mouth. o Propagated wave of contraction (PERISTALSIS): moves contents in one direction → plays major role in most regions of the GIT in mediating propulsion Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 1 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler Resistance: at normal circumstances, the meal encounters few. It used to be thought that the various sphincters which separate the organs of the GIT played a major role regulating the transport of the meal. We now know that, normally, these sphincters do NOT offer resistance. They actually open reflexely, anticipating the arrival of the meal contents in the lumen of the GIT. They allow the meal to go thru and close to prevent regurgitation of the contents from 1 organ to the organ above it. Pathologically, there are situations that prevent the sphincters to relax or more commonly, there are situations that prevent the sphincters to close completely & allow for reflux to happen. However, NORMALLY, there is little or no resistance. Normally, the flow is slow (several hours for the meal to go the GIT), aboral (away from the mouth towards the anus) and meets little/no resistance. First propulsive force : DEGLUTITION (Vander’s pp. 590-593) Immediately after digestion Deglutition is a process which involves highly coordinated muscular activities. Result: transport of the food thru the oral cavity, across the pharynx, into the esophagus & all the way into the stomach. We usually discuss the mechanical of deglutition in terms of 3 phases: Oral: transport thru the oral cavity Pharyngeal: transport across the pharynx Esophageal: transport into the stomach All these phases proceed smoothly and sequentially Deglutition (swallowing): is accomplished thru a complex series of highly coordinated muscular mvts aimed at building up pressure, temporarily sealing off of compartments to prevent dissipation of pressure and decreasing resistance (by relaxation of the sphincters) Oral phase Transport from anterior portion of the mouth into the pharynx voluntary control You take a morsel of food, you chew it & it becomes coated w/ saliva. Thru the combined actions of muscles in cheeks, lips tongue, the food is brought on the upper surface part of the tongue. Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 2 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler Once it is in that position, thru the elevation of the upper tip of the tongue and retraction of the lower tip, the food is rolled b/w the tongue and palate, it takes a rounded shape and becomes known as the bolus. It rolls to the back of the mouth and the bolus is projected into the pharynx The oral phase of deglutition is under voluntary control. You can start/stop to swallow at will. From evolutionary standpoint: transport across the rest of the GIT is involuntary (except defecation, which can be initiated voluntarily). The initiation is voluntary, but the act itself is carried out by highly coordinated reflexes (by definition, involuntary) Oral phase: transport of bolus (masticated, ensalivated mass of food) from anterior to posterior portion of mouth This involves a series of reflexes coordinated in deglutition centre in medulla oblongata Cortical vs Medullary centers There is a region in the precentral cortex of the gyrus that, when stimulated, will initiate swallowing. Also involves reflexes that are initated by presence of food in the mouth that are coordinated in the medulla oblongata which is the deglutition center. → can carry out the sequence of mvt involved in the oral phase of deglutition When you voluntarily swallow, the impulses from the cortical center facilitate the reflexes which are coordinated in the deglutition centre (this also applies to the defecation) Voluntary – in cortex Deglutition centre – “involuntary” – in the medulla Oral Phase 1. ability to initiate: voluntary (cortex) 2. coordinated movements: reflex, involuntary (medulla) Pharyngeal Phase Pharynx: where the respiratory and digestive pathways cross Pathway from the nose, across the pharynx into the trachea & pathway across the mouth, thru the pharynx and into the esophagus It is obvious that for swallowing to occur safely and w/ right pressure for the bolus to enter esophagus, all the openings leading from the phrarynx, have to be closed (protect the resp passages). The pharangeal phase is strictly involuntarily (automatic). Once the bolus has entered the pharynx, we can no longer control anything. Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 3 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler This involves coordinated reflexes, activated by pharyngeal receptors that send afferent impulses to the deglutition center in medulla. The efferent output gives rise to a # of events. There are a series of protective rxns that separate the digestive tract from the respritory tract. To further control this, there is temporary apnea (for fractions of seconds). Respiration is temporarily arrested. Then, the upper esophageal sphincter relaxes (to ↓ resistance & release pressure) and the pharynx muscles contract to push the bolus down (generated by pressure gradient). The passages into the nose: Soft palate is raised for the food not to go into the nose. Base of tongue raised: prevent food from going back into the mouth. Trachea (entire larynx) is raised upwards and moved forward to fit under the base of tongue. Upward mvt of the larynx is the major protective mechanism of the resp syst (glottis is closed, the vocal cords are pulled together). → apnea Then, relaxation of the UES and the pharynx muscles push bolus down. The bolus also presses down on the epiglottis. Epiglottis also flips over and offers further, secondary protection. There are about 25 diff. muscles that must contract to assure safe swallowing. Pharyngeal Phase – Involuntary 1. passages into nose, mouth and trachea are blocked 2. apnea 3. UES relaxes 4. Pharynx muscles contract In elderly: aspiration pneumonia inappropriate deglutition, so food goes into lungs and brings bacteria in Pharyngeal Phase under involuntary control – consists of a) a series of protective reflexes, initiated by stimulation of afferent fibres in the pharynx, organized in deglutition center, Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 4 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler closing off nasal, oral and larygeal cavities, preventing misdirection of the bolus simultaneously… b) transfer to esophagus, as pharyngeal muscles contract and upper esophageal sphincter relaxes Deglutition Reflexes The pharyngeal reflex consists of the following steps: 1- There are pharyngeal receptors that send information, thru afferent nerves, to the deglutition center in the medulla. 2- From here, there is efferent info sent to the diff. parts of the pharynx in a coordinated fashion in order to control the whole INVOLUNTARY phase of pharyngeal deglutition. Upper esophageal sphincter Corresponds anatomically to the cricopharyngeus muscle. This muscle is usually kept contracted → always closed (normally) Train of impulses that are mediated to this muscle along the vagus nerve keeps it closed. Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 5 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler This is striated muscle, so there is direct innervation by the vagus nerve. There is release of ACh that acts on nicotinic receptors (block with curare) causing contraction of the cricopharyngeal muscle. During swallowing, the muscle is relaxed. Relaxation is mediated by the arrest of these impulses. From the deglutition center, there is inhibition of these excitatory impulses that arrive to the muscle. Vagus nerve innervates the cricopharyngeus thru ACh (Nicotinic receptors) closure – impulses originate in CNS, mediated by vagus, releasing ACh, causing muscle contraction relaxation – mediated by cessation/arrest of impulses, results in muscle relaxation Pharyngeal phase 1. Involuntary 2. Rapid – takes 1/5th of a second (we are not aware that we stopped breathing and talking) 3. “stereotyped” -- Automatic. The sequence proceeds w/o modification in normal circumstances 4. temporospatial coordination – muscles contract in appropriate order & w/ particular strength (sequencial and appropriate matter for this stereotyped response) Esophageal phase Simplest portion of the digestive. No digestion or absorption. The main fctn are muscular to allow transport of the bolus from the pharynx all the way along the esophagus into the stomach. It is a very muscular organ. Both the circular and longitudinal layer are well-developed. Upper regions of the esophagus are striated, and the lower regions becomes smooth Body of esophagus lies within thoracic cavity – therefore, it is subjected to the intrathoracic pressure (it is negative, -5 to -10 mmHg; so the pressure in the esophagus is also negative). The consequence of this is that you have a (-) pressure in the organ, and above it, in the pharynx it is higher (atmospheric) and below it, in the stomach, it is positive (+5-10mmHg). So we can appreciate the role of the UES and LES w/o contracted sphincters you would always be aspirating air and saliva into the esophagus (UES) and refluxing the acidic gastric contents into the esophagus (LES). Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 6 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler The innervation of these upper and lower esophagus regions is diff. both by vagus nerve. In striated region, the innervation is direct (somatic vagal fibers release ACh which acts on nicotinic receptor). The smooth muscle indirect innervation. It synapses w/ enteric neurons, which will then act on the muscular cells. There are 2 forces that play a role in pushing down the bolus: 1. gravity (minor role → facilitates flow of non-viscous material down the esophagus) 2. peristalsis (major mech to carry bolus down the esophagus) – propagated wave of contraction that narrows the lumen and sets up a gradient of pressure which favors aboral mvt Each time we swallow, a primary (single) peristaltic wave is generated. There is a definite link b/w the # of times we swallow and the # of primary peristaltic wave. (If swallow once a minute → one peristaltic wave) It takes 8-10 secs for the bolus to move from the lower part of the UES to be brought into the stomach The primary peristaltis waves are part of the deglutition reflexes. When the pharyngeal receptors are stimulated, they set into motion reflexes that result in primary peristalsis moving along the esophagus. The stimulation of the pharyngeal receptors sends afferent impulses to the deglutition centers, from where the vagal somatic fibers to the striated muscle portion will be activated & these impulses arrive sequentially. It is a smoothly propagated wave (in the striated muscle region). Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 7 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler The autonomic vagal fibers to the distal region of the esophagus are activated. But the excitation arrives synchronously in all the vagal fibers to this region. There is delay in the activation of enteric neurons, so the muscle here is also activated sequentially (not b/c the impulses arrive sequentially which delay to the muscle, but b/c of the progressive delay in activation of the enteric neurons) The significance of having 2 types of innervation: In the esophagus, there is a peristaltic wave moving over the entire organ (moves down). The innervation & the responses of the musculature are diff. (striated and smooth). If you cut the vagus nerve high up in the neck so that the somatic and the autonomic fibers are disrupted, you can no longer generate a primary peristaltic wave. You need the vagus nerve to be intact in order to do that. If you leave the somatic vagal innervation intact, but you cut the vagus at the level of the atria, trans-thoracically. As long as you leave the somatic fibers intact and a few autonomic vagal fibers innervating some of the enteric neurons intact, the primary peristaltic wave will be carried and uninterrupted: the distal esophagus, once you have activated only a few of the enteric neurons, there is relay b/w the enteric neurons that is preprogrammed so that the wave is propagated. So the vagus is ESSENTIAL for initiating peristalsis in proximal esophagus. (striated muscle) But, if you activate just a few of the enteric neurons in smooth muscle, there will be propagation of the peristaltic wave, so the continuation & propagation in the distal part relies mainly on the intactness of the enteric innervation. Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 8 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler When you have a large bolus of food: Local distension within the body of the esophagus created by the presence of a large bolus, will gives rise to secondary peristaltic wave (stimulus: local distension). This may be mediated by short intramural enteric reflexes (stimulate at one pt and give rise to activation at a diff. pt, mediated by enteric nerves). There are also activation of sensory afferent vagal fibers up from the gut to the CNS, resulting in efferent output. So we have several secondary peristaltic waves generated until the bolus has been displaced. Lower Esophageal Sphincter Corresponds anatomically to the terminal 4 cm of the esophagus. Not an anatomically distinct region (hardly recognizable anatomically) Functionnaly imp. b/c it allows a pH gradient of 5 units (esophagus = 7 and stomach = 2). It is contracted tighly, preventing reflux of gastric contents. The closure of this region to act as sphincter is thought to be myogenic (property of that muscle to remain tonically contracted at rest even in the absence of innervation, either vagal or enteric) Relaxation: neurogenic results from the local release of NANC inhibitory neurotransmitter During swallowing, it is the vagus nerve that activated these inhibitory enteric neurons allowing for the relaxation of the sphincter. Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 9 PHGY 210 – Digestion Lecture02 Friday, March 24, 2006 Ann Wechsler Pharyngeal receptors Enteric activation also brings of the relaxation of LES. The LES normally straddles the diaphragm. 2 cm are in the thorax, and 2 cm are in the abdominal cavity. The area that lies in the abdominal cavity gives additional protection to the prevention reflux. Any increase in the intra-abdominal pressure increases pressure equally on the stomach & on LES. In individuals that have a hiatus hernia (all LES is in the thoracic cavity), this doesn’t happen. They have a greater tendency to reflux. In pregnancy, in later months, women have a tendency to reflux. b/c as the uterus grows, it displaces the abdominal organs upwards and a hiatus hernia develops. The sphincter – intrinsic property of the muscle, helped by intraabdominal segment Reflux – pyrosis (heart burn) It used to be thought that gastrin tightened the LES. → false Gastrin plays a role in the secretion of acid, doesn’t cause the LES to contract, the only hormone which acts to relax the LES is progesterone. (2nd reason why women who are pregnant or are on the pill have higher tendency to reflux) Sarantis Abatzoglou, Natasha Cohen, Emilie Trinh page 10