* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The investigation of enzymes structure, physical
Metabolic network modelling wikipedia , lookup
Enzyme inhibitor wikipedia , lookup
Western blot wikipedia , lookup
Point mutation wikipedia , lookup
Peptide synthesis wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Lipid signaling wikipedia , lookup
Butyric acid wikipedia , lookup
Genetic code wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Metalloprotein wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Specialized pro-resolving mediators wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Proteolysis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Citric acid cycle wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Amino acid synthesis wikipedia , lookup
1
Table of contents
Module 2. The common mechanisms of metabolism. Metabolism of
carbohydrates, lipids and proteins. Regulation.
Substantial module 2. 1. The role of enzymes and vitamins in metabolism"
Topic 2.1.
Topic 2.2.
Topic2.3.
Topic 2.4.
The control of original knowledge level. Subject and task of biochemistry.
The investigation of protein structure and physical-chemical properties.
Quantitative definition of protein by the biuretic method. The proof of protein
nature of enzymes. ……...............................................................................
P.3-6
The investigation of enzymes structure, physical-chemical properties and
conditions of action ………………………………………………………….. P 7-9.
Determination of enzyme activity. Investigation of enzyme catalysis kinetics …..P.10-12
and activators and inhibitors influence on enzyme activity.
Investigation of the vitamins coenzyme form role in catalytic enzymes activity. P.13-15
Topic 2.5. Investigation of the vitamins and vitamins coenzyme form function ……………...P.16-18
In different biochemical processes.
Substantial module 2. 2“ Basic concepts of metabolism, bioenergetics.
Investigation of oxidative phosphorylation and ATP synthesis. Inhibitors ………P.19-22
and uncouples of oxidative phosphorylation.
Topic 2.7. Bioenergetics and general pathways of a metabolism. The investigation of…….. P.23-25
citric acid cycle action.
Topic 2.6.
Substantial module 2. 3 “Metabolism of carbohydrates, its regulation”.
Topic 2.8.
Topic 2.9.
Topic 2. 10
Investigation of carbohydrate digestion peculiarities. Glycogen biosynthesis P. 26-29
and degradation. Conversion of monosacharides to glucose in the liver.
Anaerobic oxidation of carbohydrates. Glycolysis. Synthesis of glucose –
gluconeogenesis. ……………………………………………………………… P. 30-32
Investigation of aerobic oxidation of glucose. Pentose phosphate pathway….. P. 33-35
of glucose conversion.
Substantial module module 2. 4“Metabolism of lipids, its regulation”.
Topic 2. 11
Structure and functions of cellular membranses.
P.36-40
Topic 2. 12
Investigation of lipids digestion peculiarities. Possible disturbanses of
P. 41-44
exogenic lipids digestion, absorbtion and transtort.
Topic 2. 13
Investigation of fatty acids and keton bodies metabolism. β-oxidation of fatty P. 45-49
acids. Cholesterol synthesis and steroid metabolism. Disturbances of lipid
metabolism atherosclerosis.
Topic 2. 14 Investigation of fatty acids, triacylglycerol and phospholipid synthesis. ….. P. 50-52
Disturbances of lipid metabolism: obesity; lipid dystrophy of the liver.
Substantial module 2. 5 “Metabolism of amino acids, its regulation”.
Topic 2.15
Investigation of gastric juice chemical composition. Studies of proteins
digestion peculiarities.
P. 53-57
2
Topic 2. 16. Studies of amino acids transformation (deamination, transamination…………. P.58-65
decarboxylation) Investigation of separate amino acid metabolism pathways.
synthesis. Disturbances of amino acid metabolism
Topic 2. 17 Investigation of ammonia detoxication and urea synthesis mechanisms.
P. 66-68
.
.
Questions for Module 2
P.69-71
Task for control module preparing.
P.72-75
3
Topic 2.1. THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
The control of initial knowledge level. Subject and task of biochemistry. The investigation of
protein structure and physical-chemical properties. Quantitative definition of protein by a
biuretic method. The proof of protein nature of enzymes.
Biomedical importance:
Thousands of proteins present in the human body perform functions too numerous to list. These
include serving as carriers of vitamins, oxygen, and carbon dioxide plus structural, kinetic, catalytic,
and signaling roles. It thus is not surprising that dire consequences can arise from mutations either in
genes that encode proteins or in regions of DNA that control gene expression. Consequences equally
adverse can also result in deficiency of cofactors essential for maturation of a protein. Ehlers-Danlos
syndrome illustrates a genetic defect in protein maturation and scurvy a deficiency of a cofactor
essential for protein maturation Gross changes in the secondary-tertiary structure of proteins that occur
independently of changes in primary structure also are responsible form major diseases. Diseases
characterized by significant alterations in secondary-tertiary structure include the prion diseases
Creutzfeldt-Jakob disease, scrapie, and bovine spongiform encephalopathy ("mad cow" disease), each
characterized by pathologic neurological changes that result from deposition of insoluble proteins in
amyloid fibrils composed of continuously hydrogen-bonded β-sheets.
Proteins play the central role during living of cells and forming of the cellular structures. The
analysis of the contents in blood of the certain proteins and enzymes is widely used in the diagnostic
purposes. At diseases of a liver diagnostic inspection by all means includes electrophoretic definition
of the relative contents of albumins and globulins in the plasma of blood. The analysis of the contents
lipoproteins and antibodies is usually used at diagnostics of specific types hypoproteinemia and
immune infringements. Detection even small amounts of fiber serve in urine the important parameter
of disease of kidneys.Now familiarize with the purpose of occupation, think over them, acquire
necessity of their studying.
The purpose:
To develop skills in qualitative and quantitative determination of protein in biological fluids
and interpreting of results of analysis in norm and pathology.To develop the proof of protein nature of
enzymes.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p. 5-22
2. "Biochemistry", Pamela C. Champe at al.2005.p. 1-5, 13-21
3. The «Proteins», Lecture Materials;
Basic level tasks:
1. Which one of the following statements
concerning aspartate is correct?
A. It contains an amino group
B. It is classified as acidic amino acid
in neutral solutions.
C. It is classified as basic amino acid in
neutral solutions.
D. It has isoelectric form at pH 7,0.
E. It migrates to the cathode during
electrophoresis in basic solution.
2. Which amino acid contains an amide
group?
A. Alanin
B. Serine
C. Valine
D. Arginine
E. Glutamine
4
3.
Which amino acid is
hydrophobic?
A. Glutaminic acid.
B. Lysine
C. asparaginic acid
D. Cysteine
E. Methionine
4. Which amino acid can participate in
disulphide bond formation?
A. Valine
B. Tryptophan
C. Cysteine
D. Serine
E. Glutamate.
5. Which amino acid has isoelectric
form in neutral solution?
A. Alanine
B. Lysine
C. Hystidine
D. Glutamic acid.
E. Arginine
The main theoretical questions:
1. Structure, physical and chemical properties, classification of amino acids.
2. Structure of peptides and peptide-bond characteristics.
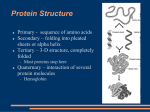
3. Structural organization of protein molecules (primary, secondary, tertiary and quaternary structure)
4. Classification, physical and chemical properties of protein. (Charge, electrophoresis, denaturation)
5. The biological functions and role of proteins.
6. Proof of protein nature of enzymes.
Practice instructions:
Work 1. Quantitative definition of protein by a biuretic method.
The essence of the method:
The method is based on ability of peptide bonds of protein to form in
an alkaline conditions with ions of copper (Cu2+) complex of violet color, which intensity proportional
to the contents of protein in medium.
Sequence of procedure:
1. Put 1 ml of protein solution (blood serum) in tube.
2. Add 1 ml 3% NaOH and 0, 1 ml of Benedict’s reagent.
3. Mix the content of tube good and leave for 15 min.
4. In 15 min. determine density of solution on photoelectrocolorimetre at a green light filter (wave
length 540 nm.)
5. Protein concentration (in gram/l) determine from the standard curve.
6. By plotting density as ordinate versus concentration as abscissa is obtained standard curve. You can
get this plot from technicians and should copy it's into followed axes:
D
C, protein
concentrati
on mmol/l
gr/l
5
Results:
Work 2. Proof of protein nature of enzymes.
The color reactions have been used to indicate the protein presence in solutions and establish amino
acid composition of proteins.
There are 2 types color reaction:
1. Universal (biuret and ninhydrine)
2. Specific reaction for individual amino acids (for example, xantoprotein – for aromatic
amino acids)
1.
2.
3.
4.
1.
2.
3.
4.
A. Biuret reaction: Sequence of procedure:
Put 3 tubes in support.
Pour 1 ml of ovoalbumin into the first tube, 1 ml of pepsin into the second tube and 1 ml of
amylase solution into third tube.
Add 1 ml 3% NaOH and 0,2 ml Benedict solution into each of three tubes.
Mix well and observe the color. The appearance of violet color is a good evidence for the presence
of a protein.
B. Ninhydrine reaction: Αmino acids (free and included in proteins and peptides) give complex
compound of dark blue and blue –violet color with ninhydrine
Sequence of procedure:
Put 3 tubes in support.
Pour 1 ml of ovoalbumin into the first tube, 1 ml of pepsin into the second tube and 1 ml amylase
solution into third tube.
Add 0,5 ml 0,5 ninhydrin solution into each of three tubes.
Boil solutions in the tubes 1-2 min carefully and observe the color.
The appearance of pink-violet color (which can become dark-blue in time) is a good evidence for
the presence of a protein.
C. Xantoprotein reaction.
Aromatic amino acids (free and included in peptides and proteins) form compound of yellow color
with concentrated nitric acid, which changes to orange by alkali addition.
Sequence of procedure:
1. Put 3 tubes in support.
2. Pour 1 ml of ovoalbumin into the first tube, 1 ml of pepsin into the second tube and 1 ml of
amylase solution into third tube.
3. Add 5 drops of concentrated nitric acid into all 3 tubes.
4. Hit solutions carefully and observe the color.
5. Cool the tubes, add 0,5 ml of 20% NaOH and observe the change of color
Yellow color appeases and change to orange after expositing to cold and addition of NaOH if
the solution contains an aromatic amino acid.
6. Put the date into the table.
№ of the Research solution Color of solutions in reaction
tube
Biuret Ninhydrine Xantoprotein
1
ovoalbumin
2
pepsin
3
amylase solution
Conclusions:
6
1. Which of the following reagents can
denature proteins?
A.
Trypsine
B.
NaCl
C.
Concentrated HCl
D.
Glucose
E.
0,01 mol/l NaOH
M. C. Q
6. The primary structure of protein is
stabilized by:
A. Hydrogen bonds
B. Peptide bonds
C.Hydrophobic interactions
D. Ionic interactions
E. Phosphoester bonds
2.Which one of the following statements
concerning lysine is correct?
A.. .It contains an amino group in side chain.
B. It is classified as acidic amino acid in neutral
solutions.
C. It is classified as basic amino acid in neutral
solutions.
D. It has isoelectric form at pH 7,0.
E. It migrates to the anode during
electrophoresis in basic solution.
3. Which one of the following statements
concerning phenylalanine is correct?
A.. It contains an amino group in side chain.
B. It is classified as acidic amino acid in neutral
solutions.
C.It is classified as basic amino acid in neutral
solutions.
D. It is hydrophobic amino acid
5. It migrates to the anode during
electrophoresis in neutral solution.
4. Which amino acid is hydrophobic?
A..
Glutamic aci 4.
B.
Lysine
C.
Aspartic acid
D.
Cysteine
E.
Methionine
5. Denaturation of protein is:
A.. The hydrolysis of peptide bonds
B. The cleavage of protein into small peptides
C.The cleavage of amino acids from N-terminal
end of protein
D. Unfolding and disorganization of protein
structure
E. The cleavage of amino acids from Cterminal end of protein
7. The secondary structure of protein is
stabilized by:
A. Phosphodiester bonds
B. Hydrophobic interactions
C.Covalent polar bonds
D. Hydrogen bonds
E. Ionic interactions
8. Which one of the following statements
concerning primary structure of protein is
correct?
A.. It is unique three-dimensional structur 5.
B. It is stabilized by hydrogen bonds.
C.It is stabilized by hydrophobic interactions
D. It is a sequence of amino acids binding by
peptide bonds
5. It is a sequence of nucleotides.
9. Which one of the following statements
concerning secondary structure of proteinis
correct?
A.. It is unique three-dimensional structur 5.
B. It is stabilized by hydrogen bonds.
C.It is stabilized by hydrophobic interactions
D. It is a sequence of amino acids binding by
peptide bonds
E. It is a sequence of nucleotides.
10. Which one of the following statements
concerning tertiary structure of protein is
correct?
A.. It is unique three-dimensional structur 5.
B. It is stabilized by ester bonds.
C. It is an arrangement of several polypeptide
subunits into multimeric structur 5.
D. It is a sequence of amino acids binding by
peptide bonds
E. It is a sequence of nucleotides.
7
Topic 2.2. THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
The investigation of enzymes structure, physical-chemical properties and conditions of action.
Biomedical importance:
Without enzymes, life as we know it would not be possible. As the biocatalysts that regulate
the rates at which all physiologic processes take place, enzymes occupy central roles in health and
disease. While in health all physiologic processes occur in an ordered, regulated manner and
homeostasis is maintained, homeostasis can be profoundly disturbed in pathologic states. For example,
the severe tissue injury that characterizes liver cirrhosis can profoundly impair the ability of cells to
form the enzymes, which catalyze a key metabolic process such as urea synthesis. The resultant
inability to convert toxic ammonia to nontoxic urea is then followed by ammonia intoxication and
ultimately hepatic coma. A spectrum of rare but frequently debilitating and often fatal genetic diseases
provides additional dramatic examples of the drastic physiologic consequences that can follow
impairment of the activity of but a single enzyme.
Following severe tissue injury (eg, cardiac or lung infarct, crushed limb) or uncontrolled cell growth
(eg, prostatic carcinoma), enzymes that may be unique to specific tissues are released into the blood.
Measurement of these intracellular enzymes in blood serum therefore provides physicians with
invaluable diagnostic and prognostic information.
The purpose: To develop skills in interpreting the properties and functions of enzymes for use this
knowledge in diagnostics, prevention and treatment of diseases related to enzyme disorder.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.39-41,43-44
2. "Biochemistry", Pamela C. Champe at al.2005.p. 53-58
3. Lecture on the theme «Enzymes»,
The main theoretical questions:
1. Definition and chemical nature of enzymes.
1.1. Proof of protein nature of enzymes;
1.2. Common and distinct features in enzymes and non enzymic catalysts.
2. Structural and functional organization of enzymes:
2.1. Simple and compound enzyme proteins. Cofactors, their nature and role in enzyme function;
2.2. Structure of an Active centre, its role in enzyme function;
2.3. Allosteric centre.
3. Properties of enzymes:
3.1 Dependence of enzymatic reaction rate on temperature.
3.2. Dependence of enzymatic reaction rate on рН of medium.
3.3. Specificity of enzyme action, kinds and examples of specificity.
4. Estimation of enzyme activity; methods and units. The essence of laboratory work
5. Classification of enzymes
Practice instructions
Work № 1. «STUDY OF ENZYME THERMOLABILITY»
In this experiment you should study the influence of high temperature on the activity of saliva
amylase. The activity of amylase can be measured by the degree of starch hydrolysis (Non-hydrolyzed
starch with iodine solution gives dark blue color, while starch hydrolysis makes the color fade).
8
1.
2.
3.
4.
5.
6.
7.
8.
Sequence of procedure:
Dilute 1 ml saliva 10 times in measured tube.
Poor 2-3 ml of diluted saliva in the empty tube and boil it for 5-8 minutes on gas.
Cool the tube to room temperature.
Take 3 clean tubes. Pour 10 drops of starch into each of them
Add into tube 1 – 10 drops of non boiled saliva, into tube 2 – 10 drops of boiled saliva and into
tube 3 – 10 drops of distilled water (control on starch
Incubate the tubes for 10 min at 38oC.
Perform the qualitative reaction for starch with iodine/KI solution (1-2 drops into each tube).
Compare the color of solutions and make conclusions.
Scheme of experiment:
N
Starch
Saliva diluted in the Incubation
Color with I2/KI
Enzyme
tube
10 times
solution
activity
1
10 drops Non
10 drops 10 min
boiled
2
10 drops Boiled
10 drops 10 min
3
10 drops dist.water 10 drops 10 min
Conclusions:
Work № 2. «INFLUENCE of рН ON ENZYME ACTIVITY»
In this work you should determine activity optimum for -amylase.
1. Dilute saliva 100 times in mesuare tube/
2. Take 6 test tubes and pour into each of 2 ml of buffer solution with various value of рН:
6,0; 6,4; 6.8; 7,2; 7,6; 8,0.
3. Add 1 ml of 0,5 % starch solution and 1 ml of diluted saliva into each tube
4. Stir contents of the test tubes and incubate them at 38°С for 10 minutes.
5. Add 1 drop of iodine solution in all test tubes and stir the contents well.
6. Observe the color and mark рН at which amylase has the most activity.
Results: pH optimum for -amylase is:
Work № 3. «DEFINITION OF AMYLASE AND SUCRASE SPECIFICITY»
1. Use saliva diluted 10 times for amylase specificity research.
2. To researches sucrase specificity, prepare a yeast extract: grind 1 g of yeast in mortar, add 5 ml of
distillated water, stir well and filter the suspension. Use the filtrate as a source of sucrase.
3. Take 4 tubes and performs the experiment according to the scheme:
N
tube
Enzyme
(1ml)
1
2
3
4
Substrat
e (1 ml)
Incubation
Qualitative reaction on
starch (+ I2/KI
solution)
Amount
Color
1 drop
Qualitative reaction on
glucose (+ Feling
reagent )
Amount
Color
15 min
Amylase
Starch
Amylase
Sucrose 15 min
1 drop
15 min
Sucrase
Starch
1 drop
Sucrase
Sucrose 15 min
1 drop
To carry out Feling reaction heat the test tubes flame after adding of Feling reagent
Conclusions:
9
M.C.Q
1. Which one of the following can proof the
protein nature of enzymes?
A. The association with protein cofactor
B. The ability to increase the velocity of
reactions
C. The ability to electrophoresis
D. The nucleotides composition
E. The availability of the active site
2. Enzymes, which belong to class of
hydrolase’s catalyze:
A. Removal or additional H+ and electrons
B. Cleavage a bonds by addition of water
molecules
C. Cleavage a C-C, C-S, C-N bonds by non
hydrolytic pathway
D. Racemization of the optical or geometrical
isomers
E. Transfer of C-, N- or P-containing groups
between compounds
3. Enzymes, which belong to class of lyases
catalyze:
A. Removal or additional H+ and electrons
B. Cleavage a bonds by addition of water
molecules
C. Cleavage a C-C, C-S, C-N bonds by no
hydrolytic pathway
D. Racemization of the optical or geometrical
isomers
E. Transfer of C-, N- or P-containing groups
between compounds
4. Enzymes, which belong to class of
oxidoreductases catalyze:
A. Removal or additional H+ and electrons
B. Cleavage a bonds by addition of water
molecules
C. Cleavage a C-C, C-S, C-N bonds by non
hydrolytic pathway
D. Racemization of the optical or geometrical
isomers
E. Transfer of C-, N- or P-containing groups
between compounds
5. What is holoenzyme is?
A. Complete structure of conjugated enzymes
B. Prosthetic group
C. Active site
D. Protein part of conjugated enzymes
E. Non-protein organic substance of
conjugated enzymes
6. What is coenzyme?
A. Complete structure of conjugated enzymes
B. Prosthetic group
C. Active site
D. Protein part of conjugated enzymes
E. Non-protein organic substance of
conjugated enzymes
7. What occurs with enzyme at too high pH?
A. Active site is ionized
B. Enzyme has the highest activity
C. Enzyme is denatured
D. Tertiary structure is stabilized
E. Primary structure is destroyed
8. What statement about enzymes state at
100° C is correct?
A. They are denatured
B. They split up to amino acids
C. They reversibly loose activity
D. They have the highest activity
E. All their side chains are ionized
9. Enzymes have a –D shape due to which
type of protein structure?
A. Quaternary structure
B. Primary structure
C. Tertiary structure
D. Secondary structure
E. Domains
10. Enzymes:
A. are composed primarily of polypeptides,
which are polymers of amino acids.
B. can bind prosthetic groups such as metal
ions that participate in enzyme reactions.
C. have defined structures.
D. bind their substrates at active sites.
E. all statements are true.
10
Topic 2.3. THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME: Determination
of enzyme activity. Investigation of enzyme catalysis kinetics. A activators and inhibitors
influence on enzyme activity.
Biomedical importance:
The mechanisms by which cells and intact organisms regulate and coordinate overall metabolism
are of concern to workers in areas of the biomedical sciences as diverse as cancer, heart disease, aging,
mi-crobial physiology, differentiation, metamorphosis, hormone action, and drug action. In all of these
areas, important examples of normal or abnormal regulation of enzymes are to be found. For example,
many cancer cells exhibit abnormalities in the regulation of their enzyme complement (lack of
induction or repression). This illustrates the well-established conclusion that alterations of gene control
are fundamental events in cancer cells. Again, certain oncogenic viruses contain a gene that codes for a
tyrosine-protein kinase. When this kinase is expressed in host cells, it can phosphorylate proteins and
enzymes that are normally not phosphorylated and thus lead to dramatic changes in cell phenotype. A
change of this nature appears to lie at the heart of certain types of viral oncogenic transformation. Drug
action provides another important example involving enzyme regulation. Enzyme induction is one
important biochemical cause of a drug interaction, the situation in which the administration of one
drug results in a significant change in the metabolism of another.
The purpose: To develop skills in utilization of enzyme activity regulation mechanisms to study both
metabolism state and mechanism of action of drugs working as enzyme inhibitors or activators.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.41-42,43 (A), 44-52
2. "Biochemistry", Pamela C. Champe at al.2005.p. 55-56,58-64
3. The «Enzymes» Lecture materials.
The main theoretical questions:
1. The mechanism of enzymatic catalysis
1.1. The idea about energy of activation
1.2. The theory of enzyme-substrate complex
1.3. Fisher hypothesis and Koschland theory
2. The kinetics of the enzymatic reactions.
2.1. The enzyme reaction velocity dependence on substrate concentration
2.2. Michaelis-Menten equation. Michaelis constant
3. Activators and inhibitors of enzymes
3.1. Activation of the enzymes (examples)
3.2. Inhibition: reversible and irreversible, competitive and noncompetitive.
3.3. The useful of the activators and the inhibitors in medical practice.
4. Regulation of enzymes activity.
4.1. Irreversible covalent activation.
4.2. Reversible covalent modification.
4.3. Allosteric regulation. (Feedback inhibition)
4.4. Induction and repression of enzyme synthesis.
11
Practice instructions:
Work № 1. Study of activators and inhibitors action on enzyme activity.
Sequence of operations:
1. Dilute 1 ml of saliva 10 times.
2. Take 3 test tubes.
3. Pour the researched substances into the test tubes according to the scheme of experiment:
Researched
Substances
Dissolved 1:10
enzyme
Starch
Solution Color after
(substrate)
iodine adding
N
1
distilled water
1 ml
1 ml
0.5 ml
2
3
1 % sodium chloride
1 % of copper sulfate
1 ml
1 ml
1 ml
1 ml
0.5 ml
0.5 ml
4. Incubate all test tubes for 10 minutes at the temperature of 25Co.
5. Add 1 drop of iodine solution to each test tube, mix, observe color and determine which substances
act as activators and which as inhibitors. You may add approximately 2 ml of water in order for color
differences to become more visible.
Conclusions:
Work № 2.
Each student takes individual activity sheets from the teacher to study other activators and
inhibitors. Adhere to the scheme mentioned in Work 1.
N
Researched
Substances
1
2
3
4
5
Conclusions:
Enzyme
Saliva amylase
Starch
(substrate)
Incubation
time
Solution
Color after
adding of
iodine
12
M.C.Q.
1. In competitive inhibition which of the
following kinetic effect is true?
A. Decreases Km without affecting Vmax
B. Increases both Km and Vmax,
C. Increases Km without affecting Vmax
D. Decreases both Km and Vmax
E. Increases Vmax without affecting Km.
2. The inhibitor, which binds active site only
most likely (best answer):
A. Is a competitive inhibitor
B. Is a noncompetitive inhibitor
C. Is an allosteric inhibitor
D. Is an irreversible inhibitor
E. Is a homotropic inhibitor
3. Regulation of enzyme activity by excess of
reaction product in the body names:
A. Reversible inhibition
B. Fid-back inhibition
C. Non-competitive inhibition
D. Competitive inhibition
E. Irreversible inhibition
4. "Lock and кеу" model of enzyme action
proposed by Fisher implies that:
A. The active site is complementary in shape to
that of the substrate
B. The active site requires removal of PO3H
group
C. The active site is flexible and adjusts to
substrate
D. Substrates change conformation prior to
active site interaction,
E. None of the above.
5. Irreversible inhibitors of enzyme:
A. Binds to enzyme through covalent bonds
B. It is structurally similar to the substrate
C. Binds to the allosteric site only
D. It is not structurally similar to the substrate
E. Binds to enzyme through noncovalent bonds
6. Enzyme arginase does not affect any
substrates except arginine. Which property
of enzyme shows in this way?
A. Absolute specificity
B. Relative specificity
C. Dependence on pH of medium.
D. High biological activity
E. Thermo ability
7. An allosteric enzyme influences the
enzyme activity by:
A. Competing for the catalytic site with the
substrate
B. Changing the nature of the products formed
C. Changing the conformation of the enzyme
by binding to a site other than catalytic site
D. Changing the specificity of the enzyme for
the substrate
E. All of the above
8. Which one of the following statements is
characteristic of isoenzymes?
A. They do not requires cofactors for action
B. They have the same physical-chemical
properties
C. They have the same amino acid sequence
D. They have genetically determined
differences in primary structure
E. They catalyze different reaction in different
issues
9. Enzymes, which belong to class of ligases
catalyze:
A. Cleavage a bonds by addition of water
molecules
B. Removal or additional H+ and electrons
C. Racemization of the optical or geometrical
isomer
D. Cleavage a C-C, C-S, C-N bonds by non
hydrolytic pathway
E. Synthetic reactions coupled to hydrolysis of
high-energy phosphates (ATP)
10. Which of the following regulatory actions
involves an irreversible covalent
modification of an enzyme?
A. Allosteric modulation
B. Partial proteolysis
C. Non-competitive inhibition
D. Phosphorylation-dephosphorylation the
enzyme
E. Competitive inhibition
13
Topic 2.4. THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
Investigation of the vitamins coenzyme form role in catalytic enzymes activity.
Biomedical importance:
At present we are aware of the importance of vitamins for normal life and activity of an organism.
Their value lies in the participation in enzyme formation. Being a part of enzymes vitamins form a
non-protein part of an enzyme-coenzyme. A compound enzyme can’t function without a coenzyme as
a coenzyme, as a rule, directly contacts a substrate and is a carrier of electrons, atoms or groups of
atoms (aminogroups, methyl groups, etc.), thus participating in catalysis of certain types of metabolic
reactions. Knowledge of vitamin coenzyme function is necessary for the further study of metabolism
of organs and tissues in biochemistry, pharmacology, and clinical and hygienic disciplines.
The objective of study:
To develop skills in substantiating the biological function of vitamins as enzyme structural
components for the further use of this knowledge in the study of metabolism disorders and their
clinical manifestations at the lack (excess) of vitamins in an organism, and also in understanding the
principles of antivitamin application in medical practice.
Literature:
The tutorial book, "Principles of biochemistry", 2005.p.247-252, 256-257.
"Biochemistry", Pamela C. Champe at al.2005. 371, 376-379.
Lecture on the theme «Vitamins»,
The main theoretical questions:
1. Definition and classification of vitamins.
2. Vitamin balance disorders in an organism.
2.1. Primary and secondary avitaminosis and hypovitaminosis
2.2. Hypervitaminosis, 2.3. Antivitamins and provitamins
3. Properties, role in metabolism of B1, B2, B6, PP vitamins Symptoms of vitamins
deficiency. Deceases.
The principle of laboratory works on determination of coenzyme role of vitamins В1,
РР.
Instructions to practice:
Work № 1. STUDY of COENZYME FUNCTION OF VITAMIN В1
The essence of the method: Activity of enzyme pyruvatedecarboxylase is determined by diminution of
substrate, which is defined qualitatively by color reaction.
Sequence of procedures:
1. Put the 2 tubes (control and experimental) in support.
2. Pour the following reagents into both tubes according to this scheme::
The contents of test tubes
control
experimental
1. Apoenzyme of pyruvatedecarboxylase
0,5 ml
0,5 ml
2. Thiamin diphosphate
1,0
3. Buffer solution рН=6,8
2,0
2,0
4. Pyruvate (substrate)
1,0
1,0
Incubate the contents of both tubes for 15 minutes at 25º C.
After the incubation carry out a qualitative test on pyruvate by adding of:
14
5. Dinitrophenilhydrasine
1,0
1,0
In the presence of pyruvic acid the color turns to pink.
Compare colors of the tubes and draw conclusions.
Conclusions:
Work № 2. STUDY of COENZYME FUNCTION OF VITAMIN РР IN LACTATDEHYDROGENASE
REACTION
The essence of the method: Activity of enzyme lactate dehydrogenase is determined by diminution of
substrate, which is defined qualitatively by color reaction.
Sequence of procedures is to be carried out in accordance with the following scheme:
1. Put the 2 tubes (control and experimental) in support.
2. Pour the reagents into both control and experimental tubes:
The contents of test tubes
control (ml) experimental (ml)
1. Apoenzyme of lactate dehydrogenase
0,5
0,5
2. NAD
1,0
3. Buffer solution рН=7,4
1,0
1,0
4. Lactate
1,0
1,0
5. Bidistilled water
1,0
Incubate the contents of both tubes for 15 minutes at 25º C.
Carry out the qualitative reaction on lactate with the Uffelman reactant. To do this follows the
instructions:
a) Take 2 clean tubes and prepare the Uffelman reactant by pouring of 1 ml of 1% phenol solution
into them and adding 0,2 ml of 1% iron chloride ( FeCl3 ). A solution of violet color is obtained
(the so-called phenolate of iron (C6H5O3)Fe.)
b) Add by drops the contents of the control tube to one of the tubes with the Uffelman reactant, and
the contents of the experimental tube to the other. Mix the contents of the tubes well. Compare
colors of the tubes and draw the conclusions. In the presence of lactic acid violet color turns to
green-yellow, which proves the ironic lactate formation.
Conclusions:
Task. 1. Name the vitamin (see the formula below):
2. What coenzyme forms does it have? (Name only):
3. With which enzyme class this cofactor works?
4. Which reactions are catalyzed by these enzymes?
15
M.C.Q.
1. The biological activity of B1 has been
attributed, in part, to its action:
A. Decarboxylation substance for α-keto acids
B. An anti-oxidant
С.. An anti-coagulant
D. An antidote for KCN poisoning
E. A methylation substance
2. Which co-enzyme is involved in oxidative
decarboxylation of pyruvic acid?
A. TPP
B. Pyridoxal phosphate
C. Vit C
D. Biotin
E. Methylcobalamin
3. The disease Pellagra is due to a
deficiency of:
A. Vitamin C
B. Pantothenic acid
C. Vitamin B1
D. Folic acid
E. Vitamin PP
4. Which co-enzyme is involved in oxidativereduction reaction?
A. Thiamine pyrophosphate
B. Pyridoxal phosphate
C. Methylcobalamin
D. NAD
E. Biotin
5. Which of the following statements
regarding vitamins is correct?
A. All water-soluble vitamins act as coenzymes
or coenzyme precursors,
B. All coenzymes contain vitamins or are
vitamins
C. Prostaglandins can be derived from fat
soluble vitamins
D. All vitamins can act as coenzymes
E. Ergosterol is provitamin A.
6. Which of the following vitamins would
most likely become deficient whose staple
diet is maize?
A. Riboflavin
B. Thiamine
C. Niacin
D. Pantothenic acid
E. Ascorbic acid
7. Which of the following characteristics
would be seen in a patient with severe
deficiency of thiamine?
A. Peripheral nervous system damage
symptoms
B. Diarrhea
C. Fragile blood vessels
D. Spongy gums
E. Dermatitis
8. Pyridoxal-phosphate is a co-factor for
which of the following enzymatic reactions?
A. Fixation of CO2
B. Decarboxylation
C. Phosphate group transfer
D. Transmethylation
E. Dehydrogenating
9. Vitamins are essential to the survival of
organisms because vitamins usually function
as:
A. Substrates
B. Nucleic acids
C. Coenzymes
D. Nucleotides
E. .Lipids
10. Which of the following coenzymes
participates in amino group transfer
reactions?
A Coenzyme A
B Thiamin pyrophosphate
C Flavinadenine dinucleotide (FAD)
D. Pyridoxal phosphate
E Biotin
16
Topic 2.5. THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:«Investigation of
the vitamins and vitamin’s coenzymes functions in different biochemical processes».
Biomedical importance:
The structure of ascorbic acid is reminiscent of glucose, from which it is derived in the
majority of mammals. However, in primates, including humans, and a number of other animals, eg,
guinea pigs, some bats, birds, fishes, and invertebrates, the absence of the enzyme L-gulonolactone
oxidase prevents this synthesis. Active vitamin C is Ascorbic acid itself, a donor of reducing
equivalents. When ascorbic acid acts as a donor of reducing equivalents, it is oxidized to
dehydroascorbic acid, which itself can act as a source of the vitamin. Ascorbic acid is a reducing agent
with a hydrogen potential of +0.08 V, making it capable of reducing such compounds as molecular
oxygen, nitrate, and cytochromes a and c. The mechanism of action of ascorbic acid in many of its
activities is far from clear, but the following are some of the better documented processes requiring
ascorbic acid. In many of these processes, ascorbic acid does not participate directly but is required to
maintain a metal cofactor in the reduced state. This includes Cu+ in monooxigenases and Fe2+ in
dioxigenases.
The purpose:
To develop skills in substantiating the biological function of vitamins as
enzyme structural components for the further use of this knowledge in the study of metabolism
disorders and their clinical manifestations at the lack (excess) of vitamins in an organism, and also in
understanding the principles of antivitamin application in medical practice.
Literature:
1. The tutorial book, "Principles of biochemistry", 2005.p.252- 258, 269-270.
2. "Biochemistry", Pamela C. Champe at al.2005.p. 372-375,379.
3. Lecture on a theme «Vitamins»,
The main theoretical questions:
1. Structure, properties, role in metabolism of C, Р (bioflavonoid), В12, folic acid, biotin,
pantothenic acid. Symptoms of their deficiency (avitaminosis). Sources of vitamins.
4. The principle of quantitative definition of vitamins C and Р in food.
The instruction to practice
The essence of the method is based on ability of vitamin C to reduce 2,6-DCPI. When 2,6-DCPI is
reduced its color at once changes from blue (in alkaline medium) to colorless and then to pink (in
acidic medium).
Work 1. THE DETERMINATION OF VITAMIN C IN CABBAGE.
Sequence of procedures is to be carried out in accordance with the following scheme:
1. Pound 1g of cabbage with 2ml 10 % solution hydrochloric acid.
2. Add 8ml of distillate water and filtrate suspension throw a paper filter.
3. Take 2ml of the filtrate into clean flask, add 10 drops of 10 % hydrochloride acid. solution
4. Titrate the content of the flask by 2,6-DCPI till pink painting.
5. Write down the obtained results. (ml of DCPI)
6. Calculate of vitamin C amount by the formula:
17
0.088AD100
X = ------------------------------ =
BC
Where:
0.088 – coefficient
A – result of titration
B – volume of extract for titration (2 ml)
C – total amount of product
D – total volume of extract
Content of vit. C in cabbage is 40-50 mg %.
Work 2. DETERMINATION OF VITAMIN C IN A POTATOES.
Sequence of procedures is to be carried out in accordance with the following scheme:
1. Pound 5g a potato with 20 drops of 10 % HCl
2. Add 20 ml of dist. water and filtrate suspension throw a paper filter
3. Take 5 ml of the obtained mixture and titrate by 2,6-DCPI until pink color appears.
4. Write down the obtained result (ml of DCPI)
5. Calculate of vitamin C amount by the formula:
0.088AD100
X = ------------------------------ =
BC
Where:
0.088 – coefficient
A – result of titration
B – volume of extract for titration (2 ml)
C – total amount of product
D – total volume of extract
Content of vit. C in potatoes is 20 mg %.
Work 3. DEFINITION OF VITAMIN Р IN A TEA.
Sequence of procedures is to be carried out in accordance with the following scheme:
1. Take 10ml of tea extract (100 mg of tea in 50ml of the hot distilled water) into clean flask add
10ml distilled water and 5drops of indigokarmine. A dark blue color appears. Titrate by 0,05 n.
КМпO4 until yellow color appears.
2. Calculate of vitamin P amount by the formula:
0.0032 x А (КМпО4) x V1 x 100
Х (mg)= ---------------------------------------------V2 x Р
Where:
0.0032-coeff. of recalculation,
Aresult of titration,
100 - percentage,
P–
weight of sample,
V1 - Total volume of extract,
V2 - Volume for titration.
Content of vit. P in tea is 30-50 mg %
Conclusions:
=
18
M.C.Q.:
1. The absence of fresh vegetables and fruits
in the diet may result in deficiency of:
A. Riboflavin;
B. Biotin
C. Ascorbic acid
D. Thiamine
E. Cyanocobalamine
2. Hydroxyproline is an essential amino acid
in the collagen structure. Which of the
following vitamins takes part in the
formation of this amino acid by the proline
hydroxylation pathway?
A. B1.
B. D.
C. С
D. B2.
E. В12
3. A patient was diagnosed with
megaloblastic anemia. The lack of
whichsubstance in the human organism can
cause this disease?
A. Copper.
B.
Glycine.
C.
Cobalamine.
D.
Cholecalciferol.
E.
Magnesium
4. A biochemical indication of vitamin B12
deficiency can be obtained by measuring the
urinary excretion of:
A. Pyruvic acid
B. Lactic acid
C. Malic acid
D. Methyl malonic acid
E. Cytric acid
5. Sulphadrugs interfere with bacterial
synthesis of:
A. Vitamin C
B. Lipoate
C. Vitamin B1
D. Tetrahydrofolate (F-H4)
E. Pantothenic acid
6. Pantothenic acid is a constituent of the
coenzyme involved in:
A. Dehydrogenation
B. Acetylation
C. Decarboxylation
D. Reductation
E. Methylation
7. A patient was diagnosed with
dermatitis as a result of prolonged consumption of uncooked eggs. What vita
min deficiency developed in this case?
A. Folic acid.
B. Biotin.
С. Pantothenic acid.
D. Para-amino benzoic acid.
E. Vitamin C.
8. Vitamin B12 is the constituent of the
coenzyme involved in:
A. Methylatoin
B. Acyl group transfer
C. Amination
D. Amino group transfer
E. Carboxylation
9. Rutin is the constituent of the coenzyme
involved in:
A. Oxidation
B. Acetyl group transfer
C. Amination
D. Amino group transfer
E. Methylation
10. Scurvy is due to a deficiency of:
A. Vit. 12
B. Nicotitic acid
C. Pantotenic acid
D. Ascorbic acid
E. Folic acid
19
Substantial module 2. 2 “Basic concepts of metabolism, bioenergetics».
Topic 2.6.
THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
Investigation of oxidative phosphorylation and ATP synthesis. Inhibitors and uncouples of
oxidative phosphorylation”.
To find out the question how the organism extracts energy from foodstuffs, which is necessary
for his functioning, is the basis for understanding processes of normal nutrition and metabolism.
Oxidative phosphorylation allows to aerobic organisms to catch a substantial portion of potential free
energy in the form of ATP during respiration and is so important process that disturbance its normal
course is incompatible with life. In-depth study of this material gives possibility for medical students
to understand the role of oxygen in organism’s vital functions, about using oxygen in treatment
patients with respiratory affection and circulatory disturbances, and also mechanisms of various
biologically active substances (thyroxin, adrenaline), antibiotics, toxic substance.
The purpose: To develop skills in studying the tissue respiration and oxidative phosphorylation
mechanisms, influence on these active conditions different substances. This material will help in future
to make a correct interpretation the diseases proceeding with cell’s bioenergetics disturbances on
clinical hairs.
The literature:
2. The tutorial book "Principles of biochemistry", 2005.p.252- 258, 269-270.
3. "Biochemistry", Pamela C. Champe at al.2005.p. 72 (IV) -82.
4. Lecture on the theme «The bioenergetics and oxidative phosphorylation»
The main theoretical questions:
1.
2.
The types of biological oxidation reactions
Structure and functions of electron transport chain components (dehydrogenase and
cytochromes, cofactors).
3.
Electron transport chain, localization in cells, role of redox potential in components
arrangement.
4.
ATP as main form of energy storage and carries in cells. Types of ATP synthesis reactions:
substrate level phosphorilation (OP), oxidative phosphorilation.
5.
Coupling tissue respiration with ATP synthesis (oxidative phosphorylation). Location of
phosphorylation sites.
6.
Regulation of oxidative phosphorylation, respiratory control.
7.
Possible mechanism of oxidative phosphorylation. Mitchell’s theory.
8.
Energy value of substrates, P/O coefficient.
9.
Inhibitors of respiration chain, their mechanisms of action, influence on organism.
10.
Uncouples of OP. Free non- oxidative phosphorylation, its biological role.
11.
Biological importance of tissue respiration and oxidative phosphorylation.
12.
Principle and progress of work on tissue respiration and oxidative phosphorylation modeling.
13.
Active oxygen forms (AOF): singlet oxygen, hydrogen peroxide, hydroxyl radical, and
superoxide
radicals, reasons of toxicity, biological role.
The practice instruction.
Work №1. “Study of malatedehydrogenase activity.”
The essence of the method: Malate dehydrogenase oxidizes malic acid. By way as final acceptor of
hydrogen atoms is used 2,6-dichlorphenolindophenol (2,6-DCPI ). If the enzyme is active color
begins to abate.
20
Take 2 tubes (control and experimental) and do experiment by the scheme:
Contents of test tubes
Control
1. Phosphate buffer pH=7.4
1.0 ml
2. Solution of malic acid (malate)
0.5
3. Solution of 2,6-DCPI
0.5
4. Suspension of mitochondria
5. Boiled suspension of mitochondria
0.5
Incubate at room temperature during 10 minutes.
Results (coloring):
Experimental
1.0 ml
0.5
0.5
0.5
-
Conclusions:
Work №2. “Study succinate dehydrogenase activity”.
The essence of the method: Succinic dehydrogenase oxidizes succinic acid. By way of final
acceptor of atoms of hydrogen is used 2,6-dichlorphenolindophenol (2,6-DCPI ). If the enzyme is
active color begins to disappear.
Take 2 tubes (control and experimental) and do experiment by the scheme:
Contents of test tubes
Control
1. Phosphate buffer pH=7.4
1.0 ml
2. Solution of succinate
0.5
3. Solution of 2,6-DCPI
0.5
4. Suspension of mitochondria
5. Boiled suspension of mitochondria
0.5
Incubate at room temperature during 10 minutes.
Results (coloring).
Experimental
1.0 ml
0.5
0.5
0.5
-
Conclusions.
Work №3. “Study reactions of oxidative phosphorylation”
Energy releases during the oxidation of substrates in the respiratory chain, one its part is used for
phosphorylation reaction ADP by inorganic phosphate:
ADP + H3PO4 + energy = ATP + H2O
Range of oxidative phosphorylation (energy value of substrates) is determined by decreasing of
inorganic phosphate (coefficient P/O = 1-3 ). To determine the extent of oxidative phosphorylation
are used different substrates (malic acid, succinic acid, ascorbic acid). Quantity of the phosphoric
acid can be fixed in the reaction with molibdate ammonium and reducing solution of the ascorbic
acid by color intensity.
21
Take 4 tubes (1 control and 3 experimental) and do experiment by the scheme:
Contents of test tubes
Control
Experimental
1. Incubatory mixture
1.0
2. Physiological solution
0.5
3. Solution of malic acid
4. Solution of succinic acid
5. Solution of ascorbic acid
6. Suspension of mitochondria
0.5
Incubate at room temperature during 10 minutes, then add:
7. Solution of trichloroacetic acid ( TCA )
1.0
8. Solution of molibdate ammonium
0.5
9. Reducing solution Fiske and Subarroy
0.5
Results (coloring by the four-ball scale):
P/O coefficient
1
2
3
1.0
0.5
0.5
1.0
0.5
0.5
1.0
0.5
0.5
1.0
0.5
0.5
1.0
0.5
0.5
1.0
0.5
0.5
Conclusions:
Work №4. “Study of 2,4-dinitrophenol (2,4-DNP) influence on oxidative phosphorylation”.
The essence of the method: 2,4-DNP is uncoupler of the oxidative phosphorylation. Decreasing of
inorganic phosphate (which is determined by the way described in work №3) in the incubate medium
confirms the oxidative phosphorylation occure.
Take 2 tubes (control and experimental) and do experiment by the scheme:
Contents of test tubes
Control
1. Solution of malic acid
0.5
2. Solution of 2,4-DNP
3. Suspension of mitochondria
0.5
Incubate at room temperature during 10 minutes, then add:
4. Solution of TCA
1.0
5. Solution of molibdate ammonium
0.5
6. Reducing solution
0.5
Experimental
0.5
0.5
0.5
1.0
0.5
0.5
Results (coloring):
Conclusions:
CONTROL QUESTIONS AND TASKS:
1 Upon what avitaminosis and why the tissue respiration is broken?
2. On what the arrangement of components of electron transport chain depends?
3. Write structure of the oxidized and reduced coenzymes NAD + and FAD.
4. Count up, how many moles ATP are formed in a chain of tissue respiration at oxidation of the
following substrates:
а) Hydroxy-butanedioic acid +NAD---- > substrate oxidized + Н2О
б) Succinic acid + FAD---- > substrate oxidized + Н2О
22
M.C.Q
1. In the presence of rotenone:
A, NADH is oxidized by electron transport,
B. FAD H2 is oxidized by electron transport
C. Cytochrome a is reduced by electron
transport
D. Cytochrome c is reduced
E. Cytochrome a3 is reduced.
2. Which of the following statements
describing cytochrome oxidase is true?
A It is inhibited by copper
B. It is also known as cytochrome b
C. It transfers electrons from CoQ to
cytochrome b.
D. It transfers four electrons and four protons
to form H2O molecule
E. It is a single cytochrome.
3. Which of the following vitamins is not a
component of electron transport chain?
A. Nicotinamide
B. Ubiquinone
C. Biotin
D. Riboflavin
E. None of the above
4. Dinitrophenol (DNP) causes which of
the following in biologic oxidation.
A. It increases hydrolysis of ATP
B. It increases synthesis of ATP
C. It prevents electrons transfer
D. It lowers the body heat production
E. All of the above
5. The chemical energy required for the
synthetic processes is provided by:
A. Phosphorylation of ATP
B. Dephosphorylation of ATP
C. Phosphorylation of ADP.
D. Dephosphorylation of ADP.
E. All of the above processes.
6. The enzymes of the electron transport
chain are bound to the surface of the cristae.
The cristae are folded inward in order to:
A. Decrease the intermembrane space;
B. Increase diffusion surface for glycolysis;
C. Separate the products from the substrate in
the Krebs cycle;
D. Form a battery like "cells" for the electron
transport chain;
E. Reduce the distance the FADH2 and NADH
has to travel, and place the products of one
reaction ear the enzymes for the next reaction.
7. Which one is the component of electron
transport chain?
A TPP
B Cytochrom P450
C Cytochrom C
D ATP
E Coenzyme A
8. Choose enzyme, which forms ATP by
oxidative phosphorilation?
A. HADH dehydrogenase
B. Protein kinase
C.Pyruvate kinase
D. ATPase
E. Diphosphate kinase
9. Choose specific site of electron transport
chain blocking by antimycin A?
A. NAD -FMN
B. FMN -CoQ
C. Cyt a+a3 - O2
D. Cyt b - Cyt c
E. CoQ - Cyt b
10. Choose specific site of electron transport
chain blocking by Phenobarbital?
A. NAD -FMN
B. FMN -CoQ
C. Cyt a+a3 - O2
D. Cyt b - Cyt c
E. CoQ - Cyt b
Task .
Isocitrate → NAD →FMN•FeS→?→ cit.b(FeS)·citC1 →cit C → cit аа3 → О2
1. Name missing component of e. t.c. and write its formula
2. Point coupling sites in this e. t.c.
3. Name inhibitors of the site I
4. P/O coefficient for the given substrate = ? How many ATPs are formed in this case?
5. Point vitamin which is the part of NAD
23
Topic 2.7. THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
“Bioenergetics and general pathways of a metabolism. The ivestigation of citric acid sycle
fanctioning".
Biomedical importance:
The major function of the citric acid cycle is to act as the final common pathway for the oxidation of
carbohydrate, lipids, and protein. This is because glucose, fatty acids, and many amino acids are all metabolized
to acetyl-CoA or intermediates of the cycle. It also plays a major role in gluconeogenesis, transamination,
deamination, and lipogenesis. Several of these processes are carried out in many tissues, but the liver is the only
tissue in which all occur to a significant extent A mute testimony to the vital importance of the citric acid cycle
is the fact that very few if any genetic abnormalities of its enzymes have been reported in humans; such
abnormalities are presumably incompatible with normal development.
Understanding of CAC mechanism will help to comprehend many sections of Pathophysiology,
pharmacology, endocrinology, the therapies concerning bio-energetic and its regulation. Energy exchange
disorders underlie many diseases.
The purpose:
To develop skills in interpreting CAC functioning mechanism by the results of reactions
determining its final products formation for estimation of energy supply of an organism in norm and at
metabolic disorders.
Literature:
5. The tutorial book "Principles of biochemistry", 2005.p.85,87; 97-102
6. "Biochemistry", Pamela C. Champe at al.2005.p. 89-91, 103,104,107-114.,
7. Lecture on the theme «The oxidative decarboxylation of pyruvate. CAC»,
The main theoretical questions:
1. Catabolism and anabolism, their interrelation.
2. Specific and general pathways of catabolism.
3. The oxidative decarboxylation of pyruvate. Characteristic of enzyme complex.
4. Specific reactions of CAC, enzymes.
4. The relationship of CAC and electron transport chain.
5. Biological role of CAC.
6. Techniques of CAC functioning estimation by determination of its final
products.
Instructions to practice
Work №1. STUDY OF CAC FUNCTIONING BY ACETYL-CОА CONSUMPTION AND KOA-SH FORMATION
The ssence of the method: The first stage of CAC is the reaction of condensation of Acetyl CоА with oxaloacetate, which is catalyzed by citrate synthase. The formed citric acid is exposed to
transformation in the citric acid cycle, and released CоА-SH may be determined by Folin reactant
(there is a dark blue colouring). If malonic acid blocks CAC Acetyl - CоА is not used and CоА-SH is
not released.
Sequence of procedures:
Take 2 tubes (Control and Experimental) and do experiment according to scheme:
Contents of test tubes
Control
Experimental
1.
Phosphate buffer рН=7,4
2,0 ml
2,0 ml
2.
Sol. acetyl-CоА
0,5
0,5
3..
Sol oxaloacetate
0,5
0,5
4.
1% Sol malonic acid
1,0
-5.
Physiological Sol
1,0
6.
Homogenate
0,5
0,5
Incubate 10 minutes at room temperature, and then add:
Folin’s reactant A
0,5
0,5
8.
Folin’s reactant B
0,5
0,5
24
Results (color of solutions).
Conclusions:
Work 2. STUDY OF CAC FUNCTIONING BY CARBON DIOXIDE FORMATION.
Essence of the method: During Acetyl – CoA oxidation in CAC carbon dioxide formed,
which is attached to calcium hydroxide and may be determined by addition of sulphuric acid. If CO2
formation occurs, gas bubbles are released.
Sequence of procedures:
Take 2 tubes (Control and Experimental) and do experiment according to scheme:
№№
Contents of test tubes
Control
Experimental
___________________________________________________________________________
1.
Phosphate buffer рН=7,4
2,0 ml
2,0 ml
2.
Sol. Acetyl - CоА
0,5
0,5
3.
Sol. oxaloacetate
0,5
0,5
4.
2%Sol. malonic acid
1,0
5.
Physiological sol.
1,0
6.
Sol. Са (OH) 2
1,0
1,0
7.
Homogenate
0,5
0,5
Incubate 10 minutes at room temperature. and than add:
8.
0,1 N sol. sulphuric acid
1,0
1,0
Results (release of carbonic gas).
Conclusions:
Work №3. Study of CAC by formation of hydrogen.
Essence of the method: During Acetyl-CоА oxidation in CAC 8 atoms of hydrogen is
formed. They are further detached with the participation of the corresponding dehydrogenises. 2,6dichlorophenelidophenol (2,6-DNPP) is used as an acceptor of H at this experiment. If the cycle
functions, 2,6-DNPP (dark blue color) is reduced and the solution becomes colorless.
Sequence of procedures:
Take 2 tubes (Control and Experimental) and do experiment according to scheme:
№№
1.
2.
3.
4.
5.
6.
Contents of test tubes
Control
Experimental
Phosphate buffer рН=7,4
2,0 ml
2,0 ml
Sol. Acetyl - CоА
0,5
Sol. Oxaloacetate
0,5
Distilled water
1,0
0,001 n. sol. DNPP
1,0
1,0
Homogenate
1,0
1,0
Incubate 10-15 minutes at room temperature
Results (color of solutions).
Conclusions.
25
M.C.Q.
1. The second stage of aerobic oxidation of
glucose in a cell is the oxidative
decarboxylation of pyruvate. Name the
main products of this process:
A. Acetyl-CоA
B. CO2
C. Citrate
D. Oxaloacetate
E. NADH
2. Which vitamin is required for
isocitratedehydrogenase (in CAC) activity?
A. Biotine
B. Vit. K
C. Folic acid
D. Niacine
E. Riboflavin
3. All of the following compounds are
intermediates of TCA cycle except:
A. Malate
B. Pyruvate
C. Oxalo-acetate
D. Fumarate
E. Succinate
4. Out of 12 moles of ATP formed in citric
acid cycle, one molecule of ATP can be
formed at "substrate level". By which
of the following reactions?
A.Citric acid —>to Isocitric acid
B.Isocitrate —>to oxalosuccinate
C.Malate --- >to oxalo acetate
D.Succinic acid ->to fumarate
E.Succinyl CoA to succinic acid
5. Which of the following statements
regarding T.C.A cycle is true?
A. is an anaerobic process
B. it occurs in cytosol
C. it contains no intermediates for
gluconeogenesis
D. it generates 10 molecules of ATP per cycle.
E. it generates 12 molecules of ATP per cycle.
6. A specific inhibitor for succinate
dehydrogenase is:
A. Arsenite
B. Malonate
C. Citrate
D. Cyanide
E. Fluoride.
7. Most of metabolic pathways are either
anabolic (synthetic) or catabolic
(degradation). Which of the following
pathways is considered as "amphibolic" in
nature?
A. Glycogenesis (Glycogen synthesis)
B. Glycolytic pathway (degradation of glucose)
C. Lipolysis (Lipid degradation)
D. Citric acid cycle
E. Oxidative decarboxylation of pyruvate
8. In which synthetic reaction does CAC
participate?
A. Fatty acids synthesis
B. Formation of glycogen
C. Cholesterol synthesis
D. Formation of phospholipids
E. Formation of glucose from carbon skeletons
of amino acids
9. Which enzyme binds FAD in pyruvate
dehydrogenase complex?
A. Pyruvate decarboxylase
B. Dihydrolipoyl dehydrgenase
C. Dihydrolipoyl transacelylase
D. Pyruvate carboxilase
E. Acetyl-CoA dehydrogenase
10. An allosteric enzyme responsible for
controlling the rate of T.C.A cycle is:
A. Isocitratedehydrogenase
B. Malatedehydrogenase
C. Fumarase
D. Aconitase
E. Succinate thiokinase
Task .
1. Write the reaction of isocitrate conversion to α-ketoglutarate.
2. Name the enzyme, coenzyme, its activators and inhibitors:
3. How many ATP give this substrate?
P/O =
26
Substantial module 2. 3 “Metabolism of carbohydrates, its regulation”.
Topic 2.8
THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME :
Investigation of carbohydrate digestion peculiarities. Glycogen biosynthesis and
degradation.
Conversion of monosaccharides to glucose in the liver.
Biomedical importance:
Carbohydrates are widely distributed in plants and animals, where they fulfill both structural and
metabolic roles. In plants, glucose is synthesized from carbon dioxide and water by photosynthesis and
stored as starch or is converted to the cellulose of the plant framework. Animals can synthesize some
carbohydrate from fat and protein, but the bulk of animal carbohydrate is derived ultimately from
plants.
Knowledge of the structure and properties of the physiologically significant carbohydrates is essential
to understanding their role in the economy of the mammalian organism. The sugar glucose is the most
important carbohydrate. It is as glucose that the bulk of dietary carbohydrate is absorbed into the
bloodstream or into which it is converted in the liver, and it is from glucose that all other carbohydrates
in the body can be formed. Glucose is a major fuel of the tissues of mammals (except ruminants) and a
universal fuel of the fetus. It is converted to other carbohydrates having highly specific functions, eg,
glycogen for storage; ribose in nucleic acids; galactose in lactose of milk, in certain complex lipids,
and in combination with protein in glycoproteins and proteoglycans. Diseases associated with
carbohydrates include diabetes mellitus, galactose, glycogen storage diseases, and milk intolerance.
Glycogen is the major storage form of carbohydrate in animals and corresponds to starch in plants. It
occurs mainly in liver (up to 6%) and muscle, where it rarely exceeds 1%. However, because of its
greater mass, muscle represents some 3—4 times as much glycogen store as liver. Like starch, it is a
branched polymer of a-D-glucose. The function of muscle glycogen is to act as a readily available
source of hexose’s units for glycolysis within the muscle itself. Liver glycogen is largely concerned
with storage and export of hexose’s units for maintenance of the blood glucose, particularly between
meals. After 12-18 hours of fasting, the liver becomes almost totally depleted of glycogen, whereas
muscle glycogen is only depleted significantly alter prolonged vigorous exercise. Glycogen storage
diseases are a group of inherited disorders characterized by deficient mobilization of glycogen or
deposition of abnormal forms of glycogen, leading to muscular weakness or even death.
The purpose:
On the basis of structural and functional features of carbohydrates knowledge to be able to
interpret the mechanism of their digestion, mechanisms of deposition and disintegration glycogen, a
pathology of these processes for subsequent use in clinical practice.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.111-125,127-134.
2. "Biochemistry", Pamela C. Champe at al.2005.p. 83-88,123-129,135-140.
3. Lecture on the theme «Carbohydrates »
The main theoretical questions:
1. Carbohydrates structure, properties and functions (the characteristic of dietary
carbohydrates);
1.1. Monosaccharides: glucose, galactose, fructose, ribose, deoxyribose.
1.2. Disaccharides: maltose, sucrose, lactose.
1.3. Homopolysaccharides: starch, glycogen, cellulose. (composition, types of
linkages)
2. Digestion and absorption of carbohydrates: enzymes, products.
27
2.1. Digestion in the mouth cavity;
2.2. Digestion in the small intestine;
2.3. Absorption of monosaccharides.
2.4. Abnormal degradation of disaccharides: lactose intolerance.
3. Interconversion of monosaccharides in the liver. Disturbances of monosaccharides
metabolism: galactosemia, fructosuria.
4. Glycogen metabolism:
4.1. The basic steps in glycogen synthesis. Regulation.
4.2. Degradation of glycogen in the liver (for glucose); regulation.
4.3. Interrelation of glycogen synthesis and degradation.
4.4. Glycogen storage diseases. (Von Gierke’s diseases).
5. A principle of the method and a course of definition of activity salivary amylase
by Wolgelmgutt. Clinical value.
The instruction to practice
Work №1. THE DETERMINATION OF SALIVERY AMYLASE ACTIVITY.
The essence of method: the method is based on determination of the least amount of amylase
(when dilution of a saliva in maximum) which completely splitting all added starch. Amylase activity
of saliva is determined by amount of 1, 0 % of a solution of starch (in milliliters) which is split by 1ml
undiluted saliva under 38oC in 30 minutes. Amylase activity of saliva is equal norm 160-320. This
method is widely used for definition amylase activity in urine.
Sequence of procedure.
1.
Place 10 tubes into a support.
2. Pour 1 ml of distilled water into each of them.
3. In a separate tube dilute the saliva in 10 times.
4. Pour 1 ml of diluted saliva into 1st tube and mix well. Transfer 1 ml of solution from 1st tube into
second one.
5. Repeat this procedure till tenth tube.
6. Pour out and dump 1 ml solution from the last tube.
7. Add 1 ml of distilled water and 2 ml 0.1% starch solution into each tube, mix well and incubate 30
min at 38oC.
8. Add 1 drop of 0.1% iodine solution to each tube and mix.
9. Tube contents become yellow, pink or violet upon receiving with iodine
10. Mark the last yellow-colored tube (A) in which starch hydrolysis accomplished completely and
make the calculations. Fill the table:
1
2
Test tubes
1:20 1:40
Dilution of a
1:10240
saliva
Coloring
with
iodine
solution
3
4
1:80 1:160
5
6
1:320
7
1:640
11. Use the following formula to calculate amylase activity of saliva:
2ml x 1
X = --------------- =
A
8
1:1280
9
1:2560
10
1:5120
28
Where:
2 – amount of 0.1% starch solution,
1 – amount of saliva diluted 1 : 10
A – amount of saliva in the marked tube.
For example, yellow color appears first of all in 4-th tube, where saliva is diluted 1:160.
2 ml of 0,1% starch was degraded by 1/160 of ml of saliva, than X ml of 0,1% starch solution is
degraded by 1 ml undiluted saliva,
2ml x 1 x160
X = --------------- ---------= 320
1
Thus amylase activity (A 38oC/30) equals 320 under 38oC after 30 min incubation.
Conclusions:
Task:
Write the reaction (by formulas):
1. X + UDP-glucose - - Y + glucose-1- P
Hexose 1- phosphate uridyltranseferase
2. Fructose + X -------------------- Y + ADP
hexokinase
3. Write the reactions of glucose phosphorylation: Name enzyme which catalyse reaction
a) in the liver; b) in other tissues. Describe difference in enzymes.
29
M.C.Q.
1. Which bonds in carbohydrate molecules
does salivery amilase cleave?
A. α-(1-4) between glucose in maltodextrins
B. α -(1,2) beta between glucose and fructose in
sucrose
C. α -(1-4) between glucose residues in starch
D. β-(1-4) between galactose and glucose in
lactose
E. α -(1-6) between glucose residues in starch
2. Diarrhea, which starts in a child after
milk intake is associated with absence of the
enzyme:
A. Galactokinase
B. β-fructophyranosidase
C. Maltase D. Saccharase
E. Gexokinase
3. What is impaired in glycogen synthase
deficiency?
A. Glucosuria
B. Fructosemia
C. Glycogenosis
D. Aglicogenesis
E. Galactosemia
4. Glucose may be transformed into glucose6-phosphate due to the action of various
enzymes in human tissues. Point out the liver
enzyme for this conversion:
A. Glucokinase
B. Hexokinase
C. Fructokinase
D. Galactokinase
E. Phosphofructokinase
5. The role of the patient's salivary enzymes
in the intestine was examined. Your opinion,
what will happen to them?
A. are digested into the monomers and
absorbed
B. inhibit the intestinal secretion
C. continue to digest carbohydrates
D. are excreted
E. activate the intestinal secretion
6. Mental retardation, lens opacity in the
newborn is associated with…
A. Galactosemia
B. diabetes mellitus
C. Albinism
D. Ketonemia
E. Fructosemia
7. A newborn had dyspepsia, vomiting after
milk feeding. These symptoms disappeared
after feeding with glucose solution.
Insufficient activity of what enzyme taking
part in digestion of carbohydrates leads to
such disorders?
A. Lactas
B. Amylase
C. Maltase
D. Saccharase
E. Isomaltase
8. Von Gierke's disease is characterized by
a deficiency of which enzyme?
A. Glucokinase
B. Glucose-6-phosphatase
C. α —1-6 glucosidase
D. glycogensynthase
E. de-branching enzyme
9. An essential for converting glucose to
glycogen in Liver is:
A. Lactic acid
B. GTP
C. CTP
D. UTP
E. Pyruvic acid.
10. The fructokinase reaction in fructose
metabolism produces which of the
following intermediates?
a. Fructose-6-P
b. fructose-1-p
c. fructose-1, 6-bi-p
d. glyceraldehyde-3-p
e. Pyruvate
30
Topic 2. 9
THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
Anaerobic oxidation of carbohydrates - Glycolysis. Synthesis of glucose –
gluconeogenesis.
Biomedical importance:
Most tissues have at least a minimal requirement for glucose. In some cases, e.g., brain, the
requirement is substantial, while in others, e. g., erythrocytes, it is nearly total. Glycolysis is the major
pathway for the utilization of glucose and is found in the cytosol of all cells. It is a unique pathway,
since it can utilize oxygen if available (aerobic), or it can function in the total absence of oxygen
(anaerobic). However, to oxidize glucose beyond the pyruvate/lactate end stage of glycolysis requires
not only molecular oxygen but also mitochondrial enzyme systems such as the pyruvate
dehydrogenase complex, the citric acid cycle, and the respiratory chain.
Glycolysis is not only the principal route for glucose metabolism leading to the production of
acetyl-CoA and oxidation in the citric acid cycle, but it also provides the main pathway for the
metabolism of fructose and galactose derived from the diet. Of crucial biomedical significance is the
ability of glycolysis to provide ATP in the absence of oxygen, because this allows skeletal muscle to
perform at very high levels when aerobic oxidation becomes insufficient and it allows tissues with
significant Glycolytic ability to survive anoxic episodes. Conversely, heart muscle, which is adapted
for aerobic performance, has relatively poor Glycolytic ability and poor survival under conditions of
ischemia. A small number of diseases occur in which enzymes of glycolysis (e. g., pyruvate kinase) are
deficient in activity; these conditions are mainly manifested as hemolytic anemias or, if they occur in
skeletal muscle (e. g., phosphofructokinase), as fatigue. In fast-growing cancer cells, glycolysis
proceeds at a much higher rate than is required by the citric acid cycle. Thus, more pyruvate is
produced than can be metabolized. This in turn results in excessive production of lactate, which favors
a relatively acid local environment in the tumor, a situation that may have implications for certain
types of cancer therapy. Lactacidosis results from several causes, including pyruvate dehydrogenase
deficiency.
The purpose: To develop skills in interpreting the mechanism of anaerobic oxidation of carbohydrates
in an organism by the final products of this process for estimation of energy supply in norm and
pathology.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.79-85, 87, 91-96.
2. "Biochemistry", Pamela C. Champe at al.2005.p. 94 (III), 95-103 (V,VI),115-122.
3. Lecture on the theme «Carbohydrates»
The main theoretical questions:
1. Definition of glycolysis and glycogenolysis as the processes of anaerobic formation
of energy from carbohydrates.
2. Specific reactions of glycolysis, enzymes.
3. Energy balance and biological function of anaerobic glycolysis.
4. Degradation of glycogen (glycogenolysis).
5. Degradation of other monosaccharides (fructose and galactose).
6. Alcoholic fermentation.
7. Gluconeogenesis: mechanism, indirect pathway, non carbohydrate sources for this
process.
8. Hypo energy states connected with hypoxia. Fate of resulting lactate.
9. The Cory cycle.
10.Interrelation of glycogen synthesis and degradation.
31
11.Techniques of glycogenolysis functioning estimation by its final products
definition.
Practice instructions:
Work №1. Modeling of glycogenolysis reactions.
Essence of the method: The method is based on the formation of lactate and the loss of inorganic
phosphate upon glycolysis after incubation of tissue homogenate with glycogen.
Sequence of Procedures:
1. Pour 5 ml of muscular homogenate into each of two test tubes (control and experimental).
2. Add 5 ml of the phosphate buffer with pH 7.4 to both of them.
3. Add 5 ml of 1% glycogen solution to the control tube, and 5 ml of physiological solution to the
experimental tube.
4. Incubate the contents of both test tubes for 15 min at 37˚ C.
5. After the incubation perform the test on lactate and inorganic phosphate in both control and
experimental tubes. (First, separate contents of both tubes in two parts). Make conclusions.
Determination of lactate.
Sequence of procedures:
1. Prepare Uffelman reagent in 2 clean tubes as follows: pour 1 ml of 1% phenol solution and
add 0.2 ml of 1% chloride iron (FeCL3). Iron phenolate of violet color is formed.
2. To the reagent obtained add by drops (20-30 drops) the studied solutions (control into the 1-st
and experimental into the second) and mix well.
3. In the presence of lactic acid the color becomes green-yellow as a result of lactic-acid iron
formation.
4. Compare colors of the tubes and draw conclusions.
Determination of inorganic phosphate.
Sequence of procedures:
1. Pour 1 ml of molybdenum-acid ammonium and 1 ml of ascorbic acid into both tubes with the
studied solutions.
2. The contents of the tube acquire violet color if they contain inorganic phosphate. Intensity of
the color is proportional to the inorganic phosphate amount.
3. Compare colors of the tubes and draw conclusions.
Conclusions:
Essay questions.
1. Write the 3 -d irreversible reaction in the glycolysis. Name enzyme, its activators and
inhibitors
2. Write the reaction of the gluconeogenesis, catalyzed by pyruvatecarboxilase. Name coenzyme.
32
M.C.Q.
1. The gluconeogenesis is activated in the liver
after intensive physical trainings of organism.
Point the substance that is utilized in
gluconeogenesis first of all in this case:
A. Lactate
B. Pyruvate
C. Glucose
D. Glutamate
E. Alanine
2. In conversion of Lactic acid to glucose, three
reactions of glycolytic pathway are
circumvented. Which of the following enzymes
do not participate in this process?
1. Pyruvate carboxylase
2. Phospho-enolpyruvatecarboxykinase
3. Pyruvate kinase
4. Glucose-6-phosphatase
5. Fructose-1, 6-biphosphatase
3. What are the enzymes that catalyze the three
regulated steps of glycolysis?
A. glyceraldehyde-3-phosphate dehydrogenase,
phosphofructokinase, pyruvate kinase
B. hexokinase, phosphofructokinase, pyruvate
kinase
C. fructose-1,6-bisphosphatase, hexokinase,
phosphofructokinase
D. hexokinase, glyceraldehyde-3-phosphate
dehydrogenase, phosphofructokinase
E. phosphoglycerate kinase, hexokinase,
phosphofructokinase
4. The reciprocal regulation of glycogen
synthesis and breakdown is primarily controlled
by which of the following?
A. hormonal regulation of adenylate cyclase and
biological amplification
B. glucagon mediated inhibition of phosphorylase
kinase and subsequent activation of glycogen
synthase
C. cAMP mediated regulation of kinases that lead
to the activation of glycogen phosphorylase and
glycogen synthase
D. A and C
E. All of the above
5. Which of the following best describes
phosphoenolpyruvate carboxykinase (PEPCK)?
A. catalyzes the conversion of oxaloacetate to
phosphoenolpyruvate
B. is located in the cytosol
C. is negatively regulated by glucagon
D. A and B
E. all of the above
6. When glucose is oxidized to two lactate
molecules, the total number of ATP molecules
that can be produced is:
A. 4 ATP
B. 8 ATP
C. 2 ATP
D. 6 ATP
E. 38 ATP
7. Buffer capacity of blood was decreased in the
worker due to exhausting muscular work. Entry
of what acid substance to the blood can this state
be explained?
A. Lactate
B. α-ketoglutarate
C. Pyruvate
D. 1,3-bisphosphoglycerate
E. 3-phosphoglycerate
8. A 7-year-old girl has signs of anemia.
Laboratory analysis found deficiency of
pyruvatekinase in erythrocytes. Impairment of
what process plays the main role in development
of anemia in the girl?
A. Anaerobic glycolysis
B. Desamination of aminoacids
C. tissue respiration
D. Oxidative phoshorylation
E. Decomposition of peroxides
9. The patient is revealed to have hypoxia. Name
the main cellular mechanism of adaptation to
hypoxia.
A. anaerobic glycolysis
B. Krebs cycle
C. gluconeogenesis
D. pentosophosphate way
E. oxidative decarboxilation of PTA
10. Which of the following is a substrate for
aldolase activity in glycolytic pathway?
A. Glyceraldehydr-3-p
B. Glucose-6-p
C. Fructose-6-p
D. l-3-diphospho-glycerate
E. Fructose-1, 6-bi-p
33
Topic 2.10
THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
Investigation of aerobic oxidation of glucose. Pentose phosphate pathway for glucose conversion
Biomedical importance:
Deficiencies of certain enzymes of the pentose phosphate pathway are major causes of
hemolysis of red blood cells, resulting in one type of hemolytic anemia. The principal enzyme
involved is glucose-6-phosphate dehydrogenase. More than 100 million people in the world may have
genetically determined low levels of this enzyme.
The major metabolic routes for the utilization of glucose are glycolysis and the pentose
phosphate pathway. Of minor quantitative importance but of major significance for the excretion of
metabolites and foreign chemicals (xenobiotics) as glucuronides is the elaboration of glucuronic acid
from glucose via the uronic acid pathway. A deficiency in the pathway leads to the condition of
essential pentosuria. The total absence of one particular enzyme of the pathway in all primates
accounts for the fact that ascorbic acid (vitamin C) is required in the diet of humans but not in that of
most other mammals. Deficiencies in the enzymes of fructose and galactose metabolism lead to
metabolic diseases such as essential fructosuria and the galactosemias. Fructose has been used for
parenteral nutrition, but at high concentration it can cause depletion of adenine nucleotides in liver and
hepatic necrosis.
The purpose: To develop skills in the interpreting of mechanism carbohydrates oxidation in anaerobic
and aerobic conditions in the organism for estimation of the supply of energy in norm and pathological
changes.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.85-88, 97-102 (recall without
reactions),103-105, 107-108 (V A),110.
2. "Biochemistry", Pamela C. Champe at al.2005.p.103,107-114 (recall without reactions),
110,143-145,149-150(V A),
3. Lecture on the theme «Carbohydrates»
The main theoretical questions:
1. Two pathways of utilization of pyruvate of the major intermediate product of
carbohydrate metabolism under anaerobic and aerobic conditions.
2. Aerobic oxidation of carbohydrates.
2.1. Scheme of glucose degradation to CO2
and H20
2.2. Calculation of power balance of aerobic oxidation of one molecule of glucose.
2.3. Biomedical importance of this process.
2.4. Pasteur’s and Crabtree effects.
3. The pentose phosphate pathway of glucose oxidation.
3.1. Reactions of oxidative phase (1 stage)
3.2. Scheme of non-oxidation phase (2 stage)
3.3 The overall reaction of this pathway.
3.4. The biological importance of the pentose phosphate pathway
3.5 Deficiency of glucose-6 phosphatedehydrogenase.
4. Quantitative definition of pyruvate in urine.
34
Practice instructions
The essence of the method:
Pyruvic acid react with 2,4 dinitrophenilhydruzine in alkaline medium to form 2,4
dinitrophenilhydruzone an yellow-orange color.
Intensity of color is proportional on concentration of pyruvate.
Sequence of Procedures:
1. Pour in test tube 1 ml urine, and 1 ml 2,5 % alcohol solution KOH,
2. Mix 1 minute, then add 0,5 ml of 0,1% of a solution 2,4 dinitrophenilhydruzine,
3. Again mix and leave to stand for 15 minutes at room temperature.
4. After that measure the optical density on the photoelektrocolorimeter.
5. Pyruvate concentration is derived from the standard curve. (mg/day)
D
C, mg/day
Results:
Conclusions:
35
M.C.Q.
1. Which one of the following
metabolites is directly produced in the
PPP?
A. Ribose-5-phosphate
B. Fructose-1-phosphate
C. Deoxyribose-5-phosphate
D. Lactate
E. NADP
2. The "Primaquin sensitivity type" of
hemolytic anemia has been found to
be related to reduce R.B. Cells
activity of which enzyme?
A. Pyruvate kinase deficiency
B. Glucose-6-phosphatase deficiency
C. Glucose-6-P-dehydrogenase deficiency
D. Hexokinase deficiency
E. Phosphogluconate\dehydrogenase
deficiency.
3.
Dehydrogenases involved in-HMP
shunt are specific for:
A. NADP +
B. NAD
C. FAD
D. FMN
E. none of the above
4.
Which of the following enzyme is not
involved in HMP shunt?
A. glyceraldehyde-3-p-dehydrogenase
B. glucose-6-P-dehydrogenase
C. transketolase
D. phosphogluconatedehydrogenase
E. transaldolase
5. Which one of the following metabolites is
directly produced in the PPP?
A. Ribose-5-phosphate
B. Fructose-1-phosphate
C. Deoxyribose-5-phosphate
D. Lactate
E. NADP
6. An alcoholic patient is often observed to
have hypovitaminosis B1 due to
malnutrition. Symphtoms of
hypovitaminosis B1 are disorders of the
nervous system, psychoses, loss of memory.
Why are nervous tissues especially sensitive
to deficiency of vitamin B1?
A. aerobic decomposition of glucose is
impaired
B. intensity of glycolysis increases
C. lipolysis of the fatty tissues is enhanced
D. oxidation of the fatty acids is impaired
E. intensity of glycolysis decreases
7. A 42-year-old man was administered
prymahin in order to prevent the distant
results of quartan malaria. 3 days since the
beginning of the treatment with therapeutic
dosage of this medicine the patient has
developed pain in the cardiac and abdominal
regions, dyspepsia and general cyanosis.
What could cause such side effects?
A. Accumulation of the medication
B. Delay preparation excretion with urine
C. Reduced activity of microsomal liver
enzymes
D. Potential activity with other preparations
E. Genetic insufficiency of glucose 6phosphate dehydrogenase
8. The second stage of aerobic oxidation of
glucose in a cell is the oxidative
decarboxylation of pyruvate. Name the main
product of this process:
A. Acetyl-CоA
B. Glutamate
C. Citrate
D. Oxaloacetate
E. Succinyl-CоА
9. Which one of the following is NOT
characteristic of the pentose monophosphate
pathway?
A. It produces ribulose-5-phosphate
B. It requires NADP
C. NADPH is a inhibitor of glucoso-6phosphate dehydrogenase
D. TPP is a coenzyme of transketolase
E. It include of one carbon groups transfer
reaction
10. Match the following:
A. Glucose-6-p-dehydrogenase
B. Phosphopentose epimerase
C. Transketolase
D. Hexokinase
E. Phosphopentoseisomerase.
A.
B.
C.
D.
E.
Generates NADPH
Requires TPP as coenzyme
Converts ribulose-5-phoaphate to xylulose-5converts ribulose-5-p to ribose-5-p
activates glucose
36
Substantial module 2. 4:
Topic 2.11
"Metabolism of lipids, its regulation".
THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME :
Structure and functions of cellular membranes.
Biomedical importance:
Studying of biological membranes is necessary for understanding of such processes, as interaction
of cells at formation of tissues, a feed of tissues, phagocytosis, secretions, and transformations of
energy in a cell. The structure and function of membranes are broken at a number of diseases and
quite often make essential stage of disease pathogenesis. Membranes are the most widespread
subcellular structures. The basic membranes structures of a cells are plasmatic membranes,
microsomal membranes, Golgi apparatus, mitochondrion and nuclear membranes. Each of them has
the structural features and carries out specific functions, but all of them are constructed on common
type.
The purpose:
To develop skills in interpreting of physical and chemical properties and functions of
cellular membranes on the basis of their chemical composition.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p. 147-149,157( Fig),168.
2."Biochemistry", Pamela C. Champe at al.2005.p.199-200, 206-207,217-218,179-180,
3. The "Membranes" Lecture Materials;
4. Appendix, topic 2.4.
The main theoretical questions:
1. Classification of lipids.
2. Structure, properties and
functions of lipids:
• With formulas:
a) fatty acids: Palmitic, stearic, oleic, linoleic.( For example, palmitic acid C15H31COOH)
b) triacylglycerols,
c) Phosphpglycerides : Phosphatidic acid, Phosphatidylethanolamine,
Phosphatidylserine,
Phosphatidlycholine,
d) Cholesterol
• Composition only:
a) Sphingomielin;
b) Glycosphingolipids (neutral and acidic);
3. Membrane proteins.
4. Composition of the cellular membranes (lipid bilayers and proteins)
5. Functions of cellular membranes
6. Transport mechanisms across membranes.
7. Peroxide oxidation of membrane lipids. Maintenance of the
membranes integrity.
Task:
1. Write a formula of phosphatidylcholine (R1- palmitic acid, R2 oleic).
2. Name products of complete hydrolysis of cerebrosides
3. Name products of complete hydrolysis of Sphingomielin.
4. Write a formula of phosphatidylethanolamin (R1- C-14, R2 oleic, C-18).
37
5. Oxygen molecules (O2) move from the lungs into the bloodstream. Movement across the cell
membrane in this diagram is called:
M.C.Q.
1. Which of the following forms of
cell transport requires the input of
energy?
A. Movement of a solute down its
concentrated gradient
B. Diffusion
C. Active transport
D. Osmosis
E. Facilitated diffusion
phospholipids from one side of the
membrane to the other.
2. What is the movement of water
through a selectively permeable
membrane called?
A. Equilibrium
B. Diffusion
C. Active transport
D. Facilitated diffusion
E. Osmosis
6. What is another name for the
transport proteins used in active
transport?
A. Pumps
B. Enzymes
C. Receptors
D. Pores
E. Hormone
3. __________ help(s) to transfer
substances through cell membrane.
A. Osmosis
B. Cholesterol
C. Carbohydrates
D. Proteins
E. The lipid bilayer
7. Glycolipids, which are abundant
in the brain and the myelin sheaths
of nerves, contain:
A. sphingosine + a fatty acids +
phosphate + choline
B. sphingosine + three fatty acids
C. glycerol + two fatty acids +
phosphate + choline
D. glycerol + two fatty acids + a
monosaccharide
E. gycerol + three fatty acids
4. Which statement is true about the
plasmatic membrane?
A. The model can be likened to a
sandwich where phospholipids are like
the bread and proteins are like the
filling.
B. Plasma proteins are responsible for
membrane functions
C. The proteins make up the matrix of
the membrane.
D. The fluid nature of the membrane is
regulated by flip-flopping of the
5. A fatty acid is a compound made
of a chain of carbon atoms plus:
A. an acid group at one end
B. amino group at both ends
C. an amino group
D. acid group at both ends
8. A phospholipid molecule has a
head and two tails. The tails are
found:
A. Where the environment is
hydrophilic
B. In the interior of the membrane
C. Spanning the membrane
D. At the surface of the membrane
E. In the nucleus
38
9. The sodium pump:
A. Is a DNA
B. Is an integral (transmembrane)
protein
C. Produces ATP
D. Is a glycolipid
E. Requires no energy to move ions
10. Most of the cell membrane is
made up of fats that are arranged in
a _______.
A. Lipid bilayer
B. Cholesterol layer
C. Protein layer
D. DNA layer
E. Carbohydrate layer
Appendix.
Lipids in Biological Membranes.
Biological membranes contain an interesting array of molecules. These include glycerophospholipids,
cholesterol ( formulas see in the book), sphingolipids, , proteins, carbohydrates, and some molecules
which are conjugates containing molecules from two or more of these groups .The primary structural
requirement for a molecule to reside in a lipid bilayer is an amphiphilic nature (i.e., part polar, part
nonpolar). Molecules are oriented within the lipid bilayer so that their nonpolar portion is inserted into
(and sometimes through) the nonpolar core of the bilayer. The polar portion associates with the polar
outsides of the bilayer. Membrane proteins have their polypeptide chains folded so that the nonpolar
regions associate with each other in a cluster. This nonpolar unit then sticks into the nonpolar part of
the bilayer with the remaining polar parts sticking out. Some protein molecules, such as
bacteriorhodopsin, actually extend though both sides of the lipid bilayer. The presence of bulky
nonpolar molecules, such as cholesterol, disrupts the regularity of a lipid bilayer.
Sphingolipids
Spingolipids are a class of lipids found in membranes, particularly of nervous tissue. Sphingosine is
an alcohol back bone and is derived ultimately from palmitoyl-CoA and serine. Ceramides are
sphingolipids containing two acyl-moieties. The more complex, carbohydrate-containing
sphingolipids, such as the cerebrosides and the gangliosides, are derived from the ceramides.
Sphingolipids containing a carbohydrate are called glycosphingolipids.
A.
Sphingomielins:
Contain: Sphingosine + Fatty acid +phosphocholine (See formula below)
ceramide
B. Gglycosphingolipids ( are divided in two group_)
1. Cerebrosides (neutral)
Cerebrosides are sphingolipids made by attaching a sugar to a ceramide . Cerebrosides are
prominent components of membranes, particularly in the brain. Cerebrosides are distinguished from
gangliosides in that the latter contain at least one sialic acid within them. The most common
cerebrosides include galactosylceramide, glucosylceramide, and sulfatides . Sulfatides are made by
transferring a sulfate group to a galactosylceramide).
39
Composition: ceramide (Sphingosine + Fatty acid) + Sugar (Galactose ore glucose)
Hydrophobic tail
Hydrophylic head
2. Gangliosides ( acidic)
Gangliosides are glycosphingolipids that contain the structure of a ceramide plus carbohydrate
moieties. Sialic acid is a part of the carbohydrate component. Gangliosides are found primarily in the
ganglion cells of the central nervous system, particularly at the nerve endings. They are also receptors
for specific agents, such as cholera toxin and influenza virus.The influenza virus then cleaves the
gangliosides as part of its entry process into cells. Some gangliosides promote the growth of neural
tissue in cell culture, suggesting they might be used to promote regeneration of nerve tissue after spinal
cord injury.
Composition: ceramide (Sphingosine + Fatty acid) + Sugar (Galactose ore glucose)+ Nacetylgalactoseamine ore N-acetylneuraminic acid (Sialic acid)
Acid charge
Membrane Proteins
Membrane proteins can be distinguished from other globular proteins by the high proportion of
hydrophobic amino acids they contain.The nonpolar amino acids are typically arranged in parts of the
protein that are embedded in the nonpolar part of the lipid bilayer. These segments are often -helical
and can sometimes be identified by plotting the hydrophobicity of the polypeptide sequence.
Membrane proteins are of two general types-integral and peripheral. Integral membrane proteins
project through both sides of the lipid bilayer whereas peripheral membrane proteins project through
only one side of the lipid bilayer .Some membrane proteins are also covalently linked to either
carbohydrate or lipid moieties. As can be seen in the lipid, protein and carbohydrate composition of
membranes can vary considerably.
Passive Transport Mechanisms
Passive transport mechanisms use no external energy source to bring about diffusion of a substance
across a membrane. The most common passive transport systems are diffusion and facilitated
transport.Diffusion - Diffusion happens, and there is very little cells can do about it. lists permeability
coefficients for selected ions and molecules through membranes. Because the driving force for
diffusion is a concentration gradient, active transport pumps, such as the sodium-potassium pump,
create gradients of these two ions that are continually (though slowly) degraded by diffusion. Note in
that sodium and potassium ions do not have facilitated transport systems, so their permeability
constants are very low. Facilitated transport (or facilitated diffusion) - Includes pore-facilitated
transport and carrier-facilitated transport systems. One notable feature of facilitated transport
systems is that even though the driving force is also the process of diffusion and the end result is the
same as diffusion, facilitated transport systems speed up diffusion by a factor of up to 10,000,000fold.
Pore-facilitated transport - Band 3 protein of the erythrocyte is an example of a pore-facilitated
transport system It contains a highly specific channel to transport bicarbonate ions out of cells as it
transports chloride ions in. Note that the net charge difference in the transport is zero, so there is no
electrical polarization of the membrane. Another kind of pore is gramicidin A, which is a simple 15residue polypeptide that allows potassium and sodium ions to pass through it Still another porefacilitated system is that of the glucose transport protein of erythrocytes which strongly favors
transport of D-glucose over other sugars.
The different types of diffusion (facilitated versus simple diffusion) can be distinguished because
facilitated systems have only a fixed number of sites through which transport occurs, but simple
diffusion occurs across the entire surface of the cell. Thus, facilitated transport has a rate which is
limited by the number of sites. Researchers attempting to increase the rate by increasing the
concentration of transported molecule find that facilitated systems reach a maximum rate than cannot
be substantially increased with increasing concentration of molecule. Facilitated diffusion systems
are therefore saturable. Simple diffusion systems do not behave in this way. They slowly increase
40
transport simply as the concentration of transported molecule increases. vAn ionophore is a system
that transports ions. If the result of the transfer is a change in charge, the process is called electrogenic;
if there is no charge difference, it is called electroneutral.
Active Transport Mechanisms
Active transport mechanisms use energy sources to "pump" ions against concentration gradients. It is
estimated that cells expend about 25% of their ATP just on active transport. Three common active
transport mechanisms are described below. Ion pumps - Directly couple ATP hydrolysis to
transport. A well-studied example is the sodium-potassium pump of the plasma membrane. Note that
in one turn of the multistep cycle, two potassiums are pumped in, three sodiums are pumped out, and
one ATP is cleaved. The pump can be blocked by ouabain which, in the heart, stimulates contraction
because sodium concentration increases and stimulates the sodium-calcium pump to remove sodium
and import calcium. Increasing calcium leads to stronger muscular contraction.
Cotransport Systems - The sodium-glucose cotransport system relies on the concentration gradient
built up by the sodium-potassium pump to drive the import of glucose into cells. In this case, sodium
outside the cell binds to the receptor and, upon binding of a glucose molecule, the sodium
concentration gradient drives the sodium inward and glucose is carried with it).
Transport by Modification - This system relies upon covalently modifying a molecule during (or
shortly after) passive or facilitated transport so that it can no longer pass back through the membrane.
For example, the phosphotransferase system of E. coli uses ATP to phosphorylate sugars as they are
transported into the cell. The phosphorylated sugars cannot pass back out.
Important terminology for active transport mechanisms:
Antiport - moves one or more molecules in as it moves one or more molecules out
Synport - moves all molecules in same direction
Electrogenic - causes change in charge as a result of transport
Electroneutral - causes no change in charge as a result of transport
Peroxide oxidation of membrane lipids. Maintenance of the
membranes integrity.
The peroxidative reaction result from the generation of free radicals, in particular oxygen species,
which have an unpaired electron in the outer shell. The most important of these are superoxyde (O2-),
hydrogen peroxide and hydroxyl radical (OH). These can be produced intracellulary at various sites
such as mitochondria, lysosomes, and sytosol, and they are normally inactivated by the enzymes
superoxid dismutase, catalases and glytathione reductase. Iron is an important factor free radical in cell
injury. Unmodified oxygen free radicals are extremely reactive species that produce among other
things , lipid peroxides which are also reactive species and can propagate the reaction.
Large scale production of reactive oxygen species has the potential to inflict considerable damage
on the tissues in which they are produced, a situation called oxidative stress.
Antioxidant compounds, such as glutathione, vitamin C and vitamin E, and uric acid provide
non-enzymatic protection against oxidative stress because they can scavenge ROS (Reactive oxigen
species) before the ROS can cause damage. Alternatively, antioxidant compounds can prevent
oxidative damage from spreading, such as the chain reaction of lipid peroxidation. Vitamin E is the
principal lipid-soluble antioxidant compound and plays an important role in preventing membrane
damage. -Carotene and other carotenoid compounds related to vitamin A are lipid-soluble
antioxidants that also play roles in free radical trapping. Glutathione plays an important role in
cellular antioxidant protection. Vitamin C (ascorbic acid) is present in far higher amounts in cellular
fluids and probably plays the predominant role in extracellular antioxidant protection. Many
antioxidants act by scavenging reactive oxygen molecules or by chemically reducing oxidized
compounds.
41
Topic 2.12 THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
Investigation of lipids digestion peculiarities. Possible disturbanses of exogenic lipids digestion,
absorbtion and transtort.
Biomedical importance.
Lipids are a heterogeneous group of water-insoluble (hydrophobic) organic molecules that can be
extracted from tissues by no polar solvents. Because of their insolubility in aqueous solutions, body
lipids are generally found either compartmentalized, as in the case of membrane-associated lipids and
droplets of triacylglycerols in adipocytes, or transported by plasma in association with protein as
lipoprotein particles. Lipids are not only a major source of energy for the body, but also provide the
hydrophobic barrier that permits partitioning of the aqueous contents of cells and subcellular
structures. In addition, lipids provide many functions in the body, for example, some fat-soluble
vitamins have regulatory or coenzyme functions, and the prostaglandins and steroid hormones play
major roles in the control of the body's homeostasis. Not surprisingly, deficiencies or imbalances of
lipid metabolism can lead to some of the major clinical problems encountered by physicians, for
example, atherosclerosis and obesity.
The purpose: To develop skills in studying of pancreatic lipase action in order to estimate the role of
bile and lipase in lipid digestion for the further interpreting pathological states of gastrointestinal tract
in clinics.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.139-146, 147-149, 167-168, 172 (A)
(II),173-174 Fig.20.9.(E,F),176-177
2. "Biochemistry", Pamela C. Champe at al.2005.p. 171-180, 187 Fig.16.14.,199-200,217219(A,B),223(E), fig.18.9,18.10.225-226.
3. The «Lipids» Lecture materials.
The main theoretical questions:
1. Structure and properties of dietary lipids (fatty acids, triacylglycerols, phospholipids,
cholesterol)
2. Digestion of triacylglycerols, phospholipids and cholesteryl esters.
2.1. Emulsification of lipid in the small intestine.
2.2. Enzymic degradation of lipids by pancreatic enzymes.
3. Absorption of lipid digestion products.
4. Structure, properties and role of bile acids in digestion and absorption of lipids.
5. Resynthesis of lipids in the intestinal cells.
6. Exogenous lipid transport by blood. Chylomicrons and VLDL.
Disturbance of lipid digestion and absorption: steatorrhea, familiar lipoproteinlipase
deficiency (Chylomicronemia).
Practice instructions for work: «The study of kinetics of pancreatic lipase action».
Essence of the method: The pancreatic lipase activity rate in certain portions of milk is measured by
the amount of fatty acids formed at milk fat hydrolysis at a definite interval of time. The amount of
fatty acids is determined by titration with NaOH solution.
Sequence of Procedures:
42
1. Take 2 test glasses.
2. Pour 10 ml of milk and 1 ml of pancreatic extract into each of them.
3. Add 1 ml of distilled water to one of them and 1 ml of bile to the other.
4. Mix the liquids quickly.
5. Take 1 ml of the mixture out of each glass and put it into 2 clean flasks, add 1-2 drops of 0.5 %
phenolphthalein solution and titrate them by 0.05N NaOH until you get a stable pink color which
remains for at least 30 sec.
6. After that incubate both glasses with the remains of the mixture at 370 C.
7. Take 1 ml of the mixture out of the glasses and titrate it by 0, 05 n. NaOH in the presence of
phenolphthalein every 10 minutes (3-4 estimations).
8. Put the results down in the table.
9. Draw two curves on the basis of these data. They reflect the rate of fat hydrolysis by pancreatic
lipase both in the presence and in the absence of bile.
10. Draw conclusions about bile influence on the lipase activity.
Time of
incubation (in
minutes)
Amount of 0,05n. NаОН (in ml) spent on titration
Test with bile
Test without bile
0
10
20
30
40
50
The curve of pancreatic lipase action in a given time (Plot the amount of 0,05N NaOH (in ml)
spent on titration on axis C).
C
time
Conclusions:
43
M.C.Q.
1. Which amino acid is used for conjugation
with bile acids?
A. alanine;
B. glutamate;
C. tryptophan;
D. glycine;
E. proline
2. Bile salts are necessary for:
A. Absorption of lipid in stomach
B. Creating of low pH in small intestine
C. Emulsification of dietary lipid in small
intestine
D. Secretion of pancreatic enzymes
E. Inhibition of pancreatic lipase
3. What is the function of chylomicrons?
A. Transport of lipid from intestine to tissues
B. Absorption of lipid in the intestine
C. Transport of lipid from adipocytes to
muscle
D. Emulsification of dietary lipid in the
intestine
E. Transport of protein from intestine to tissues
4. What is the primary product of
phospholipase A2 action?
A. monoacylglycerol
B. 1,2-diacylglycerol
C. Glycerylphosphorylcholine
D. Lysophosphatidylcholine
E. 2,3-diacylglycerol
5. At the patient with a chronic hepatitis
significant decrease in synthesis and secretion
of bile is revealed. What substances digestion
and absorption in intestines will be broken at
our patient?
A. Proteins
B. Lipids
C. Carbohydrates
D. Vitamins soluble in water
E. Nucleoproteins
6. Where are chylomicrons formed?
A. In the lacuna of intestine
B.
C.
D.
E.
In the intestinal mucosal cells
In the liver
In the pancreas
In the gall bladder
7. What is the role of mixed micelle?
A. Transport of lipid from intestine to tissues
B. Absorption of lipid in the intestine
C. Transport of lipid from adypocytes to
muscle
D. Degradation of triacylglycerol
E. Transport of protein from intestine to
tissues
8. Food fats in gastrointestinal tract are
exposed to enzymatic hydrolysis. In what
department of gastrointestinal tract is there
splitting of fats at adult people?
A. Oral cavity
B. Thick intestines
C. Stomach
D. Small intestines
E. Gullet
9. Feces of the patient with bilestone illness
contain unsplit fat and have gray-white
color. Specify the possible reason of this
phenomenon.
A. Impossibility of mixed micelles formation in
intestine
B. Absence of pancreatic phospholipases
C. Absence of emulsifying actions of bile salts
on fats
D. Absence of pancreatic lipase
E. Presence plenty of cholesterol in micelles
10. What is the fate of absorbed 2monoacylglycerols in the intestine?
A. They take part in resynthesis of lipids
B. Intestine cells oxidizes them to produce
energy
C. They are stored in the intestine cells
D. They are carried by portal blood circulation
to the liver
E. They are packaged in chylomicrons
44
Task:
1. Write reaction (by formulas ) of phosphatidylcholine (R1- palmitic acid, R2 oleic) hydrolysis
by pancreatic enzymes. Name products.
2. Write reaction (by formulas ) of palmitoiloleilstearate hydrolysis by pancreatic enzymes.
Name products.
3. Write a formulas of conjugated bile acid. Describe functions of bile acids.
45
Topic 2.13
THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
Investigation of fatty acids and keton bodies metabolism. β-oxidation of fatty acids. Cholesterol
synthesis and steroid metabolism. Disturbances of lipid metabolism: atherosclerosis.
Biomedical importance:
Increased fatty acid oxidation is characteristic of starvation and of diabetes mellitus, leading to
ketone body production by the liver (ketosis). Ketone bodies are acidic and when produced in excess
over long periods, as in diabetes, cause ketoacidosis, which is ultimately fatal. Because
gluconeogenesis is dependent upon fatty acid oxidation, any impairment in fatty acid oxidation leads
to hypoglycemia. This occurs in various states of carnitine deficiency or deficiency of essential
enzymes in fatty acid oxidation, eg, carnitine palmitoyltransferase, or inhibition of fatty acid oxidation
by poisons, e. g, hypoglycin.
Impaired Oxidation of Fatty Acids Gives Rise to Diseases Often Associated With Hypoglycemia
Carnitine deficiency can occur particularly in the newborn and especially in preterm infants owing
to inadequate biosynthesis or renal leakage. Losses can also occur in hemodialysis; patients with
organic aciduria have large losses of carnitine, which is excreted conjugated to the organic acids. This
indicates a vitamin like dietary requirement for carnitine in some individuals. Signs and symptoms of
deficiency include episodic periods of hypoglycemia owing to reduced gluconeogenesis resulting from
impaired fatty acid oxidation and ketogenesis in the presence of raised plasma FFA, leading to a lipid
accumulation with muscular weakness. Treatment is by oral supplementation of carnitine. The
symptoms are similar to Reye's syndrome (encephalopathy with fatty degeneration of the viscera), in
which carnitine is adequate, but the cause of Reye's syndrome is unknown. Carnitine
palmitoytransferase I deficiency affects only the liver, resulting in reduced fatty acid oxidation.
Cholesterol is present in tissues and in plasma lipoproteins either as free cholesterol or, combined
with a long-chain fatty acid, as cholesteryl ester. It is synthesized in many tissues from acetyl-CoA and
is ultimately eliminated from the body in the bile as cholesterol or bile salts. Cholesterol is the
precursor of all other steroids in the body such as corticosteroids, sex hormones, bile acids, and
vitamin D. It is typically a product of animal metabolism and therefore occurs in foods of animal
origin such as egg yolk, meat, liver, and brain.
The purpose: To develop skills in analyzing cholesterol and ketone bodies content in biological liquids
for estimation of lipid metabolism in norm and pathology.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p 2005.p 157-160, 163(VI)172,.178-184(D,E).
2. "Biochemistry", Pamela C. Champe at al.2005.p. . 187-198, 217-221, 225 A, 229-235
(D,E).
3. The «Lipids» Lecture materials.
The main theoretical questions:
1. Mobilization of stored fats.
1.1 Fat degradation by hormone-sensitive lipase
1.2 Fate of glycerol
1.3 Fate of fatty acids
2. β-oxidation of fatty acids
2.1 Activation of fatty acids
2.2 Transport of fatty acids in mitochondria
2.3. The reactions of B-oxidation
46
2.4. Energy field from fatty acids oxidations (calculating the amount of ATP by
equation)
2.5. Possible disturbances of carnitine deficiency
3. Ketone bodies metabolism
3.1 Categories of ketone bodies and their role as alternate fuel for cells.
3.2 Synthesis of ketone bodies in the liver
3.3 Utilization of ketone bodies in the peripheral tissues.
3.4 Excessive production of ketone bodies. Ketoacidosis. (Starvations and
diabetes mellitus)
4. Metabolism of cholesterol
4.1 The role of cholesterol in organism
4.2 Synthesis of cholesterol (stage 1 - reactions to mevalonate, stages 2,3 – by
chime)
4.3 Regulation of cholesterol synthesis
4.4 Transport of cholesterol by blood. Metabolism of plasma lipoproteins (LDL
and HDL) and their role in atherosclerosis.
4.5. Degradation of cholesterol
5. The technique of determination of cholesterol and ketone bodies and clinical
importance of these investigations.
Practice instructions
Work № 1.
Determination of cholesterol in blood serum.
Essence of the method is based on Lieberman – Burchard reaction: Cholesterol gives an intense green
color in combination with acetic anhydride and concentrated sulfuric acid. The intensity of the color
proportionally depends on the concentration of cholesterol.
Sequence of procedures:
1. Pour 0.1 ml of blood serum on the bottom of a dry measured tube
2. Add 2.1 ml of reagent № 1 to the tube (reagent № 1is a mixture of ice acetic acid, acetic
anhydride and concentrated sulfuric acid.
ATTENTION!
Pour this reagent only with a MEASURED tube, not a PIPETTE! It’s DANGEROUS.
3. Shake the mixture and leave it for 20 min at room temperature. Green color is developed.
4. After that measure the optical density of the mixture on the photoelectrical colorimeter.
5. Cholesterol concentration is obtained from the standard curve. The normal content of total
cholesterol in blood serum is 2.97 - 8.79 mmol/l
Use the ready standard curve to determine the cholesterol amount by the obtained optical density
47
D
C, mmol/l
Result:
Work № 2. Liebermann-Burchard color reaction for cholesterol
Essence of the method: A chloroform solution of a sterol, when treated with conc. H2SO4, gives a
grass-green color. The usefulness of this reaction is limited by the fact that various sterols give the
same or similar color.
Sequence of procedures:
1. Pour 1 ml of chloroform extract of a cholesterol into the tube
2. Add 10 drops of acetic anhydride and 2 drops of concentrated H2SO4. Carefully!
3. Mix well and observe appearance of green color.
Work № 3. Qualitative reactions for acetoacetate.
Essence of the method: Acetone and acetoacetate turn orange-red with sodium nitroprusside in alkali
medium.
Sequence of procedures:
1. Pour 5 drops of urine into a tube.
2. Add 5% FeCl3 solution by drops until precipitate is formed.
3. Continue to pipette FeCl3. If the solution contains acetoacetate, cherry-red color will appear.
Boiling will speed up this process.
Work № 4. Color reaction for acetone.
Sequence of procedures:
1. Pour 5 drops of urine into a tube
2. Add 5 drops of 10% NaOH solution and 5 drops of Na-nitroprusside. Red-orange color appears.
3. Add 10 drops of ice acetic acid. Color changes to cherry-red.
Conclusions:
48
Task:
1. Write the formula and calculate the yield of ATP associated with the complete oxidation of 1,2
DAG:
R1 – C 26, saturated, R2 –C 14, 1 double bond
2. Write the formula and calculate the yield of ATP associated with the complete oxidation of DAG:
R1 – C 14, saturated, R2 – linoleic acid (C18, 2 double bonds)
3. Write the scheme of glycerol complete oxidation ( throw glycolysis) and calculate the yield of ATP..
49
M.C.Q.
1. The intermediate precursor of mevalonic
acid is:
A Mevalonyl CoA
B. Mevalonyl pyrophosphate
C. Acetyl CoA
D. 3-hydroxy-3-methylglutaryl CoA
E. Isopentenyl pyrophosphate
2. The key enzyme of cholesterol synthesis is:
A. HMG CoA synthetase
B. HMG CoA reductase
C. Mevalonate kinase
D. HMG CoA lyase
E. Squalene synthesis
3. The enzyme triacylglycerol lipase is
activated by hormone:
A. Insulin
B. Glucagon
C. Calcitonin
D. Parathyroid hormone
4.
The 'committed step' in the
biosynthesis of cholesterol from acetylCoA is:
A. Formation of acetoacetyl CoA from
acetyl GoA
B. formation of mevalonate from HMGCoA
C. formation of HMG-CoA from acetyl CoA
and aceto-acetyl CoA
D. formation of squalene by squalene
synthetase
E. formation of lanosterol from squalene
by cyclization.
5.
All statements regarding 3-OH-3
methylglutaryl CoA are true, except:
A. it is formed in the cytoplasm
B. required in ketogenesis
E. VLDL
Task 1.
C. involved in synthesis of FA
D. an intermediate in cholesterol biosynthesis
E. enzyme involved is HMG-CoA synthase.
6. b-oxydation of fatty acid produces:
A. Succinyl CoA
B. Propionyl CoA
C. Acetyl CoA
D. Malonyl CoA
E. Acetoacetyl CoA
7. The rate limiting step in cholesterol
biosynthesis catalyses by:
A. Acetoacetyl synthetase
B. Mevalonate kinase
C. HMG CoA synthetase
D. HMG CoA reductase
E. Thiolase
8. Ketosis is partly ascribed to:
A. Over production of glucose
B. Decreased fat utilization
C. Increased carbohydrate utilization
D. Increased fat utilization
E. Increased level of pyruvate in liver
9. All of the following tissues are capable
of using ketone bodies except:
A. Brain
B. Renal cortex
C. Red blood cells
D. Cardiac muscle
E. Skeletal muscle
10. The major source of cholesterol in
arterial smooth muscle cells is from:
A. IDL
B. LDL
C. HDL
D. Chylomicrons
E. Free cholesterol
1. Which metabolic process is described by scheme below?
Fatty acid A Acylcarnitine Acyl-CoA B β- Hydroxyacyl-CoA
2. Write the names of compounds A and B
3. What is the biological role of this process in the body?
4. Draw the equation of the reaction in fragment that is printed in bold type. (By formulas and words).
5. Name enzyme that catalyses this reaction.
50
Topic 2.14
THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME :
Investigation of fatty acids, triacylglycerol and phospholipid synthesis. Disturbances of lipid
metabolism: obesity; lipid dystrophy of the liver.
Biomedical importance:
Acylglycerols constitute the majority of lipids in the body. Triacylglycerols are the major lipids
in fall deposits and in food. In addition, acylglycerols, particularly phospholipids, are major
components of the plasma and other membranes. Phospholipids also take part in the metabolism of
many lipids. Glycosphingolipids, which contain sphingosine and sugar residues as well as fatty acids,
account for 5-10% of the lipids of the plasma membrane. Phosphoglycerols, phosphosphingolipids,
and glycosphingolipids are all amphipathic lipids and consequently ideally suited as the main lipid
constituents of the plasma membrane.
Fat absorbed from the diet and lipids synthesized by the liver and adipose tissue must be
transported between the various tissues and organs for utilization and storage. Since lipids are
insoluble in water, the problem arises of how to transport them in an aqueous environment—the blood
plasma. This is solved by associating nonpolar lipids (triacylglycerol and cholesteryl esters) with
amphipathic lipids (phospholipids and cholesterol Cholesterol is an amphipathic lipid and as such is an
essential structural component of membranes and of the outer layer of plasma Lipoproteins.
Lipoproteins transport free cholesterol in the circulation, where it readily equilibrates with cholesterol
in other lipoproteins and in membranes. Cholesteryl ester is a storage form of cholesterol found in
most tissues. It is transported as cargo in the hydrophobic core of lipoproteins.
Abnormalities of lipoprotein metabolism occur at the sites of production or utilization of lipoproteins,
causing various hypo- or hyper-lipoproteinemias. The most common of these is diabetes mellitus,
where insulin deficiency causes excessive mobilization of FFA and underutilization of chylomicrons
and VLDL, leading to hypertriacyglycerolemia. Most other pathologic conditions affecting lipid
transport are due primarily to inherited defects in synthesis of the apoprotein portion of the lipoprotein,
of key enzymes, or of lipoprotein receptors. Some of these defects cause hypercholesterolemia and
premature atherosclerosis.
The purpose:
To develop skills in interpreting the content of various lipoproteins in blood serum depending on
lipid metabolism state for the subsequent use of this knowledge in clinical sciences.
The literature:
1. The tutorial book "Principles of biochemistry", 2005.p.148-157, 178-184.
2. "Biochemistry", Pamela C. Champe at al.2005.p. 179-187, 199-202, 229-235.
3. Lecture on the theme «Lipid metabolism»
The main theoretical questions:
1. Fatty acid synthesis
1.1. Transport of acetyl-KoA from mitochondria into cytosol.
1.2. Carboxylation of acetyl KoA. Regulation of acetyl-KoA carboxylase.
1.3 Fatty acid synthase. Reactions, which are catalyzed by synthase. (Scheme)
1.4 Desaturation of fatty acid. The essential fatty acids. (Scheme)
2. Synthesis and deposition of Triacylglycerols. Different fates of Triacylglycerols in
the liver and adipose tissue.
3. Synthesis of glycerophospholipids (phosphatidylethanolamin (P.E.) and
phosphatidylcholine (PC), their
functions.
4. Interrelation between carbohydrates and lipid metabolism.
51
5. Plasma lipoproteins: composition, size and density of lipoprotein particles, functions,
metabolism.
6. Role of lipoprotein in heart disease.
7. Disturbances of lipid metabolism: atherosclerosis, obesity, lipid dystrophy of the
liver.
8. Essence of the method of total lipids determination in blood serum.
Practice instruction.
Work: “Quantative determination of total lipids in blood serum”
Essence of the method: Products of unsaturated lipids breakdown form dark -blue compounds
with the special reagent (which is composed of sulfuric and phosphoric acids and vanillin C)
Intensity of color proportionally depends on concentration of total lipids in blood serum.
Sequence of Procedures:
1. Pour 1 ml of blood serum into the tube.
2. Add 1 ml of phosphonovanillin mixture
3. Mix the contents of the tube well and leave it for 5 min at room temperature. Blue colour develops.
4. Measure the intensity of the colour on photoelectrical colorimeter with green light filter.
5. Obtain the amount of total lipids from the standard curve in the sample and calculate their
concentration in g/l.
The normal content of total lipids in blood serum is 3, 5-8 g/l
D
C, mmol/l
Results:
Conclusions:
52
M.C.Q.
A.
B.
C.
D.
E.
1. A pathway that requires NADPH as
a cofactor is:
Fatty acid oxidation
Extramitochondrial de novo fatty acid
synthesis
Ketone bodies formation
Glycogenesis
Gluconeogenesis.
2. LCAT activity is associated with which of
the lipoprotein complex?
A. LVLDL
B. Chylomicrons
C. IDL
D. LDL
E. HDL
3. The most important source of
reducing equivalents for FA synthesis in the
Liver is:
A. Glycolysis
B. HMP-shunt
C. ТСА cycle
D. Uronic acid pathway
E. Gluconeogenesis.
4. The lipoproteins with the fastest
electrophoretic mobility and the lowest TG
content are:
A. VLDL
B. IDL
C. LDL
D. HDL
E. Chylomicrons
5. Chain elongation of fatty acids occurring
in mammalian. Liver takes place in which of
the following subcellular fractions of the
cell?
A. Nucleus
B. Ribosomes
C. Lysosomes
D. Microsomes
E. Golgi apparatus
6. Which of the following cofactors must be
present for the conversion of acetyl CoA to
Malonyl CoA in extramitochondrial FA
synthesis?
A.
B.
C.
D.
E.
FAD
FMN
АСР
NAD +
Boitin
7. Which lipoprotein accumulates in the
blood stream of patients with familial
hypercholesterolemia?
A. HDL
B. VLDL
C. Chylomicrons
D. IDL
E. LDL
8. In eukaryotic organisms,
phosphatidylcholine can be synthesized
from:
A. Diacylglycerol
B. Phosphatidylseryn
C. Phosphatidate
D. Monoacylglycerol
E. Triacetate
9. Which of the following components is a
precursor of both triacylglycerols and
phospholipids?
A. Phosphatidylethanolamine
B. Acetylcholine
C. Glycerol 3-phosphate
D. Urydine diphosphate glucose
E. Cytidine diphosphate choline (CDPholineA
10. Match the following:
A. Lipoprotein lipase deficiency
B. Obesity
C. Diabetes mellitus — Type-I
D. a-lipoprotein deficiency
E. Deficiency of choline
1. Increase FA acid esterification
2. Increased fat accumulation in liver
3. High levels of free FA-albumin complex
4. Low level or absent high density lipo
proteins
5. High level of chylomicrons in plasma
following a 2 hr fast Substantial module
5“Metabolism of amino acids, its regulation”.
53
Topic 2.15. THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
Digestion of dietary proteins. Investigation of gastric juice chemical composition.
Biomedical importance:
To refer to nutritionally essential amino acids as "essential" or "indispensable" and to
nutritionally nonessential amino acids as "nonessential" or "dispensable" is misleading. While in a nutritional context these terms are correct, they obscure the biologically essential nature of all 20 amino
acids. It might be argued that the nutritionally nonessential amino acids are more important to the cell
than the nutritionally essential ones, since organisms (e.g., humans) have evolved that lack the ability
to manufacture the latter but not the former group.
Medical implications of the material in this chapter relate to amino acid deficiency states that
can result if any of the nutritionally essential amino acids are omitted from the diet or are present in
inadequate amounts. Since certain grains are relatively poor sources of tryptophan and lysine, in
regions where the diet relies heavily on these grains for total protein and is unsupplemented by protein
sources such as milk, fish, or meat, dramatic deficiency states may be observed. Kwashiorkor and
marasmus are endemic in certain regions of West Africa. Kwashiorkor results when a child is weaned
onto a starchy diet poor in protein. In marasmus, both caloric intake and specific amino acids are
deficient.
The purpose:
To develop skills in analyzing of the results of gastric juice acidity determination to use this
knowledge further in clinics for interpreting gastrointestinal tract pathology.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.243-246, 260 (Fig 20.2), 365-367
2. "Biochemistry", Pamela C. Champe at al.2005.p.
3. Lecture on a theme «Protein metabolism»
4. Appendix
The main theoretical questions:
1. Role of dietary proteins in overall nitrogen metabolism.
2. Nitrogen balance.
3. Digestion of dietary proteins.
3.1. Digestion of proteins by gastric secretion
3.2. Digestion of proteins by pancreatic enzymes.
3.3. Digestion of olygopeptides by enzymes of small intestine.
3.4. Absorption of amino acids and dipeptides.
4. Chemical composition of gastric juice.
5. Kinds of gastric juice acidity. The methods of their determination.
6. Abnormalities components of gastric juice.
7. Interpreting of gastric juice analysis results to estimate of stomach secretion function.
Description of the Experiment
The essence of the method is based on the ability of the indicators such as phenolphthalein and
dimethylaminoazobensol (DMA) to change color at definite acidity of media.
DMA changes its color from red in media more acid than 2.9 to yellow in media with pH higher than
4.0. At pH 3.5 intermediate orange colors is observed.
The color of phenolphthalein changes from colorless at pH more acid than 8 to intensive pink at pH
more alkaline than 8.
Work №1.The determination of all kinds of gastric juice acidity in one test tube.
Sequence of Procedures:
1. Pour 5 ml gastric juice into the glass.
54
2. Add one drop of DMA and one drop of phenolphthalein.
If free HCl presents in gastric juice, the simple has red colour.
3. Titrate the solution with 0,1M NaOH to appearance of orange color.
4. Write down this result in the table (point a).
5. Continue the titration until yellow color appears and mark the second point (b).
6. Continue the titration to appearance of pink color and mark the point (c).
Calculation the different kinds of acidity (in 1 ml of 0,1M NaOH):
a). The 1-st result corresponds to the free HCl:
X1 = a •1000 • 0,1
5
b). To calculate total HCl use results of 2-nd and 3-d titration:
(b+c) •1000•0,1
2
5
c). Bound HCl calculate by subtracting the free HCl from the total HCl
X2
==
X3 = X2 - X1
d). The 3-d point corresponds to the total acidity:
X4 = c•1000•0,1
5
Where:
5(ml) - quantity of gastric juice for titration
1000 – Re-calculation coefficient on 1 liter of gastric juice
0,1 – concentration of NaOH
7. Results of titration and calculation put down into the table.
Kinds of
gastric juice
Results of titration( ml of NaOH)
a
b
c
Free HCl
Bound
HCl
Total HCl
Total
acidity
Normal
Hypo acidity
Hyperacidity
Zero acidity
Conclusions:
Work №2.
The determination of gastric juice pathological components. (lactic acid by Uffelman reaction).
Determination of lactate:
Prepare Uffelman reagent in 2 clean tubes as follows: pour 1 ml of 1% phenol solution and add 0.2
ml of 1% chloride iron (iron phenolate of violet color is formed).
Add by drops (20-30 drops) researched solution (gastric juice with pathological components) there
and mix well.
A green-yellow color, which is the characteristics of lactate, appears in the tube, if it contains lactic
acid.
Conclusions:
55
Appendix
In diseases of the stomach and duodenum alterations of gastric secretion often occur. Chemical
examination of gastric contents has a limited but specific value in the diagnosis and assessment of disorders of
the upper gastro-intestinal tract, e.g. peptic ulcer, cancer of the stomach, etc. In order to obtain complete data
regarding gastric function, the contents of the stomach should be examined (a) during the resting period, (b)
during the period of digestion after giving a meal, and (c) after stimulation.
In 24 hours the normal healthy stomach secretes about 1000 ml of gastric juice when the subject is fasting.
But the stomach of a person taking a normal diet secretes 2000-3000 ml of juice per 24 hrs.
The chief constituents of gastric juice are:
(i) HCl secreted by the parietal cells,
(ii) Pepsinogen (and itsisomer gastrixin)e secreted by zymogen cells or "chief cells,
(iii) Rennin — not found in adult gastric juice. Only found in infants/babies,
(iv) Intrinsic factor—required for absorption of vitamin B12, and
(v) Other cells produce an alkaline mucus.
Indications of Gastric Functions Tests
Gastric analysis may be of value in the following:
(i) Diagnosis of gastric ulcer
(ii) Exclusion of diagnosis of pernicious anemia and of peptic ulcer in a patient with gastric ulceration.
The following kinds of gastric juice acidity are determined under clinical analysis:
Total acidity • Free hydrochloric acid • Bound HCl • Total HCl
The acidity of gastric juice is determined after test breakfast, which stimulates gastric secretion.
Total acidity is the sum of all compounds in gastric juice, which can react as acid i.e. free HCl, acid
phosphates, and organic acids. It’s determined by the titration of juice with 0.1M NaOH and measured in
mmol/l. Total acidity in norm for healthy people are:
Adults –
40-60 mmol/l; Newborn –
2.8 mmol/l; Infants – 4-20 mmol/l
Free HCl is unbound acid, which produces hydrogen ions and which makes up acid medium of gastric juice.
(pH 1.5-2.5). Besides as a result of contact with gastric HCl, proteins are denatured. This allows the polypeptide
chain to unfold, making it more accessible to the actions of proteolytic enzymes. HCl activates pepsinogen and
at least low pH has the effect of destroying most microorganisms entering the gastrointestinal tract. In norm the
amount of free HCl is folloving:
For adults –
20-40 mmol/l; For newborn – 0.5 mmol/l
Bound HCl is which present in gastric juice in non-dissociated state like salts with proteins and products of
their degradation (HCl is bound with NH2 groups of this compounds). The amount of bound HCl in norm is:
For adults –
10-20 mmol/l
Total HCl is the sum of Bound HCl and Free HCl.
Abnormal Responses.
Three types of abnormal responses:
(a) Hyperacidity (hyperchlorhydria) in which free acid reaches a higher concentration than in normal
persons.
(b) Hypoacidity (hypochlorhydria) in which though free acid is present, it is present in a concentration
below the normal range.
(c) Achlorhydria in which there is no secretion of free acid at all.
dHyperchlorhydria: This occurs when the maximum free acidity exceeds 45 mmol/L, some prefer to keep at
50 mmol/L, and combined acid remains the same as in normal persons.
56
Causes:
a. Hyperacidity is found in the following:
(i)
In duodenal ulcer
(ii)
In gastric ulcer: Though hyperacidity is common, 50% cases may give normal results, whilst in
some chronic cases, due to associated gastritis, hypoacidity may be found.
Blood may be present in gastric contents. Blood together + hyperchlorhydria are suggestive of gastric ulcer.
(iii) Gastric carcinoma: small % of cases shows hyperacidity and blood.
(iv) Jejunal and gastro-jejunal ulcers occur as sequela to gastroenterostomy — they are often found
associated with hyperacidity after operation.
Other disorders where hyperacidity may be found are — gastric neurosis, hyperirritability and pylorospasm,
pyloric stenosis, chronic cholecystitis, chronic appendicitis, etc.
(b) Hypoacidity (hypochlorhydria): It is difficult to define this zone. Low acidities are found in carcinoma
of stomach and in atonic dyspepsia. In pernicious anemia, free HC1 is absent in gastric secretion.
Gastroenterostomy—hypoacidity seen.
(c) Achlorhydria: This term is used when there is no secretion of HCI, but enzyme like pepsin is present.
Achlorhydria can be differentiated from hypochlorhydria by stimulation test with histamine.
In hypochlorhydria-histamine stimulation shows rise in free HCI.
In achlorhydria-histamine stimulation does not show response.
Causes:
(i) Found in some normal people increasing with age about 60 to 75 years.
(ii) High incidence in carcinoma of stomach.
(iii) In chronic gastritis, tendency of gastric acidity to be reduced. As the disease progresses, increasing
incidence of achlorhydria seen.
(iv) Partial gastrectomy leads to reduction of gastric acidity often and to achlorhydria in a considerable
number of cases.
(v) In pernicious anemia.
(vi) Other diseases — Microcytic hypochromic anemia (in 80% cases), hyperthyroidism and myxedema may
be associated with achlorhydria.
d) Achylia gastrica: The term is used when both enzymes and acids are absent indicating there is a
complete absence of gastric secretion.
Causes: (i) in advanced cases of cancer of stomach, (ii) advanced cases of gastritis, (iii) typically found in
pernicious anemia and of subacute combined degeneration of the spinal cord (100% cases).
Abnormal components of gastric juice:
Organic Acids
Lactic acid and butyric acid may be present in large amounts in cases where there is achlorhydria and
hypochlorhydria and residual foods must remain in stomach. In absence of HCl, the microorganisms can thrive
well and ferment the food residues to produce the organic acids, lactic acid and butyric acid.
Achlorhydria associated with retention of food materials is exclusively found in carcinoma stomach.
57
M.C.Q.
1
. An important etiologic factor in
Kwashiorkor is:
A. Excess dietary vitamins;
B. Steatorrea;
C. Anaemia;
D. Dietary protein deficiency;
E. Dietary mineral deficiency.
2. The zymogene form tripsinogen of
pancreatic juice is converted to active tripsin
by:
A. Pepsin;
B. Enterokinin;
C. Enterokinase;
D. Rennin;
E. Gastrin
6. What component of gastric juice is
responsible for low pH in the stomach?
A. Inactive pepsinogen
B. Bound hydrochloric acid
C. Rennine
D. Free hydrochloric acid
E. Lactic acid
7. Choose an abnormal component of gastric
juice:
A. Mucus
B. Lactic acid
C. HCl
D. Pepsinogen
E. Rennin
3. Gastric juice contains the enzyme:
A. Tripsinogen
B. Pepsinogen
C. Amylase
D. Chymotripsinogen
E. Enterokinase
8. What gastric juice factor deficiency is the
results in megaloblastic anemia?
A. Pepsin
B. Chlorine hydrate
C. Gastromucoprotein
D. Mucin
E. Gastrin
4. The milk protein in the stomach in an
adult is digested by:
A. Pepsin
B. Rennin
C. HCL
D. Tripsin
E. Chymotripsin
9. The very acid pH in the stomach, about
1,5-2, causes all of the following Except:
A. Denaturation of food proteins
B. Emulsification of fats
C. Activation of pepsinogen
D. Maximum activity of pepsin
E. High death rate of bacteria in the stomach
5. What kind of posttranslational
modification results in activation of
pancreatic enzymes?
A. proteolytic cleavage;
B. methylation;
C. acylation;
D. sulfation;
E. phosphorylation
10. There are three residues of aromatic
acids in protein structure, but only one of
them is synthesized in humans. Point out it:
A. Tyr
B. Ala
C. Phe
D. Trp
E. Ser
11. Which peptide bond is most likely to be hydrolyzed by chymotrypsin?
A
B
C
D
E
Cys ----- Glu ----- Phe ----- Ala ----- Lys ------ Asn
58
Topic 1.16. THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME:
Studies of amino acids transformation (deamination, transamination, decarboxylation)
Investigation of separate amino acid metabolism pathways. Disturbances of amino acid
metabolism
Biomedical importance.
Certain disorders of amino acid metabolism have played major roles in elucidating the pathways by
which amino acids are metabolized in normal human subjects. While most of these diseases are rare and hence
are unlikely to be encountered by most practicing physicians, they pose formidable challenges for psychiatrists,
pediatricians, genetic counselors, and molecular biologists. Left untreated, many of these genetic disorders
result in irreversible brain damage and early mortality. Prenatal or early postnatal detection and rapid initiation
of appropriate treatment, if available, therefore is essential. Since several of the enzymes concerned are
detectable in cultures of amniotic fluid cells, prenatal diagnosis by amniocentesis is possible. Treatment consists
primarily of feeding diets low in the amino acids whose catabolism is impaired. Recombinant DNA technology
may, however, ultimately provide ways to correct genetic defects by "gene therapy."
Mutations in the exons or regulatory regions of a gene that encodes an enzyme of amino acid catabolism
can result in a nonfunctional enzyme or in complete failure to synthesize that enzyme. While some changes in
the primary structures of enzymes may have little effect, others may profoundly modify the 3-dimensional
structure of catalytic or regulatory sites. The modified or mutant enzyme may possess altered catalytic
efficiency (low V max or high Km) or altered ability to bind an allosteric regulator of its catalytic activity. A
variety of mutations may cause the same clinical symptoms. For example, any mutation that significantly lowers
the catalytic activity of argininosuccinase will cause the metabolic disorder.
The catabolism of the 20 amino acids found in proteins involves the removal of a-amfno groups
followed by the breakdown of the resulting carbon skeletons. The catabolism of the carbon skeletons
converges to form seven products: oxaioacetate, a-ketoglutarate, pyruvate, fumarate, acetyl CoA,
acetoacetyl CoA, and succinyl CoA. These products enter the pathways of intermediary metabolism,
resulting either in the synthesis of glucose or lipid, or in the production of energy through their
oxidation to CO2 and water by the citric acid cycle.
Mutant genes that generally result in abnormal proteins, most often enzymes, commonly cause inborn
errors of metabolism. The inherited defects may be expressed as a total loss of enzyme activity or,
more frequently, as a partial deficiency in catalytic activity. Without treatment, the inherited defects of
amino acid metabolism almost invariably result in mental retardation or other developmental abnormalities due to harmful accumulation of metabolites. Although more than 50 of these disorders have
been described, most are rare, occurring less than 1 per 500,000 in most populations. Collectively,
however, they constitute a very significant portion of pediatric medicine. Phenylketonuria is discussed
in some detail, because screening tests and prenatal diagnosis are available
The purpose:
To develop skills in analyzing of aminotransferases activity results in blood serum for the further
use of these knowledges in clinic diagnostic of internal organs pathology and in interpreting of amino
acids conversion to specialized products, metabolism of amino acids carbon skeletons and metabolic
defects in amino acid metabolism.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.195-198. 204-208
2. "Biochemistry", Pamela C. Champe at al.2005.p. 247-250, 259-264,283-A , 285 C,D261263(E,), 264 (H),266 (D,E),266-274, 285 (B).
3. Lecture on a theme «Protein metabolism»,.«Amino acids metabolism»
The main theoretical questions:
1. Sources and fates of amino acids.
2. Deamination of amino acids (remuvel of nitrogen). The direct oxidative
deamination.
2.1.D-and L-amino acid oxidase, coenzymes.
59
3.
4.
5.
6.
2.2. Glutamate dehydrogenase, coenzymes.
Indirect deamination.
3.1.Transamination as funneling of aminogroups to glutamate.
3.2. Glutamate dehydrogenase reaction.
Transamination
4.1.Action of aminotransferases and coenzymes.
4.2. The role of the transamination in amino acids metabolism.
4.3. Diagnostic value of plasma aminotranseferases (AST and ALT)
The glucose-alanine cycle and it role in the organism.
Decarboxylation of amino acids. Synthesis and degradation of biogenic amines:
histamine, seratonine, dophamine and Gamma-amino-butysic acid. Biological action
of these compounds. The role of MAO.
7. The metabolic pathways for carbon skeleton of amino acids. Glucogenic and
ketogenic amino acids.
8. Metabolism of glycine and serine. (scheme only).The role of folic acid in amino
acid metabolism
9. Methionine as methyl-group donor in reactions of synthesis ( creatine,
phosphatidylcholine, epinephrine).
10.Amino acids as precursors of specialized products:
a) tryptophan -niacin and serotonine,
b) histidine - histamine,
c) tyrosine- catecholamines and melanin.
d) glutamate- GABA
11. Metabolism of phenylalanine and tyrosine.
a) conversion of phenylalanine to tyrosine (reaction);
b) formation of catecholamines and melanin ( scheme)
c) degradation of phenylalanine and tyrosine (scheme, final products)
12. Metabolic defects in amino acid metabolism.
a) Phenylketonuria , alcaptonuria, albinism (phenylalanine and tyrosine);
Practice instructions
Work №1.
The essence of the method is based on the transamination reaction of alanine and aspartate.
Aminotransferases are normally intracellular enzymes. Their value in the parenchime organ’s tissues
of healthy people is about 1000 times as great as in the blood serum. Thus, the presence of elevated
levels of aminotransferases in the serum indicates damage to cells riche in these enzymes. Desease
processes can cause cell lysis, resulting in release of intracellulas enzymes into the blood.
Sequence of Procedures: Perform epeeriment for blood serum 1 and 2.
Work №1. The determination of AST activity.
1. Pour 0.5 ml of the substrate-buffer mixture № 1 into the tubes.
2. Add 0.1 ml of blood serum .
3. Incubate at 37C for 15 minutes.
4. Add 0.5 ml of 2,4 dinitrofenilhydrazine solution and stay for 20 minutes at room temperature.
5. Add 5 ml 0,4 N NaOH.
6. Measure the optical density on photocolourimeter at green filter.
60
Work №2. The determination of ALT activity.
1. Pour 0.5 ml of the substrate-buffer mixture № 2 into the tubes.
2. Add 0.1 ml of blood serum.
3. Incubate at 37oC for 30 minutes.
4. Add 0.5 ml dinitrophenil hydruzine solution and leave for 20 minutes.
5. Add 5 ml 0,4 N NaOH.
6. Measure the optical density at green filter.
D
C, mmol/l
CALCULATION:
1. Derive the piruvate concentration (C) from the standart curve.
2. Calculate the activity of the enzymes in mkMol of pyruvate which forms during incubation 1
ml of blood serum by the formulas:
XAst = 10 C =
XAlt = 10 2 C =
Where:
C – the amount of piruvic acid from standard curve.
10 – coefficient of re-calculation to 1 ml of serum.
2 – coefficient
Results of experiment: AST1 =
ALT1 =
AST2 =
ALT2 =
Normal activities:
AST = 0.1-0.5 mkMol/ml
Conclusions:
ALT = 0.1-0.7 mkMol/ml
61
M. C.Q.
1. Transamination from alanine to αA. thiamine pyrophosphate (TPP).
B. NADH
C. biotin
D. pyridoxal phosphate (PLP).
E. No coenzyme is involved
2. In amino acid catabolism, the first
reaction for many amino acids is an:
A. decarboxylation requiring thiamine
pyrophosphate (TPP).
B. reduction requiring pyridoxal phosphate
(PLP).
C. transamination requiring pyridoxal
phosphate.
D. hydroxylation requiring NADPH and O2.
E. oxidative deamination requiring NAD+.
3. Which of the following amino acids are
both ketogenic and glucogenic?
A. trptophan
B. tyrosine
C. threonine
D. arginine
E. lysin
4. Which of the following enzymes is
responsible for the oxidative deamination of
glutamate?
A. glutaminase
B. glutamate dehydrogenase
C. glutamate transaminase
D. none of the above
E. all of the above
5. Which amino acid is a precursor of
serotonin and melatonin?
A. asparagine
B. Histidine
C. glycine
D. tryptophan
E. Serine
6. In examining blood serum the patient was
revealed to have increased activity of AlT.
What organism changes at the cellular level
lead to such impairments?
*A. Impairment of plasma membranes
B. Impairment of intercellular interactions
C. Impairment of enzyme system
D. Impairment of energy provision
E. Impairment of the genetic apparatuses
Task 1.
Fulfill
1.
2.
3.
4.
the following task for each equation:
Write the missing substrates and products:
Give the names and formulas of all compounds
Which metabolic process does this equation belong to? Its biological role
Name enzyme and coenzyme ( if it requires in this reaction)
1. a-ketoglutarate + ? ---
2. Histidine -- ? + CO2
.
.
pyruvate + ?
62
M.C.Q.
1. In newborn the hypertonia of muscles and
seizures are observed. On the forth day of
life the specific ‘mousy’ odor was felt from
infant. After interaction of urine with FeCl3
the green-blue color appears. What
additional investigations are the most
important?
A. Phenylalanine in blood serum and urine
B. Adrenalin, noradrenalin in blood serum and
urine
C. Thyroxin, TSH in blood serum
D. Sodium chloride in sweat
E. Glucose in blood serum and urine
2. In newborn the hypertonia of muscles
and seizures are observed. On the forth day
of life the specific ‘mousy’ odor was felt
from infant. After interaction of urine with
FeCl3 the green-blue color appears. What
disease is it possible to think about?
A. Phenylketonuria
B. Branched chain aminoaciduria (maple
syrup disease)
C. Tyrosinosis
D. Hartnup’s disease
E. Familial cystinuria
3. In newborn the hypertonia of muscles and
seizures are observed. On the forth day of
life the specific ‘mousy’odor was felt from
infant. After interaction of urine with FeCl3
the green-blue color appears. The cause of
such state can be absence of:
A.phenylalaninhydroxylase
B. xantinoxydase
C. oxydase of homogentisic acid
D. phosphorilase
E. glucose-6-phosphatase
4. Mother of year old boy complaints that
his ears and tip of nose became darker, urine
is to darken upon standing. Blood level of
bilirubin is 19.5 mmol/l (norm). What is the
more possible reason for this state?
A. Deficiency of oxidase of homogentisic acid
B. Deficiency of phenylalanine oxidase
C. Deficiency of glucuronyl transferase
D. Parenchimatous jaundice
E. Hemolytic jaundice
5. Mother of 5-year old boy complaints that
his ears and tip of nose became darker, urine
is to darken upon standing. Color of feces is
as usual. The cause of such state can be:
A. alkaptonuria
B. phenylketonuria
C. branched chain aminoaciduria (maple syrup
disease)
D. Hartnup’s disease
E. podagra (gout)
6. In a year old child urine is to darken upon
standing. In the blood and urine
homohentisine acid is found. Мetabolism of
what substance is disordered?
A. Tyrosine
B. Purine nucleotides
C. Leicine
D. Tryptophan
E. Melanin
7. There are three residues of aromatic acids
in protein structure, but only one of them is
synthesized in humans. Point out it:
A. Tyr
B. Trp
C. Phe
D. Ser
E.Ala
8. In traumatology department the patient
with crushing of muscle tissue is admitted.
What biochemical parameter of urine will be
increased?
A. Creatin
B. Creatinine
C. Carmine
D. Carotine
E. Carnitin
63
9. Result of biochemical investigation of
patients blood serum shown that activity of
aspartate aminotraspherase is 1.5 mmol/h*l,
alanine aminotransperase – 0.47 mmol/h*l.
Pathology of what organ is more probable in
this patient?
A. Heart
B. Liver
C. Kidney
D. Intestinum
E. Vessels
10. In the young men, 18 years, the muscle
dystrophy is diagnosed. Increase of what
blood serum parameters is most
characteristic for this pathology?
A. Creatin, creatin kinase (MM–form, and
particularly MB–form)
activity
B. Creatinin, creatin kinase (BB–form, and
particularly MB–form)
activity
C. Activity of aminotransferases
D. Activity of LDH4
E. Activity of alkaline phosphotase
11. A patient with crash of the muscular
tissue was brought to a tramatological
department. What biochemical index of
urine will be increased?
A. Creatinine
B. Uric acid
C. General lipids
D. Mineral salts
E. Glucose
12. Synthesis of phospholipids is disordered
due to fat infiltration of liver. Indicate which
of the presented substances can enhance the
process of methylation during phospholipids
synthesis?
A. Methionine
B. Glucose
C. Ascorbic acid
D. Citrate
E. Glycerin
13. A patient, undergoing a course of
curative starvation, has a normal glucose
level of the blood mainly due to glucogenesis.
What amino acid in human liver the most
actively synthesizes glucose?
A. Valine
B. Glutamic acid
C. Lysine
D. Leucine
E. Alanine
14. Patient with encephalopathy was
admitted to the neurological in-patient
department. Correlation of increasing of
encephalopathy and substances absorbed by
the bloodstream from the intestines was
revealed. What substances that are created
in the intestines can cause endotoxemia?
A. Indole
B. Acetacetate
C. Ornithine
D. Butyrate
E. Biotin
15. Which amino acid defective metabolism
is associated with urine that darkens up
standing and with ochronosis?
A. histidine
B. aspartate
C. alanine
D. proline
E. Tyrosine
16. Inherited disorder cystinuria is
associated with abnormal metabolism of:
A. isoleucine
B. glutamate
C. cysteine
D. proline
E. alanine
64
Appendix .
Alkaptonuria
A rare inborn error or hereditary defect in metabolism of Phenylalanine and Tyrosine. It is of
historical interest - Garrod's ideas concerning heritable metabolic disorders was proposed.
Inheritance — autosomal recessive
Incidence — Estim
ated incidence 2 to 5 per million live births. Over 600 cases have been reported in literature.
Enzyme deficiency—lack of the enzyme homogentisate oxidase. Homogentisic acid
accumulates in the tissues and blood and appears in urine. Most striking clinical manifestation —
is occurrence of dark urine on standing in air. Homogentisic acid like many derivatives of
tyrosine is readily oxidized to black pigments ("alkapton"). Urine when exposed to air slowly
turns black from top to down.
In long standing cases, deposition of homogentisic acid derivatives in cartilages of ears and other
exposed places leading to generalised pigmentation of connective tissues and deposition in joints
leading to arthritis, a condition called Ochronosis.
Treatment — involves a diet low in phenyl alanine and tyrosine.
Hereditary Tyrosinaemia
An uncommon inherited disorder. More than 100 cases have been reported in literature.
Enzyme deficiency—inherited deficiency of the enzyme p-OH-pftenylpyruvate oxidase.
Biochemical features similar to phenylketonuria. Blood levels of tyrosine and phenylalanine are
elevated.
Urinary excretion of the following increases — increased excretion of tyrosine, p-OH-Phenyl
acetate, and N-acetyl tyrosine. Usually death ensues before six months due to Liver failure.
Treatment involves feeding a diet low in protein, specially with low phenylalanine and tyrosine.
Albinism
It includes a spectrum of clinical syndromes characterized by "hypomelanosis", arising from
inherited defects in the pigment cells (melanocytes) of eye and skin.
There are various forms of the disease. But can be divided into two major groups —
(a) Oculo-cutaneous albinism: More than ten forms are known.
In this there is decreased pigmentation of skin and eyes. They can be differentiated by clinical
presentation and biochemical and other features.
(b) Ocular albinism: Affects only eye and not the skin. Occurs both as autosomal recessive and
as an X-linked trait.
Metabolism of Sulphur-containing Amino acids
Sulphur containing aniinoacids are three:
1. L-Methionine — essential aminoacid,
2. L-Cysteine } Non-essential aminoacid
3. L-Cystine } (both)
Metabolic Role of Methionine
Methionine is "glucogenic": Propionyl CoA the endprocluct of catabolisni is converted to
succinyl-coA an intennediate of T.C.A. cycle.
Lipotropic function: "Active" methionine can donate "methyl group" and can form choline
from ethanolamine. Choline is lipotropic and prevents accumulation of fat Liver ( fatty Liver).
Transmetliyhition: Certain compounds of the body, with structures containing -CH3 group
attached to an atom other than carbon can take part in enzymic reactions, whereby these —
CH3 group are transferred to a suitable "acceptor", which have no — СНз group.
Such reactions are termed as "transmethylation reaction", and the substrate i.e. the —CH3
donor is said to possess biologically labile-—CH3 group". The methionine is most important
compounds with biologically labile methyl group :(— S — CH3 group).
"Active" Methionine
Chemically called as "S-adenosyl methionine"
65
Activation of methionine occurs in presence of ATP, catalyzed by an enzyme, called Lmethionine-adenosyl transferase. In the process of activation, ATP donates the entire
adenosine moiety to methionine and loses 3 molecules of PO4, one as orthophosphate and two
as Pyrophosphate.
CH3 group forms a 'high energy' bond with sulphur (— S – CH3), this attributes to lability of
methyl group. Formation of 'active' methionine is shown below:
Adeninc-R-P - (P) - (P)
(ATP)
Methionine.
Mg++
Glutathion- SH
L-methionine adenosyl transferase
S-adcnosyl methionine
COOH
CHNH2
CH2
I
+
S-R-Adenine
ICH3
Active methionine is – CH3 group donor in the synthesis of:
Epinephrine, Choline, Creatine, Melatonin
Homocystinuria
An inborn error of metabolism, which involves the catabolism of methionine or more
specifically its metabolic intermediates, homocysteine/and homo-cystine.
Enzyme deficiency — Genetic deficiency of the enzyme cystathionine synthetase
Accumulation of homocysteine. Plasma level of homocystine and exretion in urine
increases.
Clinical features: Mental retardation – in children and surviving adults, hepatomegaly,
skeletal deformities.
1. Maple Syrup Urine Disease
An inherited disorder of branched chain amino acids.
Enzyme defect—Absence of α-ketoacid decarboxylase or greatly reduced activity of the
enzyme.
As a result the conversion of all three branched chain α-keto acids to CO2 and acyl CoAthioesters is interferred with ketoacids are excreted. Hence it is also called as — Branchedchain ketonuria
Small amounts of branched-chain a-OH-acids, formed by reduction of α-keto acids are also
excreted in urine.
The urine has characteristic odour, which resembles that of maple syrup or burnt sugar,
hence the name.
Treatment: Infant is fed a diet in which protein is replaced by a mixture of purified
aminoacids from which branched chain aminoacids leucine, valine and iso-leucine are omitted.
66
Topic 1.17 THE METHODICAL GUIDELINES FOR PRACTICE ACTIVITY ON THE THEME
Investigation of ammonia detoxication and urea synthesis mechanisms.
Biomedical importance:
Ammonia, derived mainly from deamination of the a-amino nitrogen of amino acids, is toxic to
all animals. Human tissues therefore initially detoxify ammonia by converting it to glutamine for
transport to the liver. Deamination of glutamine in the liver releases ammonia, which then is efficiently
converted to the nontoxic, nitrogen-rich compound urea. Efficient biosynthesis of urea is essential for
health. Where liver function is seriously compromised, eg, in individuals with massive cirrhosis or
severe hepatitis, ammonia accumulates in the blood and generates clinical signs and symptoms. Rare
but injurious metabolic disorders of all 5 urea cycle enzymes and of N-acetylglutamate synthetase have
been reported. In those few infants bom with a deficiency in the activity of an enzyme of the urea
cycle, appropriate treatment requires an understanding of the biochemistry of urea synthesis.
The purpose: To develop skills in estimating of nitrogen metabolism, liver and kidney functional
state by urea content results in blood for the further use in clinic diagnostic.
Literature:
1. The tutorial book "Principles of biochemistry", 2005.p.198-203.
2. "Biochemistry", Pamela C. Champe at al.2005.p.250-258.
3. The «The amino acid metabolism» Lecture Materials;
The main theoretical questions:
1. Metabolism of ammonia:
1.1. Ammonia sources.
1.2. Hyperammonemia, symptoms of poisoning.
1.3. Mechanism of ammonia toxicity
1.4. Transport of ammonia in the circulation.
2. Render harmless of ammonia in periphery tissues.
2.1 . Reductive animation of α-ketoglutarate.
2.2 . The formation of glutamine and asparagine, their role and fate.
2.3 . Glucose-alanine cycle.
2.4 . Formation of ammonia salts in the kidney.
3. Urea cycle.
3.1. Reactions of the cycle, enzymes.
3.2. Regulation of the urea cycle.
3.3. Fate of urea.
3.4. Interrelation between urea cycle, CAC and transamination.
3.5. Genetic deficiency of the urea cycle enzymes.
Practice instructions
The essence of the method is based on the urea cleavage to CO2 and NH3 by urease. The amount of
NH3 is determined calorimetrically.
Description of experiment:
Making urease preparation by following method:
1. Peel 3-4 water-melon seeds and pound them with 1 ml of water in mortar.
2. Add 10 ml of distilled water, pound again.
3. Filtrate obtained suspension and use the filtrate as the urease source.
67
4. Take 2 test tubes: experimental and standard (tubes for centrifugation)
5. Pour 1.5 ml distilled water both into the tubes.
6. Add 0.1 ml of the blood serum into the 1-st and 0.1 ml of 30% standard urea solution into second
tube.
7. Add 0.5 ml urease preparation both into the tubes, mix well and incubate at 37C for 20 minutes.
8. Cool the tubes with cold water and add 0.2 ml 7.5% ZnSO4 solution and 0.2 ml 1.5% NaOH4 both
into them.
9. Mix well and centrifuge both tubes for 10 min, until transparent supernatant will be obtained.
10. Pour out 1.5 ml of the supernatant both from the tubes into two clean tubes.
11. Add 2.5 ml of segnet salt and 0.5 ml Nessler reagent.
12. Mix the contents of the tubes and measure optical density with blue light filter in 0.5 mm flask
Calculate the amount of urea by the formula:
X mg %
D0 30mg%
Dst
Where:
D0 – Density of experimental solution
Dst – density of standard urea solution
To obtain result in SI-system (mmol/l) multiply the data by 0.1665
Normal content of urea in blood: 20-40 mg% or 3,33 – 08,32 mmol/l
Results:
Conclusions:
Task.
1. High concentration of citrulline was found in urine of newborn.
1. Name this disease.
2. Which enzyme deficiency is observed in this case?
3. Draw the equation of citrulline formation in urea cycle ( by the formulas).
4. Name all components.
2. The brain ammonia isn’t neutralized through the formation of urea and NH3 is especially toxic for
CNS
A. Name the terminal product of ammonia neutralization in the brain:
B. Which enzyme catalyses this reaction?
C. Draw the equation of this product formation in urea in brain.
D. Name all components
E. What is the future fate of this compound?
3. Which metabolic process is described by scheme below?
(Ammonia + Carbon dioxide) A Citrulline argininosuccinate B Urea
2. Write the names of compounds A and B
3. What is the biological role of this process in the body?
4. Draw the equation of the reaction in fragment that is printed in bold type. (By formulas and words).
5. Name enzyme that catalyses this reaction.
68
M. C. Q.
1. What process enzymes deficiency can
cause hereditary hyperammonemia?
A. Urea cycle
B. CAC
C. Glucose-alanine cycle
D. Synthesis of glutamine
E. Transamination
2. The second reaction of urea synthesis
takes place in:
A. Mitochondria
B. Cytosol
C. Membrane
D. Nucleus
E. Ribosome
3. In the urea cycle, argininosuccinate
synthetase catalyzes:
A. Cleavage of urea to ammonia
B. Transamination of arginine.
C. Formation of ornithine from citrulline and
another reactant.
D. Formation of citrulline from ornithine and
another reactant.
E. Formation of argininosuccinate.
4. Which of the following compounds serves
to regulate the urea cycle?
A. Malonyl CoA
B. Citrate
C. Acetyl CoA
D. Cytoplasmic carbamoyl phosphate
E. N-acetylglutamate
5. Which of the following is NOT an
intermediate in the urea cycle?
A. Arginine
B. Citrulline
C. Ornithine
D. Glutamine
E. Fumarate
6. Which of the following statements about
the synthesis of carbamoyl phosphate by
carbamoyl phosphate synthetase I is
incorrect?
A. The reaction is allosterically activated by Nacetylglutamate
B. The reaction requires two high-energy
phosphates for each carbamoyl phosphate
molecule synthesized
C. The reaction is reversible.
D. The enzyme incorporates CO2 into
carbamoyl phosphate.
E. The enzyme catalyzes the rate-limiting
reaction in the urea cycle.
7. The source of ammonia in the body is:
A. Urea cycle
B. Deamination of heme
C. Glutamine synthesis
D. Formation of biogenic amines
E. Catabolism of purines and pyrimidines.
8. Biosynthesis of Amino Acids Animal cells
incorporates NH4+ into organic molecules.
The addition of an NH4+ molecule to αketoglutarate to produce glutamate
requires:
A. NADPH
B. NADP+
C. NADH
D. H2O
E. ATP
9. The source of ammonia in the body is:
A. Deamination of heme
B. Urea cycle
C. Glutamine synthesis
D. Bacteria action in intestine
E. Formation of biogenic amines
10. Hyperammonemia which develops under
liver cirrhosis can cause:
A. Coma and death
B. Hypoglycemia
C. Diarrhea
D. Dermatitis
E. Macrocytic anemia
69
Questions for Module 2
PROTEINS.
1.Structure, physical and chemical properties, classification of amino acids.
2. Structure of peptides and peptide-bond characteristics.
3. Structural organizations of protein molecules: primary, secondary, tertiary (fibrous and globular
protein) and quaternary structure (for example hemohlobine).
4. Physical and chemical properties of protein. (Charge, electrophoresis, denaturation).
ENZYMES.
1. Definition and chemical nature of enzymes.
1.1. Proof of protein nature of enzymes;
1.2. Common and distinct features in enzymes and non-enzymic catalysts.
2. Structural and functional organization of enzymes:
2.1. Simple and compound enzyme proteins. Cofactors, their nature and role in enzyme function;
2.2. Proenzymes, examples, biological value.
2.3. Multienzyme complexes, examples;
2.4. Isoenzymes, value of their definition in clinical diagnostics, examples;
2.5. Structure of an Active center, its role in enzyme function;
2.6. Allosteric center of enzymes, its role;
2.7.The relationship of enzyme structure and its activity.
3. Properties of enzymes:
3.1 Dependence of enzymatic reaction rate on temperature. Curve.
3.2. Dependence of enzymatic reaction rate on рН of medium. Curve.
3.3. Specificity of enzymic action, kinds and examples of specificity.
4. The mechanism of enzymatic catalysis.
4.1. The idea about energy of activation;
4.2 . The theory of enzyme-substrate complex
4.3. Fisher hypothesis and Koschland theory
5. The kinetics of the enzymatic reactions.
5.1. The enzyme reaction velocity dependence on substrate concentration
5.2.
Michaelis-Menten equation. Michaelis constant.
6. Activators and inhibitors of enzymes
6.1.
Activation of the enzymes (examples);
6.2.
Inhibition: reversible and irreversible, competitive and noncompetitive. Examples.
6.3.
The useful of the activators and the inhibitors in medical practice.
7. Regulation of the enzymes activity.
7.1.
Irreversible covalent activation (partial proteolysis).
7.2.
Reversible covalent modification (phosphorylation-dephosphorylation)
7.3.
Feedback regulation
8. Classification of enzymes: The short characteristic, examples;
1. Oxidoreductase; 2.Transferase; 3.Hydrolase; 4.Leases; 5.Isomerase; 6. Ligase (synthetases).
VITAMINS:
1. Definition, classification and nomenclature of vitamins.
2. Vitamin balance disorders in an organism: avitaminosis (exogenous and endogenic); Primary and
secondary avitaminosis and hypovitaminosis. Polyavitaminums. Hypervitaminosis. Antivitamins and
provitamins.
3. Structure, coenzyme form, biological role, sources, symptoms of avitaminosis: В1, В2, В6, С, РР, (
with formulas), В12, pantothenic and folic acid, biotin.( without formulas). Name coenzyme forms of
each vitamin. What vitamins are synthesized by a microflora of an intestine?
Basic concepts of metabolism, bioenergetics.
1. Catabolism and anabolism, their interrelation.
2. Specific and common pathways of catabolism.
70
3. Modern view on the mechanism of biological oxidation. Exergonic and endergonic reactions.
Energetic coupling in biological systems.
4. High-energy compounds: definition, types of high-energy bonds (phosphoanhydride, thioester),
and free energy of hydrolysis.
5. ATP as main form of energy storage and carries in cells. Types of ATP synthesis reactions:
substrate level phosphorilation, oxidative phosphorilation, and photophosphorilation.
6. Biologocal oxidation reaction types. Enzymes, role.
7. Active oxigen forms (AOF): singlet oxigen, hydrogen peroxide, hydroxyl radical, and superoxide
radical. Formation (Generation) in the body, reasoms of toxicity, biological role.
8. Structure, functions and localization of an electron transport chain. It’s components
(dehydrogenase and cytochromes, its cofactors); role of redox potential in components arrangement.
9. Oxidative phosphorylation. Coupling tissue respiration with ATP synthesis. Location of
phosphorylation sites in respiratory chain.
10. Energy value of substrates, P/O coefficient.
11. Inhibitors of respiration chain, influence on organism.
12. Uncouplers. Free non-oxidative phosphorylation, its biological role.
13. Mechanism and role of microsomal oxidation.
14. Biological importance of tissue respiration and oxidative phosphorylation.
15. Oxidative decarboxylation of pyruvate. Pyruvate dehydrogenises complex. Regulation.
16. Separate reactions of CAC. Enzymes, coenzymes.
17. Connection CAC with tissue respiration. Energetic balance of CAC and pyruvate decarboxylation.
Regulation.
18. Biological functions of CAC.
Metabolism of carbohydrates, lipids, proteins and it regulation
1. Sstructure and functions of monosacharides,disacharides,Homopolysacharides
2. Digestion and absorption of carbohydrates. Abnormal degradation of disacharides:
3. Interconversions of monosacharides. The metabolism of galactose and fructose.
4. The general pathways of glucose degradation in the organism. .
5. Glycogen metabolism: Synthesis of glycogen and its degradation in the liver and in the muscles
(glycogenolisis), Allosteric and hormonal regulation. Glycogen storage diseases. (Girke).
6. Glucolysis (aerobic and anaerobic). Biological role. Key reactions of glycolysis, enzymes.
Energy yield of aerobic and anaerobic degradation (the amount of ATP) of 1 molecule of glucose.
7. Interrelation between aerobic glycolysis, citric acid cycle and tissue respiration. The Paster effect.
8. Gluconeogenesis.Reactions uniqe to gluconeogenesis; substrates
9. Allosteric and hormonal regulation of glycolysis and gluconeogenesis.
10. Pentose monophosphate pathway (PPP).
11. Oxidative reactions. Biological role. Interrelation of glycolysis and PPP. Glucose-6-12.
phosphatedehydrogenase deficiency.
12. Disturbances in carbohydrate metabolism
a) fructosemia and galactosemia) lack of fructokinase
b ,Glycogen storage diseases. (Girke).
c) milk intolerance
d) Gluconeogenesis dosordes
13. Structure, classification and properties of dietary lipids (fatty, acids, triacylglycerols,
phospholipids, cholesterol). The essential fatty acids
14. Structure and function of cellular membranes
15. Digestion and Absorptionof triacylglycerols, phospholipids and cholesterol esters.
16. Synthesis of Fatty acids ,Triacylglycerols, glyc erophospholipids
17. β-oxidation of fatty acids: Energy yield.
18. Synthesis of cholesterol (stage 1 - reactions to mevalonate). Regulation.
19. Ketone bodies metabolism.Synthesis in the liver and utilization in the peripheral tissues
71
20. Plasma lipoproteins: composition, size and density of lipoprotein particles, functions, and
metabolism.
21. Disturbance of lipid metabolism:
a) Disturbance of lipid digestion and absorption: steatorrhea, familial lipoproteinlipase deficiency
(Chylomicronemia).
b)Excessive production of ketone bodies. Ketoacidosis. .
a) Obesity; lipid dystrophy of the liver.
b) Fatty liver
c) Atherosclerosis
22.Role of proteins in overall nitrogen metabolism. Nitrogen balance. Essential and non-assential
amino acids.
23. Digestion and absorption of dietary proteins. Chemical composition of gastric juice and kinds of
acidity. Abnormalities components of gastric juice.
24. Body nitrogen metabolism. Sources and fates of amino acids.
25. The direct and indirect deamination. of amino acids
26.Transamination, it role in amino acids metabolism. Diagnostic value of plasma aminotranseferases
(AST and ALT).
27. Decarboxylation of amino acids for synthesis of biogenic amines.
28..Metabolism of amino acids carbon skelletons. Glycogenic and ketogenic amino acids.
29.Metabolism of ammonia: sources, mechanism of toxicity, hyperammoniemia.
30. Render harmless of ammonia.
31. Urea cycle, its key role in ammonia detoxication. Reactions of the cycle, enzymes, fate of urea.
32. Metabolism of separate amino asids: (Metionin, Glycin and serin, Phenylalanine and tyrosine .
33. Biological role and symthesis of creatine.
34. Metabolic defects in amino acid metabolism: Phenylketonuria, alcaptonuria, and albinism,
homocystinuria).
72
Tasks for control module preparing.
Task 1.
1. Write the reaction of succinct conversion to fumarate by formulas.
2. Name the enzyme.
3. Is this enzyme simple or conjugated?
4. What coenzyme takes part in this reaction?
5. Name vitamin that is precursor of biologically active coenzyme.
6. Specific inhibitor of this enzyme is:
Task 2.
Write down the structural formula of ascorbic acid.
Task 3.
1. Give other names of vitamin PP.
2. What coenzyme forms does it have? (Name only):
3. Describe the biological functions of PP (Name reactions, processes in which it takes
part in).
4. Identify the symptoms and causes of this vitamin deficiency. Name the disease in
avitaminosis.
73
Task 4.
1. Write the structural formula of substrate in the e. t.c. below:
Isocitrate → NAD →FMN•FeS→?→ cit.b(FeS)·citC1 →cit C → cit аа3 → О2
2. Name missing component of e. t.c.
3. Point coupling sites in this e. t.c.
4. Name inhibitors of the site I
5. P/O coefficient for the given substrate = ? How many ATPs are formed in
this case?
Task 5.
Which process do these compounds take part in?
Glyceraldehyde-3-P, phosphoenolpyruvate, fructose-6-P, dihydroxyaceton-P, lactate.
*2. Arrange them in corresponding order.
3. What is the role of this process in the body?
4. Write the formula one of these compounds.
Task 6.
Which metabolic process is described by scheme below?
Fatty acid A Acylcarnitine Acyl-CoA B β- Hydroxyacyl-CoA
2. Write the names of compounds A and B
3. What is the biological role of this process in the body?
4. Draw the equation of the reaction in fragment that is printed in bold type. (By
formulas and words).
74
5. Name enzyme that catalyses this reaction.
6. Draw the reaction, which is catalyzed by this enzyme.
Task 7.
1. Which metabolic process is described by scheme below?
1,3-diphosphoglycerateA 2-phosphoglycerate (Phosphoenolpyruvate B)
Lactate
2. Write the names of compounds A and B
3. What is the biological role of this process in the body?
4. Draw the equation of the reaction in fragment that is printed in bold type. (By
formulas and words).
5. Name enzyme that catalyses this reaction.
Task 8. Patient with bile stone illness complains of sickness and apathy after
intake of fat -rich food. His feces test contains drops of unsplit fat and has a graywhite color. Pancreatic steatorrhea was diagnosed in patient on the basis of
number of objective indexes.
1.
2.
3.
4.
Which process is impaired in patient?
Draw the equation of the reaction, which is disturbed (by words).
Name the enzyme that catalyses this reaction. Where it is synthesized?
What does mean the term steatorrhea ?
A. Urine contains drops of fat .
B. Rethynthnesis of lipids is broken
C. Emulsification of lipids is broken
D. Triacylglycerols concentration in blood increased
E. Feces contains drops of fat and has a gray-white color
75
Task9. Which metabolic process is impearled under Von Girke disease? Signs of
disease.
2. Name defective enzyme.
Task 10. The cause of hemolytic anemia in patient is low activity of pyruvate
kinase of red blood cells.
1.
2.
3.
4.
Draw the equation of the reaction, which is disturbed (by words).
Which metabolic process is impaired in this patient?
What is the role of this metabolic process in erythrocytes?
Choose regulatory enzyme of this process:
A. Enolase
B. Aldolase
C. Lactate dehydrogenase
D. Phnosphofructokinase
E. Glyceradehyde-3-P- dehydrogenase
Task 11. Symptoms of ammonia neurotoxic effect on the CNS ( vomiting,
dehydration, convulsions, tremors, slurring of speech) was developed in newborn
with genetic defect of carbamoyl phosphate synthetase. It is known that this
pathology can cause coma and death.
1. Which metabolic process is impaired in deficiency of this enzyme?
2. Draw the equation of the reaction, which is catalyzed by this enzyme (by words).
3. Explain appearance of mention clinical symptoms?
4. Name this pathology:
A. Phenylketonuria
B. Galactosemia
C. Hyperammoniemia
D. Aglycogenosis
E. Intolerance to lactose
.
76