* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ppt_ch26_e_body defence mechanisms
Survey
Document related concepts
Immunocontraception wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
DNA vaccination wikipedia , lookup
Immune system wikipedia , lookup
Molecular mimicry wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Innate immune system wikipedia , lookup
Transcript
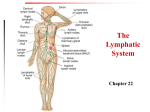
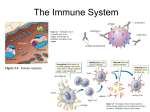
Bubble Boy Disease Severe combined immunodeficiency (SCID) It is a genetic disorder in which the adaptive immune system is nonfunctional. SCID is a severe form of heritable immunodeficiency. It is also known as the “bubble boy” disease because its victims are extremely vulnerable to infectious diseases and some of them, such as David Vetter, become famous for living in a sterile environment. The human immunodeficiency virus (HIV) infects and destroys a particular type of white blood cells. HIV white blood cell The human immunodeficiency virus (HIV) infects and destroys a particular type of white blood cells. HIV white blood cell Over time, the immunity of the infected person may be seriously weakened, resulting in AIDS. HIV white blood cell Patients usually die from infections that are harmless in healthy people. HIV white blood cell 1 What is immunity Immune System: Functions • Protects from pathogens and foreign molecules –Parasites –Bacteria –Viruses • Removes dead or damaged cells • Attempts to recognize and remove abnormal cells Immune System dysfunction • Incorrect responses –Autoimmune disease (Type 1 diabetes) • Overactive responses –Allergies • Lack of response –Immunodeficiency disease (AIDS) 9 26.1 Non-specific defence mechanisms immune system (免疫系統) pathogens Immune system • provides body defence non-specific defence mechanisms (非特異性防禦機制) specific defence mechanisms (特異性防禦機制) Non-specific defence mechanisms • provide general protection against pathogens • prevent the entry of all types of foreign substances non-specific Non-specific defence mechanisms • include physical and chemical barriers first line of defence (第一道防線) Non-specific defence mechanisms • include physical and chemical barriers blood clotting phagocytosis inflammatory responses Physical barriers • physical structures that prevent pathogens from entering the body Physical barriers 1 Skin • covers the whole body layer of dead cells - constantly worn away and replaced by new cells Physical barriers 2 Ciliated epithelium of the respiratory tract ciliated epithelial cell physical barrier closely packed cells Physical barriers 2 Ciliated epithelium of the respiratory tract mucussecreting cell produces sticky mucus traps dust and pathogens 26.1 Non-specific defence mechanisms Physical barriers 2 Ciliated epithelium of the respiratory tract cilia beating action moves dust and pathogens in mucus up from the bronchi to the pharynx Physical barriers 2 Ciliated epithelium of the respiratory tract cilia beating action dust and pathogens are swallowed or coughed out Chemical barriers • chemical secretions that may kill or stop the growth of pathogens Chemical barriers 1 Sebum • secreted by sebaceous glands • a natural antiseptic (消毒劑) • kills pathogens on the skin sebum Chemical barriers 2 Gastric juice • secreted by gastric glands • contains hydrochloric acid • kills pathogens in the food in the stomach gastric juice Chemical barriers 3 Tears and saliva • secreted by tear glands tears Chemical barriers 3 Tears and saliva • secreted by salivary glands Chemical barriers 3 Tears and saliva • contain lysozyme (溶菌酶) breaks down the cell walls of certain bacteria on the conjunctiva and in the mouth cavity Chemical barriers 4 Vaginal secretion • acidic inhibits the growth of pathogens in the vagina Mucus is a chemical barrier that kills pathogens. mucus In fact, mucus is a physical barrier that only traps pathogens without killing them. mucus 26.1 Identifying features of mammalian skin that are related to body defence 1 Examine a prepared slide of mammalian skin under a microscope using low power magnification or a skin model. 2 Identify the structures that are related to body defence. Blood clotting • blood clot (血凝塊) seals the wound and stops breeding prevents pathogens from entering through the wound Blood clotting • formation of a blood clot: - a blood vessel damaged - blood platelets attracted to the wound Blood clotting • formation of a blood clot: - blood platelets release chemicals soluble protein fibrinogen (纖維蛋白原) insoluble fibrin (纖維蛋白) 34 35 Blood clotting • formation of a blood clot: - blood cells trapped in the net of fibrin blood platelet white blood cell red blood cell Blood clotting • formation of a blood clot: - blood clot dries to form a scab (痂) covering the wound Phagocytosis • carried out by phagocytes (吞噬細胞) phagocyte bacterium Phagocytosis phagocyte pathogen enzymes nucleus Phagocytosis 1 A phagocyte engulfs a pathogen. Phagocytosis 2 The pathogen is digested by enzymes. Phagocytosis 3 The digested pathogen is released. Inflammatory responses Animation wound is infected pathogens Inflammatory responses 1 Capillary increases its permeability. capillary Inflammatory responses 2 More phagocytes come out of the capillary. phagocyte Inflammatory responses 3 Phagocytes engulf and digest the pathogens in the tissue. carrying out phagocytosis Inflammatory responses • increased blood flow and accumulation of tissue fluid infected area becomes red, hot, swollen and painful inflammation (炎症) Inflammatory responses • pus (膿) may form inside the wound - consists of the remains of killed pathogens and dead phagocytes The inflammatory response mobilizes nonspecific defense forces Tissue damage triggers the inflammatory response Skin surface Swelling Pin Phagocytes Bacteria Chemical signals White blood cell 1 Tissue injury; release of chemical signals such as histamine Phagocytes and fluid move into area 2 Dilation and increased leakiness 3 Phagocytes (macrophages and of local blood vessels; migration of phagocytes to the area neutrophils) consume bacteria and cell debris; tissue heals The inflammation can disinfect tissues and limit further infection Lymphatic system Lymphatic system = lymphatic ducts and lymph nodes The lymphatic system becomes a crucial battleground during infection It returns tissue fluid to the circulatory system It fights infections LYMPHATIC VESSEL Tonsil Right lymphatic duct, entering vein Thoracic duct VALVE Lymph nodes Thoracic duct, entering vein Blood capillary Tissue cells Interstitial fluid Thymus Appendix Spleen LYMPHATIC CAPILLARY Masses of lymphocytes and Macrophages Bone marrow Lymphatic vessels Primary lymph organs : Thymus and bone marrow Secondary lymph organs : lymph nodes This lymphatic vessel is taking up fluid from tissue spaces in the skin • It will return it as lymph to the blood – Lymph contains less oxygen and fewer nutrients than interstitial fluid LYMPHATIC VESSEL VALVE Blood capillary Tissue cells Interstitial fluid LYMPHATIC CAPILLARY Lymph nodes are key sites for fighting infection They are packed with lymphocytes and macrophages Masses of lymphocytes and macrophages Outer capsule of lymph node Macrophages Lymphocytes Figure 23.3C, D 1 Non-specific defence mechanisms prevent the entry of all types of foreign substances . 2a The first line of defence includes physical and chemical barriers that prevent pathogens from entering the blood and other tissues. 2b Possible entrance of pathogens: Body surface Barrier: Skin Physical Chemical Method of prevention: • Covers the whole body to prevent the entry of pathogens 2b Possible entrance of pathogens: Body surface Barrier: Sebum Physical Chemical Method of prevention: • An antiseptic that kills pathogens 2c Possible entrance of pathogens: Respiratory tract Barrier: Ciliated epithelium Physical Chemical Method of prevention: • Cells are closely packed to prevent the entry of pathogens 2c Possible entrance of pathogens: Respiratory tract Barrier: Ciliated epithelium Physical Chemical Method of prevention: • Mucus traps pathogens 2c Possible entrance of pathogens: Respiratory tract Barrier: Ciliated epithelium Physical Chemical Method of prevention: Cilia beat to move the trapped pathogens upwards 2c Possible entrance of pathogens: Respiratory tract Barrier: Ciliated epithelium Physical Chemical Method of prevention: • The trapped pathogens are then swallowed or coughed out 2d Possible entrance of pathogens: Stomach Barrier: Gastric juice Physical Chemical Method of prevention: • Contains hydrochloric acid to kill pathogens 2e Possible entrance of pathogens: Eyes Barrier: Tears Physical Chemical Method of prevention: • Contains lysozyme to kill pathogens 2f Possible entrance of pathogens: Mouth Barrier: Saliva Physical Chemical Method of prevention: • Contains lysozyme to kill pathogens 2g Possible entrance of pathogens: Vagina Barrier: Vaginal secretion Physical Chemical Method of prevention: • Acidity inhibits the growth of pathogens 3 Pathogens can get into the body through a wound on the skin. By blood clotting , a blood clot is formed which seals the wound to prevent the entry of pathogens. 4 Phagocytosis is the process by which phagocytes engulf pathogens. 5 In an inflammatory response, arterioles in the infected area dilate, and capillaries there increase their permeability . 5 More blood flows to the area and more phagoctyes come out of the capillaries to engulf and kill the pathogens in the tissues. 6 Signs of inflammation: Redness and heat result from the increased blood flow, and swelling and pain result from the accumulation of tissue fluid. Non-specific vs specific immunity The Nature of Immunity Immunity was originally used to indicate exemption from taxes and this meaning still exits in the term "diplomatic immunity". • adaptive immune response (應變性) / specific immunity • Major characteristics of adaptive immune response • 多樣性 (Diversity) • 專一性(specificity) • 記憶性(memory) • 自我辨識(self/non-self recognition) Characteristics of Adaptive immunity A ntigenic specificity To distinguish subtle difference among antigens I mmunologic memory A second encounter with the same antigen induces a heightened state of immune reactivity D iversity To recognize billions of uniquely different structures on foreign antigens S elf/nonself recognition To respond only to foreign antigens 26.2 Specific defence mechanisms antigens (抗原) activate lymphocytes (淋巴細胞) B cells T cells carry out immune responses (免疫反應) Lymphocytes BONE MARROW Two kinds of lymphocytes carry out the immune response B cells secrete antibodies that attack antigens T cells attack cells infected with pathogens Stem cell THYMUS Via blood Immature lymphocytes Antigen receptors T cell B cell HUMORAL IMMUNITY OTHER PARTS OF THE LYMPHATIC SYSTEM Via blood Lymph nodes, spleen, and other lymphatic organs CELLMEDIATED IMMUNITY Final maturation of B and T cells in lymphatic organ Antigens • stimulate immune responses • two groups: foreign antigens and self antigens - come from outside of the body e.g. cell surface proteins of viruses or toxins from bacteria surface proteins virus Antigens • stimulate immune responses • two groups: foreign antigens and self antigens - produced by the person’s own body e.g. surface proteins on red blood cells surface proteins red blood cell Antigens • immune system can usually recognize self antigens and does not attack them Antigens foreign antigens not yet entered the host cells activate B cells carry out humoral immune responses (HIR) (體液免疫反應) Humoral immune responses • B cells are formed and mature in the bone marrow • B cells have antigen receptors that only bind with a specific antigen B cells -- humoral immunity Triggered by a specific antigen, a B cell differentiates into an effector cell The effector cell is called a plasma cell The plasma cell secretes antibodies Humoral immune responses activated by antigens and helper T cells multiplies and differentiates into memory B cell B cell plasma cell Humoral immune responses Antibodies to act against antigens produces plasma cell Humoral immune responses • antibody is a Y-shaped protein molecule antigenbinding site polypeptide chains disulphide bond Antigens have specific regions where antibodies bind to them Antigens are molecules to which antibodies bind Antibody A molecules Antigenbinding sites Antigens Antigen Antibody B molecule Humoral immune responses antigen-antibody complex antigen Humoral immune responses • production of antibodies is specific - each type of antigen leads to the production of only one type of antibody 3D animation Humoral immune responses Actions of antibodies 1 Lysis (溶菌) a Antibodies attach to pathogen and make holes in it. Animation antibodies pathogen (virus or bacterium) Humoral immune responses Actions of antibodies 1 Lysis (溶菌) a Antibodies attach to pathogen and make holes in it. Humoral immune responses Actions of antibodies 1 Lysis (溶菌) b Pathogen is lysed (被溶解) and killed. hole Humoral immune responses Actions of antibodies 2 Help in phagocytosis a Antibodies attach to pathogen. pathogen antibody phagocyte Humoral immune responses Actions of antibodies 2 Help in phagocytosis b Phagocyte detects the antibodies and engulfs the pathogen. Humoral immune responses Actions of antibodies 2 Help in phagocytosis c Pathogen is killed by phagocytosis. Humoral immune responses Actions of antibodies 3 Stick pathogens into clumps - pathogens stuck together by antibodies and cannot reproduce or enter cells antibodies pathogens Humoral immune responses Actions of antibodies 3 Stick pathogens into clumps - pathogens stuck together by antibodies and cannot reproduce or enter cells Humoral immune responses Actions of antibodies 4 Neutralize toxins of pathogens - antibodies act as antitoxins (抗毒素) to neutralize toxins toxins antibodies Humoral immune responses Actions of antibodies 4 Neutralize toxins of pathogens - antibodies act as antitoxins (抗毒素) to neutralize toxins Binding of antibodies to antigens inactivates antigens by Neutralization Agglutination Precipitation of (blocks viral binding sites; of microbes dissolved antigens coats bacterial toxins) Make holes in cell membrane Complement Bacteria Virus molecule Antigen Bacterium molecules Enhances Phagocytosis Macrophage Foreign cell Leads to Cell lysis Hole Clonal selection musters defensive forces against specific antigens When an antigen enters the body, it activates only lymphocytes with complementary receptors B and T cells multiply into clones of specialized effector cells that defend against the triggering antigen This is called clonal selection Antigen molecules Variety of B cells in a lymph node Antigen receptor (antibody on cell surface) Cell growth division, and differentiation Clone of many effector cells secreting antibodies Endoplasmic reticulum Antibody molecules Figure 24.7 The initial immune response results in a type of “memory” In the primary immune response, clonal selection produces memory cells These cells may confer lifelong immunity When memory cells are activated by subsequent exposure to an antigen, they mount a more rapid and massive secondary immune response Unstimulated lymphocyte First exposure to antigen FIRST CLONE Memory cells Second exposure to antigen Effector cells SECOND CLONE More memory cells New effector cells Figure 24.8B PRIMARY RESPONSE (initial encounter with antigen) Antigen Antigen receptor on a B cell Antigen binding Cell growth, to a B cell division, and differentiation Clone of cells Memory B cell Plasma cell Antibody molecules Later SECONDARY RESPONSE (can be years later) exposure to Cell division, same differentiation antigen Larger clone Memory B cell of cells Plasma cell Antibody molecules Figure 24.9 Cell-mediated immune response infected cells or cancer cells stimulate T cells carry out cell-mediated immune responses (CMIR) Cell-mediated immune response • T cells are formed in the bone marrow and mature in the thymus gland (胸腺) • T cells have receptors on their surface that fit a specific antigen Cell-mediated immune response • several types: helper T cells, killer T cells and memory T cells thymus gland T helper cells activate HIR activated by infected cells or cancer cells B cell activates helper T cell carries out HIR Cell-mediated immune response activated by infected cells or cancer cells T cell secretes activates helper T cell activate phagocytes lymphokines (淋巴激活素) Cell-mediated immune response T cell multiplies and differentiates memory T cell into destroys cells directly killer T cell (殺手 T 細胞) Cytotoxic T / killer T cells bind to infected body cells and destroy them by making hole in the cell membrane 1 Cytotoxic T cell binds to infected cell Foreign antigen 2 Perforin makes holes in infected cell’s membrane 3 Infected cell is destroyed Hole forming INFECTED CELL Perforin molecule Cytotoxic T cell Figure 24.13C Killer T cells may help prevent cancer Killer T cells may attack cancer cells The surface molecules of cancer cells are altered by the disease Primary and secondary immune responses • immunological memory (免疫記憶): the ability of memory B cells and memory T cells to ‘remember’ the type of antigen from the previous exposure Primary and secondary immune responses • primary response occurs on the first exposure to an antigen • secondary response occurs when the same antigen enters the body again Primary and secondary immune responses • usually slow / longer latent period • normally takes 3–14 days to produce enough antibodies or cells • antigens have time to cause damage disease symptoms Primary and secondary immune responses • faster, stronger and lasts longer • memory cells multiply and differentiate quickly into a larger number of plasma cells, killer T cells and memory cells • kills the pathogen before it can multiply and cause a disease secondary recovery response concentration of antibodies in blood primary response 0 7 14 first exposure 21 28 35 second exposure days concentration of antibodies in blood primary response secondary recovery response latent period (潛伏期) 0 7 14 first exposure 21 28 35 second exposure days concentration of antibodies in blood primary response secondary recovery response concentration of antibodies 0 7 14 first exposure 21 28 35 second exposure days secondary recovery response primary response concentration of antibodies in blood period of existence of antibodies 0 7 14 first exposure 21 28 35 second exposure days Principle of vaccination • immunity can be enhanced by vaccination introduction of vaccines (疫苗) into the body Principle of vaccination • four types of vaccines: 1 Live, weakened pathogens e.g. vaccines of measles, mumps, rubella 2 Killed pathogens e.g. vaccines of poliomyelitis, rabies (狂犬病) Principle of vaccination • four types of vaccines: 3 Viral proteins e.g. vaccine of whooping cough 4 Inactivated bacterial toxins e.g. vaccines of diphtheria, tetanus Vaccines I # Many exotoxins can be modified chemically so that they retain their antigenicity but are no longer toxic. Such a modified exotoxin is called a toxoid. Vaccine II # Most agents used for immunization are either attenuated or inactivated pathogens or inactivated forms of natural microbial products. Alternative immunization strategies using bioengineered molecules eliminate exposure to microorganisms and, in some cases, even to protein antigen. Application of these strategies may provide safer and more targeted vaccines. Principle of vaccination • vaccine contains an antigen • introduced into the body orally or by injection Principle of vaccination antigen in vaccine stimulates primary response - production of some antibodies and killer T cells - production of memory cells that ‘remember’ the type of antigen Principle of vaccination invasion by the same antigen stimulates secondary response - production of a larger amount of specific antibodies and killer T cells in a shorter time Principle of vaccination • makes use of the specificity and immunological memory • not completely without risk • protects the health of the community if a large number of people are vaccinated Active and passive immunity • given by antibodies produced by our own plasma cells • acquired naturally when a person recovers from an infection • acquired artificially by vaccination Active and passive immunity • start of the immunity is relatively slow • long lasting Active and passive immunity • given by direct transfer of antibodies from immune persons Active and passive immunity • occurs naturally in babies when: - antibodies diffuse from mother’s blood to embryo’s blood in placenta Active and passive immunity • occurs naturally in babies when: - babies are fed with breast milk Active and passive immunity • occurs artificially when: - antibodies are injected for treatment of diseases • immunity starts immediately • lost after a short period of time when the antibodies break down Connection: Monoclonal antibodies are powerful tools in the lab and clinic fusing B cells specific for a single antigenic determinant with easy-to-grow tumor cells Antigen injected Tumor cells grown into mouse in culture B cells Tumor cells (from spleen) Cells fused to generate hybrid cells Single hybrid cell grown in culture Hybrid cell culture, producing monoclonal antibodies Antibody These cells are useful in medical diagnosis – Example: home pregnancy tests • They are also useful in the treatment of certain cancers Connection: Malfunction or failure of the immune system causes disease Autoimmune diseases : The immune system turns against the body’s own molecules, including SLE (紅斑狼瘡), RA (類風濕性關節 炎), type I diabetes, asthma, Crohn’s disease 孔羅氏症(消化道瘜肉),…. Immunodeficiency diseases : Immune components are lacking, and infections recur. Innate immune deficiency : Severe combined immunodeficiency (SCID) Acquired immune deficiency : AIDS Physical and emotional stress may weaken the immune system Arthritis X-ray RA is an autoimmune disorder in which your own body mistakenly attacks healthy tissue, causing inflammation and damage to your joints. About 1% of the US population suffers from RA. Patients usually develop the signs and symptoms of the disease between the ages of 35 and 50, with women affected 2 to 3 times more often than are men. Connection: Allergies are overreactions to certain environmental antigens Allergies are abnormal sensitivities to allergens in the surroundings B cell (plasma cell) Histamine Antigenic Mast determinant cell Allergen B cells make (pollen grain) antibodies Antibodies Allergen binds to Histamine is attach to antibodies on released, causing mast cell mast cell allergy symptoms SENSITIZATION: Initial exposure to allergen LATER EXPOSURE TO SAME ALLERGEN Allergy-causing fungal spores Figure 24.17x Connection: AIDS leaves the body defenseless The AIDS virus attacks helper T Cells This cripples both cell-mediated and humoral immunity So far, AIDS is incurable Drugs and vaccines offer hope for the future Practicing safer sex could save many lives The Continuing Problem of HIV Acquired immune deficiency syndrome (AIDS) is epidemic throughout much of the world 14,000 people are infected with the AIDS virus every day HIV is the virus that causes AIDS HIV is transmitted mainly in blood and semen Former L.A. Laker Magic Johnson is one of 900,000 Americans who are HIV-positive AIDS is an immunodeficiency disease caused by a virus In 1981, increased rates of two rare diseases, Kaposi’s sarcoma, and pneumonia caused by a protozoan P. carinii, were the first signals of a new threat to humans, later known as acquired immunodeficiency syndrome, or AIDS. Both conditions were previously known to occur mainly in severely immunosuppressed individuals. People with AIDS are susceptible to opportunistic diseases. Kaposi’s Sarcoma Unusual tumor arising from blood or lymphatic vessels in multiple locations Tumor began to appear in young men with HIV ○ 2000 time higher than period before HIV ○ So common among AIDS patients became AIDS-defining condition Pneumocystosis(肺孢子蟲病) Causative agent - Pneumocystis carinii Tiny fungus formerly considered a protozoan Differs from many fungi in cell wall components ○ Consequently resistant to many fungal medications Pathogenesis Spores of organism are inhaled into lung ○ Attach to alveolar walls Alveoli fill with fluid, mononuclear cells and organisms Alveolar walls become thickened and scarred. Interferes with free passage of oxygen In 1983, a retrovirus, now called human immunodeficiency virus (HIV), had been identified as the causative agent of AIDS. With the AIDS mortality close to 100%, HIV is the most lethal pathogen ever encountered. Molecular studies reveal that the virus probably evolved from another HIV-like virus in chimpanzees in central Africa and appeared in humans sometimes between 1915 and 1940. ○ These first rare cases of infection and AIDS went unrecognized. Two major strains HIV-1 and HIV-2. HIV-1 is the more widely distributed and more virulent. Both strains infect cells that bear CD4 molecules, especially helper T cells and also macrophages, some lymphocytes and some brain cells. HIV infected cells: Among the susceptible WBCs, what do they have in common? CD4 functions as the major receptor for the virus. Other HIV receptors present on the surface of some WBCs are implicated: • Clues: Some people who are innately resistant to HIV-1 owe their resistance to defective chemokine receptors. chemokines – chemicals secreted by WBC when signaling with one another. • What is your conclusion? What is your conclusion? The entry of the virus requires not only CD4 on the surface of the susceptible cells but also a second protein molecule, a co-receptor. Defective chemokine receptor prevents HIV from binding and infecting cells. Once inside a cell, HIV RNA is reversetranscribed, and the product DNA is integrated into the host genome. This directs the production of new virus particles. Because a retrovirus exists integrated in the host genome of the infected cell, immune responses fail to eradicate it from the body. Even more challenging : frequent mutational changes that occur in each round of virus replication. Give two reasons why it is difficult to remove the virus from our body? Give two reasons why it is difficult to remove HIV from our body? •Because a retrovirus exists integrated in the host genome of the infected cell, immune responses fail to eradicate it from the body. •Even more challenging : frequent mutational changes that occur in each round of virus replication. Give two reasons why it is difficult to remove HIV from our body? Because a retrovirus exists integrated / hidden in the host genome of the infected cell, immune responses fail to eradicate it from the body. Even more challenging : frequent mutational changes occur in each round of virus replication fools our immune system – render immunologic memory and immune specificity ineffective. The body is then engaged in a Prolonged battle against HIV. (1) The immune response diminishes the initial viral load, but HIV continues to replicate in lymphatic tissue. (2) Viral load gradually rises as HIV is released from lymphatic tissue and helper T cell levels decrease. Consequence? The body is then engaged in a Prolonged battle against HIV. (1) The immune response diminishes the initial viral load, but HIV continues to replicate in lymphatic tissue. (2) Viral load gradually rises as HIV is released from lymphatic tissue and helper T cell levels decrease. Consequence? This results in extensive loss of humoral and cell-mediated immunity. After an initial peak, virus levels in the blood fall as anti-HIV antibodies, produced 1 to 12 months after infection, rise. After the early drop in HIV levels in the blood, the virus continues to be produced by cells in the lymph nodes, causing structural and functional damage. In time, the concentration of HIV in the blood increases as a result of : the breakdown of lymphatic tissue function and diminishing responses to the infection because of the depletion of helper T cells. The time required for an HIV infection to progress to severe helper T cell depletion and AIDS varies greatly, but it currently averages about ten years. A person who is HIV-positive will have blood tested positive for the presence of antibodies to the virus. However, a HIV-negative blood test result does not completely guarantee a safe blood supply, WHY? because an infected individual may require several weeks to 6 months (window period) before anti-HIV antibodies become detectable. After the early drop in HIV levels in the blood, the virus continues to be produced by cells in the lymph nodes, causing structural and functional damage. In time, the concentration of HIV in the blood increases as a result of : the breakdown of lymphatic tissue function and diminishing responses to the infection because of the depletion of helper T cells. The time required for an HIV infection to progress to severe helper T cell depletion and AIDS varies greatly, but it currently averages about ten years. During most of this time, the individual exhibits only moderate hints of illness, such as swollen lymph nodes and occasional fever. How do you think doctors can monitor the progress of the disease? by measuring changes in the level of T cells, although measures of viral load are a better indicator of disease prognosis and of the effectiveness of anti-HIV treatment. The time required for an HIV infection to progress to severe helper T cell depletion and AIDS varies greatly, but it currently averages about ten years. During most of this time, the individual exhibits only moderate hints of illness, such as swollen lymph nodes and occasional fever. How do you think doctors can monitor the progress of the disease? by measuring changes in the level of T cells. Or measures of viral load - a better indicator of disease prognosis and of the effectiveness of anti-HIV treatment. At this time, HIV infection cannot be cured, and the progression to AIDS cannot be prevented. New, expensive drug therapies can slow this progression. Suggest how these drugs might work: slow viral replication by 1) inhibiting DNA synthesis, 2) inhibiting reverse transcriptase, and 3) protein synthesis inhibitors Combinations of these drugs (a cocktail) decrease viral load and therefore allow the number of helper T cells to rise. At this time, HIV infection cannot be cured, and the progression to AIDS cannot be prevented. New, expensive drug therapies can slow this progression. Suggest how these drugs might work: slow viral replication by • - inhibiting DNA synthesis, • - inhibiting reverse transcriptase, and • - protein synthesis inhibitors Combinations of these drugs (a cocktail) decrease viral load and therefore allow the number of helper T cells to rise. Highly Active Anti-retroviral therapy (HAART) Reverse transcriptase inhibitors and protease inhibitors, provide a "one-two punch," interrupting HIV's replication cycle at different points and reducing the virus in many cases to undetectable levels. HOW ANTI-HIV DRUGS WORK Entry inhibitors bind to the proteins on the outside of the HIV virus and stop it from entering the target cell (Fuzeon only). Nucleoside reverse transcriptase inhibitors stop HIV copying its genes into the cell. Nucleosides are the building block for genes. The drugs supply faulty versions of these building blocks (drugs include abacavir, AZT, ddI, 3TC). Non-nucleoside reverse transcriptase inhibitors also block the gene-copying process. They disable the enzyme that controls it (drugs include nevirapine and efavirenz). Protease inhibitors disable protease, an enzyme which plays a key role in the formation of the new virus (drugs include amprenavir, lopinavir, ritonavir, nelfinavir). HAART reduce the virus in many cases to undetectable levels. • Even though ARV drugs are getting more powerful in inhibiting the effects of HIV, one must remember that these do not cure HIV infection and AIDS. • Individuals who are on HAART can still transmit the virus to other people. When the (HIV) replicates, it does not make perfect copies of itself but rather, creates new strains in the process. This means that an HIV+ person actually has many different strains of the virus inside his/her system. Suggest why the ‘cocktail treatment’ is preferred rather than a single drug? Suggest why the ‘cocktail treatment’ is preferred rather than a single drug? • HIV evolve quickly because it has a very short life cycle and high mutation rate. • New strains of HIV which are resistant to the effects of a particular antiretroviral (ARV) drug may appear and then replicate quickly. • For a treatment regimen to be effective over the long term, it has to include more than one ARV drug at a time. Taking two or more ARV drugs concurrently, known as combination therapy, can vastly reduce the rate at which drug resistance develops. 170 Transmission of HIV Transmission of HIV requires the transfer of body fluids containing infected cells, such as semen or blood, from person to person: • Unprotected sex (that is, without a condom) among male homosexuals • and transmission via nonsterile needles (typically among intravenous drug users) • However, transmission of HIV among heterosexuals is rapidly increasing as a result of unprotected sex with infected partners. HIV is not transmitted by casual contact. So far, only one case of HIV transmission by kissing has been reported, and both individuals had bleeding gums. Transmission of HIV from mother to child can occur during fetal development or during nursing. Mother-to-child transmission accounts for more than 90% of all HIV infections in infants and children worldwide. HIV screening has virtually eliminated blood transfusions as a route of transmission in developed countries. 河南爱滋病村 马深义一家住在中国河南上蔡县文楼村,他的家庭就是爱滋病的受害者。他们 一家五口人,有四人感染了艾滋病,只有9岁的大女儿是健康的。《好死不如赖 活着》没有故事、没有情节、没有背景音乐、没有字正腔圆的叙述、没有宏大 的场面,整部影片就是在纪录这个家庭的日常生活。影片的镜头从2001年的春 末夏初开始,历经盛夏、深秋、严冬,一直到春节,近距离地拍摄了马深义一 家面对爱滋病和死亡的人生经历。 As of 2000 the Joint United Nations Program on AIDS estimates that 30 to 40 million people worldwide are living with HIV or HIV/AIDS. Of these, approximately 70% reside in sub- Saharan Africa. The number of people with AIDS is expected to grow by nearly 20% per year. The best approach for slowing the spread of HIV is to educate people about the practices that transmit the disease, such as using nonsterile needles and having sex without a condom. Any individual who has sex with a partner who had unprotected sex with another person during the past two decades risks exposure to HIV. HIV on a lymphocyte HIV budding collage (大雜燴) Figure 24.18x2 HIV Prevention and Treatment No approved vaccine Most people infected are unaware Virus on surfaces can be inactivated with commercially available disinfectants and heat at 56°C for more that 30 minutes Knowledge of transmission greatest tool for control Use of condoms not 100% effective but have been shown to decrease transmission Avoidance of practices that favor HIV transmission HIV vaccine prospects Currently no approved vaccines In theory, vaccine could be used in two ways Prevention vaccine Immunize uninfected individuals against disease Therapeutic vaccine Boost immunity of those already infected Successful vaccine must •get around HIV variability •Be effective in preventing direct spread of HIV from cell to cell Successful vaccine must NOT • Be capable of turning into disease-causing strain • Be oncogenic – cancer causing • Stimulate an autoimmune response Vaccine trial in humans has been undertaken for at least 10 experimental vaccines All have failed and prospects do not look favorable A monumental safe-sex message in Paris Pope says condoms are not the solution to Aids - they make it worse A monumental safe-sex message in Paris Pope says condoms are not the solution to Aids - they make it worse Pope Benedict stressed that the Roman Catholic Church is in the forefront of the battle against Aids. The Vatican encourages sexual abstinence to fight the spread of the disease. A monumental safe-sex message in Paris 14,000 people get infected with HIV every day. 2 million people die of Aids each year. A monumental safe-sex message in Paris Sub-Saharan Africa HIV & AIDS statistics (2010) Country People living with HIV/AIDS Adult (1549) rate % Women with HIV/AIDS Children with HIV/AIDS AIDS deaths Orphans due to AIDS Cameroon 610,000 5.3 320,000 54,000 37,000 330,000 Chad 210,000 3.4 110,000 23,000 11,000 120,000 Congo 77,000 3.4 40,000 7,900 5,100 51,000 Ghana 260,000 1.8 140,000 27,000 18,000 160,000 Kenya 1,500,000 6.3 760,000 180,000 80,000 1,200,000 Mozambique 1,400,000 11.5 760,000 130,000 74,000 670,000 Nigeria 3,300,000 3.6 1,700,000 360,000 220,000 2,500,000 South Africa 5,600,000 17.8 3,300,000 330,000 310,000 1,900,000 Total subSaharan Africa 22,500,000 5.0 12,100,000 2,300,000 1,300,000 14,800,000 Notes Adults in this page are defined as men and women aged over 15, unless specified otherwise. Children are defined as people under the age of 15, whilst orphans are children aged under 18 who have lost one or both parents to AIDS. There is no single perfect solution to the problem of Aids Telling people to abstain doesn’t make everyone abstain Telling people NOT to use condom undermines the effort of the fight against AIDs and makes a serious global public health problem in places where AIDs is rapidly spreading e.g. Africa Botswana, 23.9% of adults between 15 and 49 are HIV positive; Swaziland, where 26.1% of adults have HIV; 26.2 Specific defence mechanisms 1 Antigens are substances that stimulate immune responses , activate the immune system to produce antibodies , and combine with specific antibodies. 26.2 Specific defence mechanisms 2 Humoral immune response uses antibodies to act against specific antigens that have not yet entered host cells. 26.2 Specific defence mechanisms 3 How antibodies act against pathogens: a Antibodies may attach to the antigens of pathogens and lyse them. 26.2 Specific defence mechanisms 3 How antibodies act against pathogens: b Antibodies may help the phagocytes engulf the pathogens more easily. 26.2 Specific defence mechanisms 3 How antibodies act against pathogens: c Antibodies may help pathogens stick into clumps , preventing them from reproducing or entering cells. 26.2 Specific defence mechanisms 3 How antibodies act against pathogens: d Antibodies may act as antitoxins which neutralize the toxins secreted by pathogens. 26.2 Specific defence mechanisms 4 Cell-mediated immune response uses T cells to destroy cells infected with specific antigens and cancer cells. 26.2 Specific defence mechanisms 5 Compare B cells and T cells: Formed in Mature in B cells T cells Bone marrow Bone marrow Thymus gland 26.2 Specific defence mechanisms 5 Compare B cells and T cells: B cells give rise to: - Plasma cells which produce antibodies to act against antigens that have not yet entered host cells 26.2 Specific defence mechanisms 5 Compare B cells and T cells: B cells give rise to: - Memory B cells which ‘remember’ the type of antigen and are responsible for the secondary response 26.2 Specific defence mechanisms 5 Compare B cells and T cells: T cells give rise to: - Helper T cells which can activate other T cells and B cells - Killer T cells which destroy infected cells or cancer cells directly 26.2 Specific defence mechanisms 5 Compare B cells and T cells: T cells give rise to: - Memory T cells which ‘remember’ the type of antigen and are responsible for the secondary response 26.2 Specific defence mechanisms 5 Compare B cells and T cells: B cells Responsible HIR for T cells CMIR 26.2 Specific defence mechanisms 6 Distinguish primary and secondary responses: Primary response Effected by stimulation of B cells and T cells Secondary response Effected by stimulation of memory B cells and memory T cells 26.2 Specific defence mechanisms 6 Distinguish primary and secondary responses: Primary response Secondary response Shorter Longer latent period latent period ( slower response) ( faster response) 26.2 Specific defence mechanisms 6 Distinguish primary and secondary responses: Primary response Secondary response Smaller amount of antibodies and killer T cells produced Larger amount of antibodies and killer T cells produced 26.2 Specific defence mechanisms 6 Distinguish primary and secondary responses: Primary response Secondary response Lasts for a short Lasts longer period of time 26.2 Specific defence mechanisms 7a Vaccination is the introduction of a vaccine , which contains an antigen , into the body. A vaccine may contain live and weakened pathogens, killed pathogens, viral proteins or inactivated bacterial toxins. 26.2 Specific defence mechanisms 7b Vaccination makes use of the specificity and immunological memory of the specific defence mechanisms. The vaccine produces a primary response. 26.2 Specific defence mechanisms 7b Any subsequent invasion by the same antigen in the vaccine will produce a secondary response, giving enhanced immunity to the disease. 26.2 Specific defence mechanisms 8 Distinguish active immunity and passive immunity: Active immunity Passive immunity Antibodies are Antibodies are produced by our transferred from own plasma cells immune persons 26.2 Specific defence mechanisms 8 Distinguish active immunity and passive immunity: Active immunity Passive immunity Acquired naturally Acquired naturally when a person through the diffusion recovers from an of antibodies in the and placenta infection breast-feeding 26.2 Specific defence mechanisms 8 Distinguish active immunity and passive immunity: Active immunity Acquired artificially by vaccination (for disease prevention) Passive immunity Acquired artificially by injection of antibodies (for the treatment of diseases) 26.2 Specific defence mechanisms 8 Distinguish active immunity and passive immunity: Active immunity Passive immunity Start of immunity is Start of immunity is slow fast 26.2 Specific defence mechanisms 8 Distinguish active immunity and passive immunity: Active immunity Passive immunity Lasts longer Lasts for a short period of time 1 What is immunity? Immunity is the ability of the body to resist a disease. 2 Which type of white blood cell is necessary to activate the defensive reactions of the body? Helper T cells are necessary to activate the defensive reactions of the body. 3 How does a low level of those white blood cells lead to weakened immunity? With only a low level of helper T cells, few B cells and T cells are activated to carry out immune responses. Body defence consists of non-specific defence mechanisms specific defence mechanisms non-specific defence mechanisms include physical chemical barriers barriers blood clotting phagocytosis inflammatory response physical barriers chemical barriers form first line of defence phagocytosis carried out by phagocytes specific defence mechanisms include humoral immune cell-mediated response immune response carried out by carried out by T cells some are helper T cells B cells activate T cells can secrete lymphokines activate phagocytes T cells multiply and differentiate into killer T cells memory T cells B cells multiply and differentiate into memory B cells plasma cells produce antibodies memory T cells memory B cells responsible for immunological memory