* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 26 - McGraw Hill Higher Education
Light-dependent reactions wikipedia , lookup
Western blot wikipedia , lookup
Two-hybrid screening wikipedia , lookup
Point mutation wikipedia , lookup
Microbial metabolism wikipedia , lookup
Nicotinamide adenine dinucleotide wikipedia , lookup
Butyric acid wikipedia , lookup
Genetic code wikipedia , lookup
Metalloprotein wikipedia , lookup
Phosphorylation wikipedia , lookup
Glyceroneogenesis wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Blood sugar level wikipedia , lookup
Adenosine triphosphate wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Biosynthesis wikipedia , lookup
Proteolysis wikipedia , lookup
Oxidative phosphorylation wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Citric acid cycle wikipedia , lookup
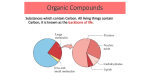
Chapter 26 Lecture Outline See PowerPoint Image Slides for all figures and tables pre-inserted into PowerPoint without notes. 26-1 Copyright (c) The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Nutrition and Metabolism • • • • • Nutrition Carbohydrate Metabolism Lipid and Protein Metabolism Metabolic States and Metabolic Rate Body Heat and Thermoregulation 26-2 Body Weight • Stable with equal energy intake and output – around a homeostatic set point • Determined by combination of environmental and hereditary factors – 30-50% of variation between individuals due to heredity – rest due to eating and exercise habits 26-3 Gut-Brain Peptides • Appetite regulators – short term • effects last minutes to hours – long term • effects last weeks to years 26-4 Short-term Appetite Regulators • Ghrelin – produces hunger • Peptide YY – satiety • Cholecystokinin – satiety 26-5 Short-term Appetite Regulators • Ghrelin – hunger – from parietal cells of empty stomach – also stimulates hypothalamus release of human growth hormone releasing hormone 26-6 Short-term Appetite Regulators • Peptide YY (PPY) – satiety – from enteroendocrine cells in ileum and colon – secreted in proportion to calories consumed – acts as ileal break • slows stomach emptying 26-7 Short-term Appetite Regulators • Cholecystokinin (CCK) – satiety – from enteroendocrine cells of duodenum and jejunum – appetite-suppressing effect on brain 26-8 Long-term Appetite Regulators • Leptin – secreted by adipocytes in proportion to body fat stores • Insulin – pancreatic beta cells – effect similar to leptin (but weaker) 26-9 Hypothalamus • Receptors for gut-brain peptides that regulate release of: 1. neuropeptide Y (hunger) • stimulated by gherlin • inhibited by PYY, leptin, and insulin 2. melanocortin (satiety) • stimulated by leptin, and CCK 26-10 Appetite Regulation 26-11 Other Factors in Appetite Regulation • Appetite is briefly satisfied by – chewing – swallowing – stomach filling • Neurotransmitters stimulate desire for different foods – norepinephrine – carbohydrates – galanin – fats – endorphins – protein 26-12 Calories • One calorie - amount of heat required to raise temperature of 1 g of water 1 °C – 1000 calories is a kilocalorie or Calorie • Fats contain about 9 kcal/g • Carbohydrates and proteins, about 4 kcal/g – sugar and alcohol are “empty” calories -- few nutrients • Substance used for fuel is oxidized primarily to make ATP 26-13 Nutrients • Ingested chemical used for growth, repair or maintenance • Macronutrients consumed in large amounts – proteins, fats and carbohydrates • Micronutrients needed in small amounts • Recommended daily allowances (RDA) – safe estimate of daily intake for standard needs • Essential nutrients can not be synthesized – minerals, vitamins, 8 amino acids and 1-3 fatty acids must be consumed in the diet 26-14 Carbohydrates • Carbohydrates found in 3 places in body – muscle and liver glycogen; blood glucose • Most carbohydrate serves as fuel – neurons and RBCs depend on glucose • Sugars do serve as structural components – nucleic acids, glycoproteins and glycolipids, ATP • Blood glucose carefully regulated by insulin and glucagon 26-15 RDA and Dietary Sources of Carbs • Carbohydrates are rapidly oxidized, RDA greater than any other nutrient (175 g/day) • Dietary sources: – monosaccharides = glucose, galactose and fructose • liver converts galactose and fructose to glucose – outside hepatic portal system, only blood sugar is glucose – normal blood sugar concentration ranges 70 to 110 mg/dL – disaccharides = table sugar (sucrose), maltose, lactose – polysaccharides = starch, glycogen and cellulose • Nearly all dietary carbohydrates come from plants 26-16 Dietary Fiber • Fibrous material that resists digestion • Fiber is important to diet (RDA is 30 g/day) – excess interferes with mineral absorption - iron • Water-soluble fiber (pectin) – blood cholesterol and LDL levels • Water-insoluble fiber (cellulose, lignin) – absorbs water in intestines, softens stool, gives it bulk, speeds transit time 26-17 Lipids • Average adult male 15% fat; female 25% fat – body’s stored energy • hydrophobic, contains 2X energy/g, compact storage • glucose and protein sparing (no protein utilized for energy) – fat-soluble vitamins (A,D,E,K) absorbed with dietary fat • ingest less than 20 g/day risks deficiency 26-18 Functions of Lipids • Diverse functions – structural • phospholipids and cholesterol are components of plasma membranes and myelin – chemical precursors • cholesterol - a precursor of steroids, bile salts and vitamin D • fatty acids - precursors of prostaglandins and other eicosanoids 26-19 Fat Requirements and Sources • Should be less than 30% of daily calorie intake – typical American gets 40-50% • Most fatty acids synthesized by body – essential fatty acids must be consumed • Saturated fats – animal origin -- meat, egg yolks and dairy products • Unsaturated fats – found in nuts, seeds and most vegetable oils • Cholesterol – found in egg yolks, cream, shellfish, organ meats and other meats 26-20 Serum Lipoproteins • Lipids transported in blood as lipoproteins – protein and phospholipid coat around a hydrophobic cholesterol and triglyceride core – soluble in plasma; bind to cells for absorption 26-21 Serum Lipoproteins • Categorized into 4 groups by density: more protein = higher density – chylomicrons – very low-density (VLDLs) – low-density (LDLs) – high-density (HDLs) 26-22 Serum Lipoproteins 26-23 Chylomicrons • Form in absorptive cells of small intestine – enter lymphatic system, then blood – capillary endothelium has lipoprotein lipase to hydrolyze monoglycerides – resulting free fatty acids (FFAs) and glycerol enter fat cells to be resynthesized into triglycerides for storage – chylomicron remnant degraded by liver 26-24 VLDL and LDL • VLDL – produced by liver to transport lipids to adipose tissue for storage – when triglycerides removed become LDLs (mostly cholesterol) • LDL – absorbed by cells in need of cholesterol for membrane repair or steroid synthesis 26-25 HDL • Production and function – liver produces an empty protein shell – travels through blood, picks up cholesterol – delivers cholesterol to liver, for elimination in bile 26-26 Total Cholesterol • Desirable to maintain total cholesterol concentration of < 200 mg/dL – most cholesterol is endogenous – dietary restrictions lower blood cholesterol levels • by 5% with restriction of dietary cholesterol • by 15 to 20% with restriction of certain saturated fats – vigorous exercise lowers blood cholesterol 26-27 Desirable Lipoprotein Levels • High levels of HDL – indicate cholesterol is being removed from arteries • Low levels LDL – high LDL correlates with cholesterol deposition in arteries • Recommendations – exercise regularly – avoid smoking, saturated fats, coffee and stress 26-28 Lipoprotein Processing • Three pathways 26-29 Proteins • 12-15% of body mass – mostly in skeletal muscles • Functions – muscle contraction • movement of body, cells, cell structures – cell membranes (receptors, cell identity, pumps) – fibrous proteins (collagen, keratin) • structural – globular proteins (antibodies, myoglobin, enzymes) • functional – plasma proteins: blood osmolarity and viscosity 26-30 Requirements for Protein • RDA - 44-60 g/day • Nutritional value depends on proportions of amino acids – 8 essential amino acids can not be synthesized • isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan and valine • Cells do not store surplus protein • Complete proteins (dietary) – supply all amino acids in right amount needed to synthesize protein 26-31 Dietary Sources • Animal proteins (meat, eggs and dairy) are complete proteins – closely match human proteins in amino acid composition • Plant sources must be combined in the right proportions – beans and rice are a complementary choice 26-32 Nitrogen Balance • Rate of nitrogen ingestion equals rate of excretion – proteins are chief dietary source of nitrogen – excretion chiefly as nitrogenous wastes • Positive nitrogen balance – occurs in children; they ingest more than they excrete – promoted by growth and sex hormones • Negative nitrogen balance – body proteins being broken down for fuel (muscle atrophy) – glucocorticoids promote protein catabolism in states of stress 26-33 Functions of Minerals • Calcium and phosphorus – bones and teeth • Phosphorus – phospholipids, ATP, CP, buffers, nucleic acids • Calcium, iron, magnesium and manganese – cofactors for enzymes • Iron - essential for hemoglobin and myoglobin • Chlorine - component of stomach acid (HCl) • Mineral salts – electrolytes; govern function of nerve and muscle cells; regulate distribution of body water 26-34 Dietary Sources of Minerals • Vegetables, legumes, milk, eggs, fish and shellfish • Animal tissues contain large amounts of salt – carnivores rarely lack salt in their diets – herbivores often supplement by ingesting soils • Recommended sodium intake is 1.1 g/day • Typical American diet contains 4.5 g/day 26-35 Vitamins • Body synthesizes some vitamins from precursors – niacin, vitamin A and D – vitamin K, pantothenic acid, biotin, folic acid • produced by intestinal bacteria • Water-soluble vitamins (C, B) – absorbed with water in small intestine; not stored • Fat-soluble vitamins (A, D, E, K) – absorbed with dietary lipids; stored 26-36 Vitamins 26-37 Carbohydrate Metabolism • Dietary carbohydrate burned as fuel within hours of absorption (glucose catabolism) C6H12O6 + 6O2 6CO2 + 6H2O • Transfers energy from sugar to ATP 26-38 Glucose Catabolism • Series of small steps to efficiently transfer energy to ATP (reduces energy lost as heat) • Three major pathways – glycolysis (yields 2 ATP) • glucose (6C) split into 2 pyruvic acid molecules (3C) – aerobic respiration (yields 34-36 ATP) • completely oxidizes pyruvic acid to CO2 and H2O – anaerobic fermentation (if no O2 available) • pyruvic acid reduced to lactic acid – replenishes NAD+ so glycolysis can continue 26-39 Overview of ATP Production 26-40 Coenzymes • Capture energetic electrons from glucose during its catabolism – coenzymes reduced • gains energy (electron) • charge reduced (electrons have negative charge) • NAD+ (nicotinamide adenine dinucleotide) – derived from niacin (B vitamin) – NAD+ + H- + H+ NADH + H+ • FAD (flavin adenine dinucleotide) – derived from riboflavin – FAD + H- + H+ FADH2 26-41 Steps of Glycolysis (1) • Phosphorylation – glucose enters cell has phosphate added - ATP used – maintains favorable concentration gradient, prevents glucose from leaving cell • Priming – isomerization occurs – phosphorylation further activates molecule ATP used • Cleavage – molecule split into 2 three-carbon molecules 26-42 Steps of Glycolysis (2) • Oxidation – removes H+ and H– NAD+ + H- NADH • Dephosphorylation – transfers phosphate groups to ADP to form ATP – 4 ATP produced (2 ATP used) for a net gain of 2 ATP – produces pyruvic acid 26-43 Anaerobic Fermentation • Fate of pyruvic acid depends on oxygen availability • In an exercising muscle, demand for ATP > oxygen supply; ATP produced by glycolysis – glycolysis can not continue without supply of NAD+ – NADH reduces pyruvic acid to lactic acid, restoring NAD+ • Lactic acid travels to liver to be oxidized back to pyruvic when O2 is available (oxygen debt) – then stored as glycogen or released as glucose • Fermentation is inefficient, not favored by brain or heart 26-44 Aerobic Respiration • Most ATP generated in mitochondria, require oxygen as final electron acceptor • Principle steps – matrix reactions occur in fluids of mitochondria – membrane reactions whose enzymes are bound to the mitochondrial membrane 26-45 Mitochondrial Matrix Reactions • Three steps prepare pyruvic acid to enter citric acid cycle – decarboxylation so that a 3-carbon becomes a 2-carbon compound – convert that to an acetyl group (remove H) – bind it to coenzyme A • Known as formation of acetyl-coenzyme A 26-46 Mitochondrial Matrix Reactions 26-47 Mitochondrial Matrix Reactions • Citric Acid Cycle • Acetyl-Co A (a C2 compound) combines with a C4 to form a C6 compound (citric acid)-- start of cycle • Water is removed -- NAD+ is reduced to NADH -CO2 is removed to form a C5 compound-- NAD+ is reduced to NADH -- CO2 is removed to form a C4 compound • FAD is reduced to FADH2 -- water is added -NAD+ is reduced to NADH • Original C4 compound is reformed – ready to restart cycle 26-48 Summary of Matrix Reactions 2 pyruvate + 6H2O 6CO2 2 ADP + 2 Pi 2 ATP 8 NAD+ + 8 H- + 8 H+ 8 NADH + 8 H+ (2 NADH produced during formation of acetyl-CoA) 2 FAD + 2 H2 2 FADH2 • Carbon atoms of glucose have all been carried away as CO2 and exhaled. • Energy lost as heat, stored in 2 ATP, 8 reduced NADH, 2 FADH2 molecules of the matrix reactions and 2 NADH from glycolysis • Citric acid cycle is a source of substances for synthesis of fats and nonessential amino acids 26-49 Membrane Reactions • Purpose - to oxidize NADH and FADH2, transfer their energy to ATP and regenerate them • Reactions carried out by series of compounds attached to inner mitochondrial membrane called electron transport chain – FMN is derivative of riboflavin, iron-sulfur centers, Coenzyme Q, Copper ions bound to membrane proteins and cytochromes (5 enzymes with iron cofactors) • As electrons are transferred along transport chain, their potential orbital energy is released • Final electron acceptor is oxygen: accepts 2 electrons and 2 H+ to form a water molecule 26-50 Electron Transport Chain 26-51 Chemiosmotic Mechanism • Electron transport chain energy fuels enzyme complexes – pump protons from matrix into space between inner and outer mitochondrial membranes – creates steep electrochemical gradient for H+ across inner mitochondrial membrane • Inner membrane is permeable to H+ at channel proteins called ATP synthase • Chemiosmotic mechanism - H+ flow rushing back through these channels drives ATP synthesis 26-52 Chemiosmotic ATP Synthesis 26-53 Overview of ATP Production • NADH releases an electron pair to electron transport system and H+ to prime pumps – enough energy to synthesize 3 ATP • FADH2 releases its electron pairs further along electron-transport system – enough energy to synthesize 2 ATP • Complete aerobic oxidation of glucose to CO2 and H2O produces 36-38 ATP – efficiency rating of 40% -- rest is body heat 26-54 ATP Generated by Oxidation of Glucose 26-55 Glycogen Metabolism • ATP is quickly used after it is formed -- it is not a storage molecule – extra glucose will not be oxidized, it will be stored • Glycogenesis -- synthesis of glycogen – stimulated by insulin (average adult contains 450 g) • Glycogenolysis -- glycogen glucose – stimulated by glucagon and epinephrine – only liver cells can release glucose back into blood • Gluconeogenesis -- synthesis of glucose from noncarbohydrates, such as fats and amino acids 26-56 Glucose Storage and Use 26-57 Lipids • Triglycerides are stored in adipocytes – constant turnover of molecules every 3 weeks • released into blood, transported and either oxidized or redeposited in other fat cells • Lipogenesis = synthesizing fat from other sources – amino acids and sugars used to make fatty acids and glycerol • Lipolysis = breaking down fat for fuel – glycerol is converted to PGAL and enters glycolysis – fatty acids are broken down 2 carbons at a time to produce acetyl-CoA (beta oxidation) 26-58 Lipogenesis and Lipolysis Pathways 26-59 Ketogenesis • Fatty acids catabolized into acetyl groups (by beta-oxidation in mitochondrial matrix) may – enter citric acid cycle as acetyl-CoA – undergo ketogenesis • metabolized by liver to produce ketone bodies – acetoacetic acid – -hydroxybutyric acid – acetone • rapid or incomplete oxidization of fats raises blood ketone levels (ketosis) and may lead to a pH imbalance (ketoacidosis) 26-60 Proteins • Amino acid pool - dietary amino acids plus 100 g of tissue protein broken down each day into free amino acids • May be used to synthesize new proteins • As fuel -- first must be deaminated (removal of NH2)--what remains is converted to pyruvic acid, acetyl-CoA or part of citric acid cycle – during shortage of amino acids, the reverse occurs for protein synthesis – the NH2 become ammonia (NH3) which is toxic and which the liver converts to urea (excreted in urine) 26-61 Pathways of Amino Acid Metabolism 26-62 Urea Synthesis • Liver converts ammonia (NH3) to urea which is removed from blood by kidneys 26-63 Absorptive State • Lasts about 4 hours during and after a meal – time of nutrient absorption and use for energy needs • Carbohydrates – blood glucose is available to all cells for ATP synthesis – excess is converted by liver to glycogen or fat • Fats – taken up by fat cells from chylomicrons in the blood – primary energy substrate for liver, fat and muscle cells • Amino acids – most pass through the liver and go onto other cells – in liver cells, may be used for protein synthesis, used for fuel for ATP synthesis or used for fatty acid synthesis 26-64 Regulation of Absorptive State • Regulated by insulin secreted in response to elevated blood glucose and amino acid levels and the hormones gastrin, secretin and cholecystokinin • Insulin – increases the cellular uptake of glucose by 20-fold – stimulates glucose oxidation, glycogenesis and lipogenesis but inhibits gluconeogenesis – stimulates active transport of amino acids into cells and promotes protein synthesis • high protein, low carbohydrate meals stimulate release of both insulin and glucagon preventing hypoglycemia 26-65 Postabsorptive State • Homeostasis of blood glucose critical to brain – when stomach and small intestine are empty- stored fuels are used • Carbohydrates – glucose is drawn from glycogen reserves for up to 4 hours and then synthesized from other compounds • Fat – adipocytes and liver cells convert glycerol to glucose – free fatty acids are oxidized by liver to ketone bodies • other cells use for energy-- leaving glucose for brain • Protein metabolism – used as fuel when glycogen and fat reserves depleted – wasting away occurs with cancer and other diseases 26-66 from loss of appetite and altered metabolism Regulation of Postabsorptive State • By sympathetic nervous system and glucagon • Blood glucose drops, glucagon secreted – glycogenolysis and gluconeogenesis raise glucose levels – lipolysis raises free fatty acid levels 26-67 Regulation of Postabsorptive State • Sympathoadrenal effects – promotes glycogenolysis and lipolysis under conditions of injury, fear, anger and stress – adipose, liver cells and muscle cells are richly innervated and also respond to epinephrine from adrenal medulla – Cortisol from adrenal cortex promotes blood glucose • fat and protein catabolism and gluconeogenesis – Growth hormone – opposes rapid in blood glucose 26-68 Metabolic Rate • Amount of energy used in the body in a given period of time (kcal/hr or kcal/day) – measured directly in calorimeter (water bath) – measured indirectly by oxygen consumption • Basal metabolic rate (BMR) – relaxed, awake, fasting, room comfortable temperature – adult male BMR is 2000 kcal/day(slightly less female) • Factors affecting total MR – pregnancy, anxiety, fever, eating, thyroid hormones, and depression 26-69 Body Heat and Thermoregulation • Homeostasis requires heat loss to match heat gain • Hypothermia - excessively low body temperature – can slow metabolic activity and cause death • Hyperthermia - excessively high body temperature – can disrupt enzymatic activity and metabolic activity and cause death • Thermoregulation - ability to balance heat production and heat loss 26-70 Body Temperature • “Normal” body temperature varies about 1.8 degrees F. in a 24-hour cycle – low in morning and high in late afternoon • Core body temperature is temperature of organs in cranial, thoracic and abdominal cavities – rectal temperature is an estimate – adult varies normally from 99.0 - 99.7 degrees F. • Shell temperature is temperature closer to the surface (oral cavity and skin) – adult varies normally from 97.9 - 98.6 degrees F. 26-71 Heat Production • Comes from energy-releasing chemical reactions such as nutrient oxidation and ATP use • From brain, heart, liver, endocrine and muscles – exercise greatly heat production in muscle 26-72 Modes of Heat Loss • Radiation - loss of body heat to objects around us – caused by molecular motion producing infrared radiation • Conduction - loss of body heat to the air which when warmed rises to be replaced by cooler air • Evaporation - heat loss as sweat evaporates – extreme conditions as much as 2L of sweat lost per hour, dissipating heat by as much as 600 kcal/hour 26-73 Thermoregulation • Hypothalamic thermostat monitors temperature of blood and skin, signals – heat-losing center to stimulate • cutaneous vasodilation • sweating – signals heat-promoting center to stimulate • • • • cutaneous vasoconstriction arrector pili muscle contraction shivering thermogenesis (if needed) nonshivering thermogenesis - thyroid hormone and BMR (seasonal adjustment) • Behavioral thermoregulation – get out of sun, remove heavy clothing 26-74 Disturbances of Thermoregulation • Fever – normal protective mechanism that elevates BMR which produces more heat elevating the BMR, etc. • Hyperthermia - exposure to excessive heat – heat cramps are muscle spasms due to electrolyte imbalance from excessive sweating – heat exhaustion -- severe electrolyte imbalance producing fainting, dizziness, hypotension – heat stroke -- body temperature > 104 °F, may cause delirium, convulsions, coma, and death • Hypothermia - exposure to excess cold – as core body temperature , BMR causing a further body temperature decrease, etc. (fatal if body 26-75 temperature 75 °F)